Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Approval
2.2. Subjects
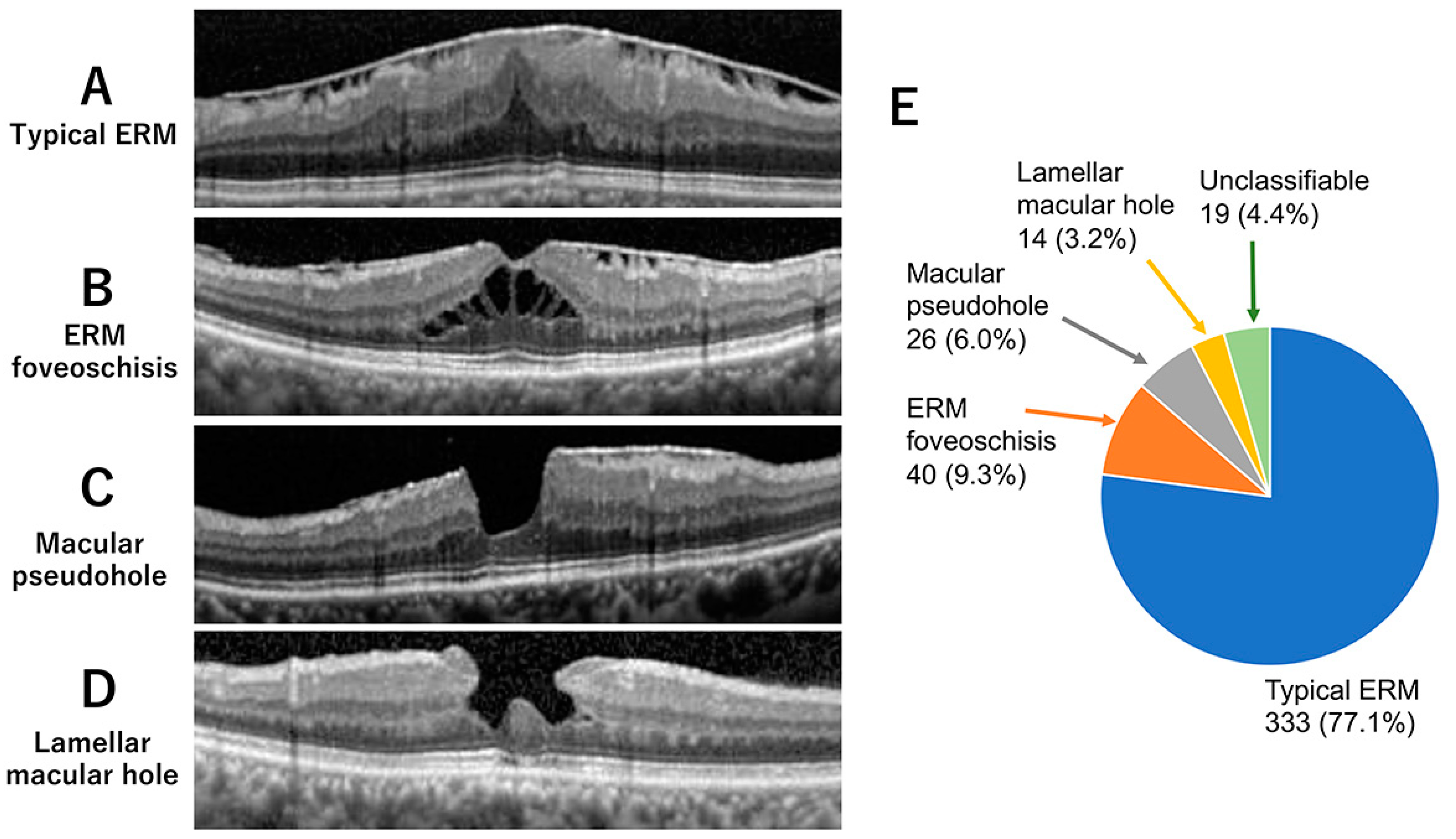
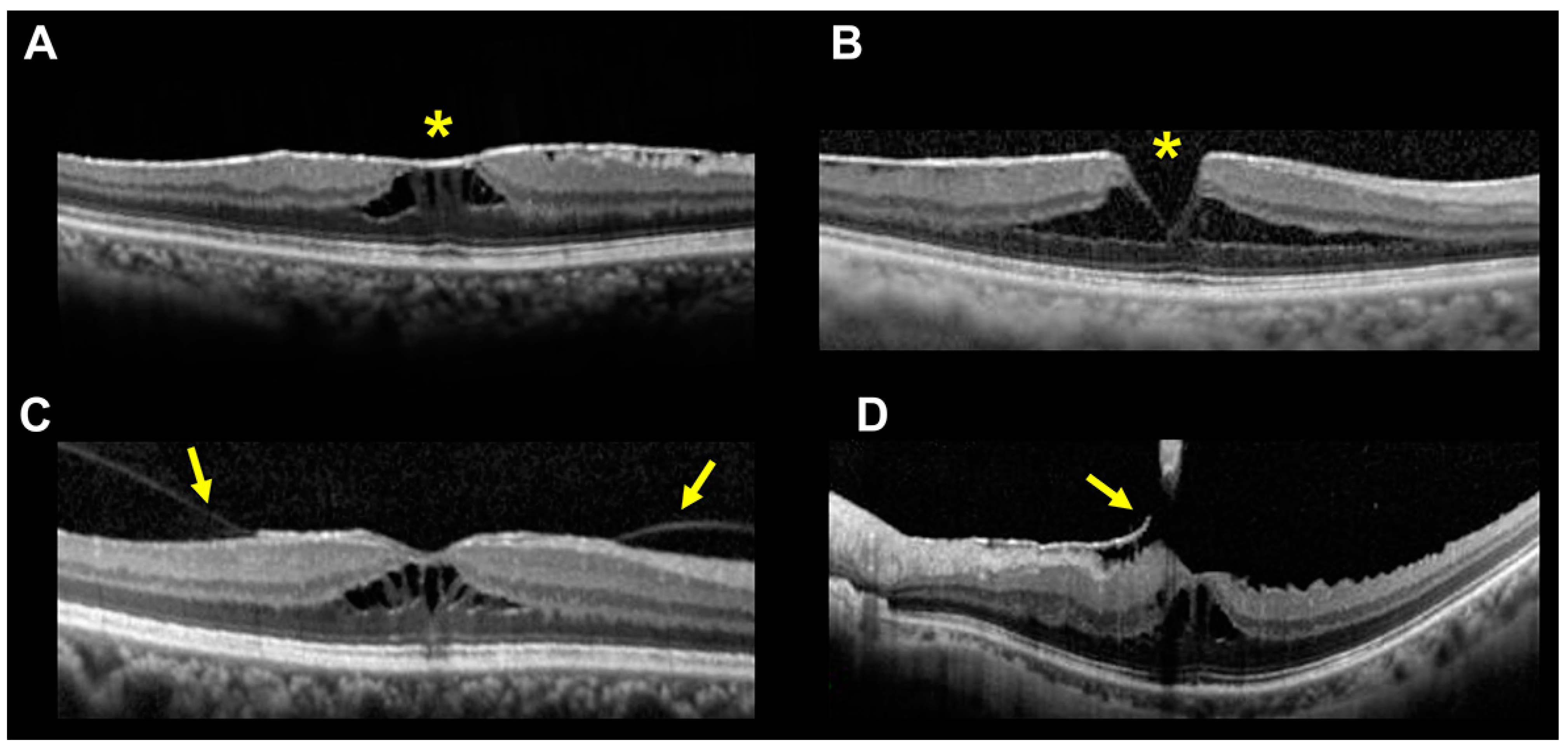
2.3. Definition of Subtypes of ERM-Related Diseases
2.4. Ophthalmological Examinations
2.5. Surgical Procedures
2.6. Statistical Analyses
3. Results
3.1. Incidence of ERM Foveoschisis
3.2. Comparison of Clinical Characteristics
3.3. Comparisons of OCT Findings
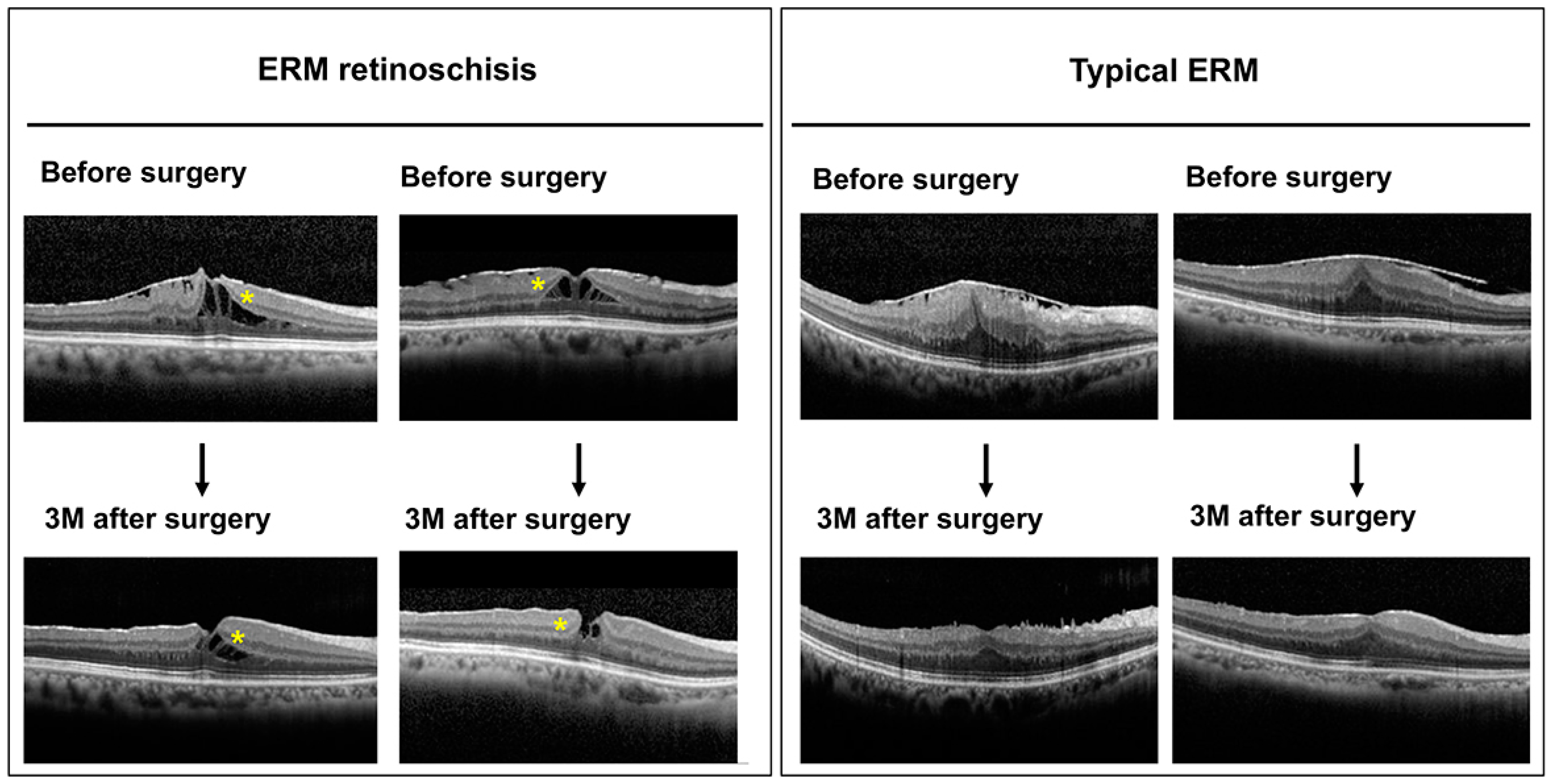
3.4. Comparison of Short-Term Surgical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hubschman, J.P.; Govetto, A.; Spaide, R.F.; Schumann, R.; Steel, D.; Figueroa, M.S.; Sebag, J.; Gaudric, A.; Staurenghi, G.; Haritoglou, C.; et al. Optical coherence tomography-based consensus definition for lamellar macular hole. Br. J. Ophthalmol. 2020, 104, 1741–1747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Govetto, A.; Dacquay, Y.; Farajzadeh, M.; Platner, E.; Hirabayashi, K.; Hosseini, H.; Schwartz, S.D.; Hubschman, J.P. Lamellar macular hole: Two distinct clinical entities? Am. J. Ophthalmol. 2016, 164, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Hirano, M.; Morizane, Y.; Kimura, S.; Hosokawa, M.; Shiode, Y.; Doi, S.; Toshima, S.; Takahashi, K.; Hosogi, M.; Fujiwara, A.; et al. Assessment of lamellar macular hole and macular pseudohole with a combination of en face and radial B-scan optical coherence tomography imaging. Am. J. Ophthalmol. 2018, 188, 29–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, J.H.; Yee, K.M.P.; Nguyen-Cuu, J.; Sebag, J. Structural and functional characteristics of lamellar macular holes. Retina 2019, 39, 2084–2089. [Google Scholar] [CrossRef]
