Real Life Observational Study of Treatment Success of Monoclonal Antibodies for Refractory Chronic Rhinosinusitis with Nasal Polyps
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Ethical Considerations
2.4. Data Collection
2.5. Primary Outcome Parameters
2.6. Secondary Outcome Parameters
2.7. Statistical Analysis
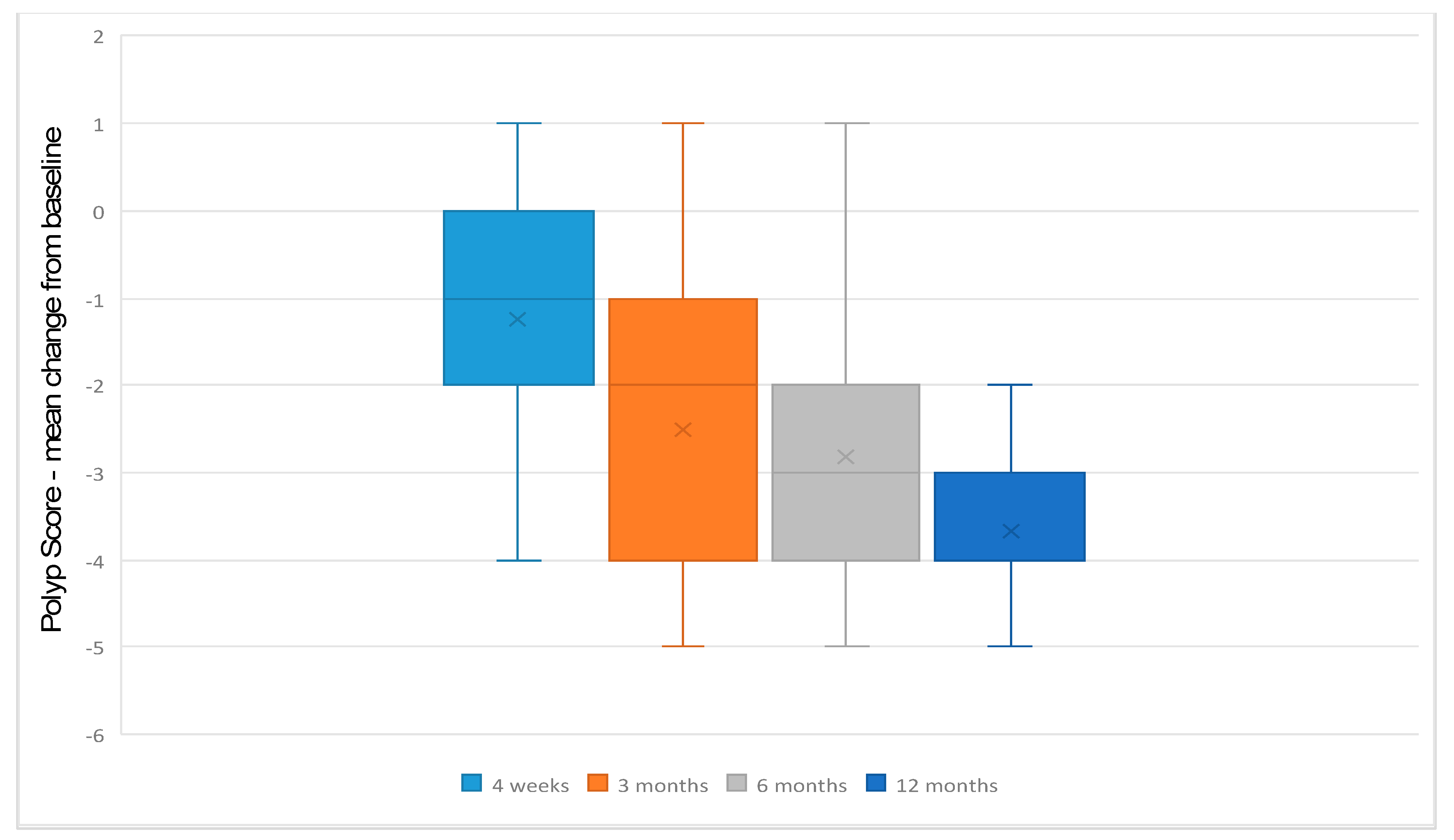
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology 2020, 58, 1–464. [Google Scholar] [CrossRef] [PubMed]
- Larsen, K.; Tos, M. The estimated incidence of symptomatic nasal polyps. Acta Otolaryngol. 2002, 122, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Johansson, L.; Akerlund, A.; Holmberg, K.; Melen, I.; Bende, M. Prevalence of nasal polyps in adults: The Skovde population-based study. Ann. Otol. Rhinol. Laryngol. 2003, 112, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Hedman, J.; Kaprio, J.; Poussa, T.; Nieminen, M.M. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int. J. Epidemiol. 1999, 28, 717–722. [Google Scholar] [CrossRef]
- Stevens, W.W.; Peters, A.T.; Tan, B.K.; Klingler, A.I.; Poposki, J.A.; Hulse, K.E.; Grammer, L.C.; Welch, K.C.; Smith, S.S.; Conley, D.B.; et al. Associations Between Inflammatory Endotypes and Clinical Presentations in Chronic Rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2019, 7, 2812–2820.e3. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, N.; Bo, M.; Holtappels, G.; Zheng, M.; Lou, H.; Wang, H.; Zhang, L.; Bachert, C. Diversity of T(H) cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J. Allergy Clin. Immunol. 2016, 138, 1344–1353. [Google Scholar] [CrossRef]
- Bachert, C.; Marple, B.; Schlosser, R.J.; Hopkins, C.; Schleimer, R.P.; Lambrecht, B.N.; Broker, B.M.; Laidlaw, T.; Song, W.J. Adult chronic rhinosinusitis. Nat. Rev. Dis. Prim. 2020, 6, 86. [Google Scholar] [CrossRef]
- Manti, S.; Parisi, G.F.; Papale, M.; Marseglia, G.L.; Licari, A.; Leonardi, S. Type 2 inflammation in cystic fibrosis: New insights. Pediatr. Allergy Immunol. 2022, 33 (Suppl. 27), 15–17. [Google Scholar] [CrossRef]
- Orlandi, R.R.; Kingdom, T.T.; Smith, T.L.; Bleier, B.; DeConde, A.; Luong, A.U.; Poetker, D.M.; Soler, Z.; Welch, K.C.; Wise, S.K.; et al. International consensus statement on allergy and rhinology: Rhinosinusitis 2021. Int. Forum Allergy Rhinol. 2021, 11, 213–739. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N.; Hellings, P.W.; Bousquet, J. Endotype-driven care pathways in patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 2018, 141, 1543–1551. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef]
