Dissecting Relations between Depression Severity, Antidepressant Use, and Metabolic Syndrome Components in the NHANES 2005–2020
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Definitions of MetS Components, Depressive Symptoms, and Antidepressant Use
2.3. Definitions of Potential Confounders
2.4. Statistical Analysis
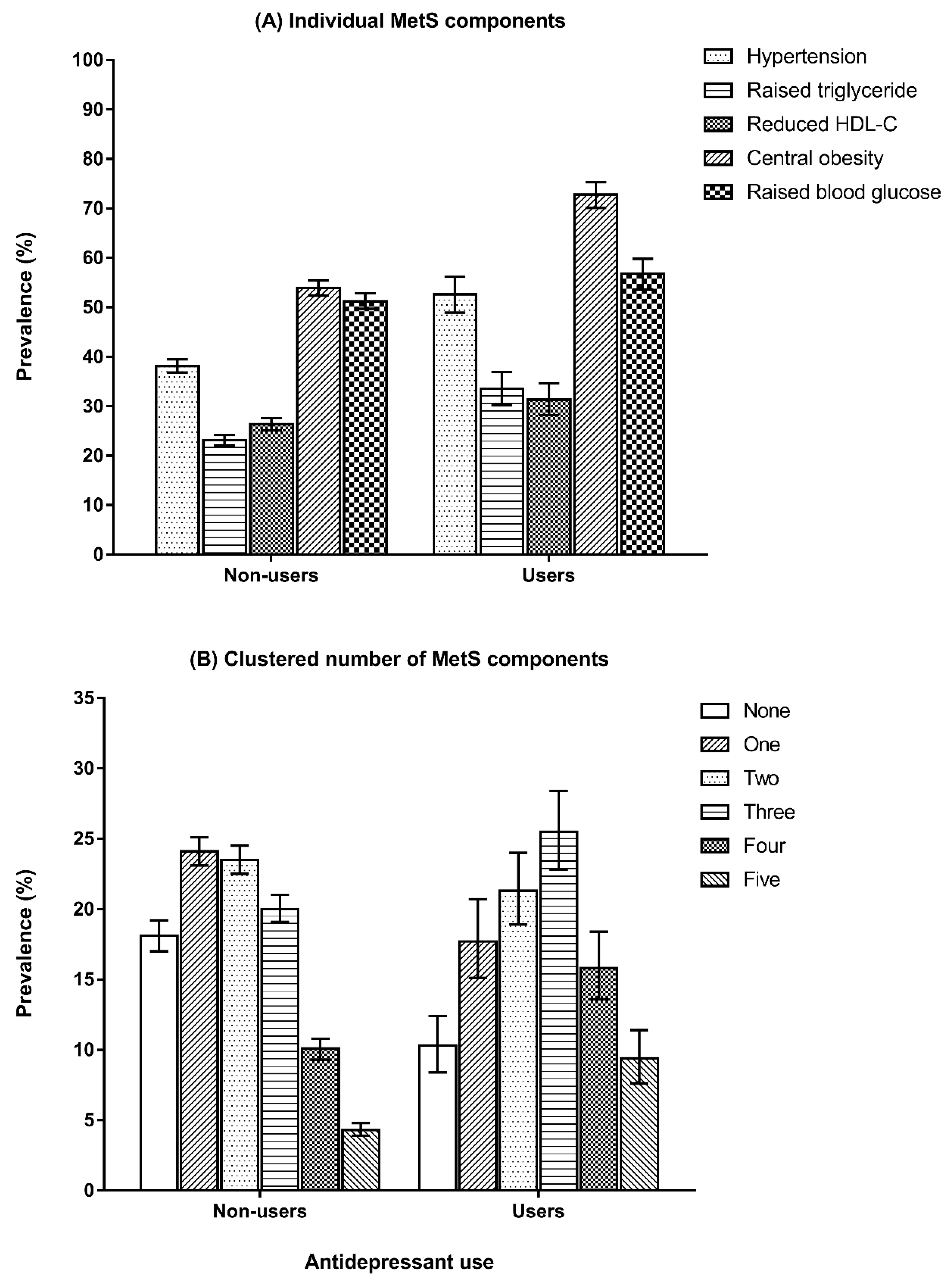
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ford, E.S. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care 2005, 28, 1769–1778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheung, B.M.; Wat, N.M.; Man, Y.B.; Tam, S.; Thomas, G.N.; Leung, G.M.; Cheng, C.H.; Woo, J.; Janus, E.D.; Lau, C.P.; et al. Development of diabetes in Chinese with the metabolic syndrome: A 6-year prospective study. Diabetes Care 2007, 30, 1430–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheung, B.M. The cardiovascular continuum in Asia—A new paradigm for the metabolic syndrome. J. Cardiovasc. Pharmacol. 2005, 46, 125–129. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (US). Expert Panel on Detection, Evaluation, & Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [Green Version]
- Penninx, B.; Lange, S.M.M. Metabolic syndrome in psychiatric patients: Overview, mechanisms, and implications. Dialogues Clin. Neurosci. 2018, 20, 63–73. [Google Scholar] [CrossRef]
- Frank, P.; Batty, G.D.; Pentti, J.; Jokela, M.; Poole, L.; Ervasti, J.; Vahtera, J.; Lewis, G.; Steptoe, A.; Kivimäki, M. Association between Depression and Physical Conditions Requiring Hospitalization. JAMA Psychiatry 2023. [Google Scholar] [CrossRef]
- Han, X.; Hou, C.; Yang, H.; Chen, W.; Ying, Z.; Hu, Y.; Sun, Y.; Qu, Y.; Yang, L.; Valdimarsdóttir, U.A.; et al. Disease trajectories and mortality among individuals diagnosed with depression: A community-based cohort study in UK Biobank. Mol. Psychiatry 2021, 26, 6736–6746. [Google Scholar] [CrossRef]
- Uher, R.; Zwicker, A. Etiology in psychiatry: Embracing the reality of poly-gene-environmental causation of mental illness. World Psychiatry 2017, 16, 121–129. [Google Scholar] [CrossRef] [Green Version]
- Fang, Y.; Scott, L.; Song, P.; Burmeister, M.; Sen, S. Genomic prediction of depression risk and resilience under stress. Nat. Hum. Behav. 2019, 4, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Herrman, H.; Patel, V.; Kieling, C.; Berk, M.; Buchweitz, C.; Cuijpers, P.; Furukawa, T.A.; Kessler, R.C.; Kohrt, B.A.; Maj, M.; et al. Time for united action on depression: A Lancet–World Psychiatric Association Commission. Lancet 2022, 399, 957–1022. [Google Scholar] [CrossRef] [PubMed]
- Howard, D.M.; Adams, M.J.; Clarke, T.-K.; Hafferty, J.D.; Gibson, J.; Shirali, M.; Coleman, J.R.I.; Hagenaars, S.P.; Ward, J.; Wigmore, E.M.; et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat. Neurosci. 2019, 22, 343–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferenczi, E.A.; Zalocusky, K.A.; Liston, C.; Grosenick, L.; Warden, M.R.; Amatya, D.; Katovich, K.; Mehta, H.; Patenaude, B.; Ramakrishnan, C.; et al. Prefrontal cortical regulation of brainwide circuit dynamics and reward-related behavior. Science 2016, 351, aac9698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duman, C.H.; Duman, R.S. Spine synapse remodeling in the pathophysiology and treatment of depression. Neurosci. Lett. 2015, 601, 20–29. [Google Scholar] [CrossRef] [Green Version]
