The Association of Infection with Delirium in the Post-Operative Period after Elective CABG Surgery
Abstract
1. Introduction
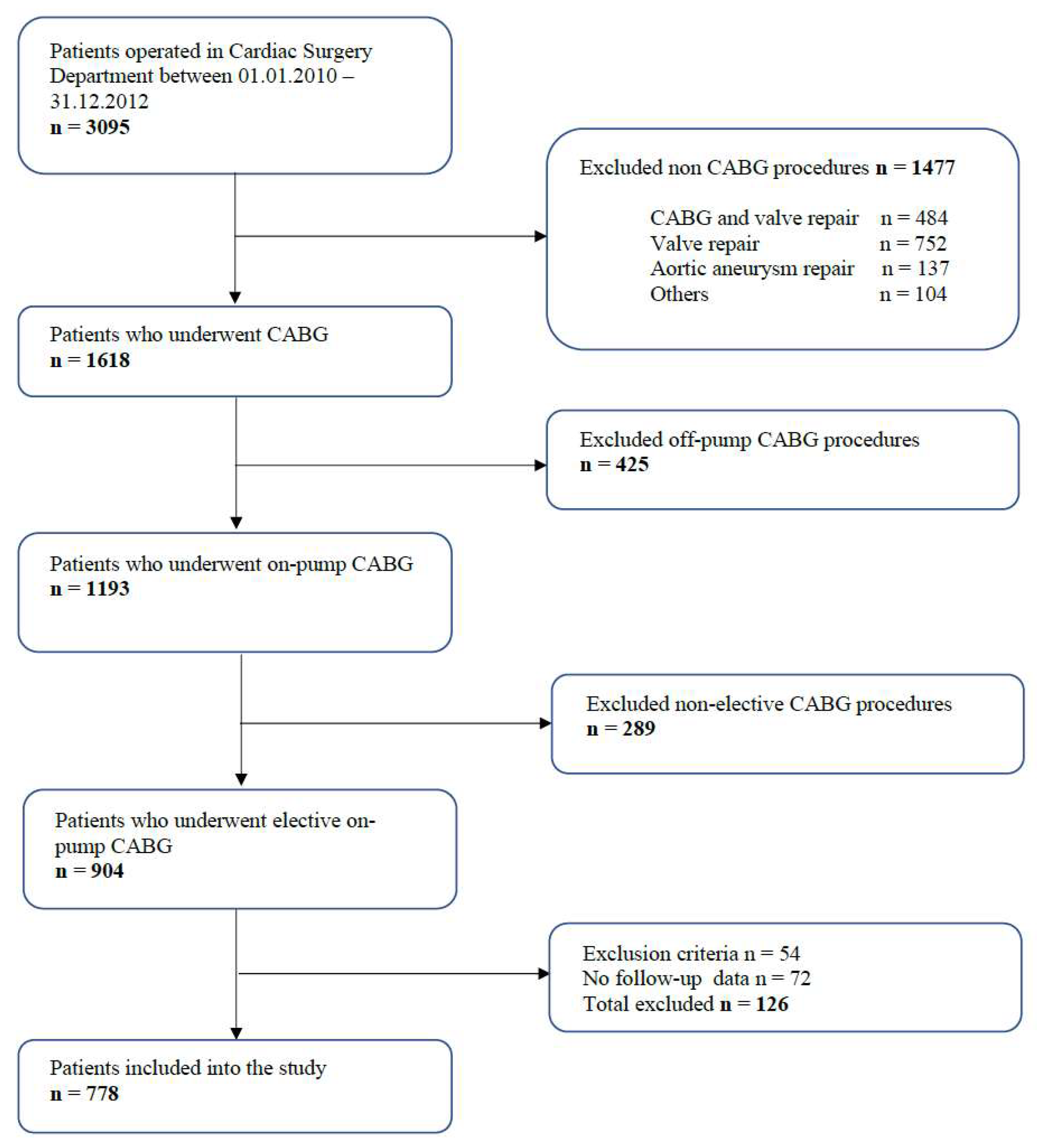
2. Materials and Methods
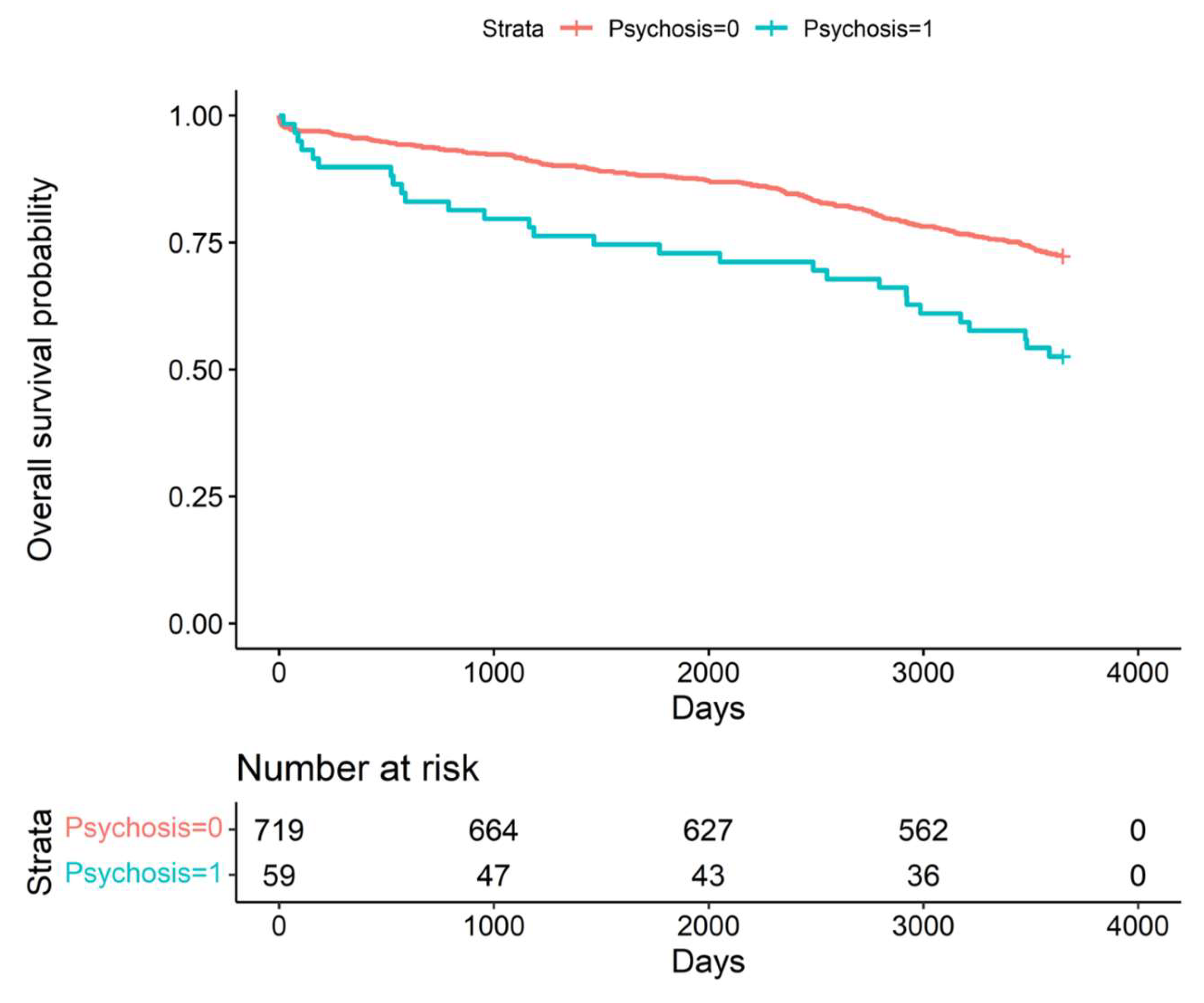
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.K.B.M.; AlKatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.E.A.H.; Alzaabi, M.E.H.; Al Darmaki, R.S. Lootah SNAH. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Nowbar, A.N.; Gitto, M.; Howard, J.P.; Francis, D.P.; Al-Lamee, R.; Shepard, D.; VanderZanden, A.; Naghavi, M.; Roth, G.A.; Huffman, M.D.; et al. Mortality From Ischemic Heart Disease. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005375. [Google Scholar] [CrossRef] [PubMed]
- Smulter, N.; Lingehall, H.C.; Gustafson, Y.; Olofsson, B.; Engström, K.G. Delirium after cardiac surgery: Incidence and risk factors. Interact. Cardiovasc. Thorac. Surg. 2013, 17, 790–796. [Google Scholar] [CrossRef]
- Sadlonova, M.; Vogelgsang, J.; Lange, C.; Günther, I.; Wiesent, A.; Eberhard, C.; Ehrentraut, J.; Kirsch, M.; Hansen, N.; Esselmann, H.; et al. Identification of risk factors for delirium, cognitive decline, and dementia after cardiac surgery (FINDERI-find delirium risk factors): A study protocol of a prospective observational study. BMC Cardiovasc. Disord. 2022, 22, 299. [Google Scholar] [CrossRef]
- Rose, L.; Burry, L.; Agar, M.; Blackwood, B.; Campbell, N.L.; Clarke, M.; Devlin, J.W.; Lee, J.; Marshall, J.C.; Needham, D.M.; et al. A core outcome set for studies evaluating interventions to prevent and/or treat delirium for adults requiring an acute care hospital admission: An international key stakeholder informed consensus study. BMC Med. 2021, 19, 143. [Google Scholar] [CrossRef] [PubMed]
- Kassie, G.M.; Nguyen, T.A.; Ellett, L.M.K.; Pratt, N.L.; Roughead, E.E. Preoperative medication use and postoperative delirium: A systematic review. BMC. Geriatr. 2017, 17, 298. [Google Scholar] [CrossRef]
- John, M.; Ely, E.W.; Halfkann, D.; Schoen, J.; Sedemund-Adib, B.; Klotz, S.; Radtke, F.; Stehr, S.; Hueppe, M. Acetylcholinesterase and butyrylcholinesterase in cardiosurgical patients with postoperative delirium. J. Intensive. Care 2017, 5, 29. [Google Scholar] [CrossRef]
