Prevalence of Migraine Disease in Electrohypersensitive Patients
Abstract
:1. Background
2. Methods
2.1. Study Design and Population
2.2. Collected Data
- family history: allergy, food intolerance, asthma, epilepsy, migraines, intolerance to noise, light, smells or vibrations, fibromyalgia, electro-sensitivity and multiple chemical sensitivity (MCS),
- personal history included the same items as well as a history of head trauma and dental care with amalgam placement,
- characteristics of the pathology included the year of the symptoms onset, sources of electromagnetic radiation involved, triggering factor, medical diagnosis, existence of a file at the Departmental House for the Disabled and recognition as a disabled worker,
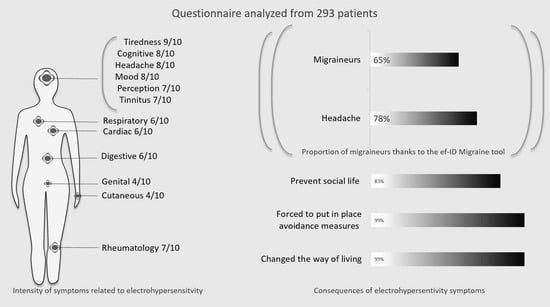
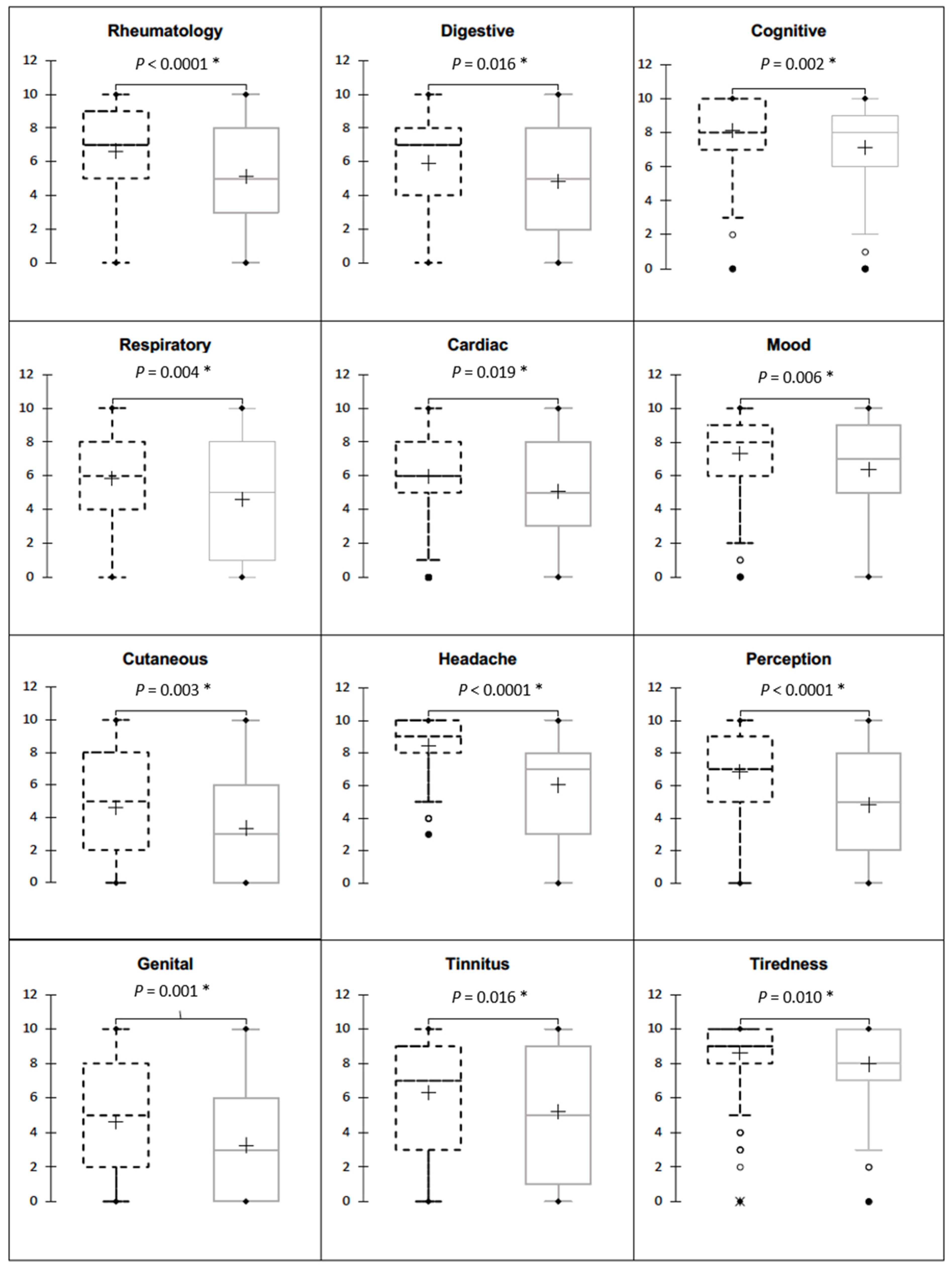
- EHS symptoms, evaluated from 0 (no symptom) to 10 (very intense and disabling symptoms) in twelve categories. Rheumatology symptoms included pain, cramps and stiffness or weakness of muscles or joints. Digestive symptoms included abdominal pain or cramps, bloating, nausea, diarrhea or constipation. Cognitive symptoms included difficulty in concentrating, memory problems, feeling of disconnection, lack of words or difficulty in making decisions. Respiratory symptoms included irritation of the eyes, shortness of breath, chest tightness or cough. Cardiac symptoms included accelerated or irregular heartbeat, extrasystoles palpitations or discomfort in the chest. Feeling tense or nervousness, irritability, depression, crying or angry outbursts or disinterest in activities that usually motivate were in the mood category. Rash, hives or dry skin concerned cutaneous. Headache symptoms included headaches or feeling of a heavy head or congested face. Perception symptoms included balance disorder or coordination disorder, numbness or tingling in extremities or blurred visual blur. Genital symptoms included pelvic pain or frequent urination. Tinnitus was defined by the sentence “noises in the ears”. Tiredness symptoms corresponded to fatigue or sleep disorders.