- Ippolito, G.; Bertaccini, R.; Tarasi, L.; Di Gregorio, F.; Trajkovic, J.; Battaglia, S.; Romei, V. The Role of Alpha Oscillations among the Main Neuropsychiatric Disorders in the Adult and Developing Human Brain: Evidence from the Last 10 Years of Research. Biomedicines 2022, 10, 3189. [Google Scholar] [CrossRef]
- Watters, A.J.; Carpenter, J.S.; Harris, A.W.; Korgaonkar, M.S.; Williams, L.M. Characterizing neurocognitive markers of familial risk for depression using multi-modal imaging, behavioral and self-report measures. J. Affect. Disord. 2019, 253, 336–342. [Google Scholar] [CrossRef]
- McEwen, B.S.; Morrison, J.H. The Brain on Stress: Vulnerability and Plasticity of the Prefrontal Cortex over the Life Course. Neuron 2013, 79, 16–29. [Google Scholar] [CrossRef] [Green Version]
- Di Gregorio, F.; La Porta, F.; Petrone, V.; Battaglia, S.; Orlandi, S.; Ippolito, G.; Romei, V.; Piperno, R.; Lullini, G. Accuracy of EEG Biomarkers in the Detection of Clinical Outcome in Disorders of Consciousness after Severe Acquired Brain Injury: Preliminary Results of a Pilot Study Using a Machine Learning Approach. Biomedicines 2022, 10, 1897. [Google Scholar] [CrossRef]
- McClung, C.A. Circadian genes, rhythms and the biology of mood disorders. Pharmacol. Ther. 2007, 114, 222–232. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, A.J.; Lord, O.; Malone, D. Differences in the prescribing of medication for physical disorders in individuals with v. without mental illness: Meta-analysis. Br. J. Psychiatry 2012, 201, 435–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henderson, D.C.; Vincenzi, B.; Andrea, N.V.; Ulloa, M.; Copeland, P.M. Pathophysiological mechanisms of increased cardiometabolic risk in people with schizophrenia and other severe mental illnesses. Lancet Psychiatry 2015, 2, 452–464. [Google Scholar] [CrossRef] [PubMed]
- Sudarshan, Y.; Cheung, B.M.Y. Hypertension and psychosis. Postgrad. Med. J. 2022. [Google Scholar] [CrossRef] [PubMed]
- Li, G.H.-Y.; Cheung, C.-L.; Chung, A.K.-K.; Cheung, B.M.-Y.; Wong, I.C.-K.; Fok, M.L.Y.; Au, P.C.-M.; Sham, P.-C. Evaluation of bi-directional causal association between depression and cardiovascular diseases: A Mendelian randomization study. Psychol. Med. 2020, 52, 1765–1776. [Google Scholar] [CrossRef]
- Frank, P.; Jokela, M.; Batty, G.D.; Cadar, D.; Steptoe, A.; Kivimäki, M. Association between Systemic Inflammation and Individual Symptoms of Depression: A Pooled Analysis of 15 Population-Based Cohort Studies. Am. J. Psychiatry 2021, 178, 1107–1118. [Google Scholar] [CrossRef]
- Pitharouli, M.C.; Hagenaars, S.P.; Glanville, K.P.; Coleman, J.R.; Hotopf, M.; Lewis, C.M.; Pariante, C.M. Elevated C-Reactive Protein in Patients with Depression, Independent of Genetic, Health, and Psychosocial Factors: Results From the UK Biobank. Am. J. Psychiatry 2021, 178, 522–529. [Google Scholar] [CrossRef]
- Hiles, S.A.; Revesz, D.; Lamers, F.; Giltay, E.; Penninx, B.W. Bidirectional Prospective Associations of Metabolic Syndrome Components with Depression, Anxiety, and Antidepressant Use. Depress. Anxiety 2016, 33, 754–764. [Google Scholar] [CrossRef] [Green Version]
- National Center for Health Statistics, Centers for Disease Control and Prevention. NHANES Questionnaires, Datasets, and Related Documentation. Available online: https://wwwn.cdc.gov/nchs/nhanes/default.aspx (accessed on 10 August 2021).