- Aiello, G.; Cuocina, M.; La Via, L.; Messina, S.; Attaguile, G.A.; Cantarella, G.; Sanfilippo, F.; Bernardini, R. Melatonin or Ramelteon for Delirium Prevention in the Intensive Care Unit: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2023, 12, 435. [Google Scholar] [CrossRef]
- Alvarez, E.A.; Rojas, V.A.; Caipo, L.I.; Galaz, M.M.; Ponce, D.P.; Gutierrez, R.G.; Salech, F.; Tobar, E.; Reyes, F.I.; Vergara, R.C.; et al. Non-pharmacological prevention of postoperative delirium by occupational therapy teams: A randomized clinical trial. Front. Med. 2023, 10, 1099594. [Google Scholar] [CrossRef]
- Pagad, S.; Somagutta, M.R.; May, V.; Arnold, A.A.; Nanthakumaran, S.; Sridharan, S.; Malik, B.H. Delirium in Cardiac Intensive Care Unit. Cureus 2020, 12, e10096. [Google Scholar] [CrossRef]
- Xu, Y.; Ma, Q.; Du, H.; Yang, C.; Lin, G. Postoperative Delirium in Neurosurgical Patients: Recent Insights into the Pathogenesis. Brain Sci. 2022, 12, 1371. [Google Scholar] [CrossRef] [PubMed]
- Fatehi Hassanabad, A.; Bahrami, N.; Novick, R.J.; Ali, I.S. Delirium and depression in cardiac surgery: A comprehensive review of risk factors, pathophysiology, and management. J. Card. Surg. 2021, 36, 2876–2889. [Google Scholar] [CrossRef] [PubMed]
- Deininger, M.M.; Schnitzler, S.; Benstoem, C.; Simon, T.P.; Marx, G.; Panagiotidis, D.; Ziles, D.; Schnoering, H.; Karasimos, E.; Breuer, T. Standardized pharmacological management of delirium after on-pump cardiac surgery reduces ICU stay and ventilation in a retrospective pre-post study. Sci. Rep. 2023, 13, 3741. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Zhang, X.; Xu, S.; Peng, Y.; Li, S.; Huang, X.; Chen, L.; Lin, Y. Outcomes of postoperative delirium in patients undergoing cardiac surgery: A systematic review and meta-analysis. Front. Cardiovasc. Med. 2022, 9, 884144. [Google Scholar] [CrossRef]
- Satomoto, M. Predicting Postoperative Emergence Delirium From the Heart Rate Variability of Patients Undergoing Elective Cardiac Surgery. Cureus 2023, 15, e34613. [Google Scholar] [CrossRef]
- Sari, S.; Brooker, J.; Montalvo-Campana, M.; Shehata, P.; Pu, X.; Insler, S.; Ruetzler, K.; Troianos, C.A.; Turan, A. The association of hemoglobin with postoperative delirium and atrial fibrillation after cardiac surgery: A retrospective sub-study. Braz. J. Anesthesiol. 2023, in press. [Google Scholar] [CrossRef]