- medical treatments ongoing,
- classification of the symptoms’ impact on daily life defined by our clinical experience: stage 1, the symptoms do not modify daily life; stage 2, the symptoms oblige the patient to implement avoidance measures and stage 3, the symptoms prevent a normal social life,
- the extended French version of thew ID Migraine questionnaire. The ef-ID Migraine is a brief, practical and easy-to-use diagnostic tool for migraines. This self-administered questionnaire composed of four items assesses disabling headaches occurring in the past year associated with nausea or vomiting and/or photophobia and/or prodromal visual signs [14,15]. The association should lead to the consideration of a migraine disease, which should be confirmed by a specialized consultation according to the criteria of the international classification of headaches (ICHD-3) [16].
2.3. Sample Size
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Prague, C.R.; Mild, K.H.; Repacholi, M.H.; van Deventer, E. World Health Organization Electromagnetic hypersensitivity. In Proceedings of the International Workshop on Electromagnetic Field Hypersensitivity, Prague, Czech Republic, 25–27 October 2004; Available online: https://apps.who.int/iris/handle/10665/43435 (accessed on 15 August 2022).
- Hypersensibilité Électromagnétique ou Intolérance Environnementale Idiopathique Attribuée aux Champs Électromagnétiques. 2018. Available online: https://www.anses.fr/fr/content/avis-et-rapport-de-lanses-relatif-à-l’expertise-sur-l’hypersensibilité-electromagnétique-ehs (accessed on 12 June 2023).
