JAK Inhibition in Juvenile Idiopathic Arthritis (JIA): Better Understanding of a Promising Therapy for Refractory Cases
Abstract
1. Introduction
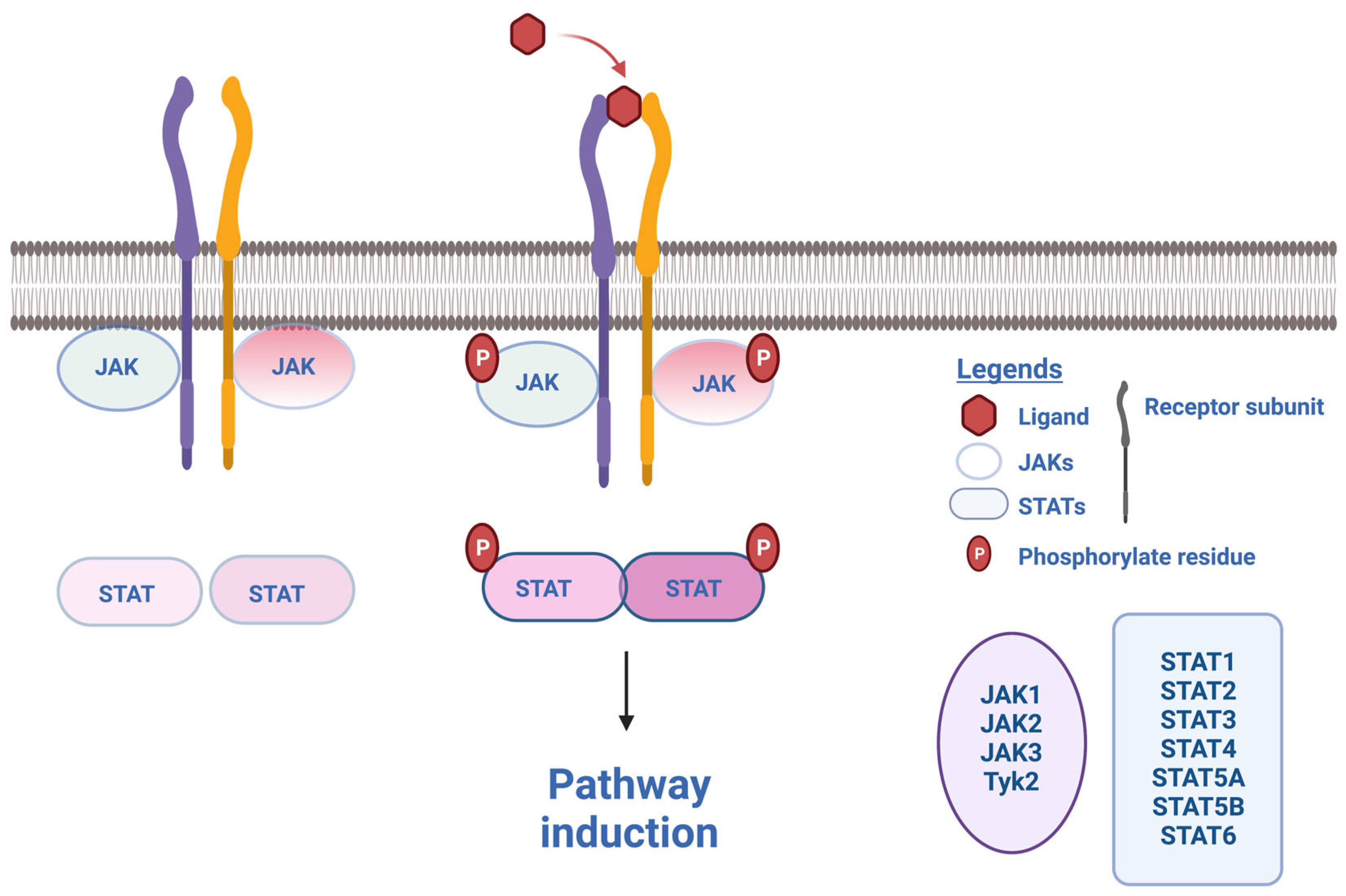
2. What Are JAK Inhibitors?
3. JAK Inhibition in Adult Arthritis and Beyond
4. JAK Inhibition in Oligoarticular, Polyarticular, Enthesitis-Related and Systemic JIA
5. JAK Inhibition in Uveitis, Alopecia Areata, Lung Disease and MAS Associated with JIA
6. JAK Inhibition in Mendelian Conditions Mimicking JIA
6.1. JAK Inhibition in Type I Interferonopathies
6.2. JAK Inhibition in JIA Associated with LACC1 Deficiency
7. Safety
7.1. Infections
7.2. Cytopenia
7.3. Thombo-Embolic Events
7.4. Metabolic Events
7.5. Neoplasic Risk
7.6. Others
7.7. Drug Interactions
7.8. Withdrawal Syndrome
7.9. Long-Term Considerations
8. Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Paper (First Author) | Drug | JIA Subtype | Associated Complications | Number of Patients | Associated Drugs | Efficacy |
|---|---|---|---|---|---|---|
| Zhang [31] | Tofacitinib 2.5 mg BID | sJIA | - | 1 | Tocilizumab | Yes |
| Gillard [32] | sJIA | - | 2 | - | Yes | |
| Pin [33] | Tofacitinib 5 mg BID | pJIA | - | 1 | Methotrexate | Yes |
| Rahman [34] | Tofacitinib | Refractory JIA (37% ERA, pJIA RF+, sJIA) | 27 | Yes | ||
| Vukić [35] | Tofacitinib | pJIA | - | 1 | Yes | |
| Huang [36] | Tofacitinib 2.5 mg BID | sJIA | 1 | Yes | ||
| Tseng [37] | Tofacitinib 5 mg BID | pJIA | Microscopic colitis (at 58 years old) | 1 | Yes | |
| Kostik [38] | Tofacitinib 0.15–0.5 mg/kg/day | Moderate to severe JIA (9 pJIA 1 oJIA + alopecia 1 ERA 4 sJIA) | Alopecia areata (1/15) | 15 | CR: 7/15 2 NR (1 pJIA/1 sJIA) | |
| Maccora [39] | Baricitinib 4 mg/day | pJIA | 4 | Yes | ||
| Bader-Meunier [40] | Ruxolitinib 1 mg/kg/day | sJIA | ILD | 1 | Yes | |
| Macaraeg [41] | Ruxolitinib | sJIA | MAS in adulthood after EBV exposition | 1 | Yes |
References
- Prakken, B.; Albani, S.; Martini, A. Juvenile idiopathic arthritis. Lancet 2011, 377, 2138–2149. [Google Scholar] [CrossRef] [PubMed]
- Verweyen, E.L.; Schulert, G.S. Interfering with interferons: Targeting the JAK-STAT pathway in complications of systemic juvenile idiopathic arthritis (SJIA). Rheumatology 2022, 61, 926–935. [Google Scholar] [CrossRef] [PubMed]
- Allantaz, F.; Chaussabel, D.; Stichweh, D.; Bennett, L.; Allman, W.; Mejias, A.; Ardura, M.; Chung, W.; Smith, E.; Wise, C.; et al. Blood leukocyte microarrays to diagnose systemic onset juvenile idiopathic arthritis and follow the response to IL-1 blockade. J. Exp. Med. 2007, 204, 2131–2144. [Google Scholar] [CrossRef] [PubMed]
- Cepika, A.-M.; Banchereau, R.; Segura, E.; Ohouo, M.; Cantarel, B.; Goller, K.; Cantrell, V.; Ruchaud, E.; Gatewood, E.; Nguyen, P.; et al. A multidimensional blood stimulation assay reveals immune alterations underlying systemic juvenile idiopathic arthritis. J. Exp. Med. 2017, 214, 3449–3466. [Google Scholar] [CrossRef] [PubMed]
- Yasin, S.; Schulert, G.S. Systemic juvenile idiopathic arthritis and macrophage activation syndrome: Update on pathogenesis and treatment. Curr. Opin. Rheumatol. 2018, 30, 514–520. [Google Scholar] [CrossRef]
- Lovell, D.J.; Giannini, E.H.; Reiff, A.; Cawkwell, G.D.; Silverman, E.D.; Nocton, J.J.; Stein, L.D.; Gedalia, A.; Ilowite, N.T.; Wallace, C.A.; et al. Etanercept in children with polyarticular juvenile rheumatoid arthritis. Pediatric Rheumatology Collaborative Study Group. N. Engl. J. Med. 2000, 342, 763–769. [Google Scholar] [CrossRef]
- Cimaz, R.; Maioli, G.; Calabrese, G. Current and emerging biologics for the treatment of juvenile idiopathic arthritis. Expert Opin. Biol. Ther. 2020, 20, 725–740. [Google Scholar] [CrossRef]
- Martini, A.; Lovell, D.J.; Albani, S.; Brunner, H.I.; Hyrich, K.L.; Thompson, S.D.; Ruperto, N. Juvenile idiopathic arthritis. Nat. Rev. Dis. Primers 2022, 8, 5. [Google Scholar] [CrossRef]
- Luo, Y.; Alexander, M.; Gadina, M.; O’Shea, J.J.; Meylan, F.; Schwartz, D.M. JAK-STAT signaling in human disease: From genetic syndromes to clinical inhibition. J. Allergy Clin. Immunol. 2021, 148, 911–925. [Google Scholar] [CrossRef]
- Kerrigan, S.A.; McInnes, I.B. JAK inhibitors in rheumatology: Implications for paediatric syndromes? Curr. Rheumatol. Rep. 2018, 20, 83. [Google Scholar] [CrossRef]
