Direct Vertebral Rotation (DVR) Does Not Improve Clinical and Radiological Results Compared to Differential Rod Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis
Abstract
:1. Introduction
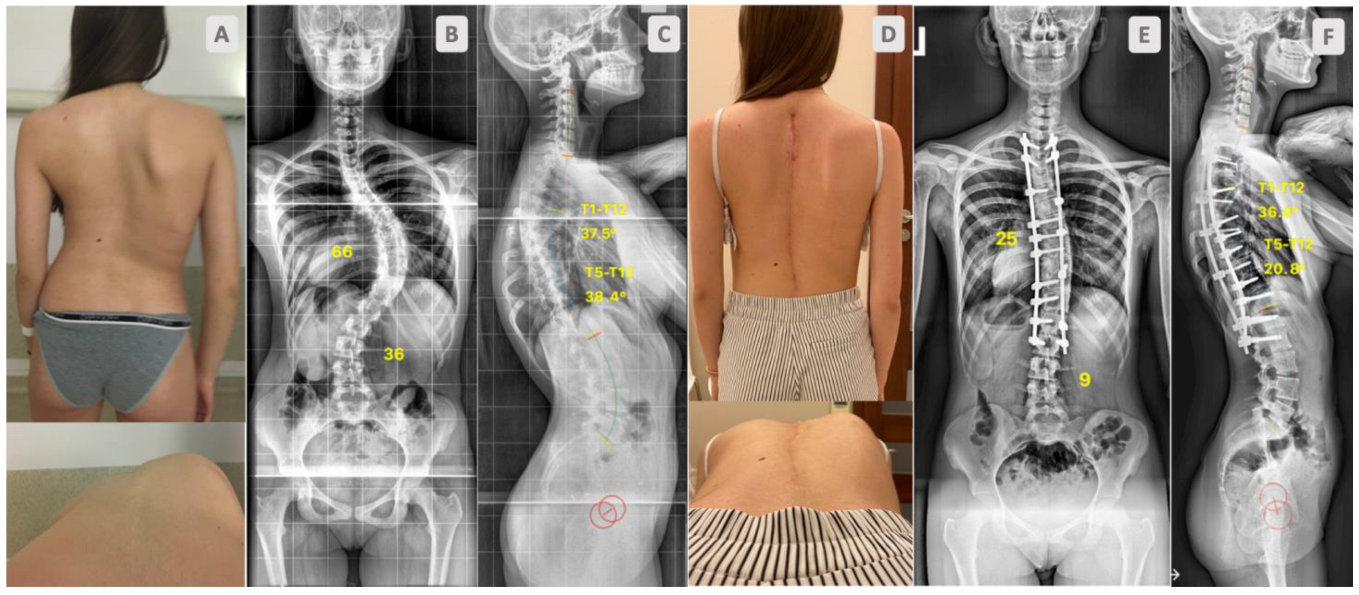
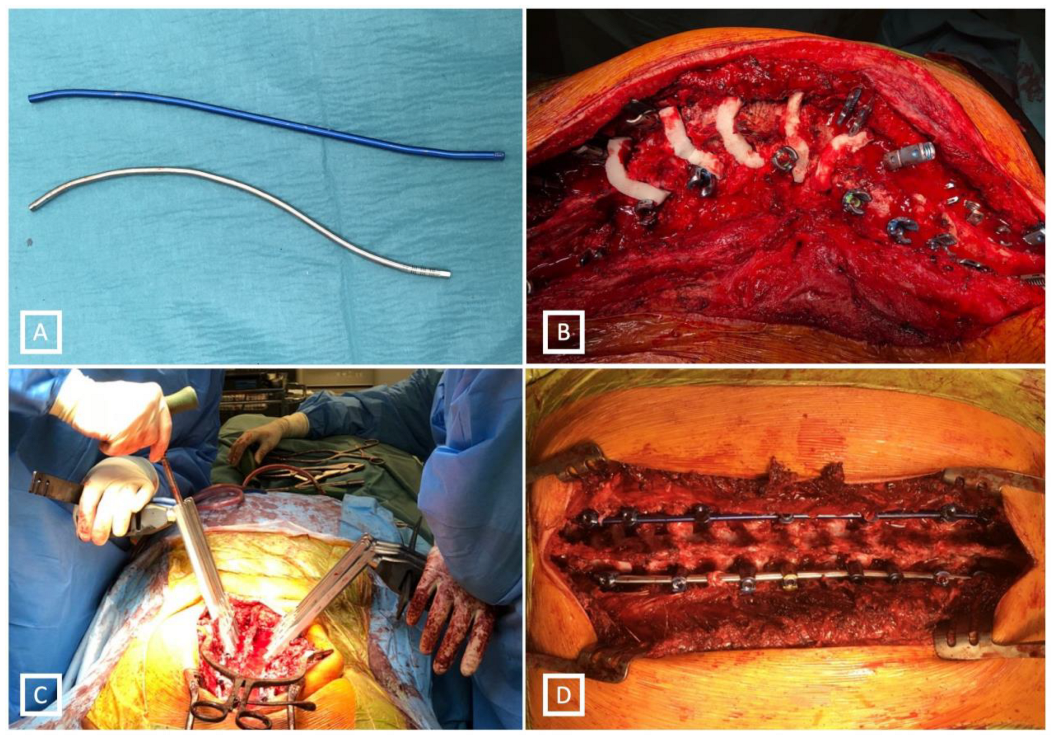
2. Material and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tambe, A.D.; Panikkar, S.J.; Millner, P.A.; Tsirikos, A.I. Current concepts in the surgical management of adolescent idiopathic scoliosis. Bone Jt. J. 2018, 100-B, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Suk, S.I.; Chung, E.R. Direct vertebral rotation: A new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine 2004, 29, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.S.; Lenke, G.L. Vertebral derotation in adolescent idiopathic scoliosis. Oper Tech. Orthop. 2009, 19, 19–23. [Google Scholar] [CrossRef]
- Urbanski, W.; Wolanczyk, M.J.; Jurasz, W.; Kulej, M.; Morasiewicz, P.; Dragan, S.L.; Sasiadek, M.; Dragan, S.F. The impact of direct vertebral rotation (DVR) on radiographic outcome in surgical correction of idiopathic scoliosis. Arch. Orthop. Trauma Surg. 2017, 137, 879–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sariyilmaz, K.; Ozkunt, O.; Gemalmaz, H.C.; Cingoz, T.; Pehlivanoglu, T.; Aksoy, T.; Kaya, O.; Baydogan, M.; Dikici, F. Direct vertebral rotation significantly decreases the pullout strength of the pedicle screw: A biomechanical study in adult cadavers. J. Pediatr. Orthop. B 2020, 30, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Badve, S.A.; Ordway, N.R.; Albanese, S.A.; Lavelle, W.F. Toward a better understanding of direct vertebral rotation for AIS surgery: Development of a multisegmental biomechanical model and factors affecting correction. Spine J. 2015, 15, 1034–1040. [Google Scholar] [CrossRef]
- Hicks, J.; Singla, A.; Arlet, V. 145. Complications of Pedicle Screw Fixation in Scoliosis Surgery: A Systematic Review. Spine J. 2009, 9, 77S. [Google Scholar] [CrossRef]
- Di Silvestre, M.; Lolli, F.; Bakaloudis, G.; Maredi, E.; Vommaro, F.; Pastorelli, F. Apical vertebral derotation in the posterior treatment of adolescent idiopathic scoliosis: Myth or reality? Eur. Spine J. 2012, 22, 313–323. [Google Scholar] [CrossRef] [Green Version]
- Rushton, P.R.P.; Grevitt, M.P. Do vertebral derotation techniques offer better outcomes compared to traditional methods in the surgical treatment of adolescent idiopathic scoliosis? Eur. Spine J. 2014, 23, 1166–1176. [Google Scholar] [CrossRef]
- Kim, G.-U.; Yang, J.H.; Chang, D.-G.; Suk, S.-I.; Suh, S.-W.; Song, K.-S.; Nam, K.-Y.; Oh, I.-S.; Park, H.-Y.; Kim, S.-I.; et al. Effect of Direct Vertebral Rotation in Single Thoracic Adolescent Idiopathic Scoliosis: Better 3-Dimensional Deformity Correction. World Neurosurg. 2019, 129, e401–e408. [Google Scholar] [CrossRef]
