Translational and Rotational Postural Aberrations Are Related to Pulmonary Functions and Skill-Related Physical Fitness Components in Collegiate Athletes
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcome Measures
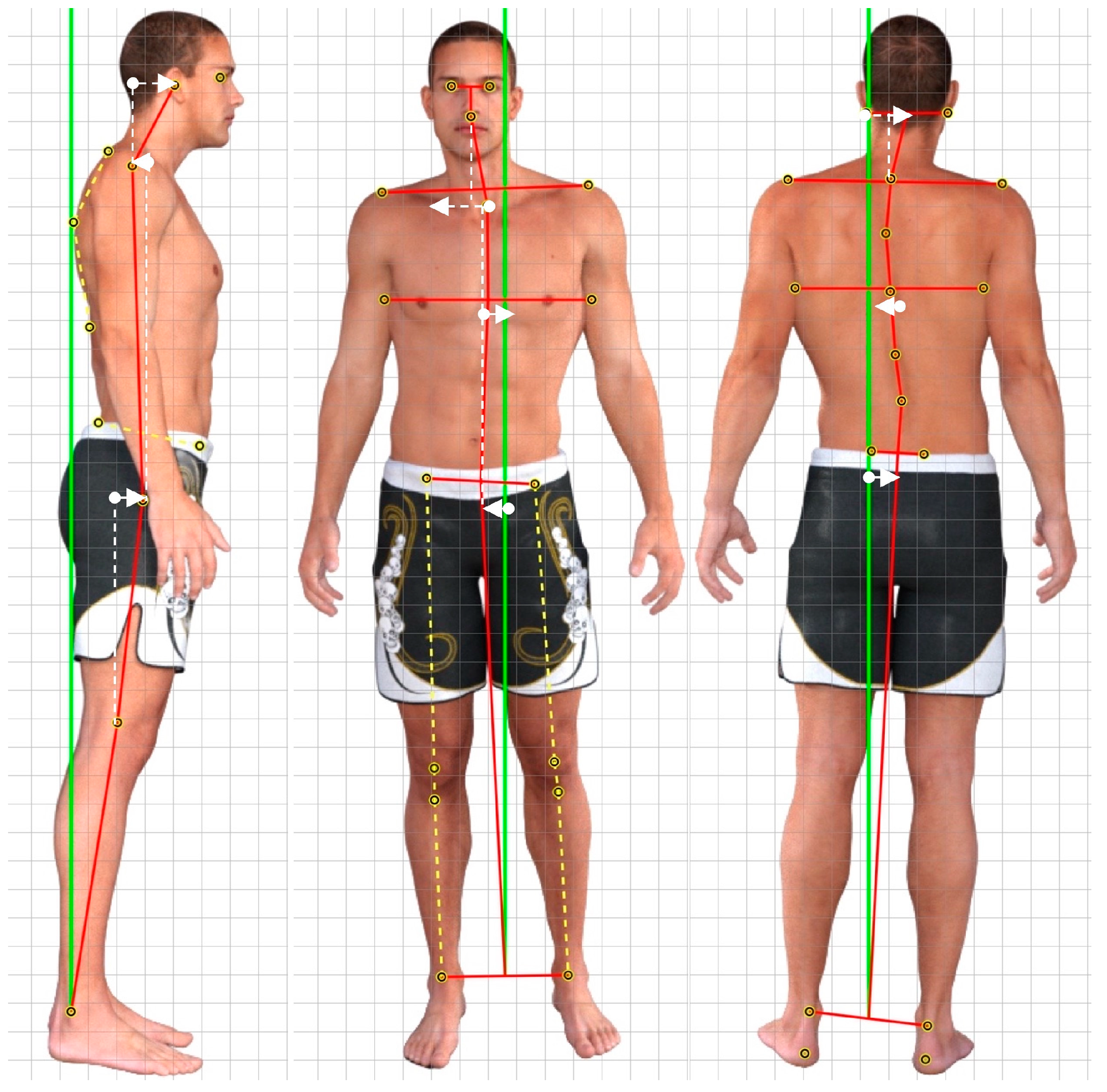
2.1.1. Posture Measurement
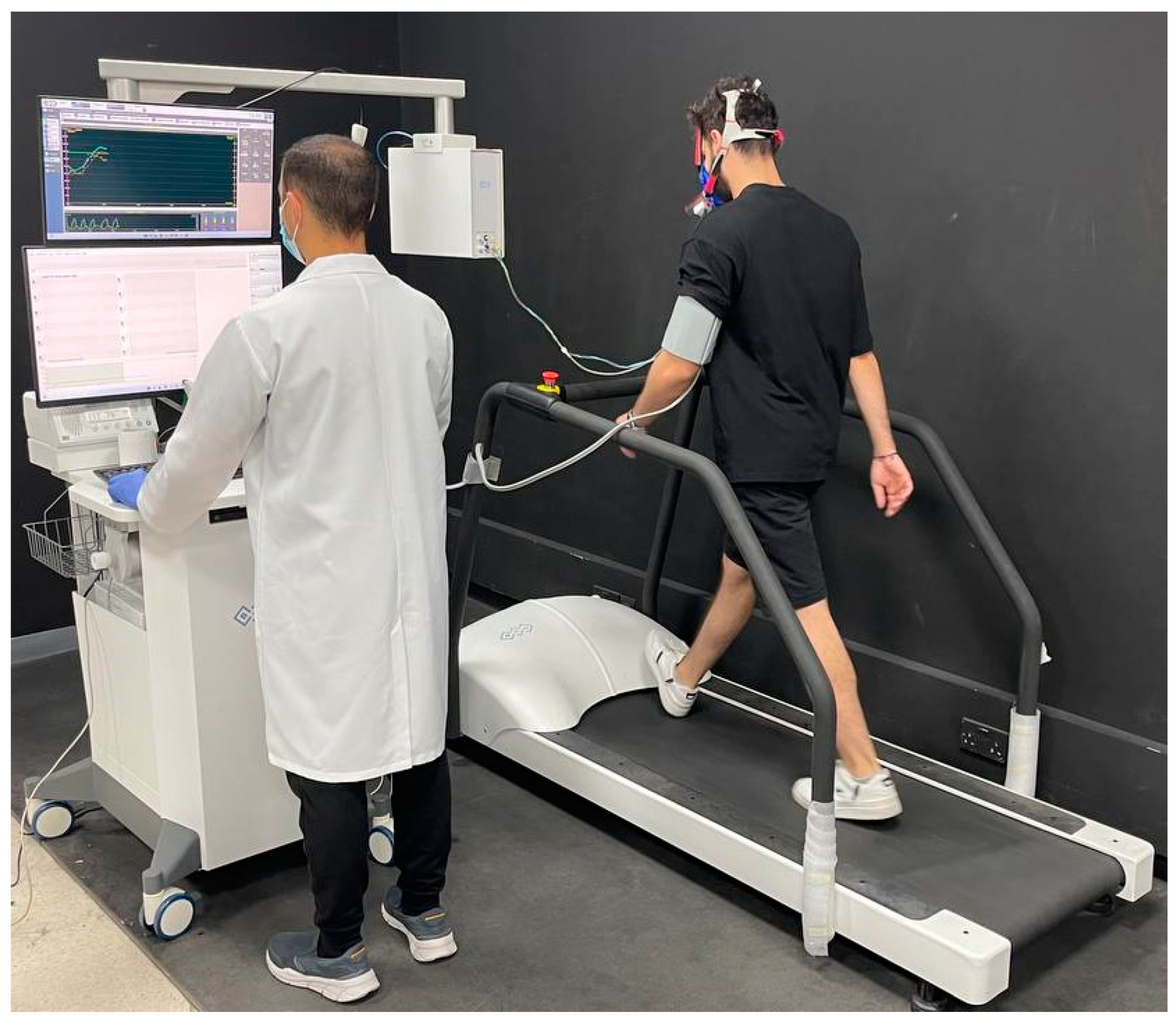
2.1.2. Cardiopulmonary Exercise Testing (CPET)
2.1.3. Athletic Performances
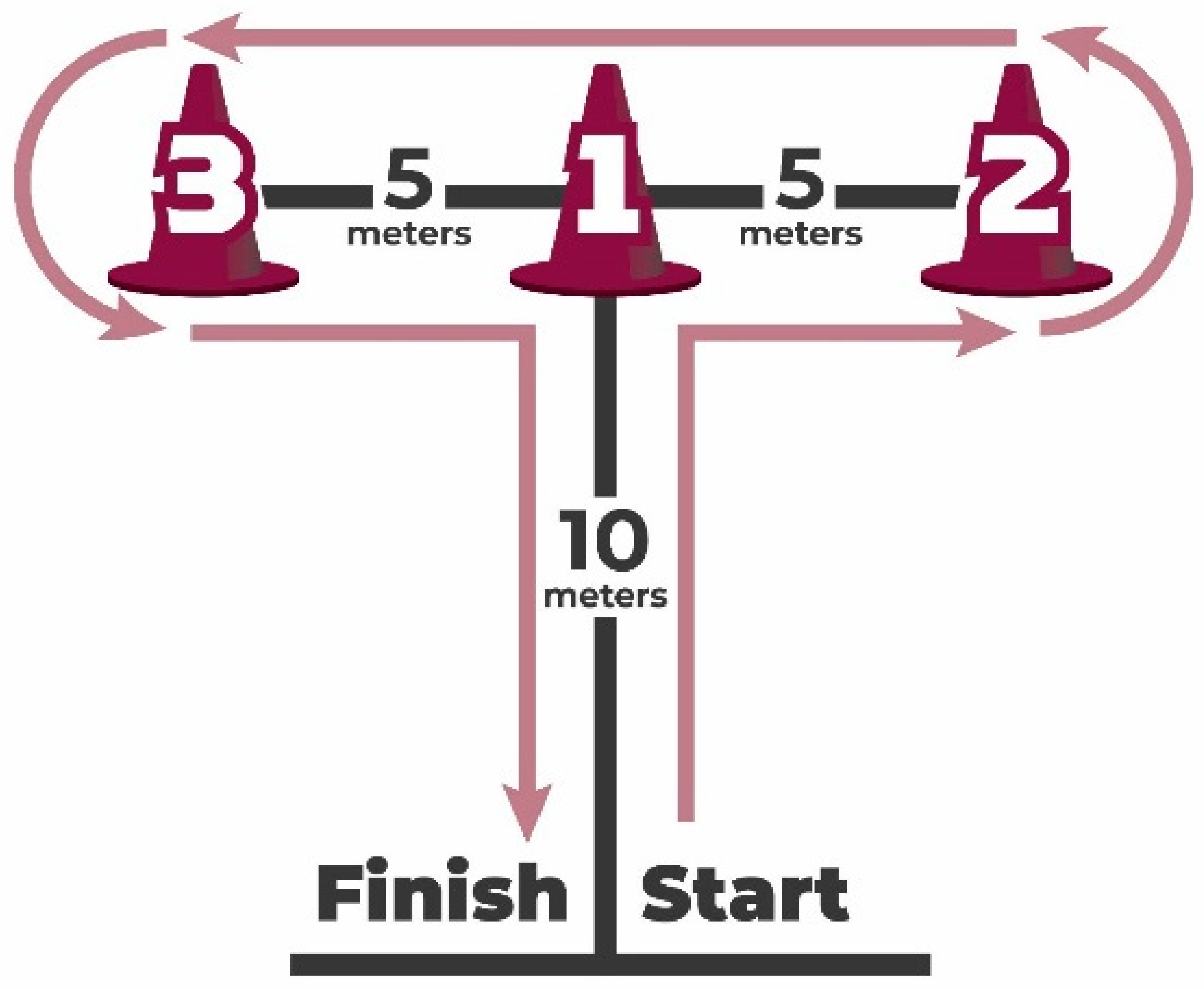
Agility: T-Test
Leg Power: Non-Countermovement Vertical Jump Test
Dynamic Balance: Y-Balance Test or YBT
2.2. Data Analysis
2.2.1. Sample Size Determination
2.2.2. Statistical Analysis
3. Results
3.1. Participant Demographics and Characteristics
3.2. Correlations between Variables
3.2.1. Correlations between Posture and Performance Skills
3.2.2. Correlations between Posture Parameters and Cardiopulmonary Measures
4. Discussion
4.1. Posture and Athletic Skill Measures
4.2. Posture and Cardiopulmonary Exercise Tests
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barley, O.R.; Chapman, D.W.; Guppy, S.N.; Abbiss, C.R. Considerations when assessing endurance in combat sport athletes. Front. Physiol. 2019, 10, 205. [Google Scholar] [CrossRef]
- Suchomel, T.J.; Nimphius, S.; Stone, M.H. The importance of muscular strength in athletic performance. Sports Med. 2016, 46, 1419–1449. [Google Scholar] [CrossRef]
- Pichardo, A.W.; Oliver, J.L.; Harrison, C.B.; Maulder, P.S.; Lloyd, R.S.; Kandoi, R. The influence of maturity offset, strength, and movement competency on motor skill performance in adolescent males. Sports 2019, 7, 168. [Google Scholar] [CrossRef]
- Zemková, E.; Zapletalová, L. The role of neuromuscular control of postural and core stability in functional movement and athlete performance. Front. Physiol. 2022, 13, 56. [Google Scholar] [CrossRef]
- Andreeva, A.; Melnikov, A.; Skvortsov, D.; Akhmerova, K.; Vavaev, A.; Golov, A.; Draugelite, V.; Nikolaev, R.; Chechelnickaia, S.; Zhuk, D.; et al. Postural stability in athletes: The role of sport direction. Gait Posture 2021, 89, 120–125. [Google Scholar] [CrossRef]
- Barczyk-Pawelec, K.; Rubajczyk, K.; Stefańska, M.; Pawik, Ł.; Dziubek, W. Characteristics of body posture in the sagittal plane in 8–13-year-old male athletes practicing soccer. Symmetry 2022, 14, 210. [Google Scholar] [CrossRef]
