Matched-Pair Analysis: Large-Sized Defects in Surgery of Lower Limb Nonunions
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Matching
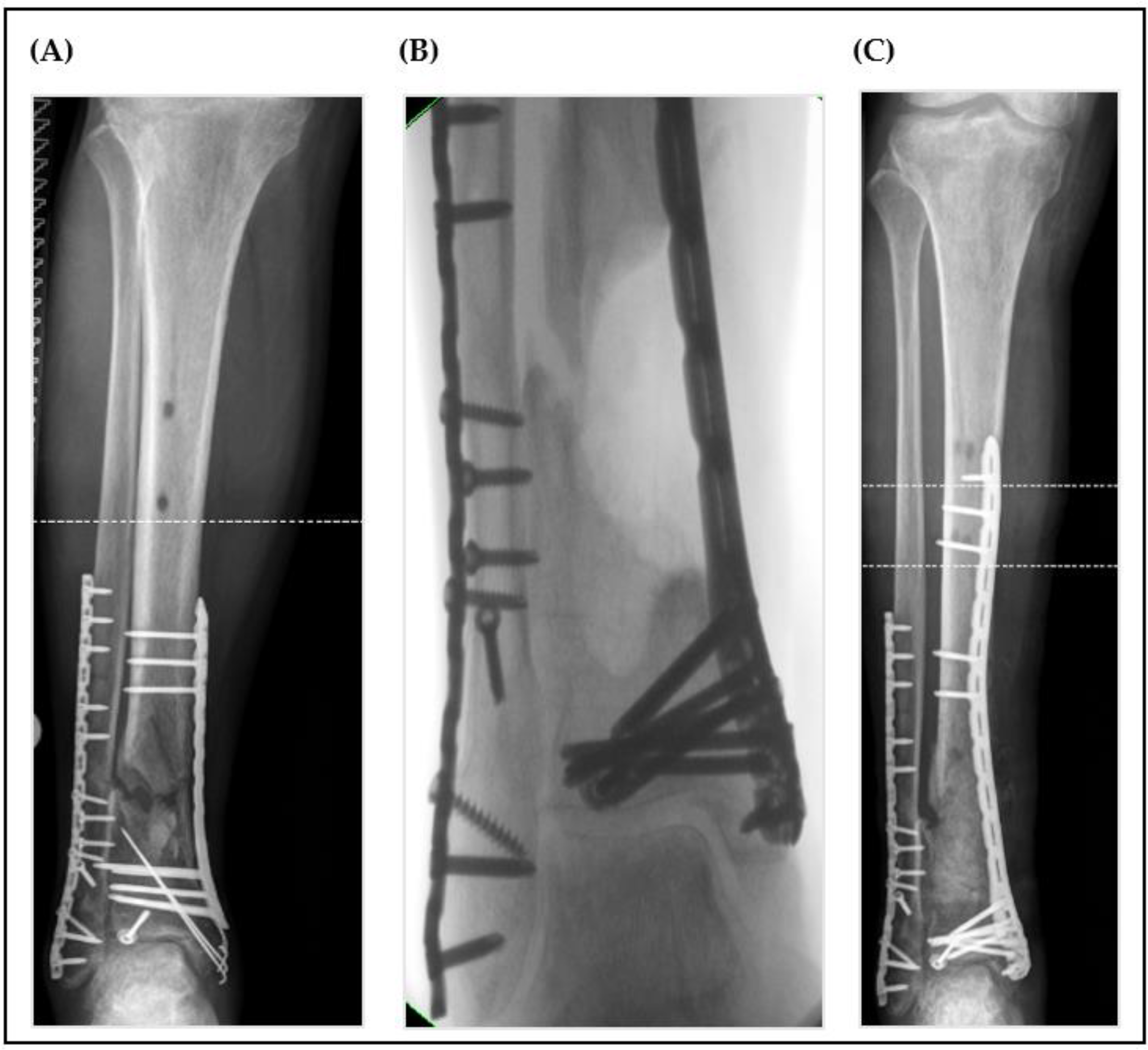
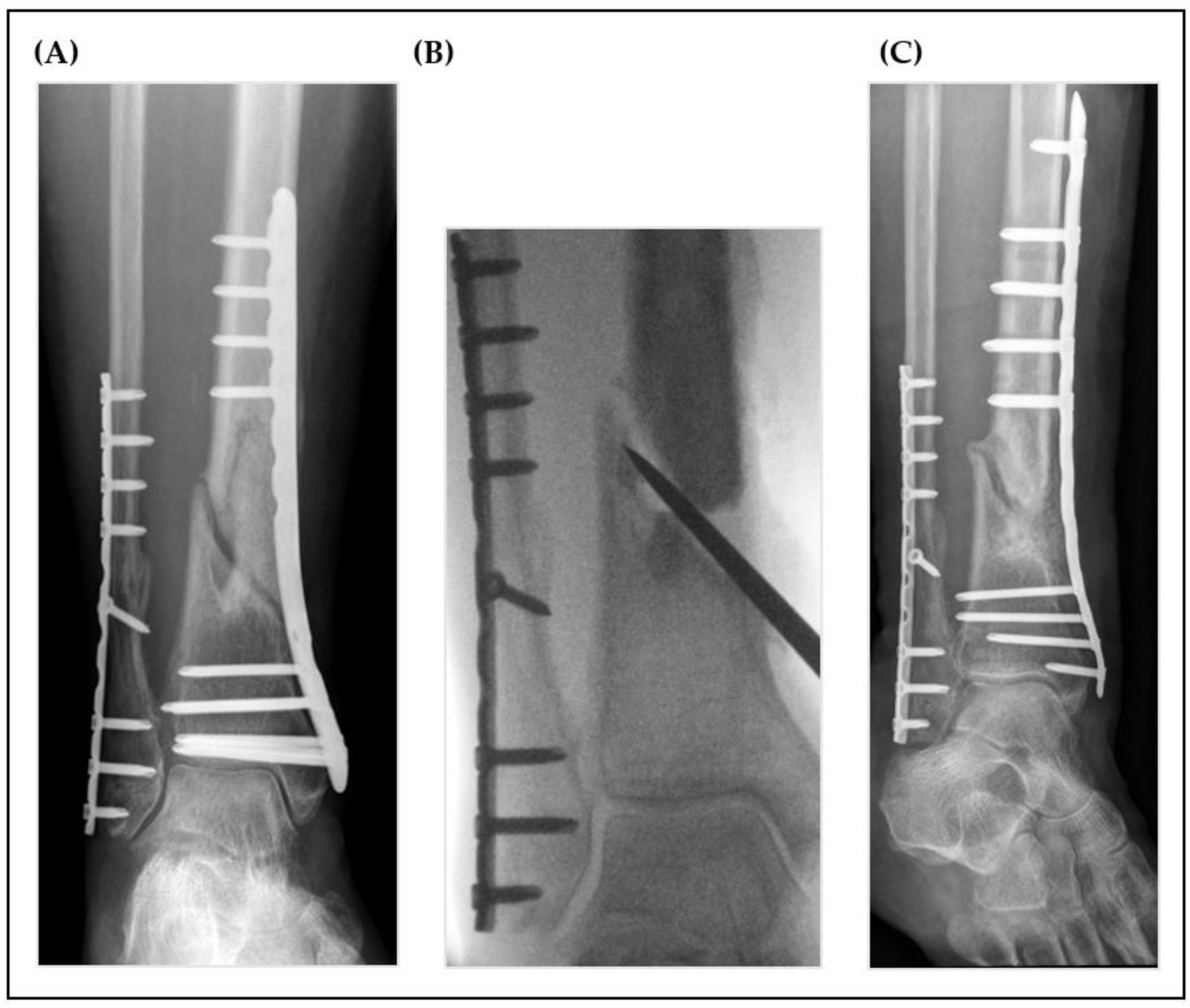
2.3. Surgical Technique
2.4. Postoperative Care and Determination of Outcome
2.5. Statistics
3. Results
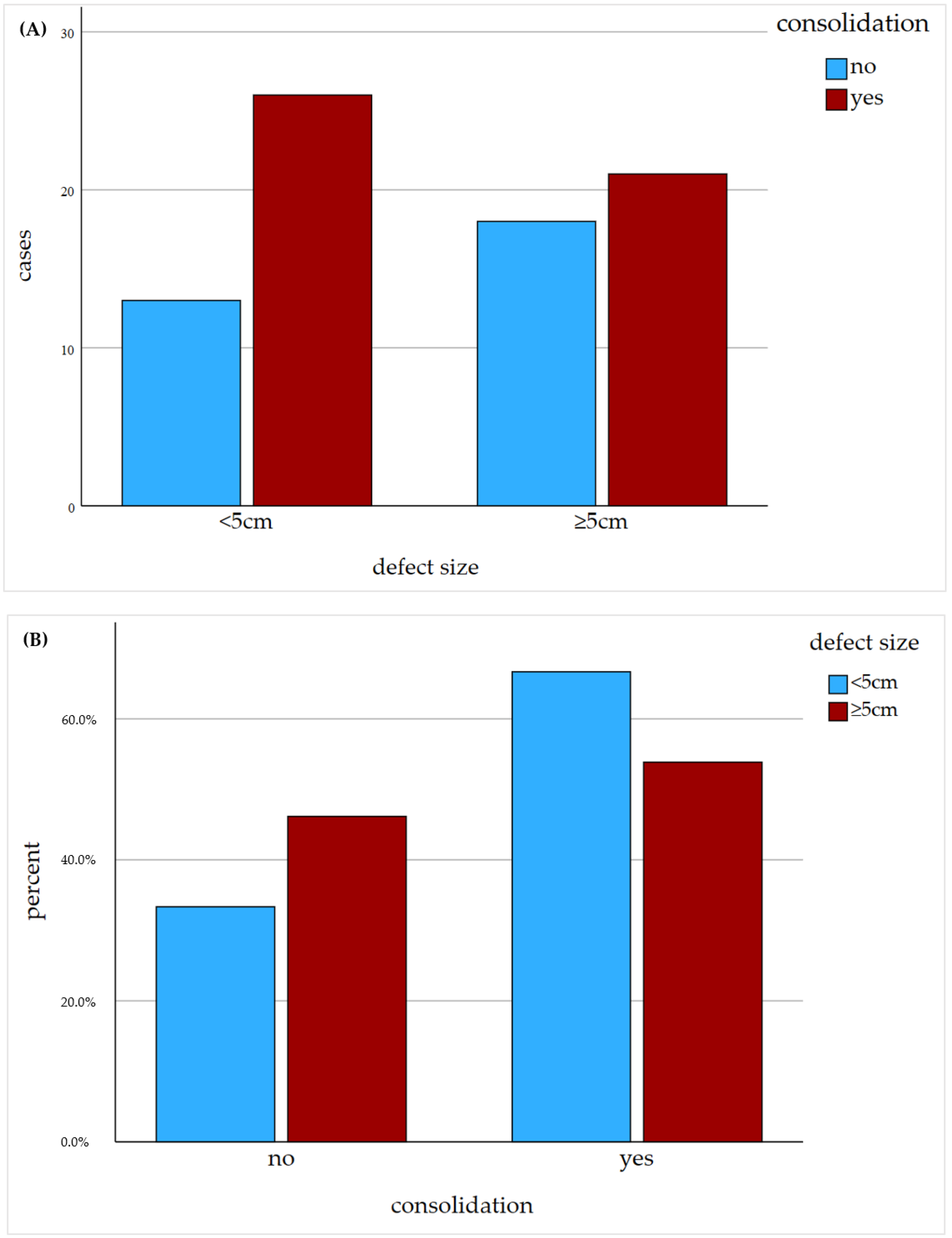
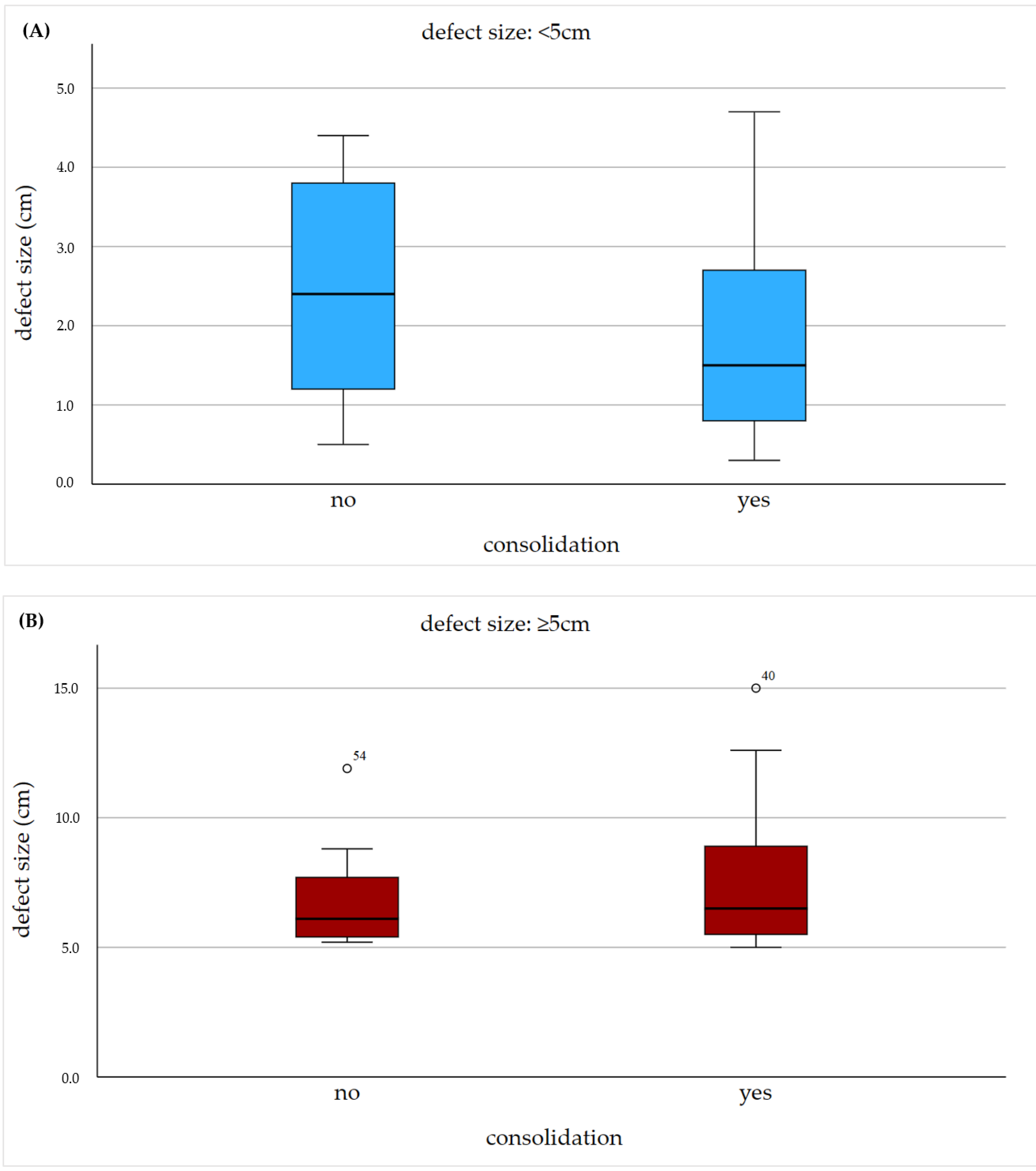
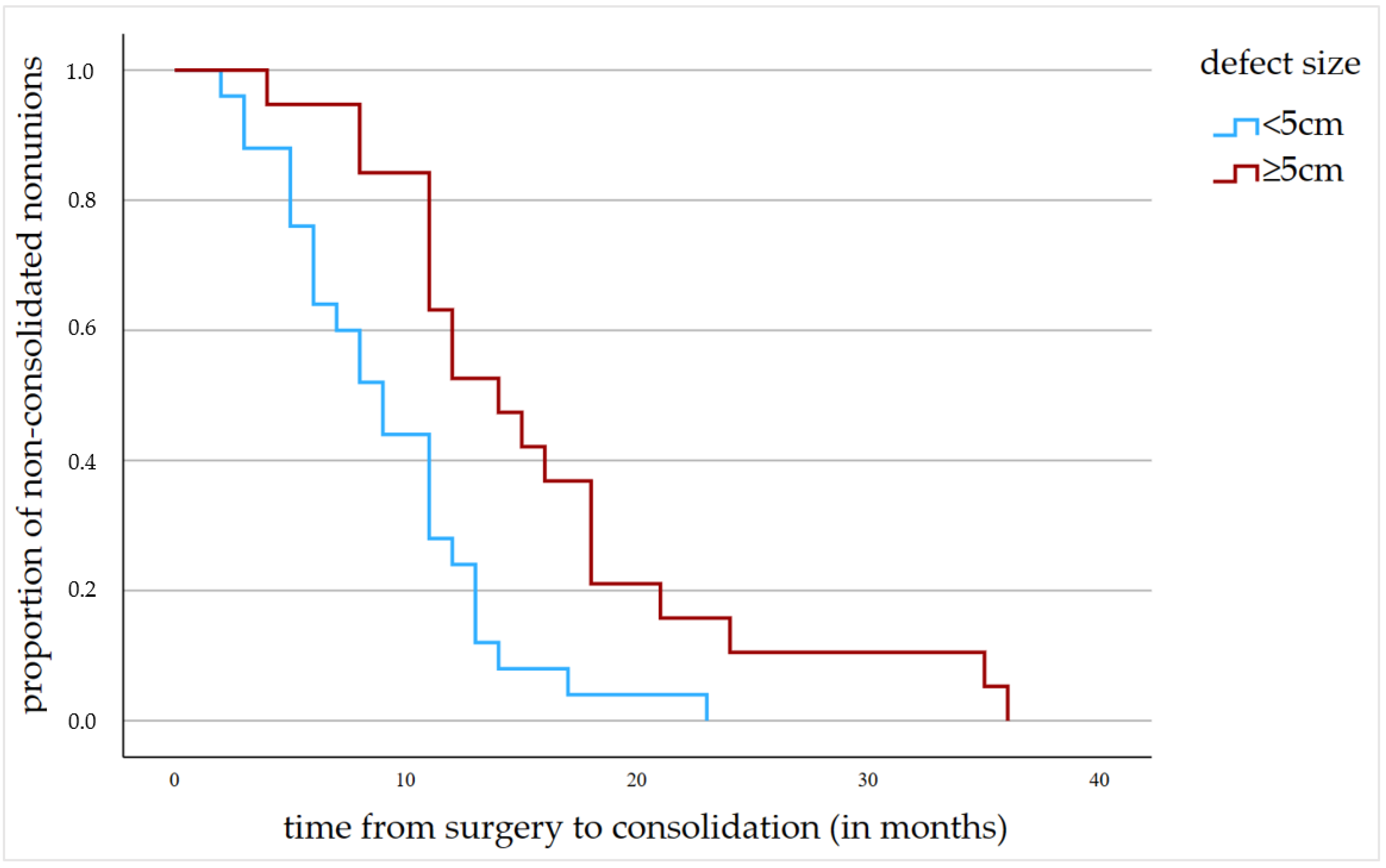
3.1. Radiological and Clinical Nonunion Therapy Outcome
3.2. Influence of Common Risk Factors on Nonunion Therapy Outcome
3.3. Influence of Therapy Modality
4. Discussion
4.1. Impact of Defect Size on Radiological Outcome of Nonunion Therapy
4.2. Influence of Common Risk Factors on the Radiological Outcome
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hernandez, R.K.; Do, T.P.; Critchlow, C.W.; Dent, R.E.; Jick, S.S. Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop. 2012, 83, 653–660. [Google Scholar] [CrossRef]
- Everding, J.; Roßlenbroich, S.; Raschke, M.J. Pseudarthroses of the long bones. Chirurg 2018, 89, 73–88. [Google Scholar] [CrossRef] [PubMed]
- Mills, L.A.; Aitken, S.A.; Simpson, A.H.R.W. The risk of non-union per fracture: Current myths and revised figures from a population of over 4 million adults. Acta Orthop. 2017, 88, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Reeh, F.M.; Sachse, S.; Wedekind, L.; Hofmann, G.O.; Lenz, M. Nonunions and Their Operative Treatment–A DRG-Based Epidemiological Analysis for the Years 2007–2019 in Germany. Dtsch. Arztebl. Int. 2022, 119, 869. [Google Scholar]
- Braun, B.J.; Menger, M.M.; Reumann, M.K.; Histing, T. Pseudarthrosen beim Erwachsenen—Ein Update. Orthop. Unf. Up2date 2022, 17, 537–558. [Google Scholar] [CrossRef]
- Nicholson, J.; Makaram, N.; Simpson, A.; Keating, J. Fracture nonunion in long bones: A literature review of risk factors and surgical management. Injury 2020, 52 (Suppl. 2), S3–S11. [Google Scholar] [CrossRef]