- Gadina, M.; Le, M.T.; Schwartz, D.M.; Silvennoinen, O.; Nakayamada, S.; Yamaoka, K.; O’Shea, J.J. Janus kinases to jakinibs: From basic insights to clinical practice. Rheumatology 2019, 58, i4–i16. [Google Scholar] [CrossRef]
- Tanaka, Y.; Luo, Y.; O’Shea, J.J.; Nakayamada, S. Janus kinase-targeting therapies in rheumatology: A mechanisms-based approach. Nat. Rev. Rheumatol. 2022, 18, 133–145. [Google Scholar] [CrossRef]
- Crow, Y.J.; Neven, B.; Frémond, M.-L. JAK inhibition in the type I interferonopathies. J. Allergy Clin. Immunol. 2021, 148, 991–993. [Google Scholar] [CrossRef]
- O’Shea, J.J.; Holland, S.M.; Staudt, L.M. JAKs and STATs in immunity, immunodeficiency, and cancer. N. Engl. J. Med. 2013, 368, 161–170. [Google Scholar] [CrossRef]
- Papp, K.A.; Menter, M.A.; Raman, M.; Disch, D.; Schlichting, D.E.; Gaich, C.; Macias, W.; Zhang, X.; Janes, J.M. A randomized phase 2b trial of baricitinib, an oral Janus kinase (JAK) 1/JAK2 inhibitor, in patients with moderate-to-severe psoriasis. Br. J. Dermatol. 2016, 174, 1266–1276. [Google Scholar] [CrossRef]
- Taylor, P.C.; Keystone, E.C.; van der Heijde, D.; Weinblatt, M.E.; Del Carmen Morales, L.; Reyes Gonzaga, J.; Yakushin, S.; Ishii, T.; Emoto, K.; Beattie, S.; et al. Baricitinib versus Placebo or Adalimumab in Rheumatoid Arthritis. N. Engl. J. Med. 2017, 376, 652–662. [Google Scholar] [CrossRef]
- Smolen, J.S.; Xie, L.; Jia, B.; Taylor, P.C.; Burmester, G.; Tanaka, Y.; Elias, A.; Cardoso, A.; Ortmann, R.; Walls, C.; et al. Efficacy of baricitinib in patients with moderate-to-severe rheumatoid arthritis with 3 years of treatment: Results from a long-term study. Rheumatology 2021, 60, 2256–2266. [Google Scholar] [CrossRef]
- Kubo, S.; Yamaoka, K.; Kondo, M.; Yamagata, K.; Zhao, J.; Iwata, S.; Tanaka, Y. The JAK inhibitor, tofacitinib, reduces the T cell stimulatory capacity of human monocyte-derived dendritic cells. Ann. Rheum. Dis. 2014, 73, 2192–2198. [Google Scholar] [CrossRef]
- Kubo, S.; Nakayamada, S.; Sakata, K.; Kitanaga, Y.; Ma, X.; Lee, S.; Ishii, A.; Yamagata, K.; Nakano, K.; Tanaka, Y. Janus kinase inhibitor baricitinib modulates human innate and adaptive immune system. Front. Immunol. 2018, 9, 1510. [Google Scholar] [CrossRef]
- Traves, P.G.; Murray, B.; Campigotto, F.; Galien, R.; Meng, A.; Di Paolo, J.A. JAK selectivity and the implications for clinical inhibition of pharmacodynamic cytokine signalling by filgotinib, upadacitinib, tofacitinib and baricitinib. Ann. Rheum. Dis. 2021, 80, 865–875. [Google Scholar] [CrossRef]
- Tanaka, Y.; Kavanaugh, A.; Wicklund, J.; McInnes, I.B. Filgotinib, a novel JAK1-preferential inhibitor for the treatment of rheumatoid arthritis: An overview from clinical trials. Mod. Rheumatol. 2022, 32, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, R.; Pangan, A.L.; Song, I.-H.; Mysler, E.; Bessette, L.; Peterfy, C.; Durez, P.; Ostor, A.J.; Li, Y.; Zhou, Y.; et al. Upadacitinib Versus Placebo or Adalimumab in Patients with Rheumatoid Arthritis and an Inadequate Response to Methotrexate: Results of a Phase III, Double-Blind, Randomized Controlled Trial. Arthritis Rheumatol. 2019, 71, 1788–1800. [Google Scholar] [CrossRef] [PubMed]
- Rubbert-Roth, A.; Enejosa, J.; Pangan, A.L.; Haraoui, B.; Rischmueller, M.; Khan, N.; Zhang, Y.; Martin, N.; Xavier, R.M. Trial of upadacitinib or abatacept in rheumatoid arthritis. N. Engl. J. Med. 2020, 383, 1511–1521. [Google Scholar] [CrossRef]
- Combe, B.; Kivitz, A.; Tanaka, Y.; van der Heijde, D.; Simon, J.A.; Baraf, H.S.B.; Kumar, U.; Matzkies, F.; Bartok, B.; Ye, L.; et al. Filgotinib versus placebo or adalimumab in patients with rheumatoid arthritis and inadequate response to methotrexate: A phase III randomised clinical trial. Ann. Rheum. Dis. 2021, 80, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Van der Heijde, D.; Song, I.-H.; Pangan, A.L.; Deodhar, A.; van den Bosch, F.; Maksymowych, W.P.; Kim, T.-H.; Kishimoto, M.; Everding, A.; Sui, Y.; et al. Efficacy and safety of upadacitinib in patients with active ankylosing spondylitis (SELECT-AXIS 1): A multicentre, randomised, double-blind, placebo-controlled, phase 2/3 trial. Lancet 2019, 394, 2108–2117. [Google Scholar] [CrossRef]