- Ginés-Díaz, A.; Martínez-Romero, M.T.; Cejudo, A.; Aparicio-Sarmiento, A.; de Baranda, P.S. Sagittal spinal morphotype assessment in dressage and show jumping riders. J. Sport Rehabil. 2019, 29, 533–540. [Google Scholar] [CrossRef]
- Cejudo, A.; Centenera-Centenera, J.M.; Santonja-Medina, F. The potential role of hamstring extensibility on sagittal pelvic tilt, sagittal spinal curves and recurrent low back pain in team sports players: A gender perspective analysis. Int. J. Environ. Res. Public Health 2021, 18, 8654. [Google Scholar] [CrossRef]
- Jackson, L.R.; Purvis, J.; Brown, T. The effects of postural and anatomical alignment on speed, power, and athletic performance in male collegiate athletes: A randomized controlled trial. Int. J. Sports Phys. Ther. 2019, 14, 623–636. [Google Scholar] [CrossRef]
- Kim, M.S.; Cha, Y.J.; Choi, J.D. Correlation between forward head posture, respiratory functions, and respiratory accessory muscles in young adults. J. Back Musculoskelet. Rehabil. 2017, 30, 711–715. [Google Scholar] [CrossRef]
- Koseki, T.; Kakizaki, F.; Hayashi, S.; Nishida, N.; Itoh, M. Effect of forward head posture on thoracic shape and respiratory. J. Phys. Ther. Sci. 2019, 31, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Koźlenia, D.; Kochan-Jacheć, K.; Domaradzki, J. The role of spine curvatures in the sagittal plane in physical performance among team sports players. J. Sports Med. Phys. Fitness 2023, 9. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.; Kim, M.; Harrison, D.E. Comparison of sensorimotor integration and skill-related physical fitness components between college athletes with and without forward head posture. J. Sport Rehabil. 2022, 32, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Ferenczi, A.; Moraux, A.; Le Gall, F.; Andr´, A.; Thevenon, A.; Erie Wieczorek, V. Relationship between spinal-pelvic sagittal balance and pelvic-femoral injuries in professional soccer players. Orthop. J. Sports Med. 2020, 8, 2325967119894962. [Google Scholar] [CrossRef] [PubMed]
- Dreimann, M.; Hoffmann, M.; Kossow, K.; Hitzl, W.; Meier, O.; Koller, H. Scoliosis and chest cage deformity measures predicting impairments in pulmonary function: A cross-sectional study of 492 patients with scoliosis to improve the early identification of patients at risk. Spine 2014, 39, 2024–2033. [Google Scholar] [CrossRef]
- Barassi, G.; Bellomo, R.G.; Di Giulio, C.; Giannuzzo, G.; Irace, G.; Barbato, C.; Saggini, R. Effects of manual somatic stimulation on the autonomic nervous system and posture. Adv. Exp. Med. Biol. 2018, 1070, 97–109. [Google Scholar]
