Defining Peri-Operative Myocardial Injury during Cardiac Surgery Using High-Sensitivity Troponin T
Abstract
1. Introduction
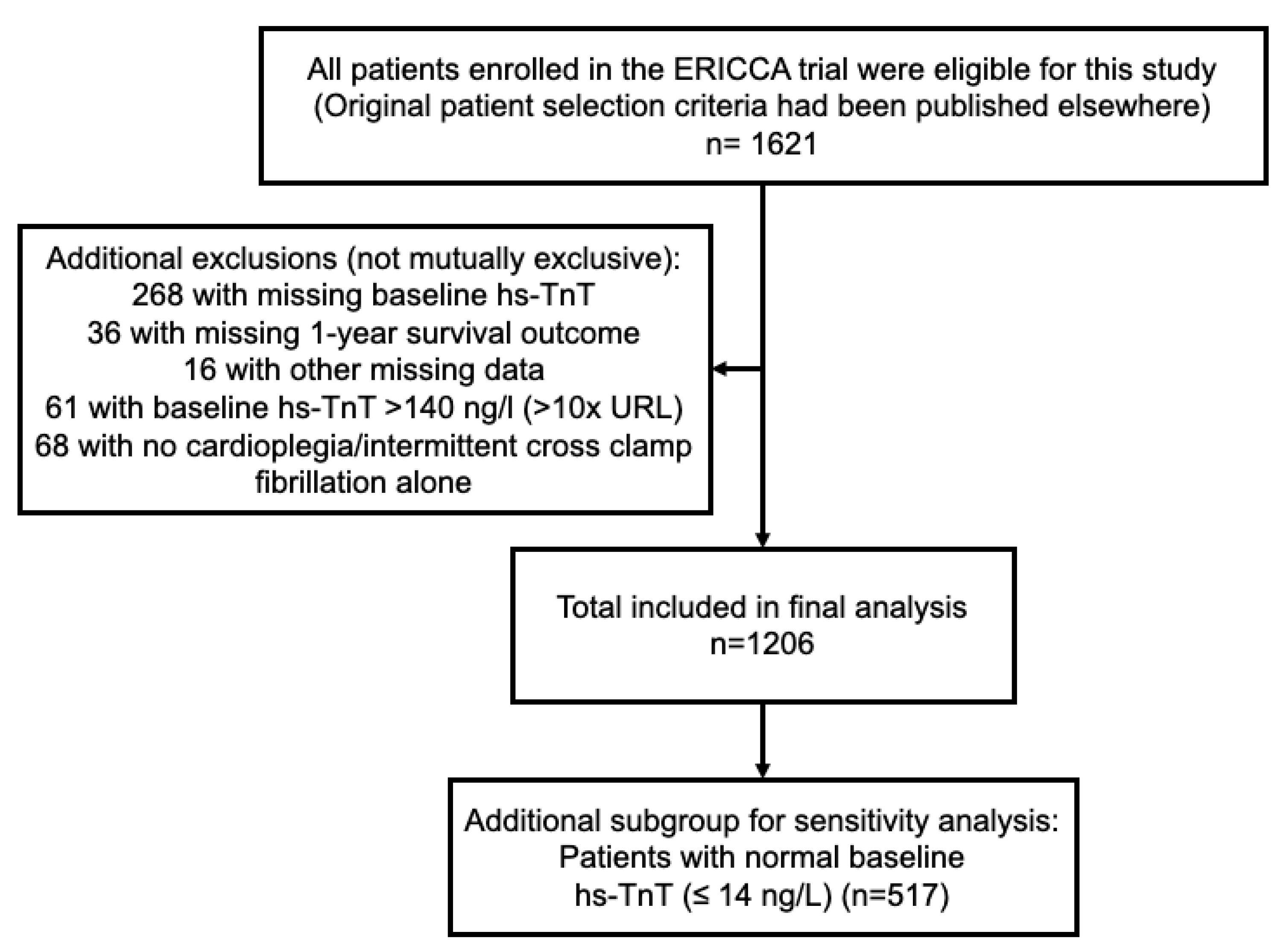
2. Methods
Statistical Analysis
3. Results
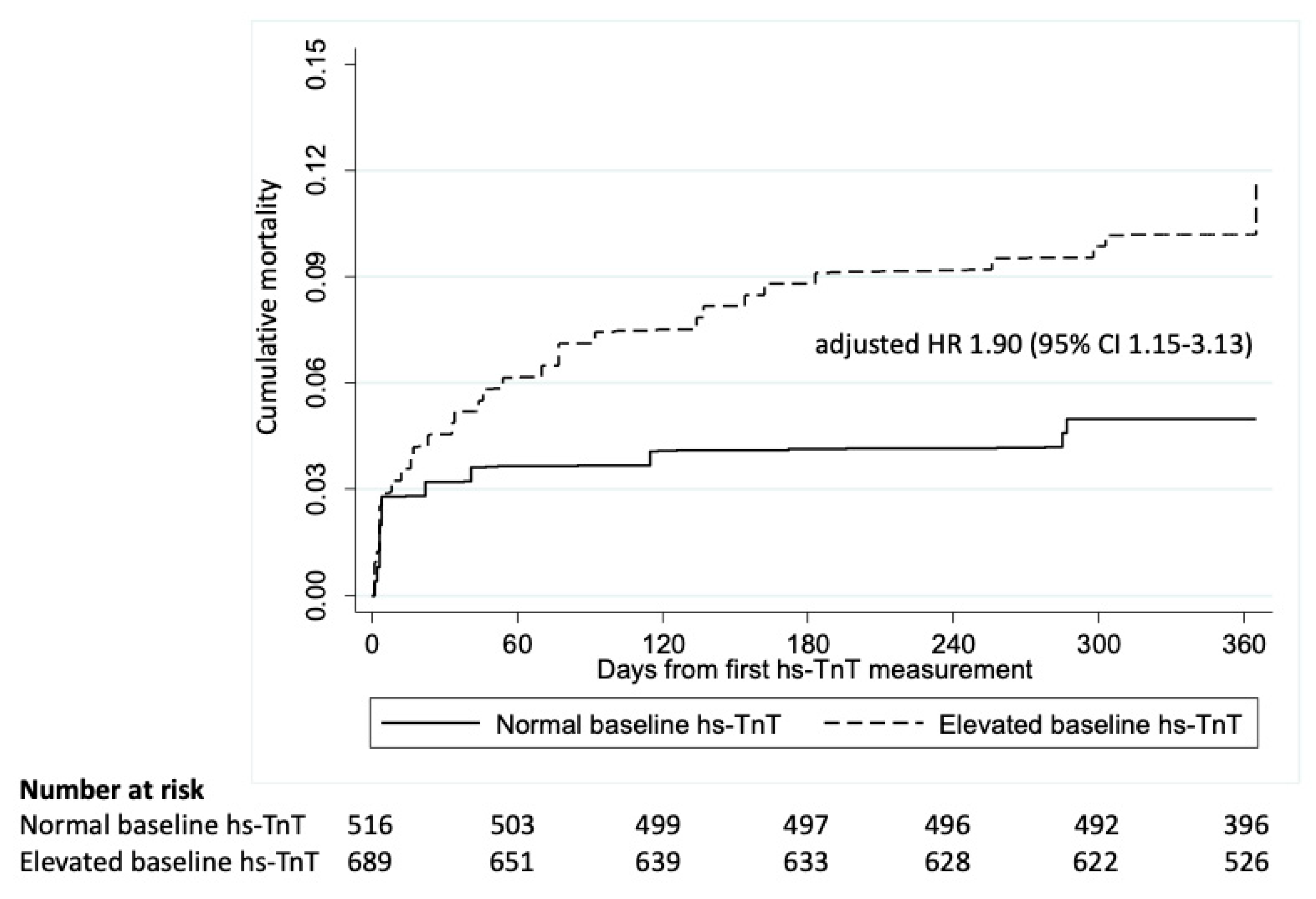
3.1. Baseline Tn-TnT Elevation and 1-Year All-Cause Mortality
3.2. Post-Operative Elevations in hs-TnT and 1-Year All-Cause Mortality in Patients with Normal Baseline hs-TnT (N = 517)
3.3. Post-Operative Elevations in hs-TnT and 1-Year All-Cause Mortality in Patients with Elevated hs-TnT (N = 689)
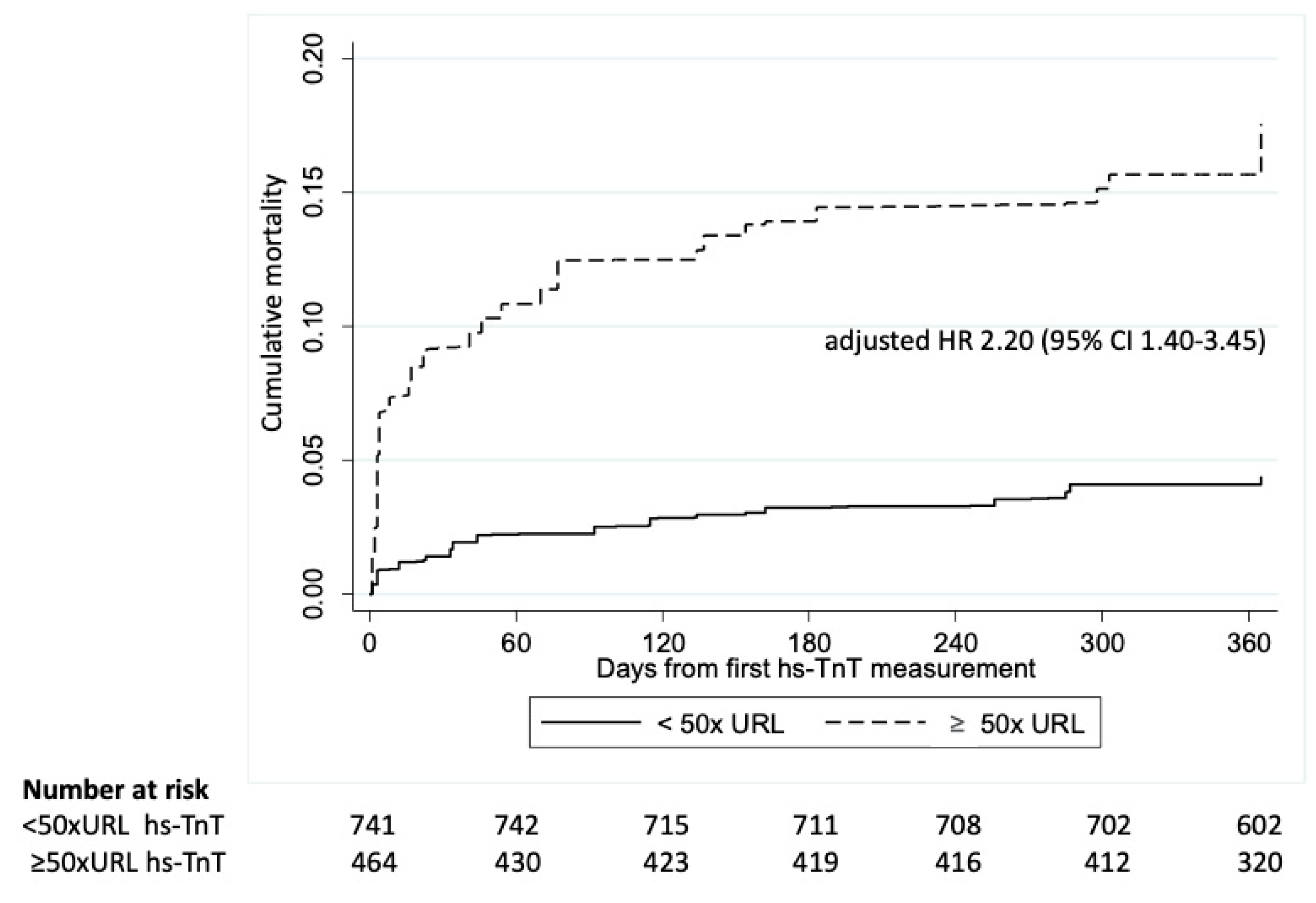
3.4. Post-Operative Elevations in hs-TnT and 1-Year All-Cause Mortality in the Whole Cohort (N = 1206)
3.5. Stratification by Left Ventricular Ejection Fraction (LVEF)
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thielmann, M.; Sharma, V.; Al-Attar, N.; Bulluck, H.; Bisleri, G.; Bunge, J.J.H.; Czerny, M.; Ferdinandy, P.; Frey, U.H.; Heusch, G.; et al. ESC Joint Working Groups on Cardiovascular Surgery and the Cellular Biology of the Heart Position Paper: Perioperative myocardial injury and infarction in patients undergoing coronary artery bypass graft surgery. Eur. Heart J. 2017, 38, 2392–2407. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Group, E.S.C.S.D. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [PubMed]
- Mauermann, E.; Bolliger, D.; Fassl, J.; Grapow, M.; Seeberger, E.E.; Seeberger, M.D.; Filipovic, M.; Lurati Buse, G.A.L. Postoperative High-Sensitivity Troponin and Its Association with 30-Day and 12-Month, All-Cause Mortality in Patients Undergoing On-Pump Cardiac Surgery. Anesth. Analg. 2017, 125, 1110–1117. [Google Scholar] [CrossRef] [PubMed]