- Deodhar, A.; Sliwinska-Stanczyk, P.; Xu, H.; Baraliakos, X.; Gensler, L.S.; Fleishaker, D.; Wang, L.; Wu, J.; Menon, S.; Wang, C.; et al. Tofacitinib for the treatment of ankylosing spondylitis: A phase III, randomised, double-blind, placebo-controlled study. Ann. Rheum. Dis. 2021, 80, 1004–1013. [Google Scholar] [CrossRef]
- Guttman-Yassky, E.; Thaçi, D.; Pangan, A.L.; Hong, H.C.-H.; Papp, K.A.; Reich, K.; Beck, L.A.; Mohamed, M.-E.F.; Othman, A.A.; Anderson, J.K.; et al. Upadacitinib in adults with moderate to severe atopic dermatitis: 16-week results from a randomized, placebo-controlled trial. J. Allergy Clin. Immunol. 2020, 145, 877–884. [Google Scholar] [CrossRef]
- King, B.; Guttman-Yassky, E.; Peeva, E.; Banerjee, A.; Sinclair, R.; Pavel, A.B.; Zhu, L.; Cox, L.A.; Craiglow, B.; Chen, L.; et al. A phase 2a randomized, placebo-controlled study to evaluate the efficacy and safety of the oral Janus kinase inhibitors ritlecitinib and brepocitinib in alopecia areata: 24-week results. J. Am. Acad. Dermatol. 2021, 85, 379–387. [Google Scholar] [CrossRef]
- Wallace, D.J.; Furie, R.A.; Tanaka, Y.; Kalunian, K.C.; Mosca, M.; Petri, M.A.; Dörner, T.; Cardiel, M.H.; Bruce, I.N.; Gomez, E.; et al. Baricitinib for systemic lupus erythematosus: A double-blind, randomised, placebo-controlled, phase 2 trial. Lancet 2018, 392, 222–231. [Google Scholar] [CrossRef]
- Ladislau, L.; Suárez-Calvet, X.; Toquet, S.; Landon-Cardinal, O.; Amelin, D.; Depp, M.; Rodero, M.P.; Hathazi, D.; Duffy, D.; Bondet, V.; et al. JAK inhibitor improves type I interferon induced damage: Proof of concept in dermatomyositis. Brain 2018, 141, 1609–1621. [Google Scholar] [CrossRef]
- Zhang, Y.; Ru, J.; Zhang, J. Sequential tocilizumab and tofacitinib treatment for systemic juvenile idiopathic arthritis: A case report. Rheumatol. Ther. 2023, 10, 293–300. [Google Scholar] [CrossRef]
- Gillard, L.; Pouchot, J.; Cohen-Aubart, F.; Koné-Paut, I.; Mouterde, G.; Michaud, M.; Reumaux, H.; Savey, L.; Belot, A.; Fautrel, B.; et al. JAK inhibitors in difficult-to-treat adult-onset Still’s disease and systemic-onset juvenile idiopathic arthritis. Rheumatology 2022, 62, 1594–1604. [Google Scholar] [CrossRef]
- Pin, A.; Tesser, A.; Pastore, S.; Moressa, V.; Valencic, E.; Arbo, A.; Maestro, A.; Tommasini, A.; Taddio, A. Biological and Clinical Changes in a Pediatric Series Treated with Off-Label JAK Inhibitors. Int. J. Mol. Sci. 2020, 21, 7767. [Google Scholar] [CrossRef]
- Rahman, M.M.; Laila, K.; Rahman, S.A. Efficacy and safety of tofacitinib in the treatment of refractory cases of polyarticular course juvenile idiopathic arthritis: A study from Bangladesh. Int. J. Rheum. Dis. 2022, 25, 678–684. [Google Scholar] [CrossRef]
- Vukić, V.; Smajo, A.; Vidović, M.; Vukojević, R.; Harjaček, M.; Lamot, L. Beyond the guidelines management of juvenile idiopathic arthritis: A case report of a girl with polyarticular disease refractory to multiple treatment options and Leri Weill syndrome. BMC Pediatr. 2021, 21, 40. [Google Scholar] [CrossRef]
- Huang, Z.; Lee, P.Y.; Yao, X.; Zheng, S.; Li, T. Tofacitinib treatment of refractory systemic juvenile idiopathic arthritis. Pediatrics 2019, 143, e20182845. [Google Scholar] [CrossRef]
- Tseng, B.; Amighi, A.; Bradford, K.; Wang, H.L.; Getzug, T.E.; Brahn, E. Tofacitinib response in juvenile idiopathic arthritis (JIA) and collagenous colitis. J. Clin. Rheumatol. 2016, 22, 446–448. [Google Scholar] [CrossRef]
- Kostik, M.M.; Raupov, R.K.; Suspitsin, E.N.; Isupova, E.A.; Gaidar, E.V.; Gabrusskaya, T.V.; Kaneva, M.A.; Snegireva, L.S.; Likhacheva, T.S.; Miulkidzhan, R.S.; et al. The safety and efficacy of tofacitinib in 24 cases of pediatric rheumatic diseases: Single centre experience. Front. Pediatr. 2022, 10, 820586. [Google Scholar] [CrossRef]
- Maccora, I.; Oliverio, T.; Pagnini, I.; Marrani, E.; Mastrolia, M.V.; Simonini, G. Baricitinib for juvenile idiopathic arthritis: A monocentric case series. Ann. Rheum. Dis. 2023, 82, 994–995. [Google Scholar] [CrossRef]
- Bader-Meunier, B.; Hadchouel, A.; Berteloot, L.; Polivka, L.; Béziat, V.; Casanova, J.-L.; Lévy, R. Effectiveness and safety of ruxolitinib for the treatment of refractory systemic idiopathic juvenile arthritis like associated with interstitial lung disease: A case report. Ann. Rheum. Dis. 2022, 81, e20. [Google Scholar] [CrossRef]