- Zura, R.; Mehta, S.; Della Rocca, G.J.; Steen, R.G. Biological Risk Factors for Nonunion of Bone Fracture. JBJS Rev. 2016, 4, e5. [Google Scholar] [CrossRef]
- Moghaddam, A.; Zimmermann, G.; Hammer, K.; Bruckner, T.; Grützner, P.A.; von Recum, J. Cigarette smoking influences the clinical and occupational outcome of patients with tibial shaft fractures. Injury 2011, 42, 1435–1442. [Google Scholar] [CrossRef]
- Audigé, L.; Griffin, D.; Bhandari, M.; Kellam, J.; Rüedi, T.P. Path Analysis of Factors for Delayed Healing and Nonunion in 416 Operatively Treated Tibial Shaft Fractures. Clin. Orthop. Relat. Res. 2005, 438, 221–232. [Google Scholar] [CrossRef]
- Lindsey, R.W.; Gugala, Z.; Milne, E.; Sun, M.; Gannon, F.H.; Latta, L.L. The efficacy of cylindrical titanium mesh cage for the reconstruction of a critical-size canine segmental femoral diaphyseal defect. J. Orthop. Res. 2006, 24, 1438–1453. [Google Scholar] [CrossRef]
- Haines, N.M.; Lack, W.D.; Seymour, R.B.; Bosse, M.J. Defining the Lower Limit of a “Critical Bone Defect” in Open Diaphyseal Tibial Fractures. J. Orthop. Trauma 2016, 30, e158–e163. [Google Scholar] [CrossRef] [PubMed]
- Hak, D.J.; Fitzpatrick, D.; Bishop, J.A.; Marsh, J.L.; Tilp, S.; Schnettler, R.; Simpson, H.; Alt, V. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014, 45 (Suppl. 2), S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Norris, B.L.; Vanderkarr, M.; Sparks, C.; Chitnis, A.S.; Ray, B.; Holy, C.E. Treatments, cost and healthcare utilization of patients with segmental bone defects. Injury 2021, 52, 2935–2940. [Google Scholar] [CrossRef]
- Moghaddam, A.; Zietzschmann, S.; Bruckner, T.; Schmidmaier, G. Treatment of atrophic tibia non-unions according to ‘diamond concept’: Results of one- and two-step treatment. Injury 2015, 46 (Suppl. 4), S39–S50. [Google Scholar] [CrossRef]
- Wang, P.; Wu, Y.; Rui, Y.; Wang, J.; Liu, J.; Ma, Y. Masquelet technique for reconstructing bone defects in open lower limb fracture: Analysis of the relationship between bone defect and bone graft. Injury 2020, 52, 988–995. [Google Scholar] [CrossRef]