- National Health and Nutrition Examination Survey. 1999–2000 Data Documentation, Codebook, and Frequencies: Mental Health—Depression (CIQMDEP). 2002. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/CIQMDEP.htm (accessed on 1 January 2023).
- National Health and Nutrition Examination Survey. 2005–2006 Data Documentation, Codebook, and Frequencies: Mental Health—Depression Screener (DPQ_D). 2008. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/DPQ_D.htm (accessed on 1 January 2023).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef] [Green Version]
- National Health and Nutrition Examination Survey. 1988–2020 Data Documentation, Codebook, and Frequencies: Prescription Medications—Drug Information (RXQ_DRUG). 2021. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/RXQ_DRUG.htm (accessed on 1 January 2023).
- National Health and Nutrition Examination Survey. 2017-March 2020 Data Documentation, Codebook, and Frequencies: Prescription Medications (P_RXQ_RX). 2021. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/P_RXQ_RX.htm (accessed on 1 January 2023).
- Rethorst, C.D.; Bernstein, I.; Trivedi, M.H. Inflammation, obesity, and metabolic syndrome in depression: Analysis of the 2009–2010 National Health and Nutrition Examination Survey (NHANES). J. Clin. Psychiatry 2014, 75, 9045. [Google Scholar] [CrossRef] [Green Version]
- Penninx, B.W. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neurosci. Biobehav. Rev. 2017, 74 Pt B, 277–286. [Google Scholar] [CrossRef]
- Lopresti, A.L.; Hood, S.D.; Drummond, P.D. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. J. Affect. Disord. 2013, 148, 12–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otte, C.; Gold, S.M.; Penninx, B.W.; Pariante, C.M.; Etkin, A.; Fava, M.; Mohr, D.C.; Schatzberg, A.F. Major depressive disorder. Nat. Rev. Dis. Prim. 2016, 2, 16065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milaneschi, Y.; Simmons, W.K.; van Rossum, E.F.C.; Penninx, B.W. Depression and obesity: Evidence of shared biological mechanisms. Mol. Psychiatry 2019, 24, 18–33. [Google Scholar] [CrossRef]
- Leonard, B.E. Inflammation and depression: A causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 2018, 30, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobrosly, R.; van Wijngaarden, E. Associations between immunologic, inflammatory, and oxidative stress markers with severity of depressive symptoms: An analysis of the 2005–2006 National Health and Nutrition Examination Survey. Neurotoxicology 2010, 31, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Esser, N.; Legrand-Poels, S.; Piette, J.; Scheen, A.J.; Paquot, N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res. Clin. Pract. 2014, 105, 141–150. [Google Scholar] [CrossRef] [Green Version]
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional Association between Depression and Metabolic Syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef] [Green Version]
- Van Reedt Dortland, A.K.; Giltay, E.J.; van Veen, T.; Zitman, F.G.; Penninx, B.W. Metabolic syndrome abnormalities are associated with severity of anxiety and depression and with tricyclic antidepressant use. Acta Psychiatr. Scand. 2010, 122, 30–39. [Google Scholar] [CrossRef]
- Licht, C.M.; de Geus, E.J.; Seldenrijk, A.; van Hout, H.P.; Zitman, F.G.; van Dyck, R.; Penninx, B.W. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension 2009, 53, 631–638. [Google Scholar] [CrossRef] [Green Version]