- Stein, Y.; Udasin, I.G. Electromagnetic hypersensitivity (EHS, microwave syndrome)—Review of mechanisms. Environ. Res. 2020, 186, 109445. [Google Scholar] [CrossRef]
- Leszczynski, D. Review of the scientific evidence on the individual sensitivity to electromagnetic fields (EHS). Rev. Environ. Health 2021, 37, 423–450. [Google Scholar] [CrossRef]
- Belpomme, D.; Carlo, G.L.; Irigaray, P.; Carpenter, D.O.; Hardell, L.; Kundi, M.; Belyaev, I.; Havas, M.; Adlkofer, F.; Heuser, G.; et al. The Critical Importance of Molecular Biomarkers and Imaging in the Study of Electrohypersensitivity. A Scientific Consensus International Report. Int. J. Mol. Sci. 2021, 22, 7321. [Google Scholar] [CrossRef]
- Dieudonné, M. Electromagnetic hypersensitivity: A critical review of explanatory hypotheses. Environ. Health 2020, 19, 48. [Google Scholar] [CrossRef]
- Belpomme, D.; Irigaray, P. Why the psychogenic or psychosomatic theories for electrohypersensitivity causality should be abandoned, but not the hypothesis of a nocebo-associated symptom formation caused by electromagnetic fields conditioning in some patients. Environ. Res. 2022, 114839, Online ahead of print. [Google Scholar] [CrossRef]
- Rubin, G.J.; Hillert, L.; Nieto-Hernandez, R.; van Rongen, E.; Oftedal, G. Do people with idiopathic environmental intolerance attributed to electromagnetic fields display physiological effects when exposed to electromagnetic fields? A systematic review of provocation studies. Bioelectromagnetics 2011, 32, 593–609. [Google Scholar] [CrossRef]
- Schmiedchen, K.; Driessen, S.; Oftedal, G. Methodological limitations in experimental studies on symptom development in individuals with idiopathic environmental intolerance attributed to electromagnetic fields (IEI-EMF)—A systematic review. Environ. Health 2019, 18, 88. [Google Scholar] [CrossRef] [Green Version]
- Bordarie, J.; Dieudonné, M.; Ledent, M.; Prignot, N. A qualitative approach to experiential knowledge identified in focus groups aimed at co-designing a provocation test in the study of electrohypersensitivity. Ann. Med. 2022, 54, 2362–2374. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Standing Committee to Advise the Department of State on Unexplained Health Effects on U.S. Government Employees and Their Families at Overseas Embassies; Health and Medicine Division; Division on Engineering and Physical Sciences. In An Assessment of Illness in U.S. Government Employees and Their Families at Overseas Embassies; Relman, D.A., Pavlin, J., Eds.; National Academies Press: Washington, DC, USA, 2020; p. 25889. ISBN 978-0-309-68137-7. Available online: https://www.nap.edu/catalog/25889 (accessed on 12 June 2023).
- Chongchitpaisan, W.; Wiwatanadate, P.; Tanprawate, S.; Narkpongphan, A.; Siripon, N. Trigger of a migraine headache among Thai adolescents smartphone users: A time series study. Environ. Anal. Health Toxicol. 2021, 36, e2021006. [Google Scholar] [CrossRef] [PubMed]
- Belpomme, D.; Irigaray, P. Electrohypersensitivity as a Newly Identified and Characterized Neurologic Pathological Disorder: How to Diagnose, Treat, and Prevent It. Int. J. Mol. Sci. 2020, 21, 1915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Streel, S.; Donneau, A.-F.; Dardenne, N.; Hoge, A.; Bruyère, O.; Albert, A.; Guillaume, M.; Schoenen, J. Validation of an extended French version of ID MigraineTM as a migraine-screening tool. Cephalalgia 2015, 35, 437–442. [Google Scholar] [CrossRef] [Green Version]
- Lipton, R.B.; Dodick, D.; Sadovsky, R.; Kolodner, K.; Endicott, J.; Hettiarachchi, J.; Harrison, W. ID Migraine validation study A self-administered screener for migraine in primary care: The ID Migraine validation study. Neurology 2003, 61, 375–382. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Stovner, L.J.; Hagen, K.; Linde, M.; Steiner, T.J. The global prevalence of headache: An update, with analysis of the influences of methodological factors on prevalence estimates. J. Headache Pain 2022, 23, 34. [Google Scholar] [CrossRef]
- Multiple chemical sensitivity: A 1999 consensus. Arch Environ. Health 1999, 54, 147–149. [CrossRef]
- Kacprzyk, A.; Kanclerz, G.; Rokita, E.; Tatoń, G. Which sources of electromagnetic field are of the highest concern for electrosensitive individuals?—Questionnaire study with a literature review. Electromagn. Biol. Med. 2021, 40, 33–40. [Google Scholar] [CrossRef]
- van Dongen, D.; Smid, T.; Timmermans, D.R.M. Symptom attribution and risk perception in individuals with idiopathic environmental intolerance to electromagnetic fields and in the general population. Perspect. Public Health 2014, 134, 160–168. [Google Scholar] [CrossRef]
- Belpomme, D.; Campagnac, C.; Irigaray, P. Reliable disease biomarkers characterizing and identifying electrohypersensitivity and multiple chemical sensitivity as two etiopathogenic aspects of a unique pathological disorder. Rev. Environ. Health 2015, 30, 251–271. [Google Scholar] [CrossRef] [PubMed]
- Toffa, D.H.; Sow, A.D. The enigma of headaches associated with electromagnetic hyperfrequencies: Hypotheses supporting non-psychogenic algogenic processes. Electromagn. Biol. Med. 2020, 39, 196–205. [Google Scholar] [CrossRef] [PubMed]
- A Nationwide Survey of Migraine in France: Prevalence and Clinical Features in Adults—Patrick Henry, Philippe Michel, Bruno Brochet, Jean François Dartigues, Sylvie Tison, Roger Salamon. 1992. Available online: https://journals.sagepub.com/doi/10.1046/j.1468-2982.1992.1204229.x (accessed on 27 June 2022).