- Mehdiani, A.; Akhyari, P.; Kamiya, H.; Ahlers, J.; Godehardt, E.; Albert, A.; Boeken, U.; Lichtenberg, A. Prognostic value of the new high sensitive cardiac troponin T assay (hs-cTnT) after coronary artery bypass grafting. Acta Cardiol. 2017, 72, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Omran, H.; Deutsch, M.A.; Groezinger, E.; Zittermann, A.; Renner, A.; Neumann, J.T.; Westermann, D.; Myles, P.; Ramosaj, B.; Pauly, M.; et al. High-sensitivity cardiac troponin I after coronary artery bypass grafting for post-operative decision-making. Eur. Heart J. 2022, 43, 2388–2403. [Google Scholar] [CrossRef] [PubMed]
- Devereaux, P.J.; Lamy, A.; Chan, M.T.V.; Allard, R.V.; Lomivorotov, V.V.; Landoni, G.; Zheng, H.; Paparella, D.; McGillion, M.H.; Belley-Cote, E.P.; et al. High-Sensitivity Troponin I after Cardiac Surgery and 30-Day Mortality. N. Engl. J. Med. 2022, 386, 827–836. [Google Scholar] [CrossRef] [PubMed]
- Heuts, S.; Denessen, E.J.S.; Daemen, J.H.T.; Vroemen, W.H.M.; Sels, J.W.; Segers, P.; Bekers, O.; van ‘t Hof, A.W.J.; Maessen, J.G.; van der Horst, I.C.C.; et al. Meta-Analysis Evaluating High-Sensitivity Cardiac Troponin T Kinetics after Coronary Artery Bypass Grafting in Relation to the Current Definitions of Myocardial Infarction. Am. J. Cardiol. 2022, 163, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Denessen, E.J.; Heuts, S.; Daemen, J.H.; van Doorn, W.P.; Vroemen, W.H.; Sels, J.W.; Segers, P.; Van’t Hof, A.W.; Maessen, J.G.; Bekers, O.; et al. High-Sensitivity Cardiac Troponin I and T Kinetics Differ following Coronary Bypass Surgery: A Systematic Review and Meta-Analysis. Clin. Chem. 2022, 68, 1564–1575. [Google Scholar] [CrossRef] [PubMed]