- Calvi, A.; Fischetti, I.; Verzicco, I.; Murri, M.B.; Zanetidou, S.; Volpi, R.; Coghi, P.; Tedeschi, S.; Amore, M.; Cabassi, A. Antidepressant drugs effects on blood pressure. Front. Cardiovasc. Med. 2021, 8, 704281. [Google Scholar] [CrossRef] [PubMed]
- Thom, R.P.; Alexander, J.L.; Baron, D.; Garakani, A.; Gross, L.; Pine, J.H.; Radhakrishnan, R.; Slaby, A.; Sumner, C.R. Selective Serotonin Reuptake Inhibitors: How Long Is Long Enough? J. Psychiatr. Pract. 2021, 27, 361–371. [Google Scholar] [CrossRef]
- Janssen, D.G.A.; Caniato, R.N.; Verster, J.C.; Baune, B.T. A psychoneuroimmunological review on cytokines involved in antidepressant treatment response. Hum. Psychopharmacol. Clin. Exp. 2010, 25, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, L.; Garner, B.; Dew, T.; Fazakerley, H.; Pariante, C. Antidepressants, but not antipsychotics, modulate GR function in human whole blood: An insight into molecular mechanisms. Eur. Neuropsychopharmacol. 2010, 20, 379–387. [Google Scholar] [CrossRef] [Green Version]
- Baumeister, H.; Hutter, N.; Bengel, J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus and depression. Cochrane Database Syst. Rev. 2012, 12, Cd008381. [Google Scholar] [CrossRef] [PubMed]
- Pizzi, C.; Rutjes, A.W.S.; Costa, G.M.; Fontana, F.; Mezzetti, A.; Manzoli, L. Meta-Analysis of Selective Serotonin Reuptake Inhibitors in Patients with Depression and Coronary Heart Disease. Am. J. Cardiol. 2011, 107, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Legg, L.A.; Rudberg, A.S.; Hua, X.; Wu, S.; Hackett, M.L.; Tilney, R.; Lindgren, L.; Kutlubaev, M.A.; Hsieh, C.F.; Barugh, A.J.; et al. Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery. Cochrane Database Syst. Rev. 2021, 11, Cd009286. [Google Scholar] [CrossRef] [Green Version]
- Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA 2003, 289, 3106–3116. [Google Scholar] [CrossRef] [Green Version]
- Martin, L.A.; Neighbors, H.W.; Griffith, D.M. The experience of symptoms of depression in men vs. women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry 2013, 70, 1100–1106. [Google Scholar] [CrossRef] [Green Version]
- Doyle, F.; McGee, H.; Conroy, R.; Conradi, H.J.; Meijer, A.; Steeds, R.; Sato, H.; Stewart, D.E.; Parakh, K.; Carney, R.; et al. Systematic Review and Individual Patient Data Meta-Analysis of Sex Differences in Depression and Prognosis in Persons with Myocardial Infarction: A MINDMAPS Study. Psychosom. Med. 2015, 77, 419–428. [Google Scholar] [CrossRef] [Green Version]

| Characteristic | Total (n = 15,315) | Hypertension | p Value | Raised Triglyceride | p Value | Reduced HDL-C | p Value | Central Obesity | p Value | Raised Blood Glucose | p Value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (n= 6952, 40.0 [38.7–41.3]) | (n = 3783, 24.4 [23.4–25.4]) | (n = 4259, 27.0 [25.8–28.2]) | (n = 8780, 56.3 [54.9–57.7]) | (n = 8493, 51.9 [50.5–53.4]) | |||||||
| Age, years | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| 20–44 | 45.5 (44.0–47.0) | 20.1 (18.8–21.6) | 39.1 (36.6–41.6) | 49.2 (47.1–51.2) | 37.5 (35.9–39.2) | 31.9 (30.1–33.7) | |||||
| 45–64 | 36.4 (35.2–37.6) | 46.1 (44.6–47.7) | 41.7 (39.3–44.1) | 35.7 (33.8–37.6) | 39.9 (38.6–41.3) | 42.7 (41.1–44.3) | |||||