- Han, J.K.; Bachert, C.; Fokkens, W.; Desrosiers, M.; Wagenmann, M.; Lee, S.E.; Smith, S.G.; Martin, N.; Mayer, B.; Yancey, S.W.; et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2021, 9, 1141–1153. [Google Scholar] [CrossRef]
- Gevaert, P.; Omachi, T.A.; Corren, J.; Mullol, J.; Han, J.; Lee, S.E.; Kaufman, D.; Ligueros-Saylan, M.; Howard, M.; Zhu, R.; et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020, 146, 595–605. [Google Scholar] [CrossRef]
- Klimek, L.; Pfaar, O.; Worm, M.; Eiwegger, T.; Hagemann, J.; Ollert, M.; Untersmayr, E.; Hoffmann-Sommergruber, K.; Vultaggio, A.; Agache, I.; et al. Use of biologicals in allergic and type-2 inflammatory diseases during the current COVID-19 pandemic: Position paper of Arzteverband Deutscher Allergologen (AeDA)(A), Deutsche Gesellschaft fur Allergologie und Klinische Immunologie (DGAKI)(B), Gesellschaft fur Padiatrische Allergologie und Umweltmedizin (GPA)(C), Osterreichische Gesellschaft fur Allergologie und Immunologie (OGAI)(D), Luxemburgische Gesellschaft fur Allergologie und Immunologie (LGAI)(E), Osterreichische Gesellschaft fur Pneumologie (OGP)(F) in co-operation with the German, Austrian, and Swiss ARIA groups(G), and the European Academy of Allergy and Clinical Immunology (EAACI)(H). Allergol. Select 2020, 4, 53–68. [Google Scholar] [CrossRef]
- Klimek, L.; Becker, S.; Chaker, A.; Strieth, S.; Hoffmann, T.K.; Dazert, S.; Deitmer, T.; Olze, H.; Glien, A.; Plontke, S.; et al. Positionspapier: Anwendung von Biologika bei chronischer Rhinosinusitis mit Polyposis nasi (CRSwNP) im deutschen Gesundheitssystem—Empfehlungen des Ärzteverbandes Deutscher Allergologen (AeDA) und der AGs Klinische Immunologie, Allergologie und Umweltmedizin und Rhinologie und Rhinochirurgie der Deutschen Gesellschaft für HNO-Heilkunde, Kopf- und Halschirurgie (DGHNOKHC). Laryngorhinootologie 2020, 99, 511–527. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Han, J.K.; Wagenmann, M.; Hosemann, W.; Lee, S.E.; Backer, V.; Mullol, J.; Gevaert, P.; Klimek, L.; Prokopakis, E.; et al. EUFOREA expert board meeting on uncontrolled severe chronic rhinosinusitis with nasal polyps (CRSwNP) and biologics: Definitions and management. J. Allergy Clin. Immunol. 2021, 147, 29–36. [Google Scholar] [CrossRef]
