Meek Micro-Skin Grafting and Acellular Dermal Matrix in Pediatric Patients: A Novel Approach to Massive Extravasation Injury
Abstract
1. Introduction
2. Case Report
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hackenberg, R.K.; Kabir, K.; Müller, A.; Heydweiller, A.; Burger, C.; Welle, K. Extravasation Injuries of the Limbs in Neonates and Children—Development of a Treatment Algorithm. Dtsch. Arztebl. Int. 2021, 118, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, C.E.; Emmerson, A.J.B. Extravasation injuries on regional neonatal units. Arch. Dis. Child.-Fetal Neonatal Ed. 2004, 89, F274–F2755. [Google Scholar] [CrossRef] [PubMed]
- Falcone, P.A.; Barrall, D.T.; Jeyarajah, D.R.; Grossman, J.A. Nonoperative management of full-thickness intravenous extravasation injuries in premature neonates using enzymatic debridement. Ann. Plast. Surg. 1989, 22, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Maruccia, M.; Ruggieri, M.; Onesti, M.G. Facial skin breakdown in patients with non-invasive ventilation devices: Report of two cases and indications for treatment and prevention. Int. Wound J. 2015, 12, 451–455. [Google Scholar] [CrossRef]
- Kostogloudis, N.; Demiri, E.; Tsimponis, A.; Dionyssiou, D.; Ioannidis, S.; Chatziioannidis, I.; Nikolaidis, N. Severe Extravasation Injuries in Neonates: A Report of 34 Cases. Pediatr. Dermatol. 2015, 32, 830–835. [Google Scholar] [CrossRef]
- Gault, D.T. Extravasation injuries. Br. J. Plast. Surg. 1993, 46, 91–96. [Google Scholar] [CrossRef]
- Hannon, M.G.; Lee, S.K. Extravasation injuries. J. Hand Surg. 2011, 36, 2060–2065. [Google Scholar] [CrossRef]
- Goverman, J.; Kraft, C.T.; Fagan, S.; Levi, B. Back Grafting the Split-Thickness Skin Graft Donor Site. J. Burn. Care Res. 2017, 38, e443–e449. [Google Scholar] [CrossRef]
- Rode, H.; Martinez, R.; Potgieter, D.; Adams, S.; Rogers, A.D. Experience and outcomes of micrografting for major paediatric burns. Burns 2017, 43, 1103–1110. [Google Scholar] [CrossRef]
- Maruccia, M.; Onesti, M.G.; Sorvillo, V.; Albano, A.; Dessy, L.A.; Carlesimo, B.; Tarallo, M.; Marcasciano, M.; Giudice, G.; Cigna, E.; et al. An Alternative Treatment Strategy for Complicated Chronic Wounds: Negative Pressure Therapy over Mesh Skin Graft. BioMed Res. Int. 2017, 2017, 8395219. [Google Scholar] [CrossRef]
- Medina, A.; Riegel, T.; Nystad, D.; Tredget, E.E. Modified Meek Micrografting Technique for Wound Coverage in Extensive Burn Injuries. J. Burn. Care Res. 2016, 37, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Gacto-Sanchez, P. Surgical treatment and management of the severely burn patient: Review and update. Med. Intensiv. 2017, 41, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Rijpma, D.; Claes, K.; Hoeksema, H.; de Decker, I.; Verbelen, J.; Monstrey, S.; Pijpe, A.; van Zuijlen, P.; Vries, A.M.-D. The Meek micrograft technique for burns; review on its outcomes: Searching for the superior skin grafting technique. Burns 2022, 48, 1287–1300. [Google Scholar] [CrossRef]