| ≥65 | 18.2 (17.2–19.2) | 33.7 (32.1–35.4) | 19.2 (17.7–20.9) | 15.1 (13.7–16.7) | 22.5 (21.3–23.8) | 25.5 (24.1–26.8) | |||||
| Women | 50.6 (49.7–51.6) | 48.3 (46.9–49.7) | <0.001 | 43.0 (40.9–45.0) | <0.001 | 54.5 (52.6–56.5) | <0.001 | 60.0 (58.6–61.5) | <0.001 | 43.0 (41.6–44.5) | <0.001 |
| Race/ethnicity | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Non-Hispanic White | 67.8 (65.4–70.1) | 69.1 (66.2–71.9) | 71.5 (68.8–74.0) | 66.7 (63.7–69.6) | 69.8 (67.1–72.4) | 67.8 (65.3–70.3) | |||||
| Non-Hispanic Black | 10.8 (9.6–12.2) | 14.0 (12.2–16.0) | 5.2 (4.4–6.2) | 9.1 (7.8–10.6) | 11.3 (9.9–13.0) | 9.8 (8.6–11.1) | |||||
| Mexican American | 8.4 (7.2–9.7) | 5.8 (4.8–7.0) | 10.2 (8.7–11.9) | 10.0 (8.5–11.7) | 8.4 (7.1–10.0) | 9.1 (7.8–10.7) | |||||
| Other Hispanic | 5.7 (4.8–6.6) | 4.6 (3.8–5.6) | 5.7 (4.5–7.1) | 6.9 (5.8–8.2) | 5.3 (4.5–6.3) | 5.7 (4.8–6.7) | |||||
| Other race | 7.3 (6.6–8.2) | 6.5 (5.6–7.5) | 7.4 (6.4–8.6) | 7.3 (6.2–8.6) | 5.1 (4.4–5.9) | 7.6 (6.7–8.6) | |||||
| Education | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| <High school | 15.1 (14.0–16.3) | 17.3 (16.0–18.7) | 18.3 (16.7–20.0) | 18.9 (17.3–20.6) | 15.7 (14.5–17.0) | 17.4 (16.1–18.8) | |||||
| High school | 23.5 (22.3–24.8) | 27 (25.4–28.8) | 25.1 (22.9–27.5) | 24.7 (22.6–26.9) | 24.6 (23.3–26.0) | 25.6 (24.1–27.2) | |||||
| Some college | 31.0 (29.8–32.3) | 31 (29.1–32.9) | 32.1 (30.0–34.3) | 33.0 (30.8–35.2) | 33.3 (31.8–34.9) | 29.6 (28–31.4) | |||||
| College or higher | 30.4 (28.4–32.4) | 24.7 (22.6–26.9) | 24.5 (22.1–27.1) | 23.4 (21.2–25.9) | 26.3 (24.3–28.5) | 27.3 (25.3–29.5) | |||||
| Family income-to-poverty ratio | 0.05 | 0.09 | <0.001 | <0.001 | 0.16 | ||||||
| <130% | 20.0 (18.6–21.4) | 19.3 (17.7–21.1) | 21.2 (19.4–23.2) | 25.2 (23.3–27.2) | 20.4 (18.9–22.0) | 19.8 (18.4–21.3) | |||||
| 130–349% | 36.1 (34.8–37.5) | 37.7 (35.9–39.5) | 36.8 (34.7–38.9) | 38.5 (36.4–40.7) | 38.0 (36.1–39.8) | 37.2 (35.5–38.9) | |||||
| ≥350% | 43.9 (42.0–45.9) | 42.9 (40.6–45.4) | 42.0 (39.6–44.5) | 36.3 (33.3–39.4) | 41.6 (39.3–44.0) | 43.0 (40.8–45.3) | |||||
| Health insurance | 82.9 (81.7–84.0) | 88.0 (86.8–89.1) | <0.001 | 82.5 (80.5–84.3) | 0.54 | 80.0 (78.3–81.7) | <0.001 | 85.7 (84.4–86.9) | <0.001 | 84.8 (83.6–86.0) | <0.001 |
| Marital status | <0.001 | <0.001 | 0.54 | <0.001 | <0.001 | ||||||
| Married/Living with Partner | 64.3 (62.6–65.9) | 65.3 (63.3–67.2) | 67.3 (64.7–69.9) | 64.5 (62.0–67.0) | 65.7 (63.6–67.8) | 66.7 (64.7–68.7) | |||||
| Widowed/Divorced/Separated | 17.7 (16.7–18.7) | 24.3 (22.7–25.9) | 19.1 (17.4–21.0) | 18.1 (16.6–19.7) | 20.6 (19.2–22.0) | 20.7 (19.2–22.2) | |||||
| Never married | 18.1 (16.8–19.4) | 10.5 (9.5–11.6) | 13.5 (11.8–15.4) | 17.3 (15.4–19.4) | 13.7 (12.4–15.0) | 12.6 (11.3–14.1) | |||||
| BMI, kg/m2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Normal (<25) | 29.6 (28.5–30.7) | 18.7 (17.6–19.9) | 13.0 (11.6–14.4) | 13.7 (12.3–15.3) | 4.8 (4.1–5.6) | 18.4 (17.3–19.6) | |||||
| Overweight (25–<30) | 33.2 (32.4–34.1) | 32.3 (30.9–33.8) | 35.4 (33.6–37.2) | 30.6 (28.7–32.6) | 31.3 (29.9–32.7) | 34.0 (32.8–35.3) | |||||
| Obese (≥30) | 37.2 (36.1–38.4) | 49.0 (47.3–50.6) | 51.6 (49.5–53.7) | 55.7 (53.4–58.0) | 63.9 (62.4–65.4) | 47.6 (46.1–49.1) | |||||
| Physical activity | <0.001 | 0.04 | 0.17 | <0.001 | 0.17 | ||||||
| Little/None | 49.9 (48.5–51.3) | 52.5 (50.7–54.3) | 48.3 (46.0–50.7) | 51.3 (49.3–53.4) | 51.6 (50.1–53.2) | 50.6 (48.9–52.3) | |||||