- Klimek, L.; Forster-Ruhrmann, U.; Olze, H.; Beule, A.G.; Chaker, A.M.; Hagemann, J.; Huppertz, T.; Hoffmann, T.K.; Dazert, S.; Deitmer, T.; et al. Empfehlungen zur Überprüfung der Wirksamkeit und Verlaufsdokumentation von Dupilumab bei chronischer Rhinosinusitis mit Nasenpolypen (CRSwNP) im deutschen Gesundheitssystem. Laryngorhinootologie 2022, 101, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Klimek, L.; Forster-Ruhrmann, U.; Olze, H.; Beule, A.G.; Chaker, A.M.; Hagemann, J.; Huppertz, T.; Hoffmann, T.K.; Dazert, S.; Deitmer, T.; et al. Empfehlungen zur Überprüfung der Wirksamkeit und Verlaufsdokumentation von Mepolizumab bei chronischer Rhinosinusitis mit Nasenpolypen (CRSwNP) im deutschen Gesundheitssystem—Empfehlungen des Ärzteverbandes Deutscher Allergologen (AeDA) und der AGs Klinische Immunologie, Allergologie und Umweltmedizin und Rhinologie und Rhinochirurgie der Deutschen Gesellschaft für HNO-Heilkunde, Kopf- und Halschirurgie (DGHNOKHC). Laryngorhinootologie 2023, 102, 89–99. [Google Scholar] [CrossRef] [PubMed]
- DeConde, A.S.; Mace, J.C.; Bodner, T.; Hwang, P.H.; Rudmik, L.; Soler, Z.M.; Smith, T.L. SNOT-22 quality of life domains differentially predict treatment modality selection in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2014, 4, 972–979. [Google Scholar] [CrossRef]
- Albrecht, T.; Beule, A.G.; Hildenbrand, T.; Gerstacker, K.; Praetorius, M.; Rudack, C.; Baumann, I. Cross-cultural adaptation and validation of the 22-item sinonasal outcome test (SNOT-22) in German-speaking patients: A prospective, multicenter cohort study. Eur. Arch. Otorhinolaryngol. 2022, 279, 2433–2439. [Google Scholar] [CrossRef]
- Hopkins, C.; Gillett, S.; Slack, R.; Lund, V.J.; Browne, J.P. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin. Otolaryngol. 2009, 34, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, P.; Calus, L.; Van Zele, T.; Blomme, K.; De Ruyck, N.; Bauters, W.; Hellings, P.; Brusselle, G.; De Bacquer, D.; van Cauwenberge, P.; et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 2013, 131, 110–116.e1. [Google Scholar] [CrossRef] [PubMed]
- Lildholdt, T.; Rundcrantz, H.; Bende, M.; Larsen, K. Glucocorticoid treatment for nasal polyps. The use of topical budesonide powder, intramuscular betamethasone, and surgical treatment. Arch. Otolaryngol. Head Neck Surg. 1997, 123, 595–600. [Google Scholar] [CrossRef]
- Scangas, G.A.; Wu, A.W.; Ting, J.Y.; Metson, R.; Walgama, E.; Shrime, M.G.; Higgins, T.S. Cost Utility Analysis of Dupilumab Versus Endoscopic Sinus Surgery for Chronic Rhinosinusitis With Nasal Polyps. Laryngoscope 2021, 131, E26–E33. [Google Scholar] [CrossRef]