- Tanner, M.C.; Heller, R.; Westhauser, F.; Miska, M.; Ferbert, T.; Fischer, C.; Gantz, S.; Schmidmaier, G.; Haubruck, P. Evaluation of the clinical effectiveness of bioactive glass (S53P4) in the treatment of non-unions of the tibia and femur: Study protocol of a randomized controlled non-inferiority trial. Trials 2018, 19, 299. [Google Scholar] [CrossRef]
- Chmell, M.J.; McAndrew, M.P.; Thomas, R.; Schwartz, H.S. Structural Allografts for Reconstruction of Lower Extremity Open Fractures with 10 Centimeters or More of Acute Segmental Defects. J. Orthop. Trauma 1995, 9, 222–226. [Google Scholar] [CrossRef]
- Bumbasirevic, M.; Stevanovic, M.; Bumbasirevic, V.; Lesic, A.; Atkinson, H.D.E. Free vascularised fibular grafts in orthopaedics. Int. Orthop. 2014, 38, 1277–1282. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Crimì, A.; Fantoni, I.; Vigo, M.; Iacobellis, C.; Ruggieri, P. Functional outcome and complications after treatment of comminuted tibial fractures or deformities using Ilizarov bone transport: A single-center study at 15- to 30-year follow-up. Arch. Orthop. Trauma Surg. 2020, 141, 1825–1833. [Google Scholar] [CrossRef]
- Moghaddam, A.; Thaler, B.; Bruckner, T.; Tanner, M.; Schmidmaier, G. Treatment of atrophic femoral non-unions according to the diamond concept: Results of one- and two-step surgical procedure. J. Orthop. 2017, 14, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Tanner, M.C.; Hagelskamp, S.; Vlachopoulos, W.; Miska, M.; Findeisen, S.; Grimm, A.; Schmidmaier, G.; Haubruck, P. Non-Union Treatment Based on the “Diamond Concept” Is a Clinically Effective and Safe Treatment Option in Older Adults. Clin. Interv. Aging 2020, 15, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Einhorn, T.A.; Marsh, D. Fracture healing: The diamond concept. Injury 2007, 38 (Suppl. 4), S3–S6. [Google Scholar] [CrossRef]