- Hausenloy, D.J.; Candilio, L.; Evans, R.; Ariti, C.; Jenkins, D.P.; Kolvekar, S.; Knight, R.; Kunst, G.; Laing, C.; Nicholas, J.; et al. Remote Ischemic Preconditioning and Outcomes of Cardiac Surgery. N. Engl. J. Med. 2015, 373, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Hamarneh, A.; Ho, A.F.W.; Bulluck, H.; Sivaraman, V.; Ricciardi, F.; Nicholas, J.; Shanahan, H.; Hardman, E.A.; Wicks, P.; Ramlall, M.; et al. Negative interaction between nitrates and remote ischemic preconditioning in patients undergoing cardiac surgery: The ERIC-GTN and ERICCA studies. Basic Res. Cardiol. 2022, 117, 31. [Google Scholar] [CrossRef] [PubMed]
- Bulluck, H.; Maiti, R.; Chakraborty, B.; Candilio, L.; Clayton, T.; Evans, R.; Jenkins, D.P.; Kolvekar, S.; Kunst, G.; Laing, C.; et al. Neutrophil gelatinase-associated lipocalin prior to cardiac surgery predicts acute kidney injury and mortality. Heart 2018, 104, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Moussa, I.D.; Klein, L.W.; Shah, B.; Mehran, R.; Mack, M.J.; Brilakis, E.S.; Reilly, J.P.; Zoghbi, G.; Holper, E.; Stone, G.W. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: An expert consensus document from the Society for Cardiovascular Angiography and Interventions (SCAI). J. Am. Coll. Cardiol. 2013, 62, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, H.M.; McFadden, E.P.; Farb, A.; Mehran, R.; Stone, G.W.; Spertus, J.; Onuma, Y.; Morel, M.A.; van Es, G.A.; Zuckerman, B.; et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Circulation 2018, 137, 2635–2650. [Google Scholar] [CrossRef] [PubMed]