- Damask, C.; Chen, M.; Holweg, C.T.J.; Yoo, B.; Millette, L.A.; Franzese, C. Defining the Efficacy of Omalizumab in Nasal Polyposis: A POLYP 1 and POLYP 2 Subgroup Analysis. Am. J. Rhinol. Allergy 2022, 36, 135–141. [Google Scholar] [CrossRef]
- Gevaert, P.; Saenz, R.; Corren, J.; Han, J.K.; Mullol, J.; Lee, S.E.; Ow, R.A.; Zhao, R.; Howard, M.; Wong, K.; et al. Long-term efficacy and safety of omalizumab for nasal polyposis in an open-label extension study. J. Allergy Clin. Immunol. 2022, 149, 957–965.e3. [Google Scholar] [CrossRef]
- Haxel, B.R.; Hummel, T.; Fruth, K.; Lorenz, K.; Gunder, N.; Nahrath, P.; Cuevas, M. Real-world-effectiveness of biological treatment for severe chronic rhinosinusitis with nasal polyps. Rhinology 2022, 60, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Jansen, F.; Becker, B.; Eden, J.K.; Breda, P.C.; Hot, A.; Oqueka, T.; Betz, C.S.; Hoffmann, A.S. Dupilumab (Dupixent((R))) tends to be an effective therapy for uncontrolled severe chronic rhinosinusitis with nasal polyps: Real data of a single-centered, retrospective single-arm longitudinal study from a university hospital in Germany. Eur. Arch. Otorhinolaryngol. 2023, 280, 1741–1755. [Google Scholar] [CrossRef]
- Meier, E.C.; Schmid-Grendelmeier, P.; Steiner, U.C.; Soyka, M.B. Real-Life Experience of Monoclonal Antibody Treatments in Chronic Rhinosinusitis with Nasal Polyposis. Int. Arch. Allergy Immunol. 2021, 182, 736–743. [Google Scholar] [CrossRef]
- Detoraki, A.; Tremante, E.; Poto, R.; Morelli, E.; Quaremba, G.; Granata, F.; Romano, A.; Mormile, I.; Rossi, F.W.; de Paulis, A.; et al. Real-life evidence of low-dose mepolizumab efficacy in EGPA: A case series. Respir. Res. 2021, 22, 185. [Google Scholar] [CrossRef]
- Armengot-Carceller, M.; Gomez-Gomez, M.J.; Garcia-Navalon, C.; Domenech-Campos, E.; Munoz-Fernandez, N.; Miguel, A.G.; Marco-Algarra, J.; Palop-Cervera, M.; Pinero, A.G. Effects of Omalizumab Treatment in Patients With Recalcitrant Nasal Polyposis and Mild Asthma: A Multicenter Retrospective Study. Am. J. Rhinol. Allergy 2021, 35, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Kilty, S.J.; Lasso, A. Canadian real-world study of access and clinical results using dupilumab for chronic rhinosinusitis with polyps. J. Otolaryngol. Head Neck Surg. 2022, 51, 17. [Google Scholar] [CrossRef]
- Van der Lans, R.J.L.; Fokkens, W.J.; Adriaensen, G.; Hoven, D.R.; Drubbel, J.J.; Reitsma, S. Real-life observational cohort verifies high efficacy of dupilumab for chronic rhinosinusitis with nasal polyps. Allergy 2022, 77, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Forster-Ruhrmann, U.; Stergioudi, D.; Szczepek, A.J.; Fluhr, J.W.; Zuberbier, T.; Olze, H.; Bergmann, K.C. A real-life comparison of pulmonary and nasal outcomes in patients with severe asthma and nasal polyposis treated with T2-biologics. World Allergy Organ. J. 2023, 16, 100746. [Google Scholar] [CrossRef] [PubMed]