- Schmidmaier, G.; Moghaddam, A. Long Bone Nonunion. Z. Orthop. Unfall. 2015, 153, 659–674, quiz 75–76. [Google Scholar] [PubMed]
- Karger, C.; Kishi, T.; Schneider, L.; Fitoussi, F.; Masquelet, A.-C. Treatment of posttraumatic bone defects by the induced membrane technique. Orthop. Traumatol. Surg. Res. 2012, 98, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Masquelet, A.-C.; Fitoussi, F.; Begue, T.; Muller, G.P. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann. Chir. Plast. Esthet. 2000, 45, 346–353. [Google Scholar] [PubMed]
- Hackett, N.J.; De Oliveira, G.S.; Jain, U.K.; Kim, J.Y. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int. J. Surg. 2015, 18, 184–190. [Google Scholar] [CrossRef]
- Helbig, L.; Bechberger, M.; Aldeeri, R.; Ivanova, A.; Haubruck, P.; Miska, M.; Schmidmaier, G.; Omlor, G.W. Initial peri- and postoperative antibiotic treatment of infected nonunions: Results from 212 consecutive patients after mean follow-up of 34 months. Ther. Clin. Risk Manag. 2018, 14, 59–67. [Google Scholar] [CrossRef]
- Hsu, C.-A.; Chen, S.-H.; Chan, S.-Y.; Yu, Y.-H. The Induced Membrane Technique for the Management of Segmental Tibial Defect or Nonunion: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2020, 2020, 5893642. [Google Scholar] [CrossRef]
- Fung, B.; Hoit, G.; Schemitsch, E.; Godbout, C.; Nauth, A. The induced membrane technique for the management of long bone defects. Bone Jt. J. 2020, 102-B, 1723–1734. [Google Scholar] [CrossRef]
- Sun, S.H.; Tsai, W.W.; Shiu, S.I.; Chen, C.H. Induced membrane technique for large bone defects: A systematic review and individual participant data meta-analysis. Medicine 2022, 101, e29292. [Google Scholar] [CrossRef]
- El-Alfy, B.S.; Ali, A.M. Management of segmental skeletal defects by the induced membrane technique. Indian J. Orthop. 2015, 49, 643–648. [Google Scholar] [CrossRef]