- Harrison, D.D. Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static posture. In Chiropractic Family Practice; Sweere, J.J., Ed.; Aspen Publishers: Gaithersburg, MD, USA, 1992; Chapter 6–1; pp. 1–22. [Google Scholar]
- Harrison, D.D.; Janik, T.J.; Harrison, G.R.; Troyanovich, S.; Harrison, D.E.; Harrison, S.O. Chiropractic biophysics technique: A linear algebra approach to posture in chiropractic. J. Manip. Physiol. Ther. 1996, 19, 525–535. [Google Scholar]
- Harrison, D.E.; Oakley, P.A. An introduction to Chiropractic BioPhysics® (CBP®) technique: A full spine rehabilitation approach to reducing spine deformities. Complement. Ther. 2022, 125. [Google Scholar] [CrossRef]
- Widmer, J.; Cornaz, F.; Scheibler, G.; Spirig, J.M.; Snedeker, J.G.; Farshad, M. Biomechanical contribution of spinal structures to stability of the lumbar spine—Novel biomechanical insights. Spine J. 2020, 20, 1705–1716. [Google Scholar] [CrossRef]
- Liebsch, C.; Wilke, H.J. How does the rib cage affect the biomechanical properties of the thoracic spine? A systematic literature review. Front. Bioeng. Biotechnol. 2022, 10, 904539. [Google Scholar] [CrossRef]
- Striplin, M.R.; Beach, D.J. The prevalence and severity of lumbar spine motion impairment in normal subjects. Clin. Spine Surg. 2012, 25, E115–E116. [Google Scholar] [CrossRef] [PubMed]
- Nachemson, A.L.; Schultz, A.B.; Berkson, M.H. Mechanical properties of human lumbar spine motion segments. Influence of age, sex, disc level, and degeneration. Spine 1979, 4, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lowery, W.D., Jr.; Horn, T.J.; Boden, S.D.; Wiesel, S.W. Impairment evaluation based on spinal range of motion in normal subjects. J. Spinal Disord. 1992, 5, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Szucs, K.A.; Brown, E.V.D. Rater reliability and construct validity of a mobile application for posture analysis. J. Phys. Ther. Sci. 2018, 30, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Boland, D.M.; Neufeld, E.V.; Ruddell, J.; Dolezal, B.A.; Cooper, C.B. Inter- and intra-rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 2016, 28, 3398–3402. [Google Scholar] [CrossRef] [PubMed]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M. Cardiorespiratory fitness in youth: An important marker of health: A scientific statement from the American Heart Association. Circulation 2020, 142, E101–E118. [Google Scholar] [CrossRef]