- Nowsheen, S.; Darveaux, J.I. Dupilumab in the treatment of nasal polyposis: A retrospective, real-world study. Ann. Allergy Asthma Immunol. 2021, 127, 386–387. [Google Scholar] [CrossRef] [PubMed]

| Epidemiologic Data | |
|---|---|
| Gender Male Female | 19 14 |
| Age Range Mean | 22–70 years 47.3 (SD +/−12.97) |
| Comorbidities (% of patients) Asthma Aspirin-exacerbated respiratory disease (AERD) | 72.7% 45.5% |
| Eosinophilia Tissue eosinophilia Blood eosinophils > 300/μL | 21/22 16/25 |
| Previous corticosteroid treatment Topical steroids Systemic steroids > 1 course | 100% 100% |
| Previous surgeries Range Mean ≥2 surgeries (% of patients) | 1–15 2.9 (SD +/−2.5) 75.8% |
| Secondary Outcome Parameters | |
|---|---|
| Surgery during treatment | 1/33 |
| Subjective improvement of sense of smell | 81.8% |
| Discontinuation of treatment | 1/33 |
| Change in monoclonal antibody | 7/33 |
| Adverse Events Abdominal pain Headaches Dizziness Eosinophilia Acute exacerbation of CRS | 8/33 1/33 2/33 1/33 4/33 1/33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerstacker, K.; Ketterer, M.C.; Jakob, T.F.; Hildenbrand, T. Real Life Observational Study of Treatment Success of Monoclonal Antibodies for Refractory Chronic Rhinosinusitis with Nasal Polyps. J. Clin. Med. 2023, 12, 4374. https://doi.org/10.3390/jcm12134374
Gerstacker K, Ketterer MC, Jakob TF, Hildenbrand T. Real Life Observational Study of Treatment Success of Monoclonal Antibodies for Refractory Chronic Rhinosinusitis with Nasal Polyps. Journal of Clinical Medicine. 2023; 12(13):4374. https://doi.org/10.3390/jcm12134374
Chicago/Turabian StyleGerstacker, Kathrin, Manuel Christoph Ketterer, Till Fabian Jakob, and Tanja Hildenbrand. 2023. "Real Life Observational Study of Treatment Success of Monoclonal Antibodies for Refractory Chronic Rhinosinusitis with Nasal Polyps" Journal of Clinical Medicine 12, no. 13: 4374. https://doi.org/10.3390/jcm12134374
APA StyleGerstacker, K., Ketterer, M. C., Jakob, T. F., & Hildenbrand, T. (2023). Real Life Observational Study of Treatment Success of Monoclonal Antibodies for Refractory Chronic Rhinosinusitis with Nasal Polyps. Journal of Clinical Medicine, 12(13), 4374. https://doi.org/10.3390/jcm12134374