- Aktuglu, K.; Erol, K.; Vahabi, A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: A narrative review. J. Orthop. Traumatol. 2019, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Maceroli, M.A.; Gage, M.J.; Wise, B.T.; Connelly, D.; Ordonio, K.; Castillo, R.C.; Jarman, M.; Nascone, J.W.; O’Toole, R.V.; Sciadini, M.F. Risk Factors for Failure of Bone Grafting of Tibia Nonunions and Segmental Bone Defects: A New Preoperative Risk Assessment Score. J. Orthop. Trauma 2017, 31, S55–S59. [Google Scholar] [CrossRef] [PubMed]
- Tanner, M.; Vlachopoulos, W.; Findeisen, S.; Miska, M.; Ober, J.; Hagelskamp, S.; Schmidmaier, G.; Haubruck, P. Does Age Influence the Outcome of Lower Limb Non-Union Treatment? A Matched Pair Analysis. J. Clin. Med. 2019, 8, 1276. [Google Scholar] [CrossRef] [PubMed]
- Tanner, M.C.; Heller, R.A.; Grimm, A.; Zimmermann, S.; Pilz, M.; Jurytko, L.; Miska, M.; Helbig, L.; Schmidmaier, G.; Haubruck, P. The Influence of an Occult Infection on the Outcome of Autologous Bone Grafting During Surgical Bone Reconstruction: A Large Single-Center Case-Control Study. J. Inflamm. Res. 2021, 14, 995–1005. [Google Scholar] [CrossRef]

| Characteristic | Group * | |
|---|---|---|
| Bone Defect ≥5 cm (n = 39) | Bone Defect <5 cm (n = 39) | |
| Age (years) | 52.28 (±12) | 52.33 (±12) |
| Defect size (cm) | 7.13 (±2.3) | 2.09 (±1.34) |
| ASA score | 1.85 (±0.630) | 2.10 (±0.502) |
| Sex | ||
| Male | 24 (61%) | 24 (61%) |
| Female | 15 (39%) | 15 (39%) |
| Affected long bone and localisation | ||
| Femur proximal | 0 (0%) | 0 (0%) |
| Femur diaphyseal | 8 (20.5%) | 8 (20.5%) |
| Femur distal | 7 (17.9%) | 7 (17.9%) |
| Tibia proximal | 3 (7.7%) | 3 (7.7%) |
| Tibia diaphyseal | 7 (17.9%) | 7 (17.9%) |
| Tibia distal | 14 (35.9%) | 14 (35.9%) |
| Nonunion treatment | ||
| One-step | 3 (7.7%) | 3 (7.7%) |
| Two-step | 36 (92.3%) | 36 (92.3%) |
| Smoking status | ||
| Yes | 10 (25.6%) | 10 (25.6%) |
| No | 25 (64.1%) | 25 (64.1%) |
| Previous | 4 (10.3%) | 4 (10.3%) |
| Infection | ||
| Yes | 19 (48.7%) | 19 (48.7%) |
| No | 20 (51.3%) | 20 (51.3%) |
| Type of nonunion | ||
| Atrophic | 38 (97.4%) | 38 (97.4%) |