- Chen, H.; Mo, L.; Hu, H.; Ou, Y.; Luo, J. Risk factors of postoperative delirium after cardiac surgery: A meta-analysis. J. Cardiothorac. Surg. 2021, 16, 113. [Google Scholar] [CrossRef]
- Ma, X.; Chu, H.; Han, K.; Shao, Q.; Yu, Y.; Jia, S.; Wang, D.; Wang, Z.; Zhou, Y. Postoperative delirium after transcatheter aortic valve replacement: An updated systematic review and meta-analysis. J. Am. Geriatr. Soc. 2023, 71, 646–660. [Google Scholar] [CrossRef]
- Andrási, T.B.; Talipov, I.; Dinges, G.; Arndt, C.; Rastan, A.J. Risk factors for postoperative delirium after cardiac surgical procedures with cardioplegic arrest. Eur. J. Cardiothorac. Surg. 2022, 62, ezab570. [Google Scholar] [CrossRef]
- Kuswardhani, R.A.T.; Sugi, Y.S. Factors Related to the Severity of Delirium in the Elderly Patients With Infection. Gerontol. Geriatr. Med. 2017, 3, 2333721417739188. [Google Scholar] [CrossRef]
- Dutta, C.; Pasha, K.; Paul, S.; Abbas, M.S.; Nassar, S.T.; Tasha, T.; Desai, A.; Bajgain, A.; Ali, A.; Mohammed, L. Urinary Tract Infection Induced Delirium in Elderly Patients: A Systematic Review. Cureus 2022, 14, e32321. [Google Scholar] [CrossRef] [PubMed]
- Krinitski, D.; Kasina, R.; Klöppel, S.; Lenouvel, E. Associations of delirium with urinary tract infections and asymptomatic bacteriuria in adults aged 65 and older: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2021, 69, 3312–3323. [Google Scholar] [CrossRef] [PubMed]
- Mayne, S.; Bowden, A.; Sundvall, P.-D.; Gunnarsson, R. The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing—A systematic literature review. BMC Geriatr. 2019, 19, 32. [Google Scholar] [CrossRef]
- Spiropoulou, E.; Samanidis, G.; Kanakis, M.; Nenekidis, I. Risk Factors for Acute Postoperative Delirium in Cardiac Surgery Patients >65 Years Old. J. Pers. Med. 2022, 12, 1529. [Google Scholar] [CrossRef]
- Archbald-Pannone, L.R.; McMurry, T.L.; Guerrant, R.L.; Warren, C.A. Delirium and other clinical factors with Clostridium difficile infection that predict mortality in hospitalized patients. Am. J. Infect. Control. 2015, 43, 690–693. [Google Scholar] [CrossRef]
