Malignant Transformation and Long-Term Outcome of Oral and Laryngeal Leukoplakia
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baran, C.A.; Agaimy, A.; Wehrhan, F.; Weber, M.; Hille, V.; Brunner, K.; Wickenhauser, C.; Siebolts, U.; Nkenke, E.; Kesting, M.; et al. MAGE-A expression in oral and laryngeal leukoplakia predicts malignant transformation. Mod. Pathol. 2019, 32, 1068–1081. [Google Scholar] [CrossRef]
- van Hulst, A.M.; Kroon, W.; van der Linden, E.S.; Nagtzaam, L.; Ottenhof, S.R.; Wegner, I.; Gunning, A.C.; Grolman, W.; Braunius, W. Grade of dysplasia and malignant transformation in adults with premalignant laryngeal lesions. Head Neck 2016, 38, 2284–2290. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Ariyawardana, A. Malignant transformation of oral leukoplakia: A systematic review of observational studies. J. Oral Pathol. Med. 2016, 45, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Weller, M.; Nankivell, P.; McConkey, C.; Paleri, V.; Mehanna, H. The risk and interval to malignancy of patients with laryngeal dysplasia; a systematic review of case series and meta-analysis. Clin. Otolaryngol. 2010, 35, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Isenberg, J.S.; Crozier, D.L.; Dailey, S.H. Institutional and Comprehensive Review of Laryngeal Leukoplakia. Ann. Otol. Rhinol. Laryngol. 2008, 117, 74–79. [Google Scholar] [CrossRef]
- Iocca, O.; Sollecito, T.P.; Alawi, F.; Weinstein, G.S.; Newman, J.G.; De Virgilio, A.; Di Maio, P.; Spriano, G.; López, S.P.; Shanti, R.M. Potentially malignant disorders of the oral cavity and oral dysplasia: A systematic review and meta-analysis of malignant transformation rate by subtype. Head Neck 2020, 42, 539–555. [Google Scholar] [CrossRef]
- Kuribayashi, Y.; Tsushima, F.; Morita, K.-I.; Matsumoto, K.; Sakurai, J.; Uesugi, A.; Sato, K.; Oda, S.; Sakamoto, K.; Harada, H. Long-term outcome of non-surgical treatment in patients with oral leukoplakia. Oral Oncol. 2015, 51, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Kujan, O.; Aguirre-Urizar, J.M.; Bagan, J.V.; González-Moles, M.; Kerr, A.R.; Lodi, G.; Mello, F.W.; Monteiro, L.; Ogden, G.R.; et al. Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer. Oral Dis. 2021, 27, 1862–1880. [Google Scholar] [CrossRef]
- Hsue, S.S.; Wang, W.C.; Chen, C.H.; Lin, C.C.; Chen, Y.K.; Lin, L.M. Malignant transformation in 1458 patients with potentially ma-lignant oral mucosal disorders: A follow-up study based in a Taiwanese hospital. J. Oral Pathol. Med. 2007, 36, 25–29. [Google Scholar] [CrossRef]
- van der Waal, I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009, 45, 317–323. [Google Scholar] [CrossRef]