- Mazaheri, R.; Schmied, C.; Niederseer, D.; Guazzi, M. Cardiopulmonary exercise test parameters in athletic population: A review. J. Clin. Med. 2021, 10, 5073. [Google Scholar] [CrossRef]
- Price, S.; Wiecha, S.; Cieśliński, I.; Śliż, D.; Kasiak, P.S.; Lach, J.; Gruba, G.; Kowalski, T.; Mamcarz, A. Differences between treadmill and cycle ergometer cardiopulmonary exercise testing results in triathletes and their association with body composition and body mass index. Int. J. Environ. Res. Public Health 2022, 19, 3557. [Google Scholar] [CrossRef]
- Decato, T.W.; Bradley, S.M.; Wilson, E.L.; Hegewald, M.J. Repeatability and meaningful change of CPET parameters in healthy subjects. Med. Sci. Sports Exerc. 2018, 50, 589–595. [Google Scholar] [CrossRef]
- Takken, T.; Mylius, C.F.; Paap, D.; Broeders, W.; Hulzebos, H.J.; Van Brussel, M.; Bongers, B.C. Reference values for cardiopulmonary exercise testing in healthy subjects—An updated systematic review. Expert Rev. Cardiovasc. Ther. 2019, 17, 413–426. [Google Scholar] [CrossRef]
- Glaab, T.; Taube, C. Practical guide to cardiopulmonary exercise testing in adults. Respir. Res. 2022, 23, 9. [Google Scholar] [CrossRef]
- Paap, D.; Takken, T. Reference values for cardiopulmonary exercise testing in healthy adults: A systematic review. Expert Rev. Cardiovasc. Ther. 2014, 12, 1439–1453. [Google Scholar] [CrossRef]
- Gibbons, R.J.; Balady, G.J.; Beasley, J.W.; Bricker, J.T.; Duvernoy, W.F.C.; Froelicher, V.F.; Mark, D.B.; Marwick, T.H.; McCallister, B.D.; Thompson, P.D.; et al. Conference. J. Am. Coll. Cardiol. 1997, 30, 260–315. [Google Scholar]
- Pritchard, A.; Burns, P.; Correia, J.; Jamieson, P.; Moxon, P.; Purvis, J.; Thomas, M.; Tighe, H.; Sylvester, K.P. ARTP statement on cardiopulmonary exercise testing 2021. BMJ Open Respir. Res. 2021, 8, e001121. [Google Scholar] [CrossRef]
- Pauole, K.; Madole, K.; Garhammer, J.; Lacourse, M.; Rozenek, R. Reliability and validity of the T-test as a measure of agility, leg power, and leg speed in college-aged men and women. J. Strength Cond. Res. 2000, 14, 443–450. [Google Scholar]
- Van Hooren, B.; Zolotarjova, J. The difference between countermovement and squat jump performances: A review of underlying mechanisms with practical applications. J. Strength Cond. Res. 2017, 31, 2011–2020. [Google Scholar] [CrossRef]