- Petaja, L.; Rosjo, H.; Mildh, L.; Suojaranta-Ylinen, R.; Kaukonen, K.M.; Jokinen, J.J.; Salmenpera, M.; Hagve, T.A.; Omland, T.; Pettila, V. Predictive value of high-sensitivity troponin T in addition to EuroSCORE II in cardiac surgery. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Gahl, B.; Gober, V.; Odutayo, A.; Tevaearai Stahel, H.T.; da Costa, B.R.; Jakob, S.M.; Fiedler, G.M.; Chan, O.; Carrel, T.P.; Juni, P. Prognostic Value of Early Postoperative Troponin T in Patients Undergoing Coronary Artery Bypass Grafting. J. Am. Heart Assoc. 2018, 7, e007743. [Google Scholar] [CrossRef] [PubMed]
- Nellipudi, J.A.; Baker, R.A.; Dykes, L.; Krieg, B.M.; Bennetts, J.S. Prognostic Value of High-Sensitivity Troponin T After On-Pump Coronary Artery Bypass Graft Surgery. Heart Lung Circ. 2021, 30, 1562–1569. [Google Scholar] [CrossRef] [PubMed]

| Baseline Characteristics | |
|---|---|
| Age in years, median (IQR) | 77 (73–81) |
| Sex, n (%) | |
| Female | 350 (29.0) |
| Male | 856 (71.0) |
| Ethnicity, n (%) | |
| Caucasian | 1139 (94.4) |
| Asian | 57 (4.7) |
| Afro-Caribbean | 5 (0.4) |
| Others | 5 (0.4) |
| Body mass index in kg/m2, median (IQR) | 27.2 (24.6–30.4) |
| Smoking status, n (%) | |
| Current | 62 (5.1) |
| Former | 707 (58.6) |
| Never | 437 (36.2) |
| Systolic blood pressure in mmHg, median (IQR) | 133 (120–147) |
| Diastolic blood pressure in mmHg, median (IQR) | 70 (63–79) |
| Heart rate in bpm, median (IQR) | 67 (60–76) |
| NYHA class, n (%) | |
| 0 | 172 (14.3) |
| I | 168 (13.9) |
| II | 514 (42.6) |
| III | 329 (27.3) |
| IV | 23 (1.9) |
| CCS class, n (%) | |
| 0 | 361 (29.9) |
| I | 207 (17.2) |
| II | 383 (31.8) |
| III | 171 (14.2) |
| IV | 84 (7.0) |
| Left ventricular ejection fraction, n (%) | |
| >50% | 795 (68.7) |
| 30–50% | 239 (20.7) |
| <30% | 123 (10.6) |
| Past medical history | |
| Diabetes mellitus, n (%) | 325 (27.0) |