- Macaraeg, M.; Schulert, G.S. Complications of complications: Diagnosis and treatment of recurrent macrophage activation syndrome in a patient with well-controlled systemic juvenile idiopathic arthritis. RMD Open 2023, 9, e002611. [Google Scholar] [CrossRef] [PubMed]
- Ruperto, N.; Brunner, H.I.; Synoverska, O.; Ting, T.V.; Mendoza, C.A.; Spindler, A.; Vyzhga, Y.; Marzan, K.; Grebenkina, L.; Tirosh, I.; et al. Tofacitinib in juvenile idiopathic arthritis: A double-blind, placebo-controlled, withdrawal phase 3 randomised trial. Lancet 2021, 398, 1984–1996. [Google Scholar] [CrossRef] [PubMed]
- Saurenmann, R.K.; Levin, A.V.; Feldman, B.M.; Rose, J.B.; Laxer, R.M.; Schneider, R.; Silverman, E.D. Prevalence, risk factors, and outcome of uveitis in juvenile idiopathic arthritis: A long-term followup study. Arthritis Rheum. 2007, 56, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Constantin, T.; Foeldvari, I.; Anton, J.; de Boer, J.; Czitrom-Guillaume, S.; Edelsten, C.; Gepstein, R.; Heiligenhaus, A.; Pilkington, C.A.; Simonini, G.; et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: The SHARE initiative. Ann. Rheum. Dis. 2018, 77, 1107–1117. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, A.V.; Dick, A.D.; Jones, A.P.; McKay, A.; Williamson, P.R.; Compeyrot-Lacassagne, S.; Hardwick, B.; Hickey, H.; Hughes, D.; Woo, P.; et al. Adalimumab plus Methotrexate for Uveitis in Juvenile Idiopathic Arthritis. N. Engl. J. Med. 2017, 376, 1637–1646. [Google Scholar] [CrossRef]
- Angeles-Han, S.T.; Ringold, S.; Beukelman, T.; Lovell, D.; Cuello, C.A.; Becker, M.L.; Colbert, R.A.; Feldman, B.M.; Holland, G.N.; Ferguson, P.J.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Screening, Monitoring, and Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis. Arthritis Care Res. 2019, 71, 703–716. [Google Scholar] [CrossRef]
- Miserocchi, E.; Giuffrè, C.; Cornalba, M.; Pontikaki, I.; Cimaz, R. JAK inhibitors in refractory juvenile idiopathic arthritis-associated uveitis. Clin. Rheumatol. 2020, 39, 847–851. [Google Scholar] [CrossRef]
- Baquet-Walscheid, K.; Heinz, C.; Rath, T.; Scheel, M.; Heiligenhaus, A. Beneficial Effect of Upadacitinib in an Adult Patient with Juvenile Idiopathic Arthritis-associated Uveitis after Unsatisfactory Response to Tofacitinib: A Case Report. Ocul. Immunol. Inflamm. 2022, 31, 1–2. [Google Scholar] [CrossRef]
- Ramanan, A.V.; Guly, C.M.; Keller, S.Y.; Schlichting, D.E.; de Bono, S.; Liao, R.; Quartier, P. Clinical effectiveness and safety of baricitinib for the treatment of juvenile idiopathic arthritis-associated uveitis or chronic anterior antinuclear antibody-positive uveitis: Study protocol for an open-label, adalimumab active-controlled phase 3 clinical trial (JUVE-BRIGHT). Trials 2021, 22, 689. [Google Scholar]
- Saper, V.E.; Chen, G.; Deutsch, G.H.; Guillerman, R.P.; Birgmeier, J.; Jagadeesh, K.; Canna, S.; Schulert, G.; Deterding, R.; Xu, J.; et al. Emergent high fatality lung disease in systemic juvenile arthritis. Ann. Rheum. Dis. 2019, 78, 1722–1731. [Google Scholar] [CrossRef]
- Saper, V.E.; Ombrello, M.J.; Tremoulet, A.H.; Montero-Martin, G.; Prahalad, S.; Canna, S.; Shimizu, C.; Deutsch, G.; Tan, S.Y.; Remmers, E.F.; et al. Severe delayed hypersensitivity reactions to IL-1 and IL-6 inhibitors link to common HLA-DRB1*15 alleles. Ann. Rheum. Dis. 2022, 81, 406–415. [Google Scholar] [CrossRef]
- Saper, V.E.; Chen, G.; Khatri, P.; Mellins, E.D. Response to: “Effectiveness and safety of ruxolitinib for the treatment of refractory systemic idiopathic juvenile arthritis like associated with interstitial lung disease: Case report” by Bader-Meunier et al. Ann. Rheum. Dis. 2022, 81, e21. [Google Scholar] [CrossRef]
- Rood, J.E.; Rezk, A.; Pogoriler, J.; Finn, L.S.; Burnham, J.M.; Josephson, M.B.; Bar-Or, A.; Behrens, E.M.; Canna, S.W. Improvement of Refractory Systemic Juvenile Idiopathic Arthritis-Associated Lung Disease with Single-Agent Blockade of IL-1β and IL-18. J. Clin. Immunol. 2023, 43, 101–108. [Google Scholar] [CrossRef]
- Rice, G.I.; Melki, I.; Frémond, M.-L.; Briggs, T.A.; Rodero, M.P.; Kitabayashi, N.; Oojageer, A.; Bader-Meunier, B.; Belot, A.; Bodemer, C.; et al. Assessment of type I interferon signaling in pediatric inflammatory disease. J. Clin. Immunol. 2017, 37, 123–132. [Google Scholar] [CrossRef]