- Negra, Y.; Chaabene, H.; Sammoud, S.; Bouguezzi, R.; Abbes, M.A.; Hachana, Y.; Granacher, U. Effects of plyometric training on physical fitness in prepuberal soccer athletes. Int. J. Sports Med. 2017, 38, 370–377. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Diab, A.A.M.; Harrison, D.E. Does forward head posture influence somatosensory evoked potentials and somatosensory processing in asymptomatic young adults? J. Clin. Med. 2023, 12, 3217. [Google Scholar] [CrossRef]
- Roy, A.L.; Keller, T.S.; Colloca, C.J. Posture-dependent trunk extensor EMG activity during maximum isometrics exertions in normal male and female subjects. J. Electromyogr. Kinesiol. 2003, 13, 469–476. [Google Scholar] [CrossRef]
- Kumar, S.; Narayan, Y. Torque and EMG in rotation extension of the torso from pre-rotated and flexed postures. Clin. Biomech. 2006, 21, 920–931. [Google Scholar] [CrossRef]
- Grabara, M. Comparison of posture among adolescent male volleyball players and non-athletes. Biol. Sport 2015, 32, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Grabara, M. A comparison of the posture between young female handball players and non-training peers. J. Back Musculoskelet. Rehabil. 2014, 27, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Domaradzki, J.; Kochan-Jacheć, K.; Trojanowska, I.; Koźlenia, D. Kickboxers and crossfitters vertebral column curvatures in sagittal plane: Crossfit practice influence in kickboxers body posture. J. Bodyw. Mov. Ther. 2021, 25, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Kruusamäe, H.; Maasalu, K.; Wyon, M.; Jürimäe, T.; Mäestu, J.; Mooses, M.; Jürimäe, J. Spinal posture in different dance sport dance styles compared with track and field athletes. Medicina 2015, 51, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Grabara, M. Anteroposterior curvatures of the spine in adolescent athletes. J. Back Musculoskelet. Rehabil. 2014, 27, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.L.; Sahrmann, S.A. Effect of posture on hip angles and moments during gait. Man. Ther. 2015, 20, 176–182. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Saddiki, R.; Franke, J.; Rigal, J.; Aunoble, S. Equilibrium of the human body and the gravity line: The basics. Eur. Spine J. 2011, 20 (Suppl. S5), 558–563. [Google Scholar] [CrossRef]
- Kapreli, E.; Vourazanis, E.; Billis, E.; Oldham, J.A.; Strimpakos, N. Respiratory dysfunction in chronic neck pain patients. A pilot study. Cephalalgia 2009, 29, 701–710. [Google Scholar] [CrossRef]