| Moderate | 25.3 (24.2–26.4) | 26.1 (24.5–27.7) | 27.3 (25.2–29.6) | 25.0 (23.1–27.1) | 26.4 (25.1–27.7) | 25.4 (24.0–26.9) | |||||
| Vigorous | 24.9 (23.8–26) | 21.4 (20–22.9) | 24.3 (22.5–26.3) | 23.6 (21.9–25.5) | 22.0 (20.7–23.2) | 24.0 (22.7–25.4) | |||||
| Current smoking | 19.7 (18.5–20.8) | 17.3 (16.0–18.7) | <0.001 | 22.7 (21–24.5) | <0.001 | 24.8 (22.9–26.8) | <0.001 | 17.2 (16.0–18.5) | <0.001 | 18.4 (17.2–19.8) | 0.01 |
| Alcohol consumption | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Non-drinker | 21.3 (20.1–22.6) | 26.8 (25.2–28.5) | 23.5 (21.7–25.4) | 26.5 (24.6–28.5) | 24.8 (23.3–26.4) | 23.3 (21.8–24.8) | |||||
| Moderate drinker | 62.8 (61.1–64.4) | 59.4 (57.2–61.5) | 57.6 (54.9–60.2) | 55.5 (53.2–57.9) | 60.0 (58.1–61.8) | 61.7 (59.8–63.6) | |||||
| Heavy drinker | 15.9 (15–16.8) | 13.8 (12.6–15.2) | 18.9 (17.0–20.9) | 18.0 (16.4–19.7) | 15.2 (14.2–16.4) | 15.0 (13.8–16.3) | |||||
| Depressive symptoms | 0.01 | <0.001 | <0.001 | <0.001 | 0.08 | ||||||
| Normal | 77.6 (76.6–78.6) | 76.0 (74.5–77.5) | 72.7 (70.7–74.7) | 73.1 (71–75.2) | 74.7 (73.3–76.0) | 76.7 (75.2–78.2) | |||||
| Mild | 15.4 (14.6–16.3) | 16.0 (14.7–17.3) | 18.0 (16.4–19.8) | 17.4 (15.6–19.3) | 17.1 (15.9–18.3) | 15.7 (14.5–17.0) | |||||
| Moderate | 4.6 (4.2–5.1) | 5.4 (4.7–6.2) | 6.1 (5.2–7.3) | 6.1 (5.3–7.1) | 5.5 (4.9–6.2) | 5.0 (4.4–5.7) | |||||
| Severe | 2.3 (2–2.6) | 2.6 (2.1–3.2) | 3.1 (2.5–3.8) | 3.4 (2.7–4.1) | 2.7 (2.4–3.2) | 2.6 (2.2–3.0) | |||||
| Antidepressants use | 12.6 (11.8–13.4) | 16.5 (15.4–17.8) | <0.001 | 17.2 (15.3–19.3) | <0.001 | 14.6 (13–16.3) | 0.003 | 16.3 (15.2–17.4) | <0.001 | 13.7 (12.8–14.8) | <0.001 |
| Characteristic | Total (n = 15,315) | None | One | Two | Three | Four | Five | p Value |
|---|---|---|---|---|---|---|---|---|
| (n = 2230, 17.1 [16.1–18.2]) | (n = 3322, 23.3 [22.3–24.3]) | (n = 3701, 23.2 [22.2–24.2]) | (n = 3483, 20.7 [19.8–21.6]) | (n = 1801, 10.8 [10.1–11.6]) | (n = 778, 4.9 [4.5–5.4]) | |||
| Age, years | ||||||||
| 20–44 | 45.5 (44.0–47.0) | 71.9 (69.4–74.3) | 56.8 (54.4–59.1) | 40.8 (38.2–43.5) | 32.0 (29.6–34.4) | 26.5 (23.9–29.3) | 20.6 (16.8–24.9) | <0.001 |
| 45–64 | 36.4 (35.2–37.6) | 23.7 (21.4–26.1) | 31.9 (29.7–34.2) | 39.0 (36.6–41.4) | 40.3 (38.3–42.4) | 47.6 (44.6–50.6) | 47.8 (43.5–52.1) | |
| ≥65 | 18.2 (17.2–19.2) | 4.4 (3.5–5.6) | 11.3 (9.8–13) | 20.2 (18.4–22.1) | 27.7 (25.5–30) | 25.9 (23.9–27.9) | 31.6 (27.7–35.8) | |
| Women | 50.6 (49.7–51.6) | 53.7 (50.8–56.5) | 48.8 (46.3–51.4) | 50.6 (48.4–52.8) | 49.3 (47.1–51.5) | 50.5 (46.6–54.4) | 54.3 (50.0–58.6) | 0.08 |
| Race/ethnicity | ||||||||
| Non-Hispanic White | 67.8 (65.4–70.1) | 68.5 (65.7–71.2) | 65.7 (62.6–68.7) | 65.8 (62.8–68.7) | 68.1 (64.9–71.2) | 70.2 (66.8–73.4) | 77.6 (73.6–81.2) | <0.001 |
| Non-Hispanic Black | 10.8 (9.6–12.2) | 10.3 (8.9–11.8) | 11.1 (9.6–12.9) | 11.9 (10.4–13.6) | 12.0 (10.4–14) | 8.7 (7.3–10.4) | 5.7 (4.3–7.6) | |
| Mexican American | 8.4 (7.2–9.7) | 7.0 (5.9–8.3) | 8.8 (7.4–10.5) | 9.0 (7.5–10.8) | 8.5 (7.2–10.0) | 8.8 (7.1–10.8) | 6.9 (5.2–9.2) | |
| Other Hispanic | 5.7 (4.8–6.6) | 5.4 (4.2–6.8) | 6.3 (5.2–7.6) | 6.0 (5.0–7.2) | 5.1 (4.2–6.1) | 5.3 (4.3–6.6) | 5.4 (3.8–7.6) | |
| Other race | 7.3 (6.6–8.2) | 8.9 (7.5–10.5) | 8.0 (6.9–9.3) | 7.3 (6.2–8.5) | 6.3 (5.2–7.6) | 6.9 (5.5–8.7) | 4.3 (2.6–7.2) | |