- Seki, S.; Kawaguchi, Y.; Nakano, M.; Makino, H.; Mine, H.; Kimura, T. Rod rotation and differential rod contouring followed by direct vertebral rotation for treatment of adolescent idiopathic scoliosis: Effect on thoracic and thoracolumbar or lumbar curves assessed with intraoperative computed tomography. Spine J. 2015, 16, 365–371. [Google Scholar] [CrossRef]
- Wang, X.; Boyer, L.; Le Naveaux, F.; Schwend, R.M.; Aubin, C.-E. How does differential rod contouring contribute to 3-dimensional correction and affect the bone-screw forces in adolescent idiopathic scoliosis instrumentation? Clin. Biomech. 2016, 39, 115–121. [Google Scholar] [CrossRef]
- Lenke, L.G. The Lenke Classification System of Operative Adolescent Idiopathic Scoliosis. Neurosurg. Clin. N. Am. 2007, 18, 199–206. [Google Scholar] [CrossRef]
- Mladenov, K.V.; Vaeterlein, C.; Stuecker, R. Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: Effects on the sagittal alignment. Eur. Spine J. 2011, 20, 1114–1117. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, K.; Nakamura, T.; Iwanami, A.; Hosogane, N.; Tsuji, T.; Ishii, K.; Nakamura, M.; Toyama, Y.; Chiba, K.; Matsumoto, M. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet. Disord. 2012, 13, 99. [Google Scholar] [CrossRef] [Green Version]
- Tang, X.; Zhao, J.; Zhang, Y. Radiographic, clinical, and patients’ assessment of segmental direct vertebral body derotation versus simple rod derotation in main thoracic adolescent idiopathic scoliosis: A prospective, comparative cohort study. Eur. Spine J. 2014, 24, 298–305. [Google Scholar] [CrossRef]
- Sun, L.; Song, Y.; Liu, L.; An, Y.; Zhou, C.; Zhou, Z. Bilateral apical vertebral derotation technique by vertebral column manipulation compared with vertebral coplanar alignment technique in the correction of lenke type 1 idiopathic scoliosis. BMC Musculoskelet. Disord. 2013, 14, 175–179. [Google Scholar] [CrossRef] [Green Version]
- Carreon, L.Y.; Kelly, M.P.; Crawford, C.H.; Baldus, C.R.; Glassman, S.D.; Shaffrey, C.I.; Bridwell, K.H. SRS-22R Minimum Clinically Important Difference and Substantial Clinical Benefit after Adult Lumbar Scoliosis Surgery. Spine Deform. 2017, 6, 79–83. [Google Scholar] [CrossRef]
- Grivas, T.B.; Vasiliadis, E.S.; Mihas, C.; Savvidou, O. The effect of growth on the correlation between the spinal and rib cage deformity: Implications on idiopathic scoliosis pathogenesis. Scoliosis 2007, 2, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Grivas, T.B.; Vynichakis, G.; Chandrinos, M.; Mazioti, C.; Papagianni, D.; Mamzeri, A.; Mihas, C. Morphology, Development and Deformation of the Spine in Mild and Moderate Scoliosis: Are Changes in the Spine Primary or Secondary? J. Clin. Med. 2021, 10, 5901. [Google Scholar] [CrossRef]