- Szczygieł, E.; Węglarz, K.; Piotrowski, K.; Mazur, T.; Mętel, S.; Golec, J. Biomechanical influences on head posture and the respiratory movements of the chest. Acta Bioeng. Biomech. 2015, 17, 143–148. [Google Scholar]


| Variable | FHP (n = 50) |
|---|---|
| Age (years) | 22.2 ± 4 |
| Weight (kg) | 62.5 ± 3 |
| BMI | 18.2 ± 1.5 |
| Gender (%) | |
| Male | 60 |
| Female | 40 |
| Sport a, number in percent (%) | |
| Handball | 20 |
| Volleyball | 15 |
| Basketball | 25 |
| Football | 30 |
| Other | 10 |
| Smoking | |
| Non smoker | 70 |
| Smoker | 30 |
| Race/ethnicity | |
| Asian | 64 |
| African | 36 |
| Posture Parameters | N = 100 Median (IQR) |
|---|---|
| CVA (°) | 52.0 (49.0, 56.5) |
| Lateral translation head sagittal (cm) | 2.00 (1.00, 3.80) |
| AHT coronal (cm) | 0.90 (0.25, 1.07) |
| Lateral angulation head (°) | 11.6 (10.0, 15.8) |
| Thoracic kyphosis (°) | 22.0 (20.0, 30.0) |
| Rib anterior translation coronal (cm) | 0.50 (0.00, 0.70) |
| Pelvic tilt (°) | 9.80 (7.20, 12.00) |
| Pelvis lateral angulation (°) | 2.90 (1.50, 4.90) |
| Pelvis anterior translation coronal (cm) | 0.40 (0.10, 0.70) |
| Hip pelvis lateral translation (cm) | 2.10 (1.00, 2.50) |
| Physical Performance Skills | N = 100 Median (IQR) |
|---|---|
| Static stork test results | 55 (45, 64) |
| Y-balance test (cm) anterior for the left side | 94 (75, 109) |
| Y-balance test (cm) anterior for the right side | 98 (74, 107) |
| Y-balance test (cm) posterolateral for the left side | 100 (86, 112) |
| Y-balance test (cm) posterolateral for the right side | 98 (89, 111) |
| Y-balance test (cm) posteromedial for the left side | 95 (86, 109) |
| Y-balance test (cm) posteromedial for the right side | 99 (82, 110) |
| Vertical jump test (cm) | 48 (39, 55) |
| Agility test (s) | 4.97 (9.60, 11.70) |
| Cardiopulmonary Functions | N = 100 Median (IQR) |
|---|---|
| VE/VCO2 slope | 34.2 (31.4, 39.0) |
| VO2 (mL/min) at VT | 2809 (1788, 3112) |
| VO2/kg | 34 (30, 44) |
| VE I/min (VE/VO2 at VT) | 91 (87, 113) |
| Physical Performance Skills | CVA | Lateral Translation Head Sagittal | AHT Coronal | Lateral Angulation Head | Thoracic Kyphosis | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| Stork balance test (s) | 0.57 | <0.001 | −0.46 | <0.001 | −0.51 | <0.001 | −0.19 | 0.13 | −0.27 | 0.02 |
| Y-balance test (cm) anterior for the left side | 0.33 | <0.001 | −0.35 | 0.004 | −0.44 | <0.001 | −0.22 | 0.075 | −0.28 | 0.025 |