- Karatayli-Ozgursoy, S.; Pacheco-Lopez, P.; Hillel, A.T.; Best, S.R.; Bishop, J.A.; Akst, L.M. Laryngeal dysplasia, demographics, and treatment: A single-institution, 20-year review. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Eversole, L.R. Dysplasia of the upper aerodigestive tract squamous epithelium. Head Neck Pathol. 2009, 3, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Gale, N.; Zidar, N.; Poljak, M.; Cardesa, A. Current views and perspectives on classification of squamous intraepithelial lesions of the head and neck. Head Neck Pathol. 2014, 8, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, E.; Meier, P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Cox, D.R. Regression models and life-tables. J. R. Stat. Soc. 1972, 34, 187–220. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Y.-F.; Zhou, H.-W.; Shi, P.; Zhou, Z.-T.; Tang, G.-Y. Malignant transformation of oral leukoplakia: A retrospective cohort study of 218 Chinese patients. BMC Cancer 2010, 10, 685. [Google Scholar] [CrossRef]
- Liu, W.; Shi, L.J.; Wu, L.; Feng, J.Q.; Yang, X.; Li, J.; Zhou, Z.T.; Zhang, C.P. Oral cancer development in patients with leukoplakia—Clinicopathological factors affecting outcome. PLoS ONE 2012, 7, 34773. [Google Scholar] [CrossRef]
- de Vicente, J.C.; del Molino, P.D.-P.; Rodrigo, J.P.; Allonca, E.; Hermida-Prado, F.; Granda-Díaz, R.; Santamarta, T.R.; García-Pedrero, J.M. SOX2 Expression Is an Independent Predictor of Oral Cancer Progression. J. Clin. Med. 2019, 8, 1744. [Google Scholar] [CrossRef]
- Aguirre-Urizar, J.M.; de Mendoza, I.L.I.; Saman Warnakulasuriya, S. Malignant transformation of oral leukoplakia: Systematic review and meta-analysis of the last 5 years. Oral Dis. 2021, 27, 1881–1895. [Google Scholar] [CrossRef]
- Jäwert, F.; Pettersson, H.; Jagefeldt, E.; Holmberg, E.; Kjeller, G.; Öhman, J. Clinicopathologic factors associated with malignant transformation of oral leukoplakias: A retrospective cohort study. Int. J. Oral Maxillofac. Surg. 2021, 50, 1422–1428. [Google Scholar] [CrossRef]
- Bagan, J.; Martorell, M.; Cebrián, J.L.; Rubert, A.; Bagán, L.; Mezquida, C.; Hervás, D. Effect of clinical and histologic features on time to malignancy in 224 cases of oral leukoplakia treated by surgery. Clin. Oral Investig. 2022, 26, 5181–5188. [Google Scholar] [CrossRef]
- Jäwert, F.; Nyman, J.; Olsson, E.; Adok, C.; Helmersson, M.; Öhman, J. Regular clinical follow-up of oral potencially malignant dis-orders results in improved survival for patients who develop oral cancer. Oral Oncol. 2021, 121, 105469. [Google Scholar] [CrossRef]