- Figueroa, M.S.; Govetto, A.; Steel, D.H.; Sebag, J.; Virgili, G.; Hubschman, J.P. Pars plana vitrectomy for the treatment of tractional and degenerative lamellar macular holes: Functional and anatomical results. Retina 2019, 39, 2090–2098. [Google Scholar] [CrossRef]
- Yeo, J.H.; Oh, R.; Lee, J.Y.; Kim, J.G.; Yoon, Y.H.; Kim, Y.J. Optical coherence tomography angiographic findings of lamellar macular hole: Comparisons between tractional and degenerative subtypes. Sci. Rep. 2020, 10, 13331. [Google Scholar] [CrossRef]
- Hwang, J.U.; Sohn, J.; Moon, B.G.; Joe, S.G.; Lee, J.Y.; Kim, J.G.; Yoon, Y.H. Assessment of macular function for idiopathic epiretinal membranes classified by spectral-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3562–3569. [Google Scholar] [CrossRef] [Green Version]
- Gaudric, A.; Aloulou, Y.; Tadayoni, R.; Massin, P. Macular pseudoholes with lamellar cleavage of their edge remain pseudoholes. Am. J. Ophthalmol. 2013, 155, 733–742. [Google Scholar] [CrossRef]
- Zampedri, E.; Romanelli, F.; Semeraro, F.; Parolini, B.; Frisina, R. Spectral-domain optical coherence tomography findings in idiopathic lamellar macular hole. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 699–707. [Google Scholar] [CrossRef]
- dell’Omo, R.; Filippelli, M.; De Turris, S.; Cimino, L.; Steel, D.H.; Pavesio, C.E.; Govetto, A.; Chehaibou, I.; Parmeggiani, F.; Romano, M.R.; et al. Fluorescein angiography findings in eyes with lamellar macular hole and epiretinal membrane foveoschisis. Investig. Ophthalmol. Vis. Sci. 2021, 62, 34. [Google Scholar] [CrossRef]
- Nakamura, K.; Inoue, T.; Nagura, K.; Tanaka, Y.; Arasaki, R.; Asaoka, R.; Yanagi, Y.; Maruyama-Inoue, M.; Kadonosono, K. Foveal microstructure and visual function in patients with lamellar macular hole, epiretinal membrane foveoschisis or macular pseudohole. Eye 2022, 36, 2247–2252. [Google Scholar]