- Jankowski, P.P.; Yaszay, B.; Cidambi, K.R.; Bartley, C.E.; Bastrom, T.P.; Newton, P.O. The Relationship between Apical Vertebral Rotation and Truncal Rotation in Adolescent Idiopathic Scoliosis Using 3D Reconstructions. Spine Deform. 2018, 6, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Mattila, M.; Jalanko, T.; Helenius, I. En Bloc Vertebral Column Derotation Provides Spinal Derotation but no Additional Effect on Thoracic Rib Hump Correction as Compared with no Derotation in Adolescents Undergoing Surgery for Idiopathic Scoliosis with Total Pedicle Screw Instrumentation. Spine 2013, 38, 1576–1583. [Google Scholar] [CrossRef] [PubMed]
- Seki, S.; Newton, P.O.; Yahara, Y.; Makino, H.; Nakano, M.; Hirano, N.; Kawaguchi, Y.; Kimura, T. Differential rod contouring is essential for improving vertebral rotation in patients with adolescent idiopathic scoliosis: Thoracic curves assessed with intraoperative CT. Spine 2018, 43, E585–E591. [Google Scholar] [CrossRef] [PubMed]
- Son, S.M.; Choi, S.H.; Goh, T.S.; Park, W.; Lee, J.S. Efficacy and Safety of Direct Vertebral Rotation in the Surgical Correction of Scoliosis: A Meta-Analysis. World Neurosurg. 2019, 124, e641–e648. [Google Scholar] [CrossRef] [PubMed]
- Acaroglu, E.; Doany, M.; Cetin, E.; Castelein, R. Correction of rotational deformity and restoration of thoracic kyphosis are inversely related in posterior surgery for adolescent idiopathic scoliosis. Med. Hypotheses 2019, 133, 109396. [Google Scholar] [CrossRef]
- Schlösser, T.P.; van Stralen, M.; Brink, R.C.; Chu, W.C.W.; Lam, T.-P.; Vincken, K.L.; Castelein, R.M.; Cheng, J.C.Y. Three-Dimensional Characterization of Torsion and Asymmetry of the Intervertebral Discs versus Vertebral Bodies in Adolescent Idiopathic Scoliosis. Spine 2014, 39, E1159–E1166. [Google Scholar] [CrossRef]
- Hershkovich, O.; D’souza, A.; Rushton, P.R.P.; Onosi, I.S.; Yoon, W.W.; Grevitt, M.P. Essential lordosis revisited. Bone Jt. J. 2020, 102-B, 513–518. [Google Scholar] [CrossRef]
- Ruffilli, A.; Fiore, M.; Viroli, G.; Barile, F.; Manzetti, M.; Martikos, K.; Greggi, T.; Faldini, C. 5.5-mm Cobalt-Chrome vs 6-mm Titanium Alloy Rods in Surgical Treatment of Lenke 1 Adolescent Idiopathic Scoliosis with High-Density Pedicle Screws and Direct Vertebral Rotation on Differently Shaped Rods: A Retrospective Comparative Cohort Study. Int. J. Spine Surg. 2022, 17, 25–31. [Google Scholar] [CrossRef]
- Sabah, Y.; Clément, J.-L.; Solla, F.; Rosello, O.; Rampal, V. Cobalt-chrome and titanium alloy rods provide similar coronal and sagittal correction in adolescent idiopathic scoliosis. Orthop. Traumatol. Surg. Res. 2018, 104, 1073–1077. [Google Scholar] [CrossRef]