- Chaturvedi, A.K.; Udaltsova, N.; Engels, E.A.; Katzel, J.A.; Yanik, E.L.; Katki, H.A.; Lingen, M.W.; Silverberg, M.J. Oral Leukoplakia and Risk of Progression to Oral Cancer: A Population-Based Cohort Study. Gynecol. Oncol. 2020, 112, 1047–1054. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.Y.; Wang, J.; Huo, H.; Jin, X.F.; Li, W.Y.; Gao, Z.Q. Clinical analyses of 263 patients with laryngeal leukoplakia. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2018, 53, 575–580. [Google Scholar] [PubMed]
- Jabarin, B.; Pitaro, J.; Marom, T.; Muallem-Kalmovich, L. Dysplastic Changes in Patients with Recurrent Laryngeal Leukoplakia: Importance of Long-Term Follow-Up. Isr. Med. Assoc. J. 2018, 20, 623–626. [Google Scholar] [PubMed]
- Zhang, H.; Chen, X.M.; Li, Z.H. Clinical analysis of vocal cord leukoplakia in 32 cases. Lin Chuang Er Bi Yan Hou Ke Za Zhi J. Clin. Otorhinolaryngol. 2000, 14, 22–23. [Google Scholar]
- Leduchowska, A.; Morawska, J.; Pietruszewska, W. Videolaryngoendoscopic and Stroboscopic Evaluation in Predicting the Ma-lignancy Risk of Vocal Fold Leukoplakia. J. Clin. Med. 2022, 11, 5789. [Google Scholar] [CrossRef]
| Characteristic | Malignant Events n (%) | p | 10-Year MTFS % (±SD) | p | Univariate Cox HR (CI 95%) | p |
|---|---|---|---|---|---|---|
| All patients | 64/253 (25.3%) | 81.5 ± 2.6 | ||||
| Gender | ||||||
| female | 29/138 (21%) | 0.11 | 86.0 ± 3.2 | 0.061 | 1 | 0.065 |
| male | 35/115 (30.4%) | 76.3 ± 4.3 | 1.72 (0.97–3.06) | |||
| Age (years) | ||||||
| ≤60 | 38/152 (25%) | >0.999 | 79.8 ± 4.7 | 0.546 | 1 | 0.548 |
| >60 | 26/101 (25.7%) | 81.9 ± 3.3 | 1.20 (0.66–2.16) | |||
| Smoking | ||||||
| never | 5/34 (14.7%) | 0.0004 | 87.8 ± 5.7 | 0.004 | 1 | 0.009 |
| past and present | 47/96 (49%) | 62.6 ± 5.6 | 4.01 (1.42–11.30) | |||
| unknown | 12/123 (9.8%) | |||||
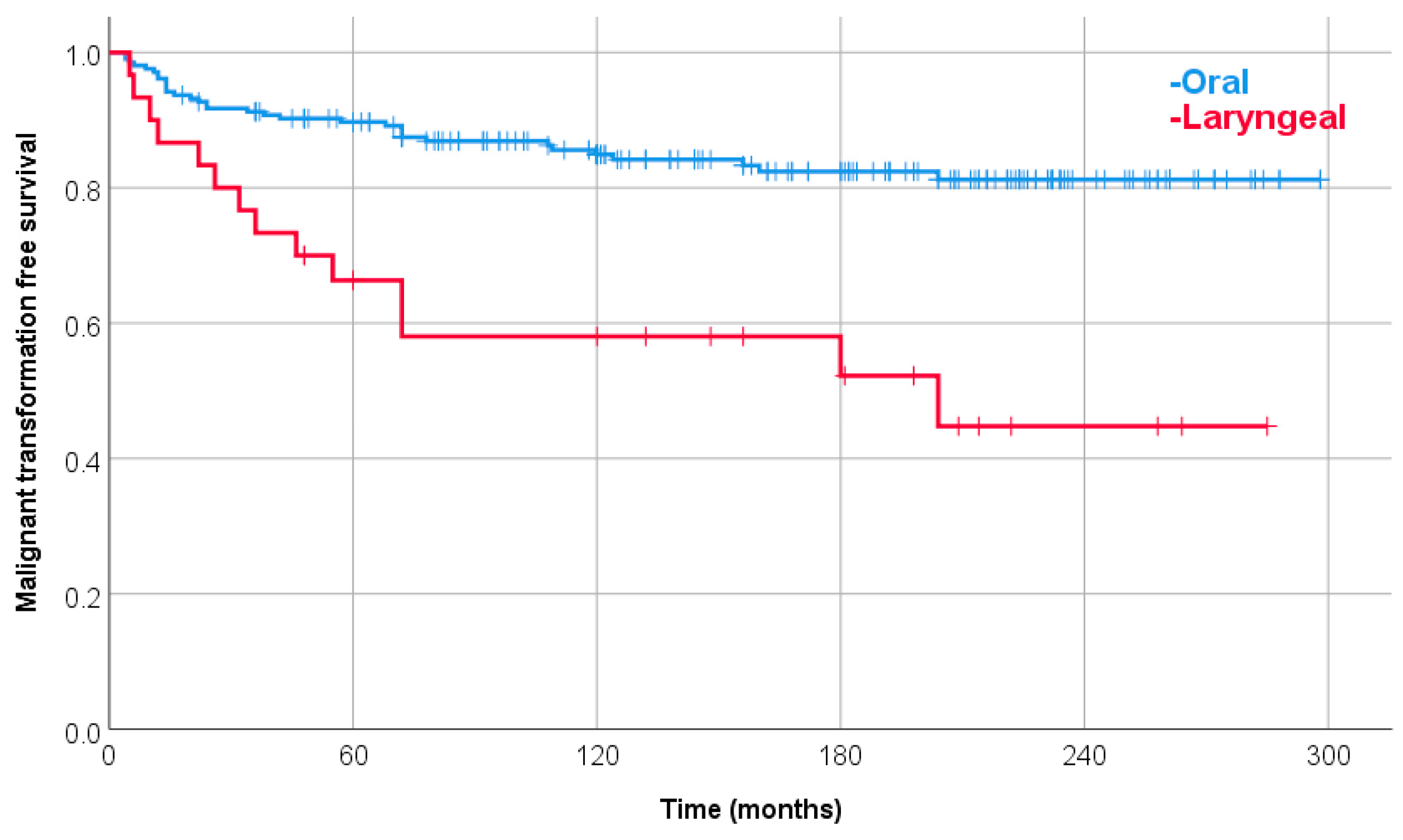
| Oral vs. laryngeal | ||||||
| oral | 48/221 (21.7%) | 0.002 | 84.9 ± 2.6 | <0.0001 | 1 | <0.0001 |
| laryngeal | 16/32 (50%) | 58.0 ± 9.4 | 3.13 (1.71–5.72) | |||
| Lesion type | ||||||
| homogenous | 53/236 (22.5%) | 0.0004 | 83.2 ± 2.6 | 0.003 | 1 | 0.005 |
| non-homogenous | 11/17 (64.7%) | 53.8 ± 13.8 | 3.46 (1.46–8.18) | |||
| Biopsy | ||||||
| no | 4/83 (4.8%) | <0.0001 | 95.9 ± 2.4 | <0.0001 | 1 | <0.0001 |
| yes | 60/170 (35.3%) | 74.0 ± 3.7 | 6.48 (2.33–18.05) | |||
| Histology | ||||||
| no dysplasia | 5/88 (5.7%) | <0.0001 | 95.3 ± 2.3 | <0.0001 | 1 | <0.0001 |
| grade I dysplasia | 7/29 (24.1%) | 79.3 ± 7.5 | 4.76 (1.51–15.03) | |||
| grade II dysplasia | 16/20 (80%) | 18.3 ± 10.3 | 32.62 (11.51–92.44) | |||
| grade III dysplasia | 15/16 (93.8%) | 18.8 ± 9.8 | 29.79 (10.73–82.73) | |||