- Lee, S.Z.; Halim, A.S.; Wan Sulaiman, W.A.; Mat Saad, A.Z. Outcome of the Modified Meek Technique in the Management of Major Pediatric Burns. Ann. Plast. Surg. 2018, 81, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; Allaire, A.; The CARE Group. The CARE guidelines: Consensus-based clinical case reporting guideline development. BMJ Case Rep. 2013, 2013, bcr2013201554. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Łabuś, W.; Słaboń, A.; Ziółkowska, K.; Ochała-Gierek, G.; Kitala, D.; Szyluk, K.; Niemiec, P. Co-Graft of Acellular Dermal Matrix and Split Thickness Skin Graft-A New Reconstructive Surgical Method in the Treatment of Hidradenitis Suppurativa. Bioengineering 2022, 9, 389. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Łabuś, W.; Kitala, D.; Lorek, A.; Ochała-Gierek, G.; Zagórska, K.M.; Waniczek, D.; Szyluk, K.; Niemiec, P. Human Acellular Dermal Matrix in Reconstructive Surgery-A Review. Biomedicines 2022, 10, 2870. [Google Scholar] [CrossRef]
- Cigna, E.; Maruccia, M.; Sorvillo, V.; Parisi, P.; Palumbo, F.; Onesti, M.G. The use of negative pressure therapy and hyaluronic acid for the management of post-traumatic lower limb injury. Int. Wound J. 2012, 10, 534–538. [Google Scholar] [CrossRef]
- Asuku, M.; Yu, T.-C.; Yan, Q.; Böing, E.; Hahn, H.; Hovland, S.; Donelan, M.B. Split-thickness skin graft donor-site morbidity: A systematic literature review. Burns 2021, 47, 1525–1546. [Google Scholar] [CrossRef]
- Kadam, D. Novel expansion techniques for skin grafts. Indian J. Plast. Surg. 2016, 49, 5–15. [Google Scholar] [CrossRef]
- Pope, E.R. Mesh skin grafting. Veter-Clin. N. Am. Small Anim. Pract. 1990, 20, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Dahmardehei, M.; Vaghardoost, R.; Saboury, M.; Zarei, H.; Saboury, S.; Molaei, M.; Seyyedi, J.; Maleknejad, A.; Hospital, I.F. Comparison of Modified Meek Technique with Standard Mesh Method in Patients with Third Degree Burns. World J. Plast. Surg. 2020, 9, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Menon, S.; Li, Z.; Harvey, J.G.; Holland, A.J.A. The use of the Meek technique in conjunction with cultured epithelial autograft in the management of major paediatric burns. Burns 2013, 39, 674–679. [Google Scholar] [CrossRef]
- Noureldin, M.A.; Said, T.A.; Makeen, K.; Kadry, H.M. Comparative study between skin micrografting (Meek technique) and meshed skin grafts in paediatric burns. Burns 2022, 48, 1632–1644. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Kawecki, M.; Mikuś, K.; Klama-Baryła, A.; Nowak, M. Biological dressings as a substitutes of the skin in the treatment of burn wounds. Ann. Surg. 2013, 85, 354–359. [Google Scholar] [CrossRef]
- Chong, S.J.; Choke, A.; Tan, B.K. Technical tips to enhance micrografting results in burn surgery. Burns 2017, 43, 983–986. [Google Scholar] [CrossRef]
- Kreis, R.W.; Mackie, D.P.; Vloemans, A.W.; Hermans, R.P.; Hoekstra, M.J. Widely expanded postage stamp skin grafts using a modified Meek technique in combination with an allograft overlay. Burns 1993, 19, 142–145. [Google Scholar] [CrossRef]
- Nicoletti, G.; Brenta, F.; Bleve, M.; Pellegatta, T.; Malovini, A.; Faga, A.; Perugini, P. Long-term in vivo assessment of bioengineered skin substitutes: A clinical study. J. Tissue Eng. Regen. Med. 2015, 9, 460–468. [Google Scholar] [CrossRef]
- Onesti, M.G.; Fioramonti, P.; Carella, S.; Maruccia, M. The importance of periwound skin in the treatment of “difficult wound”. G Chir. 2011, 32, 83–88. [Google Scholar]