- de la Varga-Martínez, O.; Gutiérrez-Bustillo, R.; Muñoz-Moreno, M.F.; López-Herrero, R.; Gómez-Sánchez, E.; Tamayo, E. Postoperative delirium: An independent risk factor for poorer quality of life with long-term cognitive and functional decline after cardiac surgery. J. Clin. Anesth. 2023, 85, 111030. [Google Scholar] [CrossRef]
- Dzahini, O.; Singh, N.; Taylor, D.; Haddad, P.M. Antipsychotic drug use and pneumonia: Systematic review and meta-analysis. J. Psychopharmacol. 2018, 32, 1167–1181. [Google Scholar] [CrossRef]
- Lewin, J.; Maconochie, I. Capillary refill time in adults. Emerg. Med. J. 2008, 25, 325–326. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Sanfilippo, F.; Continella, C.; Triolo, T.; Messina, A.; Robba, C.; Astuto, M.; Hernandez, G.; Noto, A. Agreement between Capillary Refill Time measured at Finger and Earlobe sites in different positions: A pilot prospective study on healthy volunteers. BMC Anesthesiol. 2023, 23, 30. [Google Scholar] [CrossRef]
- Yamamoto, M.; Doi, K.; Hayase, N.; Asada, T.; Akamatsu, N.; Kaneko, J.; Hasegawa, K.; Morimura, N. Pulse oximetry-based capillary refilling evaluation predicts postoperative outcomes in liver transplantation: A prospective observational cohort study. BMC Anesthesiol. 2020, 20, 251. [Google Scholar] [CrossRef] [PubMed]
- Fahmei, T.B.; El-Shazly, S.; Ibrahim, H.S. Factors Associated with Postoperative Delirium among Geriatric Patients. Alex. Sci. Nurs. J. 2014, 16, 145–160. [Google Scholar] [CrossRef]

| Parameter | Delirium (−) n = 719 | Delirium (+) n = 59 | p |
|---|---|---|---|
| Female (n. %) | 170/719 (24%) | 17/59 (29%) | 0.9999 |
| Age (years. mean ± SD) | 64 (9) | 70 (10) | 0.0002 |
| Weight (kg. mean ± SD) | 81 (13) | 78 (11) | 0.3110 |
| BMI | 29.3 (8.4) | 28.8 (3.6) | 0.6530 |
| Smoking (n. %) | 312/719 (11) | 14 (59) | 0.0602 |
| ES (mean ± SD) | 3.77 (2.69) | 5.32 (2.41) | <0.0001 |
| ESlog (mean ± SD) | 4.7 (5.3) | 6.7 (4.7) | <0.0001 |
| LVEF (%. mean ± SD) | 50 (11) | 48 (11) | 0.5801 |
| NYHA functional class (n. %) | 0.9999 | ||
| 1 | 3/706 (0.4%) | 1/59 (1.7%) | |
| 2 | 138/706 (20%) | 10/59 (17%) | |
| 3 | 400/706 (57%) | 36/59 (61%) | |
| 4 | 165/706 (23%) | 12/59 (20%) | |
| Insulin intake (n. %) | 101/718 (14%) | 10/59 (17%) | 0.7277 |
| HbA1c (%, mean ± SD) | 2.11 (3.25) | 3.18 (3.80) | 0.1557 |