| in situ cancer | 5 | |||||
| invasive cancer | 12 | |||||
| Dysplasia | ||||||
| no | 5/88 (5.7%) | <0.0001 | 95.3 ± 2.3 | <0.0001 | 1 | <0.0001 |
| yes | 38/65 (58.5) | 45.9 ± 6.4 | 14.58 (5.71–37.24) | |||
| Dysplasia | ||||||
| low grade (I) | 7/29 (24.1%) | <0.0001 | 79.3 ± 7.5 | <0.0001 | 1 | <0.0001 |
| high grade (II, III) | 31/36 (86.1%) | 18.3 ± 7.0 | 6.78 (2.94–15.63) |
| Characteristic | Multivariate Cox HR (CI 95%) | p |
|---|---|---|
| Smoking | ||
| never | 1 | 0.142 |
| past and present | 2.49 (0.74–8.44) | |
| Lesion type | ||
| homogenous | 1 | 0.014 |
| non-homogenous | 3.74 (1.31–10.09) | |
| Dysplasia | ||
| no | 1 | <0.0001 |
| low grade (I) | 4.23 (1.11–16.16) | |
| high grade (II, III) | 12.25 (4.10–36.66) |
| Characteristic | Malignant Events n (%) | p | 10-Year MTFS %, SD | p | Univariate Cox HR (CI 95%) | p |
|---|---|---|---|---|---|---|
| All patients | 48/221 (21.7%) | 84.9 ± 2.6 | ||||
| Gender | ||||||
| female | 26/128 (20.3%) | 0.621 | 85.8 ± 3.3 | 0.756 | 1 | 0.756 |
| male | 22/93 (23.7%) | 83.9 ± 4.1 | 1.12 (0.56–2.23) | |||
| Age (years) | ||||||
| ≤60 | 25/126 (19.8%) | 0.51 | 86.2 ± 3.2 | 0.235 | 1 | 0.239 |
| >60 | 23/95 (24.2%) | 81.9 ± 4.8 | 1.52 (0.76–3.02) | |||
| Smoking | ||||||
| never | 4/33 (12.1%) | 0.0004 | 90.6 ± 5.2 | 0.004 | 1 | 0.009 |
| past and present | 35/73 (48%) | 63.4 ± 6.5 | 4.93 (1.48–16.38) | |||
| unknown | 9/115 (7.8%) | |||||
| Lesion site * | ||||||
| tongue | 14/60 (23.3%) | 0.003 | 82.6 ± 5.4 | 0.007 | 2.89 (0.90–9.20) | 0.003 |
| sublingual | 6/24 (25%) | 76.7 ± 9.2 | 3.67 (0.98–13.66) | |||
| palate | 3/8 (37.5%) | 71.4 ± 17.1 | 5.00 (0.92–27.35) | |||
| buccal | 6/60 (10%) | 96.5 ± 2.4 | 1 | |||
| gingiva | 6/13 (46.1%) | 52.4 ± 15.7 | 7.17 (1.93–26.74) | |||
| lips | 0/27 (0%) | 100 | 0 | |||
| oropharyngeal | 4/10 (40%) | 75.0 ± 15.3 | 4.24 (0.78–23.13) | |||
| multifocal | 9/19 (47.4%) | 73.3 ± 11.4 | 5.47 (1.47–20.39) | |||
| Lesion type | ||||||
| homogenous | 37/203 (18.2%) | 0.0002 | 87.0 ± 2.6 | <0.0001 | 1 | 0.001 |
| non-homogenous | 11/18 (61.1%) | 53.8 ± 13.8 | 4.57 (1.88–11.13) | |||
| Biopsy | ||||||
| no | 3/77 (3.9%) | <0.0001 | 96.9 ± 2.2 | <0.0001 | 1 | <0.0001 |
| yes | 45/144 (31.3%) | 77.9 ± 3.8 | 6.60 (2.01–21.63) | |||
| Histology | ||||||
| no dysplasia | 4/79 (5.1%) | <0.0001 | 96.1 ± 2.2 | <0.0001 | 1 | <0.0001 |
| grade I dysplasia | 4/25 (16%) | 88.0 ± 6.5 | 3.43 (0.86–13.75) | |||
| grade II dysplasia | 12/15 (80%) | 22.2 ± 12.2 | 40.71 (11.91–139.11) | |||
| grade III dysplasia | 10/10 (100%) | 0 | 54.33 (15.15–194.84) | |||
| in situ cancer | 4 | |||||