| Hypertension, n (%) | 933 (77.4) |
| Hypercholesterolemia, n (%) | 850 (70.5) |
| Atrial fibrillation, n (%) | 195 (16.2) |
| Myocardial infarction, n (%) | 463 (38.4) |
| Percutaneous coronary intervention, n (%) | 181 (15.0) |
| Stroke, n (%) | 136 (11.3) |
| Coronary artery bypass graft, n (%) | 33 (2.7) |
| Peripheral arterial disease, n (%) | 90 (7.5) |
| Pre-op NGAL in ng/mL, median (IQR) | 173.2 (115.8–253.7) |
| Pre-op creatinine in mol/µL, median (IQR) | 90 (76–108) |
| EuroSCORE, median (IQR) | 6 (5–7) |
| Surgery details | |
| Bypass duration in minutes, median (IQR) | 106 (84–136) |
| Cross-clamp duration in minutes, median (IQR) | 71 (51–97) |
| Valve surgery, n (%) | 621 (51.5) |
| Number of grafts, n (%) | |
| 1 | 254 (21.5) |
| 2 | 294 (24.9) |
| 3 | 462 (39.2) |
| ≥4 | 169 (14.3) |
| Troponin T details | |
| Available at 6 h, n (%) | 1048 (86.9) |
| Available at 12 h, n (%) | 1030 (85.4) |
| Available at 24 h, n (%) | 1063 (88.1) |
| Available at 48 h, n (%) | 947 (78.5) |
| Available at 72 h, n (%) | 827 (68.6) |
| Time Point | ×URL | Deaths/N for Patients with hs-TnT above Cut-Off | Deaths/N for Patients with hs-TnT below Cut-Off | Sensitivity | Specificity | Adjusted HR (95% CI) * | AUC (95% CI) * |
|---|---|---|---|---|---|---|---|
| 6 h | 50 | 23/295 | 4/222 | 85% | 45% | 1.54 (0.63–3.79) | 0.675 (0.561–0.789) |
| 70 | 18/188 | 10/329 | 66% | 65% | 1.58 (0.67–3.71) | 0.667 (0.551–0.784) | |
| 100 | 15/101 | 13/416 | 54% | 82% | 2.86 (1.15–7.10) | 0.685 (0.573–0.798) | |
| 12 h | 35 | 26/350 | 1/167 | 95% | 34% | 1.66 (0.62–4.47) | 0.677 (0.564–0.790) |
| 50 | 25/246 | 2/271 | 92% | 55% | 2.71 (1.07–6.87) | 0.715 (0.610–0.820) | |
| 70 | 18/123 | 9/366 | 66% | 75% | 3.33 (1.43–7.74) | 0.723 (0.618–0.828) | |