- Henry, P.; Auray, J.P.; Gaudin, A.F.; Dartigues, J.F.; Duru, G.; Lantéri-Minet, M.; Lucas, C.; Pradalier, A.; Chazot, G.; El Hasnaoui, A. Prevalence and clinical characteristics of migraine in France. Neurology 2002, 59, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Streel, S.; Donneau, A.-F.; Hoge, A.; Albert, A.; Schoenen, J.; Guillaume, M. One-year prevalence of migraine using a validated extended French version of the ID MigraineTM: A Belgian population-based study. Rev. Neurol. 2015, 171, 707–714. [Google Scholar] [CrossRef]
- Demarquay, G.; Moisset, X.; Lantéri-Minet, M.; de Gaalon, S.; Donnet, A.; Giraud, P.; Guégan-Massardier, E.; Lucas, C.; Mawet, J.; Roos, C.; et al. Revised guidelines of the French Headache Society for the diagnosis and management of migraine in adults. Part 1: Diagnosis and assessment. Rev. Neurol. 2021, 177, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Ducros, A.; de Gaalon, S.; Roos, C.; Donnet, A.; Giraud, P.; Guégan-Massardier, E.; Lantéri-Minet, M.; Lucas, C.; Mawet, J.; Moisset, X.; et al. Revised guidelines of the French headache society for the diagnosis and management of migraine in adults. Part 2: Pharmacological treatment. Rev. Neurol. 2021, 177, 734–752. [Google Scholar] [CrossRef] [PubMed]
- Demarquay, G.; Mawet, J.; Guégan-Massardier, E.; de Gaalon, S.; Donnet, A.; Giraud, P.; Lantéri-Minet, M.; Lucas, C.; Moisset, X.; Roos, C.; et al. Revised guidelines of the French headache society for the diagnosis and management of migraine in adults. Part 3: Non-pharmacological treatment. Rev. Neurol. 2021, 177, 753–759. [Google Scholar] [CrossRef]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Suzuki, K.; Okamura, M.; Haruyama, Y.; Suzuki, S.; Shiina, T.; Kobashi, G.; Hirata, K. Exploring the contributing factors to multiple chemical sensitivity in patients with migraine. J. Occup. Health 2022, 64, e12328. [Google Scholar] [CrossRef] [PubMed]
- Burstein, R.; Yarnitsky, D.; Goor-Aryeh, I.; Ransil, B.J.; Bajwa, Z.H. An association between migraine and cutaneous allodynia. Ann. Neurol. 2000, 47, 614–624. [Google Scholar] [CrossRef]
- Bigal, M.E.; Ashina, S.; Burstein, R.; Reed, M.L.; Buse, D.; Serrano, D.; Lipton, R.B.; On behalf of the AMPP Group. Prevalence and characteristics of allodynia in headache sufferers: A population study. Neurology 2008, 70, 1525–1533. [Google Scholar] [CrossRef] [Green Version]
- Altay, H.; Celenay, S.T. An investigation of the relationship between cutaneous allodynia and kinesiophobia, gastrointestinal system symptom severity, physical activity and disability in individuals with migraine. Korean J. Pain 2023, 36, 137–146. [Google Scholar] [CrossRef]
- Pall, M.L. Microwave frequency electromagnetic fields (EMFs) produce widespread neuropsychiatric effects including depression. J. Chem. Neuroanat. 2016, 75, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Vaitl, D.; Propson, N.; Stark, R.; Walter, B.; Schienle, A. Headache and Sferics. Headache J. Head Face Pain 2001, 41, 845–853. [Google Scholar] [CrossRef]