| invasive cancer | 11 | |||||
| Dysplasia | ||||||
| no | 4/79 (5.1%) | <0.0001 | 96.1 ± 2.2 | <0.0001 | 1 | <0.0001 |
| yes | 26/50 (52%) | 50.0 ± 7.4 | 13.79 (4.79–39.72) | |||
| Dysplasia | ||||||
| low grade (I) | 4/25 (16%) | <0.0001 | 88.0 ± 6.5 | <0.0001 | 1 | <0.0001 |
| high grade (II, III) | 22/25 (88%) | 11.3 ± 7.1 | 14.63 (4.28–50.03) |
| Characteristic | Multivariate Cox HR (CI 95%) | p |
|---|---|---|
| Dysplasia | ||
| no | 1 | <0.0001 |
| low grade (I) | 2.47 (0.41–15.03) | |
| high grade (II, III) | 18.19 (4.71–70.25) | |
| Lesion type | ||
| homogenous | 1 | 0.063 |
| non-homogenous | 2.79 (0.95–8.24) | |
| Smoking | ||
| never | 1 | 0.098 |
| past and present | 3.51 (0.79–15.51) |
| Characteristic | Malignant Events n (%) | p |
|---|---|---|
| All patients | 16/32 (50%) | |
| Gender | ||
| female | 3/10 (30%) | 0.252 |
| male | 13/22 (59.1%) | |
| Age (years) | ||
| ≤60 | 13/26 (50%) | >0.999 |
| >60 | 3/6 (50%) | |
| Smoking | ||
| never | 1/1 (100%) | >0.999 |
| past and present | 12/23 (52.2%) | |
| unknown | 3/8 (37.5%) | |
| Site | ||
| unilateral | 9/20 (45%) | 0.717 |
| bilateral | 7/12 (58.3%) | |
| Lesion type | ||
| homogenous | 16/32 (50%) | >0.999 |
| non-homogenous | 0/0 | |
| Biopsy | ||
| no | 1/6 (16.7%) | 0.172 |
| yes | 15/26 (57.7%) | |
| Histology | ||
| in situ cancer | 1 | |
| invasive cancer | 1 | |
| Dysplasia | ||
| no | 1/9 (11.1%) | 0.002 |
| yes | 12/15 (80%) | |
| Dysplasia | ||
| low grade (I) | 3/4 (75%) | >0.999 |
| high grade (II, III) | 9/11 (81.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bukovszky, B.; Fodor, J.; Tóth, E.; Kocsis, Z.S.; Oberna, F.; Ferenczi, Ö.; Polgár, C. Malignant Transformation and Long-Term Outcome of Oral and Laryngeal Leukoplakia. J. Clin. Med. 2023, 12, 4255. https://doi.org/10.3390/jcm12134255
Bukovszky B, Fodor J, Tóth E, Kocsis ZS, Oberna F, Ferenczi Ö, Polgár C. Malignant Transformation and Long-Term Outcome of Oral and Laryngeal Leukoplakia. Journal of Clinical Medicine. 2023; 12(13):4255. https://doi.org/10.3390/jcm12134255
Chicago/Turabian StyleBukovszky, Botond, János Fodor, Erika Tóth, Zsuzsa S. Kocsis, Ferenc Oberna, Örs Ferenczi, and Csaba Polgár. 2023. "Malignant Transformation and Long-Term Outcome of Oral and Laryngeal Leukoplakia" Journal of Clinical Medicine 12, no. 13: 4255. https://doi.org/10.3390/jcm12134255
APA StyleBukovszky, B., Fodor, J., Tóth, E., Kocsis, Z. S., Oberna, F., Ferenczi, Ö., & Polgár, C. (2023). Malignant Transformation and Long-Term Outcome of Oral and Laryngeal Leukoplakia. Journal of Clinical Medicine, 12(13), 4255. https://doi.org/10.3390/jcm12134255