- Quartier, P.; Allantaz, F.; Cimaz, R.; Pillet, P.; Messiaen, C.; Bardin, C.; Bossuyt, X.; Boutten, A.; Bienvenu, J.; Duquesne, A.; et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Ann. Rheum. Dis. 2011, 70, 747–754. [Google Scholar] [CrossRef]
- Verweyen, E.; Holzinger, D.; Weinhage, T.; Hinze, C.; Wittkowski, H.; Pickkers, P.; Albeituni, S.; Verbist, K.; Nichols, K.E.; Schulert, G.; et al. Synergistic Signaling of TLR and IFNα/β Facilitates Escape of IL-18 Expression from Endotoxin Tolerance. Am. J. Respir. Crit. Care Med. 2020, 201, 526–539. [Google Scholar] [CrossRef]
- Villacis-Nunez, D.S.; Bilcha, K.; Spraker, M.; Rouster-Stevens, K.; Cooley, A. Severe immediate and delayed hypersensitivity reactions to biologics in a toddler with systemic juvenile idiopathic arthritis. J. Investig. Med. High Impact Case Rep. 2022, 10, 23247096221077836. [Google Scholar] [CrossRef]
- Borden, E.C.; Sen, G.C.; Uze, G.; Silverman, R.H.; Ransohoff, R.M.; Foster, G.R.; Stark, G.R. Interferons at age 50: Past, current and future impact on biomedicine. Nat. Rev. Drug Discov. 2007, 6, 975–990. [Google Scholar] [CrossRef]
- Broggi, A.; Ghosh, S.; Sposito, B.; Spreafico, R.; Balzarini, F.; Lo Cascio, A.; Clementi, N.; De Santis, M.; Mancini, N.; Granucci, F.; et al. Type III interferons disrupt the lung epithelial barrier upon viral recognition. Science 2020, 369, 706–712. [Google Scholar] [CrossRef]
- Crow, Y.J.; Stetson, D.B. The type I interferonopathies: 10 years on. Nat. Rev. Immunol. 2022, 22, 471–483. [Google Scholar] [CrossRef]
- Crow, Y.J. Type I interferonopathies: A novel set of inborn errors of immunity. Ann. N. Y. Acad. Sci. 2011, 1238, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Melki, I.; Frémond, M.-L. Type I Interferonopathies: From a Novel Concept to Targeted Therapeutics. Curr. Rheumatol. Rep. 2020, 22, 32. [Google Scholar] [CrossRef] [PubMed]
- Clarke, S.L.N.; Robertson, L.; Rice, G.I.; Seabra, L.; Hilliard, T.N.; Crow, Y.J.; Ramanan, A.V. Type 1 interferonopathy presenting as juvenile idiopathic arthritis with interstitial lung disease: Report of a new phenotype. Pediatr. Rheumatol. Online J. 2020, 18, 37. [Google Scholar] [CrossRef] [PubMed]
- Frémond, M.-L.; Hadchouel, A.; Berteloot, L.; Melki, I.; Bresson, V.; Barnabei, L.; Jeremiah, N.; Belot, A.; Bondet, V.; Brocq, O.; et al. Overview of STING-Associated Vasculopathy with Onset in Infancy (SAVI) Among 21 Patients. J. Allergy Clin. Immunol. Pract. 2021, 9, 803–818.e11. [Google Scholar] [CrossRef] [PubMed]
- Frémond, M.-L.; Crow, Y.J. STING-Mediated Lung Inflammation and Beyond. J. Clin. Immunol. 2021, 41, 501–514. [Google Scholar] [CrossRef]
- Bader-Meunier, B.; Bustaffa, M.; Iskounen, T.; Carter, E.; Marsh, J.A.; Baujat, G.; Crow, Y.J.; Frémond, M.-L. Rheumatoid factor positive polyarticular juvenile idiopathic arthritis associated with a novel COPA mutation. Rheumatology 2020, 60, e171–e173. [Google Scholar] [CrossRef]
- Rutsch, F.; MacDougall, M.; Lu, C.; Buers, I.; Mamaeva, O.; Nitschke, Y.; Rice, G.I.; Erlandsen, H.; Kehl, H.G.; Thiele, H.; et al. A specific IFIH1 gain-of-function mutation causes Singleton-Merten syndrome. Am. J. Hum. Genet. 2015, 96, 275–282. [Google Scholar] [CrossRef]
- de Carvalho, L.M.; Ngoumou, G.; Park, J.W.; Ehmke, N.; Deigendesch, N.; Kitabayashi, N.; Melki, I.; Souza, F.F.L.; Tzschach, A.; Nogueira-Barbosa, M.H.; et al. Musculoskeletal Disease in MDA5-Related Type I Interferonopathy: A Mendelian Mimic of Jaccoud’s Arthropathy. Arthritis Rheumatol. 2017, 69, 2081–2091. [Google Scholar] [CrossRef]
- Sanchez, G.A.M.; Reinhardt, A.; Ramsey, S.; Wittkowski, H.; Hashkes, P.J.; Berkun, Y.; Schalm, S.; Murias, S.; Dare, J.A.; Brown, D.; et al. JAK1/2 inhibition with baricitinib in the treatment of autoinflammatory interferonopathies. J. Clin. Investig. 2018, 128, 3041–3052. [Google Scholar] [CrossRef]
- Krutzke, S.; Rietschel, C.; Horneff, G. Baricitinib in therapy of COPA syndrome in a 15-year-old girl. Eur. J. Rheumatol. 2019, 7, S78. [Google Scholar] [CrossRef]
- Broser, P.; von Mengershausen, U.; Heldt, K.; Bartholdi, D.; Braun, D.; Wolf, C.; Lee-Kirsch, M.A. Precision treatment of Singleton Merten syndrome with ruxolitinib: A case report. Pediatr. Rheumatol. Online J. 2022, 20, 24. [Google Scholar] [CrossRef]