| Hb (mg/dL, mean ± SD) | 8.45 (0.79) | 8.17 (0.76) | 0.0711 |
| Hct (%, mean ± SD) | 0.41 (0.04) | 0.39 (0.04) | 0.1577 |
| PLT (mean ± SD) | 246 (66) | 261 (72) | 0.4609 |
| Serum creatinine level mg/dL (mean ± SD) | 0.95 (0.50) | 1.07 (1.08) | 0.5478 |
| Parameter | Delirium (−) n = 719 | Delirium (+) n = 59 | p |
|---|---|---|---|
| Insulin dependent diabetes (n. %) | 8/719 (1.1%) | 0/59 (0%) | 0.9999 |
| Insulin non-dependent diabetes (n. %) | 225/719 (31%) | 26/59 (44%) | 0.3664 |
| Prior stroke (n. %) | 32/719 (4.5%) | 5/59 (8.5%) | 0.9999 |
| TIA (n. %) | 6/719 (0.8%) | 0/59 (0%) | 0.9999 |
| Hypertension (n. %) | 552/719 (77%) | 52/59 (88%) | 0.2622 |
| Myocardial infarction (n. %) | 245/718 (34%) | 19/59 (32%) | 0.9999 |
| Atrial fibrillation (n. %) | 23/719 (3.2%) | 3/59 (5.1%) | 0.9999 |
| Hypercholesterolemia (n. %) | 57/719 (7.9%) | 3/59 (5.1%) | 0.9999 |
| Dyslipidemia (n. %) | 66/719 (9.2%) | 2/59 (3.4%) | 0.8493 |
| Peripheral arterial disease (n. %) | 77/719 (11%) | 10/59 (17%) | 0.8493 |
| Renal failure (n. %) | 31/719 (4.3%) | 3/59 (5.1%) | 0.9999 |
| Autoimmune diseases (n. %) | 14/719 (1.9%) | 1/59 (1.7%) | 0.9999 |
| Parameter | Delirium (−) n = 719 | Delirium (+) n = 59 | p |
|---|---|---|---|
| Duration of surgery (min. mean ± SD) | 152 (50) | 150 (22) | 0.9973 |
| Duration of CPB (min. mean ± SD) | 50 (15) | 49 (13) | 0.9973 |
| CPB fluid balance (mL. mean ± SD) | 572 (613) | 498 (749) | 0.7277 |
| IntraoperativeUF (mL. mean ± SD) | 148 (469) | 351 (671) | 0.0215 |
| LVEF day after surgery % | 52 (10) | 49 (11) | 0.1503 |
| Day 1 fluid balance (mL. mean ± SD) | −1105 (1060) | −807 (1109) | 0.2682 |
| Day 2 fluid balance (mL. mean ± SD) | −179 (849) | −115 (874) | 0.5801 |
| Overall fluid balance (mL. mean ± SD) | −1255 (1429) | −928 (1291) | 0.1557 |
| Intra-aortic balloon pump (n. %) | 4/716 (0.6%) | 0/59 (0%) | 0.9999 |
| Milrinone (n. %) | 17/704 (2.4%) | 3/58 (5.2%) | 0.9999 |
| Postoperative drainage (mL. mean ± SD) | 545 (335) | 559 (397) | 0.9973 |
| Postoperative Hb (mg/dL, mean ± SD) | 6.72 (0.81) | 6.63 (0.75) | 0.5801 |
| Postoperative Hct (%, mean ± SD) | 0.34 (0.05) | 0.32 (0.04) | 0.4609 |
| Postoperative PLT (,mean ± SD) | 189 (54) | 198 (51) | 0.4609 |
| Postoperative Cr level mg/dL (mean ± SD) | 1.03 (0.66) | 1.14 (0.61) | 0.0711 |