- Hetzel, A.; Neubauer, J.; Gelisken, F. Clinical characteristics of patients with epiretinal membrane-Foveoschisis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2022; online ahead of print. [Google Scholar]
- Omoto, T.; Asahina, Y.; Zhou, H.P.; Fujino, R.; Takao, M.; Obata, R.; Inoue, T.; Asaoka, R.; Maruyama-Inoue, M.; Yanagi, Y.; et al. Visual outcomes and prognostic factors of vitrectomy for lamellar macular holes and epiretinal membrane foveoschisis. PLoS ONE 2021, 16, e0247509. [Google Scholar] [CrossRef]
- Photcharapongsakul, C.; Chokesuwattanaskul, S.; Choovuthayakorn, J.; Chaikitmongkol, V.; Kunavisarut, P.; Watanachai, N.; Patikulsila, D. Visual acuity and anatomical changes following vitrectomy for epiretinal membrane foveoschisis: A case series. BMC Ophthalmol. 2021, 21, 433. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.; Philippakis, E.; Gaudric, A.; Tadayoni, R.; Couturier, A. Postoperative outcomes of idiopathic epiretinal membrane associated with foveoschisis. Br. J. Ophthalmol. 2022, 106, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Sekine, R.; Kogo, J.; Jujo, T.; Sato, K.; Arizono, I.; Kawagoe, T.; Tokuda, N.; Kitaoka, Y.; Takagi, H. Efficacy of fovea-sparing internal limiting membrane peeling for epiretinal membrane foveoschisis. Ophthalmic Res. 2022, 65, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, J.R.; Puliafito, C.A.; Hee, M.R.; Duker, J.S.; Reichel, E.; Coker, J.G.; Schuman, J.S.; Swanson, E.A.; Fujimoto, J.G. Characterization of epiretinal membranes using optical coherence tomography. Ophthalmology 1996, 103, 2142–2151. [Google Scholar] [CrossRef]