| Y-balance test (cm) anterior for the right side | −0.09 | 0.418 | 0.17 | 0.166 | 0.02 | 0.854 | 0.21 | 0.085 | 0.12 | 0.348 |
| Y-balance test (cm) posterolateral for the left side | 0.39 | 0.001 | −0.42 | <0.001 | −0.48 | <0.001 | −0.31 | 0.013 | −0.28 | 0.024 |
| Y-balance test (cm) posterolateral for the right side | 0.36 | 0.003 | −0.403 | <0.001 | −0.46 | <0.001 | −0.32 | 0.01 | −0.27 | 0.027 |
| Y-balance test (cm) posteromedial for the left side | 0.33 | 0.007 | −0.39 | 0.001 | −0.47 | <0.001 | −0.27 | 0.028 | −0.23 | 0.064 |
| Y-balance test (cm) posteromedial for the right side | 0.29 | 0.016 | −0.29 | 0.015 | −0.39 | 0.001 | −0.19 | 0.13 | −0.19 | 0.12 |
| Vertical jump test (cm) | 0.54 | <0.001 | −0.51 | <0.001 | −0.62 | <0.001 | −0.33 | 0.007 | −0.32 | 0.008 |
| Agility test (s) | −0.86 | <0.001 | 0.786 | <0.001 | 0.81 | <0.001 | 0.74 | <0.001 | 0.695 | <0.001 |
| Physical Performance Skills | Rib Anterior Translation Coronal | Pelvic Tilt | Hip Pelvis Lateral Angulation | Hip Pelvis Anterior Translation Coronal | Hip Pelvis Lateral Translation | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| Stork balance test (s) | −0.41 | <0.001 | −0.35 | 0.02 | −0.44 | <0.001 | −0.47 | <0.001 | −0.5 | <0.001 |
| Y-balance test (cm) anterior for the left side | −0.32 | 0.008 | −0.36 | 0.025 | −0.31 | 0.013 | −0.45 | <0.001 | −0.46 | <0.001 |
| Y-balance test (cm) anterior for the right side | 0.24 | 0.052 | 0.14 | 0.268 | 0.15 | 0.239 | −0.062 | 0.623 | 0.03 | 0.796 |
| Y-balance test (cm) posterolateral for the left side | −0.36 | 0.003 | −0.43 | <0.001 | −0.39 | 0.001 | −0.53 | <0.001 | −0.41 | <0.001 |
| Y-balance test (cm) posterolateral for the right side | −0.33 | 0.006 | −0.42 | <0.001 | −0.39 | 0.001 | −0.46 | <0.001 | −0.43 | <0.001 |
| Y-balance test (cm) posteromedial for the left side | −0.33 | 0.008 | −0.42 | <0.001 | −0.36 | 0.002 | −0.51 | <0.001 | −0.47 | <0.001 |
| Y-balance test (cm) posteromedial for the right side | −0.27 | 0.03 | −0.32 | 0.009 | −0.28 | 0.022 | −0.42 | <0.001 | −0.39 | 0.001 |
| Vertical jump test (cm) | −0.52 | <0.001 | −0.54 | <0.001 | −0.48 | <0.001 | −0.65 | <0.001 | −0.56 | <0.001 |
| Agility test (s) | 0.75 | <0.001 | 0.79 | <0.001 | 0.79 | <0.001 | 0.78 | <0.001 | 0.73 | <0.001 |