| RBC (mL. mean ± SD) | 138 (288) | 174 (296) | 0.5478 |
| PLT (mL. n. %) | 0.9973 | ||
| 0 | 599/717 (84%) | 48/59 (81%) | |
| 200 | 1/717 (0.1%) | 0/59 (0%) | |
| 250 | 60/717 (8.4%) | 4/59 (6.8%) | |
| 300 | 47/717 (6.6%) | 7/59 (12%) | |
| 500 | 2/717 (0.3%) | 0/59 (0%) | |
| 550 | 5/717 (0.7%) | 0/59 (0%) | |
| 600 | 3/717 (0.4%) | 0/59 (0%) | |
| CK-MB after 6 h | 38 (25) | 42 (32) | 0.6933 |
| CK-MB after 12 h | 44 (46) | 54 (49) | 0.4609 |
| CK-MB after 24 h | 48 (63) | 54 (47) | 0.4675 |
| Parameter | Delirium (−) n = 719 | Delirium (+) n = 59 | p |
|---|---|---|---|
| Postoperative TIA (n. %) | 4/719 (0.6%) | 1/59 (1.7%) | 0.9999 |
| Postoperative MI (n. %) | 12/719 (1.7%) | 1/59 (1.7%) | 0.9999 |
| Postoperative stroke (n. %) | 6/719 (0.8%) | 1/59 (1.7%) | 0.9999 |
| Postoperative AF (n. %) | 161/719 (22%) | 16/59 (27%) | 0.9999 |
| Infection (n. %) | 53/719 (7.4%) | 13/58 (22%) | 0.0037 |
| Infection source (n. %) | 0.0025 | ||
| 0 | 666/719 (93%) | 45/58 (78%) | |
| BSI | 14/719 (1.9%) | 1/58 (1.7%) | |
| SSI sternal | 10/719 (1.4%) | 5/58 (8.6%) | |
| SSI leg | 2/719 (0.3%) | 1/58 (1.7%) | |
| Pneumonia | 27/719 (3.8%) | 6/58 (10%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zukowska, A.; Kaczmarczyk, M.; Listewnik, M.; Zukowski, M. The Association of Infection with Delirium in the Post-Operative Period after Elective CABG Surgery. J. Clin. Med. 2023, 12, 4736. https://doi.org/10.3390/jcm12144736
Zukowska A, Kaczmarczyk M, Listewnik M, Zukowski M. The Association of Infection with Delirium in the Post-Operative Period after Elective CABG Surgery. Journal of Clinical Medicine. 2023; 12(14):4736. https://doi.org/10.3390/jcm12144736
Chicago/Turabian StyleZukowska, Agnieszka, Mariusz Kaczmarczyk, Mariusz Listewnik, and Maciej Zukowski. 2023. "The Association of Infection with Delirium in the Post-Operative Period after Elective CABG Surgery" Journal of Clinical Medicine 12, no. 14: 4736. https://doi.org/10.3390/jcm12144736
APA StyleZukowska, A., Kaczmarczyk, M., Listewnik, M., & Zukowski, M. (2023). The Association of Infection with Delirium in the Post-Operative Period after Elective CABG Surgery. Journal of Clinical Medicine, 12(14), 4736. https://doi.org/10.3390/jcm12144736