- Wakil, S.M.; Monies, D.M.; Abouelhoda, M.; Al-Tassan, N.; Al-Dusery, H.; Naim, E.A.; Al-Younes, B.; Shinwari, J.; Al-Mohanna, F.A.; Meyer, B.F.; et al. Association of a mutation in LACC1 with a monogenic form of systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2015, 67, 288–295. [Google Scholar] [CrossRef]
- Al-Mayouf, S.M.; Yateem, M.; Al-Dusery, H.; Monies, D.; Wakil, S.; AlShiakh, M.; AlEnazi, A.; Aladaileh, B.; Alzyoud, R.; Meyer, B. New or vanishing frontiers: LACC1-associated juvenile arthritis. Int. J. Pediatr. Adolesc. Med. 2021, 8, 44–47. [Google Scholar] [CrossRef]
- Omarjee, O.; Mathieu, A.-L.; Quiniou, G.; Moreews, M.; Ainouze, M.; Frachette, C.; Melki, I.; Dumaine, C.; Gerfaud-Valentin, M.; Duquesne, A.; et al. LACC1 deficiency links juvenile arthritis with autophagy and metabolism in macrophages. J. Exp. Med. 2021, 218, e20201006. [Google Scholar] [CrossRef]
- Winthrop, K.L.; Harigai, M.; Genovese, M.C.; Lindsey, S.; Takeuchi, T.; Fleischmann, R.; Bradley, J.D.; Byers, N.L.; Hyslop, D.L.; Issa, M.; et al. Infections in baricitinib clinical trials for patients with active rheumatoid arthritis. Ann. Rheum. Dis. 2020, 79, 1290–1297. [Google Scholar] [CrossRef]
- Bechman, K.; Subesinghe, S.; Norton, S.; Atzeni, F.; Galli, M.; Cope, A.P.; Winthrop, K.L.; Galloway, J.B. A systematic review and meta-analysis of infection risk with small molecule JAK inhibitors in rheumatoid arthritis. Rheumatology 2019, 58, 1755–1766. [Google Scholar] [CrossRef]
- Balanescu, A.-R.; Citera, G.; Pascual-Ramos, V.; Bhatt, D.L.; Connell, C.A.; Gold, D.; Chen, A.-S.; Sawyerr, G.; Shapiro, A.B.; Pope, J.E.; et al. Infections in patients with rheumatoid arthritis receiving tofacitinib versus tumour necrosis factor inhibitors: Results from the open-label, randomised controlled ORAL Surveillance trial. Ann. Rheum. Dis. 2022, 81, 1491–1503. [Google Scholar] [CrossRef]
- Wollenhaupt, J.; Lee, E.-B.; Curtis, J.R.; Silverfield, J.; Terry, K.; Soma, K.; Mojcik, C.; DeMasi, R.; Strengholt, S.; Kwok, K.; et al. Safety and efficacy of tofacitinib for up to 9.5 years in the treatment of rheumatoid arthritis: Final results of a global, open-label, long-term extension study. Arthritis Res. Ther. 2019, 21, 89. [Google Scholar] [CrossRef]
- Ballesta, B.; González, H.; Martín, V.; Ballesta, J.J. Fatal ruxolitinib-related JC virus meningitis. J. Neurovirol. 2017, 23, 783–785. [Google Scholar] [CrossRef]
- Villarino, A.V.; Kanno, Y.; O’Shea, J.J. Mechanisms and consequences of Jak-STAT signaling in the immune system. Nat. Immunol. 2017, 18, 374–384. [Google Scholar] [CrossRef]
- Xie, W.; Huang, Y.; Xiao, S.; Sun, X.; Fan, Y.; Zhang, Z. Impact of Janus kinase inhibitors on risk of cardiovascular events in patients with rheumatoid arthritis: Systematic review and meta-analysis of randomised controlled trials. Ann. Rheum. Dis. 2019, 78, 1048–1054. [Google Scholar] [CrossRef] [PubMed]
- Yates, M.; Mootoo, A.; Adas, M.; Bechman, K.; Rampes, S.; Patel, V.; Qureshi, S.; Cope, A.P.; Norton, S.; Galloway, J.B. Venous Thromboembolism Risk with JAK Inhibitors: A Meta-Analysis. Arthritis Rheumatol. 2021, 73, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Charles-Schoeman, C.; DeMasi, R.; Valdez, H.; Soma, K.; Hwang, L.-J.; Boy, M.G.; Biswas, P.; McInnes, I.B. Risk Factors for Major Adverse Cardiovascular Events in Phase III and Long-Term Extension Studies of Tofacitinib in Patients with Rheumatoid Arthritis. Arthritis Rheumatol. 2019, 71, 1450–1459. [Google Scholar] [CrossRef] [PubMed]
- Mollé, N.; Krichevsky, S.; Kermani, P.; Silver, R.T.; Ritchie, E.; Scandura, J.M. Ruxolitinib can cause weight gain by blocking leptin signaling in the brain via JAK2/STAT3. Blood 2020, 135, 1062–1066. [Google Scholar] [CrossRef]
- Novikova, D.S.; Udachkina, H.V.; Markelova, E.I.; Kirillova, I.G.; Misiyuk, A.S.; Demidova, N.V.; Popkova, T.V. Dynamics of body mass index and visceral adiposity index in patients with rheumatoid arthritis treated with tofacitinib. Rheumatol. Int. 2019, 39, 1181–1189. [Google Scholar] [CrossRef]