| Hypertrophic | 1 (2.6%) | 1 (2.6%) |
| Type of fracture | ||
| Closed | 19 (48.7%) | 27 (69.2%) |
| Open | 20 (51.3%) | 12 (30.8%) |
| Bone morphogenetic protein used | ||
| rhBMP-2 | 7 (17.9%) | 6 (15.4%) |
| rhBMP-7 | 17 (43.6%) | 22 (56.4%) |
| None | 15 (38.5%) | 11 (28.2%) |
| Autologous bone graft used | ||
| RIA (femur) | 31 (79.5%) | 27 (69.2%) |
| RIA (tibia) | 2 (5.1%) | 3 (7.7%) |
| RIA + iliac crest | 2 (5.1%) | 3 (7.7%) |
| Iliac crest | 2 (5.1%) | 4 (10.3%) |
| None | 2 (5.1%) | 2 (5.1%) |
| Bone substitute | ||
| Vitoss | 23 (59%) | 28 (71.8%) |
| Vitoss-BA | 4 (10.3%) | 4 (10.3%) |
| Bioglass | 6 (15.4%) | 1 (2.6%) |
| None | 6 (15.4%) | 6 (15.4%) |
| Alcohol abuse | ||
| Yes | 7 (17.9%) | 4 (10.3%) |
| No | 32 (82.1%) | 35 (89.7%) |
| Drug abuse | ||
| Yes | 2 (5.1%) | 3 (7.7%) |
| No | 37 (94.9%) | 36 (92.3%) |
| Medication intake | ||
| NSAID | 10 (25.6%) | 21 (53.8%) |
| NSAID + steroid | 0 (0%) | 1 (2.6%) |
| Steroid | 1 (2.6%) | 2 (5.1%) |
| None | 28 (71.8%) | 15 (38.5%) |
| Diabetes mellitus | ||
| Yes | 6 (15.4%) | 5 (12.8%) |
| No | 33 (84.6%) | 34 (87.2%) |
| Method of osteosynthesis | ||
| Nail | 16 (41%) | 17 (43.6%) |
| Plate | 23 (59%) | 21 (53.8%) |
| Screws | 0 (0%) | 1 (2.6%) |
| Consolidation | ||
| Yes | 21 (53.8%) | 26 (66.7%) |
| No | 18 (46.2%) | 13 (33.3%) |
| Characteristic | Group | |
|---|---|---|
| Bone Defect ≥5 cm (n = 18) | Bone Defect <5 cm (n = 13) | |
| Age (years) | 50.5 (±11.9) | 51.46 (±11.7) |
| Defect size (cm) | 6.73 (±1.8) | 2.55 (±1.4) |
| Sex | ||
| Male | 11 (61.1%) | 10 (76.9%) |
| Female | 7 (38.9%) | 3 (23.1%) |
| Affected long bone and localisation | ||
| Thigh proximal | 0 (0%) | 0 (0%) |
| Thigh diaphyseal | 4 (22.2%) | 3 (23.1%) |
| Thigh distal | 3 (16.7%) | 1 (7.7%) |
| Tibia proximal | 0 (0%) | 0 (0%) |
| Tibia diaphyseal | 4 (22.2%) | 3 (23.1%) |
| Tibia distal | 7 (38.9%) | 6 (46.2%) |
| Nonunion treatment | ||
| One-step | 2 (11.1%) | 1 (7.7%) |
| Two-step | 16 (88.9%) | 12 (92.3%) |