| Education | ||||||||
| <High school | 15.1 (14.0–16.3) | 9.6 (8.1–11.3) | 13.2 (11.6–15.0) | 16.5 (14.9–18.1) | 17.7 (16.0–19.6) | 17.5 (15.4–19.9) | 20.7 (17.9–23.9) | <0.001 |
| High school | 23.5 (22.3–24.8) | 18.0 (15.8–20.4) | 22.3 (20.1–24.7) | 23.8 (21.6–26.2) | 26.5 (24.5–28.5) | 27.9 (24.7–31.3) | 24.4 (21.1–28.1) | |
| Some college | 31.0 (29.8–32.3) | 30.4 (27.7–33.1) | 29.9 (27.7–32.1) | 30.9 (28.9–33) | 31.7 (29.7–33.9) | 32.3 (28.9–35.9) | 33.8 (29.3–38.7) | |
| College or higher | 30.4 (28.4–32.4) | 42.1 (38.8–45.5) | 34.6 (31.8–37.6) | 28.8 (26–31.7) | 24.1 (21.9–26.4) | 22.3 (19.2–25.8) | 21 (16.9–25.8) | |
| Family income-to-poverty ratio | ||||||||
| <130% | 20.0 (18.6–21.4) | 18.1 (16.3–20.0) | 19.2 (17.2–21.3) | 19.7 (17.8–21.7) | 22.0 (19.8–24.5) | 20.8 (18.3–23.5) | 21.4 (18.4–24.7) | <0.001 |
| 130–349% | 36.1 (34.8–37.5) | 31.1 (28.4–33.8) | 35.8 (33.6–38.0) | 37.1 (34.8–39.5) | 37.8 (35.2–40.6) | 39.2 (36.1–42.5) | 37.0 (32.7–41.5) | |
| ≥350% | 43.9 (42.0–45.9) | 50.9 (47.5–54.2) | 45.1 (42.5–47.7) | 43.2 (40.2–46.2) | 40.1 (36.9–43.5) | 40.0 (36.4–43.7) | 41.6 (36.6–46.8) | |
| Health insurance | 82.9 (81.7–84) | 79.5 (76.9–81.8) | 80.8 (78.8–82.6) | 82.4 (80.5–84.2) | 85.7 (84.0–87.2) | 85.7 (83.6–87.6) | 89.1 (86.5–91.2) | <0.001 |
| Marital status | ||||||||
| Married/Living with Partner | 64.3 (62.6–65.9) | 58.3 (55.6–61.0) | 64.1 (61.6–66.5) | 65.2 (62.6–67.8) | 66.7 (64.1–69.3) | 66.4 (62.5–70.0) | 66.1 (61.4–70.4) | <0.001 |
| Widowed/Divorced/Separated | 17.7 (16.7–18.7) | 9.5 (8.2–11.0) | 15.1 (13.5–16.8) | 18.8 (17.1–20.6) | 21.9 (20.1–23.9) | 23.1 (20.2–26.3) | 23.4 (20–27.3) | |
| Never married | 18.1 (16.8–19.4) | 32.1 (29.6–34.8) | 20.8 (18.6–23.2) | 16.0 (14.1–18.0) | 11.3 (9.9–12.9) | 10.5 (8.6–12.9) | 10.5 (8.0–13.8) | |
| BMI, kg/m2 | ||||||||
| Normal (<25) | 29.6 (28.5–30.7) | 74.8 (72.5–77.0) | 41.8 (39.6–44.0) | 20.6 (19.0–22.2) | 8.3 (7.1–9.8) | 4.0 (3.1–5.0) | 1.8 (1.1–3.0) | <0.001 |
| Overweight (25–<30) | 33.2 (32.4–34.1) | 23.3 (21.2–25.6) | 38.6 (36.6–40.6) | 41.7 (39.2–44.1) | 32.4 (30.4–34.5) | 26.0 (23.4–28.8) | 22.0 (18.4–26.2) | |
| Obese (≥30) | 37.2 (36.1–38.4) | 1.8 (1.3–2.7) | 19.6 (17.8–21.5) | 37.8 (35.5–40.2) | 59.3 (56.7–61.8) | 70.0 (67.3–72.7) | 76.2 (72–79.9) | |
| Physical activity | ||||||||
| Little/None | 49.9 (48.5–51.3) | 48.4 (45.4–51.4) | 47.4 (45.1–49.7) | 50.9 (48.5–53.3) | 50.5 (48.2–52.9) | 50.7 (47.3–54.0) | 57.1 (52.3–61.8) | <0.001 |
| Moderate | 25.3 (24.2–26.4) | 23.9 (21.9–26.1) | 24.2 (22.2–26.3) | 25.1 (23.0–27.3) | 26.2 (24.1–28.5) | 28.8 (26.2–31.5) | 23.9 (19.7–28.7) | |
| Vigorous | 24.9 (23.8–26) | 27.7 (25.4–30.2) | 28.4 (26.0–31.0) | 24.0 (21.9–26.2) | 23.2 (21.3–25.3) | 20.6 (18.0–23.4) | 19.0 (15.6–22.9) | |
| Current smoking | 19.7 (18.5–20.8) | 20.4 (18.3–22.6) | 20.3 (18.4–22.3) | 19.6 (17.7–21.8) | 19.2 (17.5–21.0) | 18.6 (16.1–21.3) | 18.8 (15.8–22.2) | 0.80 |
| Alcohol consumption | ||||||||
| Non-drinker | 21.3 (20.1–22.6) | 15.4 (13.3–17.7) | 16.4 (14.9–18.1) | 22.0 (20.3–23.8) | 24.6 (22.5–26.9) | 27.7 (25.1–30.5) | 33.9 (30.0–38.1) | <0.001 |
| Moderate drinker | 62.8 (61.1–64.4) | 68.9 (65.8–71.7) | 67.5 (65.2–69.7) | 62.2 (60.0–64.3) | 58.0 (55.2–60.7) | 57.2 (53.6–60.8) | 53.9 (49.0–58.8) | |
| Heavy drinker | 15.9 (15–16.8) | 15.7 (14.0–17.7) | 16.1 (14.4–17.9) | 15.8 (14.2–17.5) | 17.4 (15.5–19.4) | 15.1 (12.8–17.7) | 12.1 (9.4–15.6) | |