- Curtis, J.R.; Yamaoka, K.; Chen, Y.-H.; Bhatt, D.L.; Gunay, L.M.; Sugiyama, N.; Connell, C.A.; Wang, C.; Wu, J.; Menon, S.; et al. Malignancy risk with tofacitinib versus TNF inhibitors in rheumatoid arthritis: Results from the open-label, randomised controlled ORAL Surveillance trial. Ann. Rheum. Dis. 2023, 82, 331–343. [Google Scholar] [CrossRef]
- Shibata, T.; Muto, J.; Hirano, Y.; Takama, H.; Yanagishita, T.; Ohshima, Y.; Banno, S.; Watanabe, D. Palmoplantar pustulosis-like eruption following tofacitinib therapy for juvenile idiopathic arthritis. JAAD Case Rep. 2019, 5, 518–521. [Google Scholar] [CrossRef]
- Veeravalli, V.; Dash, R.P.; Thomas, J.A.; Babu, R.J.; Madgula, L.M.V.; Srinivas, N.R. Critical Assessment of Pharmacokinetic Drug-Drug Interaction Potential of Tofacitinib, Baricitinib and Upadacitinib, the Three Approved Janus Kinase Inhibitors for Rheumatoid Arthritis Treatment. Drug Saf. 2020, 43, 711–725. [Google Scholar] [CrossRef]
- Alim, K.; Bruyère, A.; Lescoat, A.; Jouan, E.; Lecureur, V.; Le Vée, M.; Fardel, O. Interactions of janus kinase inhibitors with drug transporters and consequences for pharmacokinetics and toxicity. Expert Opin. Drug Metab. Toxicol. 2021, 17, 259–271. [Google Scholar] [CrossRef]
- Tefferi, A.; Pardanani, A. Serious adverse events during ruxolitinib treatment discontinuation in patients with myelofibrosis. Mayo Clin. Proc. 2011, 86, 1188–1191. [Google Scholar] [CrossRef]
- Hadjadj, J.; Frémond, M.-L.; Neven, B. Emerging place of JAK inhibitors in the treatment of inborn errors of immunity. Front. Immunol. 2021, 12, 717388. [Google Scholar] [CrossRef]
- Tvorogov, D.; Thomas, D.; Liau, N.P.D.; Dottore, M.; Barry, E.F.; Lathi, M.; Kan, W.L.; Hercus, T.R.; Stomski, F.; Hughes, T.P.; et al. Accumulation of JAK activation loop phosphorylation is linked to type I JAK inhibitor withdrawal syndrome in myelofibrosis. Sci. Adv. 2018, 4, eaat3834. [Google Scholar] [CrossRef]
- Emery, P.; Tanaka, Y.; Cardillo, T.; Schlichting, D.; Rooney, T.; Beattie, S.; Helt, C.; Smolen, J.S. Temporary interruption of baricitinib: Characterization of interruptions and effect on clinical outcomes in patients with rheumatoid arthritis. Arthritis Res. Ther. 2020, 22, 115. [Google Scholar] [CrossRef]
- Adam, S.; Simon, N.; Steffen, U.; Andes, F.T.; Scholtysek, C.; Müller, D.I.H.; Weidner, D.; Andreev, D.; Kleyer, A.; Culemann, S.; et al. JAK inhibition increases bone mass in steady-state conditions and ameliorates pathological bone loss by stimulating osteoblast function. Sci. Transl. Med. 2020, 12, eaay4447. [Google Scholar] [CrossRef]
- Quartier, P. Systemic juvenile idiopathic arthritis/pediatric still’s disease, a syndrome but several clinical forms: Recent therapeutic approaches. J. Clin. Med. 2022, 11, 1357. [Google Scholar] [CrossRef]
- Simonds, M.M.; Sullivan, K.E.; Brescia, A.C. Single-cell analysis reveals heterogeneity of juvenile idiopathic arthritis fibroblast-like synoviocytes with implications for disease subtype. Arthritis Res. Ther. 2022, 24, 225. [Google Scholar] [CrossRef]

| Name | Specificity | Elimination | FDA Approved Indications | EMA Approved Indications |
|---|---|---|---|---|
| Baricitinib | JAK1, JAK2 | Urine excretion | RA, hospitalised adults with COVID-19 | RA |
| Fedratinib | JAK2, FLT3 | Metabolism by cytochrome P450 complex | Intermediate-2 or high-risk primary or secondary (post-polycythemia vera or post-essential thrombocythemia) MF | Myeloproliferative disorders, primary MF |
| Filgotinib | JAK1 | Urine excretion | None | RA |
| Peficitinib | pan-JAK | Metabolism independent of cytochrome P450 complex | None | None |
| Ruxolitinib | JAK1, JAK2 | Metabolism by cytochrome P450 complex | Topical treatment of AD and vitiligo | Topical treatment of vitiligo |
| Tofacitinib | JAK1, JAK3 (JAK2) | Metabolism by cytochrome P450 complex | RA, SPA, PsoA, moderate to severe UC, pJIA | RA |
| Upadacitinib | JAK1 | Metabolism by cytochrome P450 complex | RA, SPA, PsoA, moderate to severe UC and CD, AD | RA |
| Drug | Study (Phase) | Dose | Study Time | Population | N | Age Criteria | Primary Outcome | Main Conclusion |
|---|---|---|---|---|---|---|---|---|
| Tofacitinib (Xeljanz®) | A3921104, NCT02592434 (Phase 3) | 2–5 mg BID | 44 | ERA, pJIA, PsoJIA | 225 | 2–17 years | Disease flare | Effective |