- Ohrt-Nissen, S.; Dahl, B.; Gehrchen, M. Choice of Rods in Surgical Treatment of Adolescent Idiopathic Scoliosis: What Are the Clinical Implications of Biomechanical Properties?—A Review of the Literature. Neurospine 2018, 15, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Suk, S.I.; Lee, S.M.; Chung, E.R.; Kim, J.-H.; Kim, S.-S. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: More than 5-year follow-up. Spine 2005, 30, 1602–1609. [Google Scholar] [CrossRef]
- Pasha, S.; Cahill, P.J.; Flynn, J.M.; Sponseller, P.; Newton, P.O.; Harms Study Group. Relationships between the Axial Derotation of the Lower Instrumented Vertebra and Uninstrumented Lumbar Curve Correction: Radiographic Outcome in Lenke 1 Adolescent Idiopathic Scoliosis with a Minimum 2-Year Follow-up. J. Pediatr. Orthop. 2018, 38, e194–e201. [Google Scholar] [CrossRef]
- Chang, D.-G.; Suk, S.-I.; Kim, J.-H.; Song, K.-S.; Suh, S.-W.; Kim, S.-Y.; Kim, G.-U.; Yang, J.H.; Lee, J.-H. Long-term Outcome of Selective Thoracic Fusion Using Rod Derotation and Direct Vertebral Rotation in the Treatment of Thoracic Adolescent Idiopathic Scoliosis: More than 10-Year Follow-up Data. Clin. Spine Surg. 2020, 33, E50–E57. [Google Scholar] [CrossRef]
- Huang, Z.; Wang, Q.; Yang, J.; Yang, J.; Li, F. Vertebral Derotation by Vertebral Column Manipulator Improves Postoperative Radiographs Outcomes of Lenke 5C Patients for Follow-up of Minimum 2 Years. Clin. Spine Surg. A Spine Publ. 2016, 29, E157–E161. [Google Scholar] [CrossRef]
- Samdani, A.F.; Bennett, J.T.; Singla, A.R.; Marks, M.C.; Pahys, J.M.; Lonner, B.S.; Miyanji, F.; Shah, S.A.; Shufflebarger, H.L.; Newton, P.O.; et al. Do Ponte Osteotomies Enhance Correction in Adolescent Idiopathic Scoliosis? An Analysis of 191 Lenke 1A and 1B Curves. Spine Deform. 2015, 3, 483–488. [Google Scholar] [CrossRef]
- Halanski, M.A.; Cassidy, J.A. Do Multilevel Ponte Osteotomies in Thoracic Idiopathic Scoliosis Surgery Improve Curve Correction and Restore Thoracic Kyphosis? J. Spinal Disord. Tech. 2013, 26, 252–255. [Google Scholar] [CrossRef]
- Floccari, L.V.; Poppino, K.; Greenhill, D.A.; Sucato, D.J. Ponte osteotomies in a matched series of large AIS curves increase surgical risk without improving outcomes. Spine Deform. 2021, 9, 1411–1418. [Google Scholar] [CrossRef]
- Sangiorgio, S.N.; Borkowski, S.L.; Day, M.J.; Ho, N.C.; Knutsen, A.; Scaduto, A.A.; Bowen, R.E.; Ebramzadeh, E. Increasing loads and diminishing returns: A biomechanical study of direct vertebral rotation. Spine Deform. 2020, 8, 577–584. [Google Scholar] [CrossRef]