- Duker, J.S.; Kaiser, P.K.; Binder, S.; de Smet, M.D.; Gaudric, A.; Reichel, E.; Sadda, S.R.; Sebag, J.; Spaide, R.F.; Stalmans, P. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013, 120, 2611–2619. [Google Scholar] [CrossRef]
- Gattoussi, S.; Buitendijk, G.H.S.; Peto, T.; Leung, I.; Schmitz-Valckenberg, S.; Oishi, A.; Wolf, S.; Deák, G.; Delcourt, C.; Klaver, C.C.W.; et al. European Eye Epidemiology (E3) consortium. The European Eye Epidemiology spectral-domain optical coherence tomography classification of macular diseases for epidemiological studies. Acta Ophthalmol. 2019, 97, 364–371. [Google Scholar] [CrossRef]
- Haouchine, B.; Massin, P.; Tadayoni, R.; Erginay, A.; Gaudric, A. Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am. J. Ophthalmol. 2004, 138, 732–739. [Google Scholar] [CrossRef]
- Mirza, R.G.; Johnson, M.W.; Jampol, L.M. Optical coherence tomography use in evaluation of the vitreoretinal interface: A review. Surv. Ophthalmol. 2007, 52, 397–421. [Google Scholar] [CrossRef]
- Cheong, K.X.; Xu, L.; Ohno-Matsui, K.; Sabanayagam, C.; Saw, S.M.; Hoang, Q.V. An evidence-based review of the epidemiology of myopic traction maculopathy. Surv. Ophthalmol. 2022, 67, 1603–1630. [Google Scholar] [CrossRef]
- Mataftsi, A.; Koutsimpogeorgos, D.; Brazitikos, P.; Ziakas, N.; Haidich, A.B. Is conversion of decimal visual acuity measurements to logMAR values reliable? Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 1513–1517. [Google Scholar] [CrossRef] [PubMed]


| ERM Foveoschisis | Typical ERM | p-Value | |
|---|---|---|---|
| Number of eyes/subjects | 40/40 | 333/333 | |
| Age, mean ± SD (range), years | 69.9 ± 6.8 | 71.1 ± 8.4 | p = 0.26 |
| Sex | p < 0.01 ** | ||
| Men, number of eyes (%) | 3 (7.5%) | 170 (51.1%) | |
| Women, number of eyes (%) | 37 (92.5%) | 163 (48.9%) | |