| Baricitinib (Olumiant®) | JUVE-BASIS, NCT03773978 (Phase 3) | 4 mg (9–18 years) 2 mg (<9 years) | 44 | pJIA, extended oJIA, ERA, PsoJIA | 220 | 2–18 years | Disease flare | Effective |
| Drug | Study | Sponsor | Population | Region | Study Duration | Primary Outcome |
|---|---|---|---|---|---|---|
| Baricitinib (Olumiant®) | JUVE-BALM, NCT04088396 | Eli Lilly | sJIA 1–18 years | Global | 2/2020–4/2023 | Phase 3 Disease flare |
| Baricitinib (Olumiant®) | JUVE-X, NCT03773965 | Eli Lilly | JIA (pJIA, oJIA, PsoJIA, ERA, sJIA) 1–18 years | Global | 4/2019–12/2030 | Phase 3 Long term safety |
| Baricitinib (Olumiant®) vs. Adalimumab | JUVE-BRIGHT, NCT04088409 | Eli Lilly | JIA uveitis, chronic anterior ANA+ uveitis | Europe | 9/2019–6/2022 | Phase 3 Clinical response and safety |
| Tofacitinib (Xeljanz®) | A3921165, NCT03000439 | Pfizer | sJIA | Global | 2/2018–8/2023 | Phase 3 Disease flare |
| Tofacitinib (Xeljanz®) | NCT01500551 | Pfizer | JIA 2–18 years | Global | 3/2013–11/2025 | Phase 3 Long term safety |
| Tofacitinib (Xeljanz®) | NCT05754710 | Pfizer | pJIA and PsoJIA 2–18 years | Korea | 8/2023–1/2027 | Phase 3 Long term safety |
| Upadacitinib (Rinvoq®) | ABT494, NCT03725007 | AbbVie | pJIA 2–18 years | Global | 6/2019–8/2027 | Phase 1 PK, safety, tolerability |
| Upadacitinib (Rinvoq®) vs. Tocilizumab | NCT05609630 | AbbVie | sJIA 1–18years | Global | 3/2023–12/2028 | Phase 3 Clinical response |
| Body Weight (BW) | Dosage |
|---|---|
| 10 kg ≤ BW < 20 kg | 3.2 mg (3.2 mL oral solution) twice daily |
| 20 kg ≤ BW < 40 kg | 4 mg (4 mL oral solution) twice daily |
| BW ≥ 40 kg | 5 mg (one 5 mg tablet or 5 mL oral solution) twice daily |
| What to think of before prescribing JAKi | ||
| Infectious contraindication | Carry out a complete clinical examination and the following investigations before the introduction of these treatments to eliminate:
In patients who have not had chickenpox before JAKi initiation, anti-VZV vaccination can be discussed if it is not contraindicated (e.g., live attenuated vaccine is contraindicated in the event of immunosuppressive treatment). Treatment with JAKi will then only be started one month later. | |
| Thrombo-embolic risk | This should be looked for using, for example, antiphospholipid test. Dyslipidaemia: complete lipid profile. | |
| Treatment association | Pay specific attention to associated treatments, especially treatments with cytochrome p450 inhibitors (except filgotinib and baricitinib, see Table 1). | |
| Kidney function | Adapt dosage of medication to kidney function (filgotinib and baricitinib). | |
| What to monitor after prescribing JAKi | ||
| Type | Investigation(s)/Management | Frequency |
| Infectious monitoring | VZV
|
Each visit. |
| Growth and weight gain | Clinical follow-up: height and weight. | Each visit: Before initiation of JAKi, at the start of treatment, and then regularly (initially monthly for the first 3 months, then every 3–6 months). |
| Haematology follow-up | Laboratory monitoring: red and white blood count. | Before initiation of JAKi, at the start of treatment, and then regularly (initially monthly for the first 3 months, then every 3–6 months). |
| Liver follow-up | Laboratory monitoring: liver enzymes. | |
| Lipid profile follow-up | Laboratory monitoring: lipid profile. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melki, I.; Frémond, M.-L. JAK Inhibition in Juvenile Idiopathic Arthritis (JIA): Better Understanding of a Promising Therapy for Refractory Cases. J. Clin. Med. 2023, 12, 4695. https://doi.org/10.3390/jcm12144695
Melki I, Frémond M-L. JAK Inhibition in Juvenile Idiopathic Arthritis (JIA): Better Understanding of a Promising Therapy for Refractory Cases. Journal of Clinical Medicine. 2023; 12(14):4695. https://doi.org/10.3390/jcm12144695
Chicago/Turabian StyleMelki, Isabelle, and Marie-Louise Frémond. 2023. "JAK Inhibition in Juvenile Idiopathic Arthritis (JIA): Better Understanding of a Promising Therapy for Refractory Cases" Journal of Clinical Medicine 12, no. 14: 4695. https://doi.org/10.3390/jcm12144695
APA StyleMelki, I., & Frémond, M.-L. (2023). JAK Inhibition in Juvenile Idiopathic Arthritis (JIA): Better Understanding of a Promising Therapy for Refractory Cases. Journal of Clinical Medicine, 12(14), 4695. https://doi.org/10.3390/jcm12144695