- Seki, S.; Yahara, Y.; Makino, H.; Kawaguchi, Y.; Kimura, T. Selection of posterior spinal osteotomies for more effective periapical segmental vertebral derotation in adolescent idiopathic scoliosis–An in vivo comparative analysis between Ponte osteotomy and inferior facetectomy alone. J. Orthop. Sci. 2018, 23, 488–494. [Google Scholar] [CrossRef]




| DRC (n = 38) | DRC and DVR (n = 35) | p Value | |
|---|---|---|---|
| Age (years) | 15.6 (±1.5) | 15.5 (±1.6) | 0.814 |
| Sex (males/females) | 3/38 | 3/35 | 0.917 |
| Main curve magnitude | 62 (±10) | 58 (±14) | 0.098 |
| Coronal curve flexibility (%) | 33 (±14) | 36 (±12) | 0.372 |
| Number of instrumented levels | 11.8 (±1.7) | 11.1 (±2) | 0.107 |
| Screw density | 78 (±7.2) | 77.6 (±6.3) | 0.774 |
| SRS-22r | Total | Function | Pain | Self-Image | Mental Health | Satisfaction from Management |
|---|---|---|---|---|---|---|
| DRC | 4.23 (±0.33) | 4.26 (±0.48) | 4.36 (±0.48) | 4.14 (±0.54) | 3.88 (±0.63) | 4.86 (±0.27) |
| DRC and DVR | 4.06 (±0.33) | 4.17 (±0.59) | 4.13 (±0.55) | 4.03 (±0.59) | 3.68 (±0.51) | 4.68 (±0.35) |
| p value | 0.101 | 0.579 | 0.137 | 0.509 | 0.263 | 0.065 |
| DRC | DRC/DVR | p | ||
|---|---|---|---|---|
| Coronal curve | Pre op [°] | 62 (±10) | 58 (±14) | 0.098 |
| Post op [°] | 21 (±8) | 22 (±11) | 0.601 | |
| % of correction | 66 (±12) | 63 (±15) | 0.28 | |
| Kyphosis T1–T12 | Pre op [°] | 32 (±11) | 37 (±10) | 0.043 |
| Post op | 37 (±8) | 39 (±9) | 0.424 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urbanski, W.; Markowski, P.; Zaluski, R.; Kokaveshi, A.; Morasiewicz, P. Direct Vertebral Rotation (DVR) Does Not Improve Clinical and Radiological Results Compared to Differential Rod Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 4091. https://doi.org/10.3390/jcm12124091
Urbanski W, Markowski P, Zaluski R, Kokaveshi A, Morasiewicz P. Direct Vertebral Rotation (DVR) Does Not Improve Clinical and Radiological Results Compared to Differential Rod Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis. Journal of Clinical Medicine. 2023; 12(12):4091. https://doi.org/10.3390/jcm12124091
Chicago/Turabian StyleUrbanski, Wiktor, Piotr Markowski, Rafal Zaluski, Anis Kokaveshi, and Piotr Morasiewicz. 2023. "Direct Vertebral Rotation (DVR) Does Not Improve Clinical and Radiological Results Compared to Differential Rod Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis" Journal of Clinical Medicine 12, no. 12: 4091. https://doi.org/10.3390/jcm12124091
APA StyleUrbanski, W., Markowski, P., Zaluski, R., Kokaveshi, A., & Morasiewicz, P. (2023). Direct Vertebral Rotation (DVR) Does Not Improve Clinical and Radiological Results Compared to Differential Rod Contouring (DRC) in Patients Treated Surgically for Idiopathic Scoliosis. Journal of Clinical Medicine, 12(12), 4091. https://doi.org/10.3390/jcm12124091