| Cardiopulmonary Functions | CVA | Lateral Translation Head Sagittal | AHT Coronal | Lateral Angulation Head | Thoracic Kyphosis | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| VE/VCO2 slope | −0.09 | 0.458 | 0.16 | 0.196 | 0.14 | 0.264 | 0.16 | 0.21 | 0.19 | 0.14 |
| VO2 (mL/min) at VT | 0.65 | <0.001 | −0.62 | <0.001 | −0.69 | <0.001 | −0.48 | <0.001 | −0.39 | <0.001 |
| VO2/kg | 0.71 | <0.001 | −0.72 | <0.001 | −0.73 | <0.001 | −0.63 | <0.001 | −0.52 | <0.001 |
| VE I/min (VE/VO2 at VT) | −0.61 | <0.001 | 0.65 | <0.001 | 0.64 | <0.001 | 0.591 | <0.001 | 0.66 | <0.001 |
| Cardiopulmonary Functions | Rib Anterior Translation Coronal | Pelvic Tilt | Hip-Pelvis Lateral Angulation | Hip Pelvis Anterior Translation Coronal | Hip Pelvis Lateral Translation | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| VE/VCO2 slope | 0.13 | 0.298 | 0.2 | 0.11 | 0.173 | 0.168 | 0.18 | 0.151 | 0.13 | 0.294 |
| VO2 (mL/min) at VT | −0.52 | <0.001 | −0.62 | <0.001 | −0.58 | <0.001 | −0.63 | <0.001 | −0.6 | <0.001 |
| VO2/kg | −0.59 | <0.001 | −0.69 | <0.001 | −0.69 | <0.001 | −0.7 | <0.001 | −0.61 | <0.001 |
| VE I/min (VE/VO2 at VT) | 0.65 | <0.001 | 0.66 | <0.001 | 0.66 | <0.001 | 0.59 | <0.001 | 0.59 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tamim, M.; Moustafa, I.M.; Alaparthi, G.K.; Oakley, P.A.; Harrison, D.E. Translational and Rotational Postural Aberrations Are Related to Pulmonary Functions and Skill-Related Physical Fitness Components in Collegiate Athletes. J. Clin. Med. 2023, 12, 4618. https://doi.org/10.3390/jcm12144618
Tamim M, Moustafa IM, Alaparthi GK, Oakley PA, Harrison DE. Translational and Rotational Postural Aberrations Are Related to Pulmonary Functions and Skill-Related Physical Fitness Components in Collegiate Athletes. Journal of Clinical Medicine. 2023; 12(14):4618. https://doi.org/10.3390/jcm12144618
Chicago/Turabian StyleTamim, May, Ibrahim M. Moustafa, Gopala K. Alaparthi, Paul A. Oakley, and Deed E. Harrison. 2023. "Translational and Rotational Postural Aberrations Are Related to Pulmonary Functions and Skill-Related Physical Fitness Components in Collegiate Athletes" Journal of Clinical Medicine 12, no. 14: 4618. https://doi.org/10.3390/jcm12144618
APA StyleTamim, M., Moustafa, I. M., Alaparthi, G. K., Oakley, P. A., & Harrison, D. E. (2023). Translational and Rotational Postural Aberrations Are Related to Pulmonary Functions and Skill-Related Physical Fitness Components in Collegiate Athletes. Journal of Clinical Medicine, 12(14), 4618. https://doi.org/10.3390/jcm12144618