- Panagopoulos, D.J.; Balmori, A. On the biophysical mechanism of sensing atmospheric discharges by living organisms. Sci. Total Environ. 2017, 599–600, 2026–2034. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.P.; de Oliveira, A.C.; Meirelles, R.; Machado, M.C.C.; Zanesco, T.; Surjan, R.; Chammas, M.C.; de Souza Rocha, M.; Morgan, D.; Cantor, A.; et al. Treatment of advanced hepatocellular carcinoma with very low levels of amplitude-modulated electromagnetic fields. Br. J. Cancer 2011, 105, 640–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jimenez, H.; Wang, M.; Zimmerman, J.W.; Pennison, M.J.; Sharma, S.; Surratt, T.; Xu, Z.X.; Brezovich, I.; Absher, D.; Myers, R.M.; et al. Tumour-specific amplitude-modulated radiofrequency electromagnetic fields induce differentiation of hepatocellular carcinoma via targeting Cav3.2 T-type voltage-gated calcium channels and Ca2+ influx. eBioMedicine 2019, 44, 209–224. [Google Scholar] [CrossRef] [Green Version]
- Bertagna, F.; Lewis, R.; Silva, S.R.P.; McFadden, J.; Jeevaratnam, K. Effects of electromagnetic fields on neuronal ion channels: A systematic review. Ann. N. Y. Acad. Sci. 2021, 1499, 82–103. [Google Scholar] [CrossRef] [PubMed]


| Patients’ Description and History | n | Values |
|---|---|---|
| Women | 292 | 283 (96.9) |
| Age, years, mean ± SD | 291 | 56.5 ± 12.3 |
| BMI, kg/m2, median [IQ25-75] | 292 | 21.9 [19.7; 24.3] |
| History of allergy | 293 | 197 (67.2) |
| History of food intolerance | 293 | 188 (64.2) |
| History of asthma | 293 | 45 (15.4) |
| History of seizure | 293 | 10 (3.4) |
| History of migraine | 293 | 178 (60.7) |
| History of noise intolerance | 293 | 184 (62.8) |
| History of light intolerance | 293 | 150 (51.2) |
| History of vibrations intolerance | 293 | 123 (42,0) |
| History of smells intolerance | 293 | 185 (63.1) |
| History of MCS | 293 | 159 (54.3) |
| History of fibromyalgia | 293 | 61 (20.8) |
| History of dental care | 293 | 242 (82.6) |
| History of brain injury | 293 | 60 (20.5) |
| History of Lyme disease | 293 | 58 (19.8) |
| Electrohypersensitivity characteristics | ||
| Duration between first EHS symptoms and study, years, median [IQ25-75] | 293 | 10 [5; 16] |
| Diagnosis of EHS made by a doctor | 293 | 217 (74.1) |
| Sick leave for EHS | 293 | 64 (21.8) |
| Medication for EHS | 293 | 97 (33.1) |
| Departmental House for the Disabled file | 293 | 141 (48.1) |
| Recognition as a disabled worker | 131 | 94 (71.8) |
| Trigger identified | 293 | 204 (69.6) |
| Symptoms appear during exposure to a source of electromagnetic radiation | 293 | 293 (100) |
| Symptoms stop after exposure is stopped | 258 | 210 (81.4) |
| Symptoms appear systematically in response to new exposure | 280 | 271 (96.8) |
| During the past 12 months, symptoms have been occurring more and more frequently | 247 | 157 (63.6) |
| Symptoms triggered by new sources | 220 | 141 (64.1) |
| Headaches | 293 | 230 (78.5) |
| Headaches and nausea/vomiting | 226 | 112 (49.6) |
| Headaches and photophobia | 228 | 158 (69.3) |
| Headaches and visual disturbances | 224 | 84 (37.5) |
| Migraine | 191 (65.2) | |
| Migraine with aura | 84 (28.7) | |
| Number of electromagnetic field sources identified, mean ± SD | 293 | 12 (±5) |
| Electrohypersensitivity impact on daily life | ||
| Stage 1: Symptoms do not change the way of living | 292 | 1 (0.3) |
| Stage 2: Symptoms force putting in place avoidance measures | 291 | 47 (16) |
| Stage 3: Symptoms prevent social life | 290 | 241 (83) |