| Depressive symptoms | ||||||||
| Normal | 77.6 (76.6–78.6) | 83.0 (81.1–84.8) | 79.4 (77.4–81.3) | 77.6 (75.6–79.5) | 76.3 (74.2–78.2) | 72.8 (69.6–75.8) | 67.0 (63.0–70.8) | <0.001 |
| Mild | 15.4 (14.6–16.3) | 12.9 (11.2–14.7) | 14.4 (12.9–16.1) | 15.7 (14.2–17.4) | 16.3 (14.6–18.1) | 17.3 (14.9–20.0) | 20.2 (17.1–23.6) | |
| Moderate | 4.6 (4.2–5.1) | 3.2 (2.5–4.1) | 4.0 (3.1–5.1) | 4.3 (3.6–5.1) | 4.9 (4.1–5.9) | 6.4 (5.0–8.1) | 9.3 (6.9–12.4) | |
| Severe | 2.3 (2.0–2.6) | 1.0 (0.7–1.4) | 2.2 (1.7–2.8) | 2.4 (1.8–3.2) | 2.5 (2.0–3.2) | 3.5 (2.6–4.7) | 3.5 (2.4–5.1) | |
| Antidepressants use | 12.6 (11.8–13.4) | 7.5 (6.1–9.2) | 9.6 (8.1–11.2) | 11.6 (10.1–13.2) | 15.5 (14.0–17.1) | 18.4 (15.9–21.2) | 23.9 (19.9–28.3) | <0.001 |
| Individual MetS Components | |||||
| Depressive symptoms | Hypertension | Raised triglyceride | Reduced HDL-C | Central obesity | Raised blood glucose |
| Normal | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Mild | 1.12 (0.97–1.29) | 1.30 (1.12–1.52) | 1.05 (0.90–1.24) | 1.08 (0.89–1.32) | 1.12 (0.95–1.32) |
| Moderate | 1.37 (1.09–1.72) | 1.63 (1.25–2.14) | 1.22 (1.00–1.49) | 1.82 (1.21–2.74) | 1.37 (1.05–1.79) |
| Severe | 1.23 (0.82–1.84) | 1.44 (1.05–1.97) | 1.18 (0.87–1.59) | 1.00 (0.63–1.61) | 1.36 (0.98–1.90) |
| Clustered Number of MetS Components | |||||
| Depressive symptoms | One | Two | Three | Four | Five |
| Normal | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Mild | 1.15 (0.94–1.41) | 1.23 (0.96–1.58) | 1.25 (0.96–1.62) | 1.34 (0.99–1.83) | 1.82 (1.25–2.67) |
| Moderate | 1.52 (1.00–2.31) | 1.69 (1.09–2.62) | 1.90 (1.24–2.91) | 2.63 (1.52–4.55) | 4.31 (2.45–7.60) |
| Severe | 2.08 (1.29–3.37) | 2.11 (1.24–3.62) | 2.21 (1.18–4.12) | 3.04 (1.68–5.51) | 3.35 (1.57–7.14) |
| Individual MetS Components | |||||
| Hypertension | Raised triglyceride | Reduced HDL-C | Central obesity | Raised blood glucose | |
| Antidepressant use | 1.40 (1.14–1.72) | 1.43 (1.17–1.74) | 1.01 (0.84–1.22) | 1.14 (0.88–1.48) | 1.03 (0.88–1.21) |
| Clustered Number of MetS Components | |||||
| One | Two | Three | Four | Five | |
| Antidepressant use | 1.07 (0.78–1.47) | 1.04 (0.75–1.44) | 1.32 (0.88–1.97) | 1.44 (0.99–2.09) | 1.74 (1.13–2.68) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Z.; Chan, Y.-H.; Cheung, B.M.Y. Dissecting Relations between Depression Severity, Antidepressant Use, and Metabolic Syndrome Components in the NHANES 2005–2020. J. Clin. Med. 2023, 12, 3891. https://doi.org/10.3390/jcm12123891
Lin Z, Chan Y-H, Cheung BMY. Dissecting Relations between Depression Severity, Antidepressant Use, and Metabolic Syndrome Components in the NHANES 2005–2020. Journal of Clinical Medicine. 2023; 12(12):3891. https://doi.org/10.3390/jcm12123891
Chicago/Turabian StyleLin, Ziying, Yap-Hang Chan, and Bernard Man Yung Cheung. 2023. "Dissecting Relations between Depression Severity, Antidepressant Use, and Metabolic Syndrome Components in the NHANES 2005–2020" Journal of Clinical Medicine 12, no. 12: 3891. https://doi.org/10.3390/jcm12123891
APA StyleLin, Z., Chan, Y.-H., & Cheung, B. M. Y. (2023). Dissecting Relations between Depression Severity, Antidepressant Use, and Metabolic Syndrome Components in the NHANES 2005–2020. Journal of Clinical Medicine, 12(12), 3891. https://doi.org/10.3390/jcm12123891