| Smoking status | ||
| Yes | 4 (22.2%) | 4 (30.8%) |
| No | 10 (55.6%) | 7 (53.8%) |
| Previous | 4 (22.2%) | 2 (15.4%) |
| Infection | ||
| Yes | 10 (56.6%) | 9 (69.2%) |
| No | 8 (43.4%) | 4 (30.8%) |
| Type of nonunion | ||
| Atrophic | 17 (94.4%) | 13 (100%) |
| Hypertrophic | 1 (5.6%) | 0 (0%) |
| Type of fracture | ||
| Closed | 7 (38.9%) | 9 (69.2%) |
| Open | 11 (61.1%) | 4 (30.8%) |
| Bone morphogenetic protein used | ||
| rhBMP-2 | 2 (11.1%) | 0 (0%) |
| rhBMP-7 | 8 (44.4%) | 9 (69.2%) |
| None | 8 (44.4%) | 4 (30.8%) |
| Autologous bone graft used | ||
| RIA (femur) | 15 (83.3%) | 10 (76.9%) |
| RIA (tibia) | 2 (11.1%) | 1 (7.7%) |
| RIA + iliac crest | 1 (5.6%) | 1 (7.7%) |
| Iliac crest | 0 (0%) | 1 (7.7%) |
| None | 0 (0%) | 0 (0%) |
| Bone substitute | ||
| Vitoss | 11 (61.1%) | 10 (76.9%) |
| Vitoss-BA | 2 (11.1%) | 2 (15.4%) |
| Bioglass | 2 (11.1%) | 0 (0%) |
| None | 3 (16.7%) | 1 (7.7%) |
| Alcohol abuse | ||
| Yes | 3 (16.7%) | 0 (0%) |
| No | 15 (83.3%) | 13 (100%) |
| Drug abuse | ||
| Yes | 1 (5.6%) | 0 (0%) |
| No | 17 (94.4%) | 13 (100%) |
| Medication intake | ||
| NSAID | 7 (38.9%) | 6 (46.2%) |
| Steroid | 1 (5.6%) | 1 (7.7%) |
| None | 10 (55.6%) | 6 (46.2%) |
| Diabetes mellitus | ||
| Yes | 4 (22.2%) | 3 (23.1%) |
| No | 14 (77.8%) | 10 (76.9%) |
| Method of osteosynthesis | ||
| Nail | 6 (33.3%) | 6 (46.2%) |
| Plate | 12 (66.7%) | 7 (53.8%) |
| Screws | 0 (0%) | 0 (0%) |
| Variable | b | SD | p | OR | 95% CI | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Radiological and Clinical Nonunion Therapy Outcome | ||||||
| Defect size (cm) | −0.062 | 0.074 | 0.399 | 0.940 | 0.813 | 1.086 |
| Previous surgeries | −0.109 | 0.05 | 0.028 * | 0.896 | 0.813 | 0.988 |
| Revisions | −0.905 | 0.248 | <0.001 * | 0.404 | 0.249 | 0.658 |
| Revisions (SG) | −2.721 | 0.901 | 0.003 * | 0.66 | 0.11 | 0.385 |
| Total surgeries | −0.191 | 0.061 | 0.002 * | 0.826 | 0.734 | 0.930 |
| Full weight bearing | −0.062 | 0.092 | 0.498 | 0.940 | 0.784 | 1.125 |