| 24 h | 35 | 23/254 | 4/263 | 84% | 53% | 1.76 (0.74–4.20) | 0.685 (0.575–0.795) |
| 50 | 20/145 | 7/372 | 73% | 75% | 2.99 (1.29–6.90) | 0.705 (0.589–0.822) | |
| 70 | 18/90 | 9/427 | 66% | 85% | 3.87 (1.59–9.40) | 0.730 (0.618–0.843) | |
| 48 h | 35 | 21/171 | 6/346 | 78% | 69% | 3.47 (1.44–8.33) | 0.731 (0.626–0.836) |
| 50 | 19/97 | 9/420 | 68% | 84% | 3.96 (1.57–9.95) | 0.740 (0.634–0.845) | |
| 70 | 14/54 | 14/463 | 50% | 92% | 5.03 (1.80–14.01) | 0.728 (0.613–0.843) | |
| 72 h | 30 | 21/184 | 7/333 | 75% | 67% | 3.49 (1.31–9.30) | 0.742 (0.645–0.840) |
| 35 | 19/154 | 9/363 | 69% | 73% | 3.23 (1.21–8.59) | 0.740 (0.645–0.835) | |
| 50 | 13/85 | 15/432 | 47% | 85% | 2.18 (0.66–7.15) | 0.709 (0.602–0.817) |
| Time Point | ×URL | Deaths/N for Patients with hs-TnT above Cut-Off | Deaths/N for Patients with hs-TnT below Cut-Off | Sensitivity | Specificity | Adjusted HR (95% CI) * | AUC (95% CI) * |
|---|---|---|---|---|---|---|---|
| 6 h | 50 | 54/357 | 23/332 | 70 | 51 | 1.47 (0.88–2.45) | 0.611 (0.537–0.685) |
| 70 | 41/242 | 35/447 | 54 | 67 | 1.54 (0.92–2.56) | 0.619 (0.546–0.692) | |
| 100 | 33/136 | 44/553 | 43 | 83 | 2.60 (1.52–4.44) | 0.656 (0.582–0.729) | |
| 12 h | 35 | 62/466 | 15/223 | 81 | 34 | 1.41 (0.78–2.55) | 0.616 (0.541–0.690) |
| 50 | 52/338 | 25/351 | 68 | 53 | 1.71 (1.02–2.88) | 0.628 (0.554–0.702) | |
| 70 | 40/223 | 37/466 | 52 | 70 | 1.85 (1.11–3.10) | 0.640 (0.570–0.711) | |
| 24 h | 35 | 54/365 | 23/324 | 71 | 49 | 1.47 (0.87–2.48) | 0.619 (0.546–0.691) |
| 50 | 49/254 | 27/435 | 65 | 67 | 2.03 (1.20–3.42) | 0.648 (0.576–0.719) | |
| 70 | 37/145 | 39/544 | 49 | 83 | 2.17 (1.26–3.73) | 0.657 (0.586–0.727) | |