| Diagnosis | Age (Weeks) | Tretment | Range of Motion |
|---|---|---|---|
| Inflamed Meckel diverticulum | 8 | Total parenteral nutrition (TPN) via intravenous access in the right forearm for maintenance purposes (8 weeks) | |
| Extensive Extravasation Injury of soft tissues and skin of the right forearm | 8 | Fasciotomies of both dorsum of the hand and forearm | |
| 8 | Multidisciplinary evaluation in Neonatal Intensive Care Unit (NICU) | ||
| 8 | Increased level of procalcitonin, PCR, D-Dimer, WBC, and body temperature. blood and urinary culture tests, rectal, pharyngeal, and auricular swabs for pathogen identification. Treatment with Amoxicillin and clavulanic acid (8–9 weeks) | ||
| 9 | Surgical debridement and temporary coverage with acellular dermal matrix (Pelnac®) | ||
| Extensive Extravasation Injury with Exposed Tendons and Underlying Tissues | 9 | Culture biopsies confirming enterobacter cloacae complex infection, leading to antibiotic regimen switch to Meropenem | |
| 9–12 | Dressings applied using vaseline gauzes and sterile gauze soaked in chlorhexidine | ||
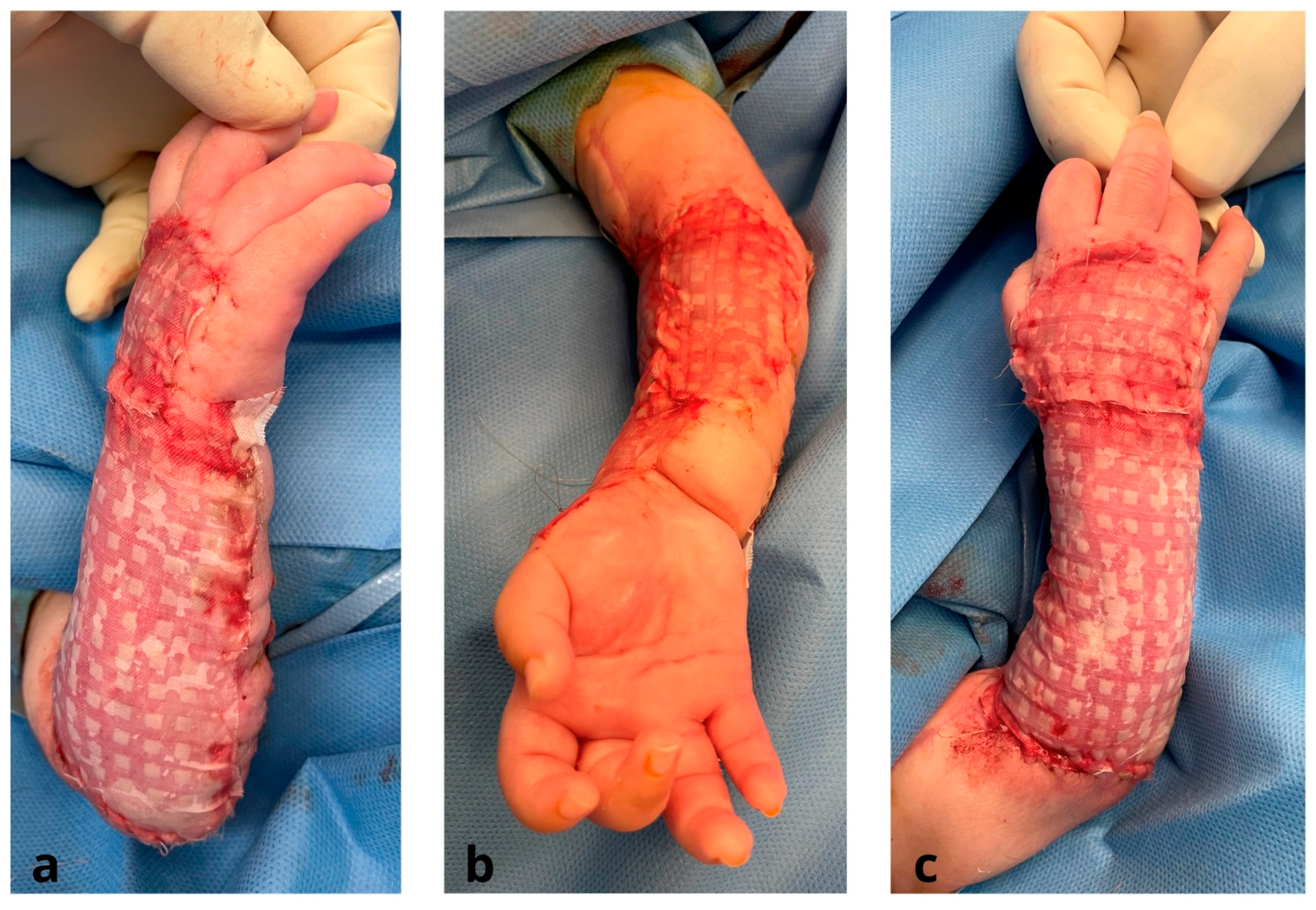
| Appropriate Wound Bed Preparation and Coverage of Exposed Tendons and underlying tissues | 12 | Meek micrografting technique for split-thickness skin graft (STSG) expansion, using the right thigh as the donor site | |
| 13 | Engraftment of Meek micrografts | ||
| 13–15 | Re-epithelialization of each Meek graft occurred from its edges, gradually covering the wound bed. | ||
| Impaired Wrist and Elbow Joints, and Inability to Extend First Finger Impaired Wrist and Elbow Joints, and Inability to Extend First Finger | 15–41 | Follow-up with a comprehensive physical therapy program | Elbow Joint:
|
| 41–67 | Follow-up with a comprehensive physical therapy program | Elbow Joint:
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maruccia, M.; Tedeschi, P.; Corrao, C.; Elia, R.; La Padula, S.; Di Summa, P.G.; Maggio, G.M.M.; Giudice, G. Meek Micro-Skin Grafting and Acellular Dermal Matrix in Pediatric Patients: A Novel Approach to Massive Extravasation Injury. J. Clin. Med. 2023, 12, 4587. https://doi.org/10.3390/jcm12144587
Maruccia M, Tedeschi P, Corrao C, Elia R, La Padula S, Di Summa PG, Maggio GMM, Giudice G. Meek Micro-Skin Grafting and Acellular Dermal Matrix in Pediatric Patients: A Novel Approach to Massive Extravasation Injury. Journal of Clinical Medicine. 2023; 12(14):4587. https://doi.org/10.3390/jcm12144587
Chicago/Turabian StyleMaruccia, Michele, Pasquale Tedeschi, Claudia Corrao, Rossella Elia, Simone La Padula, Pietro G. Di Summa, Giulio M. M. Maggio, and Giuseppe Giudice. 2023. "Meek Micro-Skin Grafting and Acellular Dermal Matrix in Pediatric Patients: A Novel Approach to Massive Extravasation Injury" Journal of Clinical Medicine 12, no. 14: 4587. https://doi.org/10.3390/jcm12144587
APA StyleMaruccia, M., Tedeschi, P., Corrao, C., Elia, R., La Padula, S., Di Summa, P. G., Maggio, G. M. M., & Giudice, G. (2023). Meek Micro-Skin Grafting and Acellular Dermal Matrix in Pediatric Patients: A Novel Approach to Massive Extravasation Injury. Journal of Clinical Medicine, 12(14), 4587. https://doi.org/10.3390/jcm12144587