| Influence of Common Risk Factors on Nonunion Therapy Outcome | ||||||
| Previous smoking | −1.762 | 0.869 | 0.043 * | 0.172 | 0.031 | 0.944 |
| Active smoking | −0.258 | 0.545 | 0.636 | 0.773 | 0.265 | 2.250 |
| Nonsmoking | 0.258 | 0.545 | 0.636 | 1.249 | 0.444 | 3.769 |
| Presence of diabetes | −1.143 | 0.677 | 0.091 | 0.319 | 0.85 | 1.201 |
| Presence of infection | −0.847 | 0.474 | 0.074 | 0.429 | 0.169 | 1.084 |
| BMI (SG) | −0.150 | 0.08 | 0.061 | 0.861 | 0.736 | 1.007 |
| NSAID intake (SG) | −1.435 | 0.795 | 0.071 | 0.238 | 0.050 | 1.131 |
| Influence of Therapy Modality | ||||||
| Use of BMP2 | 1.489 | 0.808 | 0.066 | 4.431 | 0.909 | 21.597 |
| Use of BMP7 | −0.322 | 0.464 | 0.488 | 0.725 | 0.292 | 1.801 |
| Type of procedure | 0.452 | 0.852 | 0.596 | 1.571 | 0.296 | 8.339 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Findeisen, S.; Schwilk, M.; Haubruck, P.; Ferbert, T.; Helbig, L.; Miska, M.; Schmidmaier, G.; Tanner, M.C. Matched-Pair Analysis: Large-Sized Defects in Surgery of Lower Limb Nonunions. J. Clin. Med. 2023, 12, 4239. https://doi.org/10.3390/jcm12134239
Findeisen S, Schwilk M, Haubruck P, Ferbert T, Helbig L, Miska M, Schmidmaier G, Tanner MC. Matched-Pair Analysis: Large-Sized Defects in Surgery of Lower Limb Nonunions. Journal of Clinical Medicine. 2023; 12(13):4239. https://doi.org/10.3390/jcm12134239
Chicago/Turabian StyleFindeisen, Sebastian, Melanie Schwilk, Patrick Haubruck, Thomas Ferbert, Lars Helbig, Matthias Miska, Gerhard Schmidmaier, and Michael Christopher Tanner. 2023. "Matched-Pair Analysis: Large-Sized Defects in Surgery of Lower Limb Nonunions" Journal of Clinical Medicine 12, no. 13: 4239. https://doi.org/10.3390/jcm12134239
APA StyleFindeisen, S., Schwilk, M., Haubruck, P., Ferbert, T., Helbig, L., Miska, M., Schmidmaier, G., & Tanner, M. C. (2023). Matched-Pair Analysis: Large-Sized Defects in Surgery of Lower Limb Nonunions. Journal of Clinical Medicine, 12(13), 4239. https://doi.org/10.3390/jcm12134239