| 48 h | 35 | 50/286 | 26/403 | 66 | 62 | 2.12 (1.25–3.57) | 0.656 (0.584–0.728) |
| 50 | 40/183 | 37/506 | 52 | 77 | 2.22 (1.29–3.81) | 0.655 (0.583–0.727) | |
| 70 | 32/115 | 45/574 | 42 | 86 | 3.35 (1.91–5.87) | 0.688 (0.616–0.760) | |
| 72 h | 30 | 51/296 | 26/393 | 67 | 60 | 2.14 (1.25–3.66) | 0.653 (0.580–0.726) |
| 35 | 48/259 | 29/430 | 62 | 66 | 2.15 (1.29–3.58) | 0.652 (0.581–0.723) | |
| 50 | 36/154 | 40/535 | 47 | 81 | 2.64 (1.54–4.53) | 0.657 (0.584–0.731) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, V.; Zheng, H.; Candilio, L.; Nicholas, J.M.; Clayton, T.; Yellon, D.M.; Bulluck, H.; Hausenloy, D.J. Defining Peri-Operative Myocardial Injury during Cardiac Surgery Using High-Sensitivity Troponin T. J. Clin. Med. 2023, 12, 4291. https://doi.org/10.3390/jcm12134291
Sharma V, Zheng H, Candilio L, Nicholas JM, Clayton T, Yellon DM, Bulluck H, Hausenloy DJ. Defining Peri-Operative Myocardial Injury during Cardiac Surgery Using High-Sensitivity Troponin T. Journal of Clinical Medicine. 2023; 12(13):4291. https://doi.org/10.3390/jcm12134291
Chicago/Turabian StyleSharma, Vikram, Huili Zheng, Luciano Candilio, Jennifer M. Nicholas, Tim Clayton, Derek M. Yellon, Heerajnarain Bulluck, and Derek J. Hausenloy. 2023. "Defining Peri-Operative Myocardial Injury during Cardiac Surgery Using High-Sensitivity Troponin T" Journal of Clinical Medicine 12, no. 13: 4291. https://doi.org/10.3390/jcm12134291
APA StyleSharma, V., Zheng, H., Candilio, L., Nicholas, J. M., Clayton, T., Yellon, D. M., Bulluck, H., & Hausenloy, D. J. (2023). Defining Peri-Operative Myocardial Injury during Cardiac Surgery Using High-Sensitivity Troponin T. Journal of Clinical Medicine, 12(13), 4291. https://doi.org/10.3390/jcm12134291