| Axial length, mm (number of eyes) | 23.7 ± 1.1 (30) | 23.6 ± 1.1 (253) | p = 0.54 |
| Best-corrected visual acuity, mean ± SD, logMAR | 0.23 ± 0.21 | 0.27 ± 0.25 | p = 0.34 |
| ERM Foveoschisis | Typical ERM | p-Value | |
|---|---|---|---|
| Number of eyes/subjects | 40/40 | 333/333 | |
| Central macular thickness (CMT), mean ± SD, µm | 340 ± 110 | 476 ± 111 | p < 0.01 ** |
| Absence of ERM at fovea centralis, number of eyes (%) | 22 (55.0%) | 33 (9.9%) | p < 0.01 ** |
| Continuity of ellipsoid zone number of eyes (%) | 33 (82.5%) | 207 (62.2%) | p = 0.01 * |
| Presence of vitreous adhesion, number of eyes (%) | 6 (15.0%) | 24 (7.2%) | p = 0.09 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sasaki, T.; Matsui, Y.; Kato, K.; Chujo, S.; Maeda, S.; Ozaki, A.; Ikesugi, K.; Sugimoto, M.; Matsubara, H.; Kondo, M. Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane. J. Clin. Med. 2023, 12, 4009. https://doi.org/10.3390/jcm12124009
Sasaki T, Matsui Y, Kato K, Chujo S, Maeda S, Ozaki A, Ikesugi K, Sugimoto M, Matsubara H, Kondo M. Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane. Journal of Clinical Medicine. 2023; 12(12):4009. https://doi.org/10.3390/jcm12124009
Chicago/Turabian StyleSasaki, Taku, Yoshitsugu Matsui, Kumiko Kato, Shinichiro Chujo, Satoshi Maeda, Atsuta Ozaki, Kengo Ikesugi, Masahiko Sugimoto, Hisashi Matsubara, and Mineo Kondo. 2023. "Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane" Journal of Clinical Medicine 12, no. 12: 4009. https://doi.org/10.3390/jcm12124009
APA StyleSasaki, T., Matsui, Y., Kato, K., Chujo, S., Maeda, S., Ozaki, A., Ikesugi, K., Sugimoto, M., Matsubara, H., & Kondo, M. (2023). Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane. Journal of Clinical Medicine, 12(12), 4009. https://doi.org/10.3390/jcm12124009