| Intensity of symptoms in EHS patients, median [IQ25-75] | ||
| Rheumatology | 287 | 7 [4–8] |
| Digestive | 284 | 6 [3–8] |
| Cognitive | 289 | 8 [7–10] |
| Respiratory | 286 | 6 [3–8] |
| Cardiac | 290 | 6 [4–8] |
| Mood | 284 | 8 [5–9] |
| Cutaneous | 273 | 4 [0–7] |
| Headache | 287 | 8 [7–10] |
| Perception | 284 | 7 [4–8] |
| Genital | 282 | 4.5 [0–7] |
| Tinnitus | 286 | 7 [2–9] |
| Tiredness | 286 | 9 [8–10] |
| Migraineur n = 191 | Non-Migraineur n = 102 | p | |
|---|---|---|---|
| Age, years, mean ± SD | 54.6 ± 11.9 | 59.97 ± 12.2 | <0.01 |
| Women | 183 (96.3) | 100 (98.0) | 0.68 |
| BMI, kg/cm2, median (IQ25-75) | 21.8 (19.5–24.5) | 22.0 (20.1–23.9) | 0.55 |
| History of allergy | 133 (69.6) | 64 (62.7) | 0.23 |
| History of food intolerance | 130 (68.1) | 58 (56.9) | 0.06 |
| History of asthma | 35 (18.3) | 10 (9.8) | 0.05 |
| History of seizure | 9 (4.7) | 1 (0.9) | 0.17 |
| History of migraine | 142 (74.3) | 36 (35.3) | <0.01 |
| History of noise intolerance | 130 (68.1) | 54 (52.9) | 0.01 |
| History of light intolerance | 120 (62.8) | 30 (29.4) | <0.01 |
| History of vibrations intolerance | 90 (47.1) | 33 (32.3) | 0.01 |
| History of smells intolerance | 132 (69.1) | 53 (51.9) | <0.01 |
| History of MCS | 116 (60.7) | 43 (42.2) | <0.01 |
| History of fibromyalgia | 49 (25.6) | 12 (11.8) | <0.01 |
| History of dental care | 162 (84.8) | 80 (78.4) | 0.17 |
| History of brain injury | 45 (23.6) | 15 (14.7) | 0.07 |
| History of Lyme disease | 41 (21.5) | 17 (16.7) | 0.33 |
| Electrohypersensitivity characteristics | |||
| Symptoms appear during exposure to a source of electromagnetic radiation | 191 (100.0) | 102 (100.0) | . |
| Symptoms stop after exposure is stopped | 134 (81.2) | 76 (81.7) | 0.92 |
| Symptoms appear systematically in response to new exposure | 178 (97.3) | 93 (95.9) | 0.50 |
| During the past 12 months, symptoms have been occurring more and more frequently | 111 (68.1) | 46 (54.7) | 0.04 |
| Symptoms triggered by new sources | 99 (68.7) | 42 (55.3) | 0.05 |
| Number of electromagnetic field sources identified, mean ± SD | 12.92 ± 4.7 | 10.33 ± 5.0 | <0.01 |
| Electrohypersensitivity impact on daily life | |||
| Symptoms changed the way of living | 188 (98.9) | 100 (98.0) | 0.61 |
| Symptoms forced to put in place avoidance measures | 188 (99.8) | 99 (97.0) | 0.13 |
| Symptoms prevent social life | 165 (87.8) | 76 (74.5) | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Greco, F.; Garnier, O.; Macioce, V.; Picot, M.C. Prevalence of Migraine Disease in Electrohypersensitive Patients. J. Clin. Med. 2023, 12, 4092. https://doi.org/10.3390/jcm12124092
Greco F, Garnier O, Macioce V, Picot MC. Prevalence of Migraine Disease in Electrohypersensitive Patients. Journal of Clinical Medicine. 2023; 12(12):4092. https://doi.org/10.3390/jcm12124092
Chicago/Turabian StyleGreco, Frédéric, Océane Garnier, Valérie Macioce, and Marie Christine Picot. 2023. "Prevalence of Migraine Disease in Electrohypersensitive Patients" Journal of Clinical Medicine 12, no. 12: 4092. https://doi.org/10.3390/jcm12124092
APA StyleGreco, F., Garnier, O., Macioce, V., & Picot, M. C. (2023). Prevalence of Migraine Disease in Electrohypersensitive Patients. Journal of Clinical Medicine, 12(12), 4092. https://doi.org/10.3390/jcm12124092