The Effect of Age on Peri-Operative Outcomes after FEVAR
Abstract
1. Introduction
2. Materials and Methods
2.1. IRB Approval
2.2. Design
2.3. Participants
2.4. Analysis
3. Results
3.1. Sample Characteristics
3.2. Association of Post-Operative Mortality and Age
3.3. Age and Further Procedure-Related Outcomes
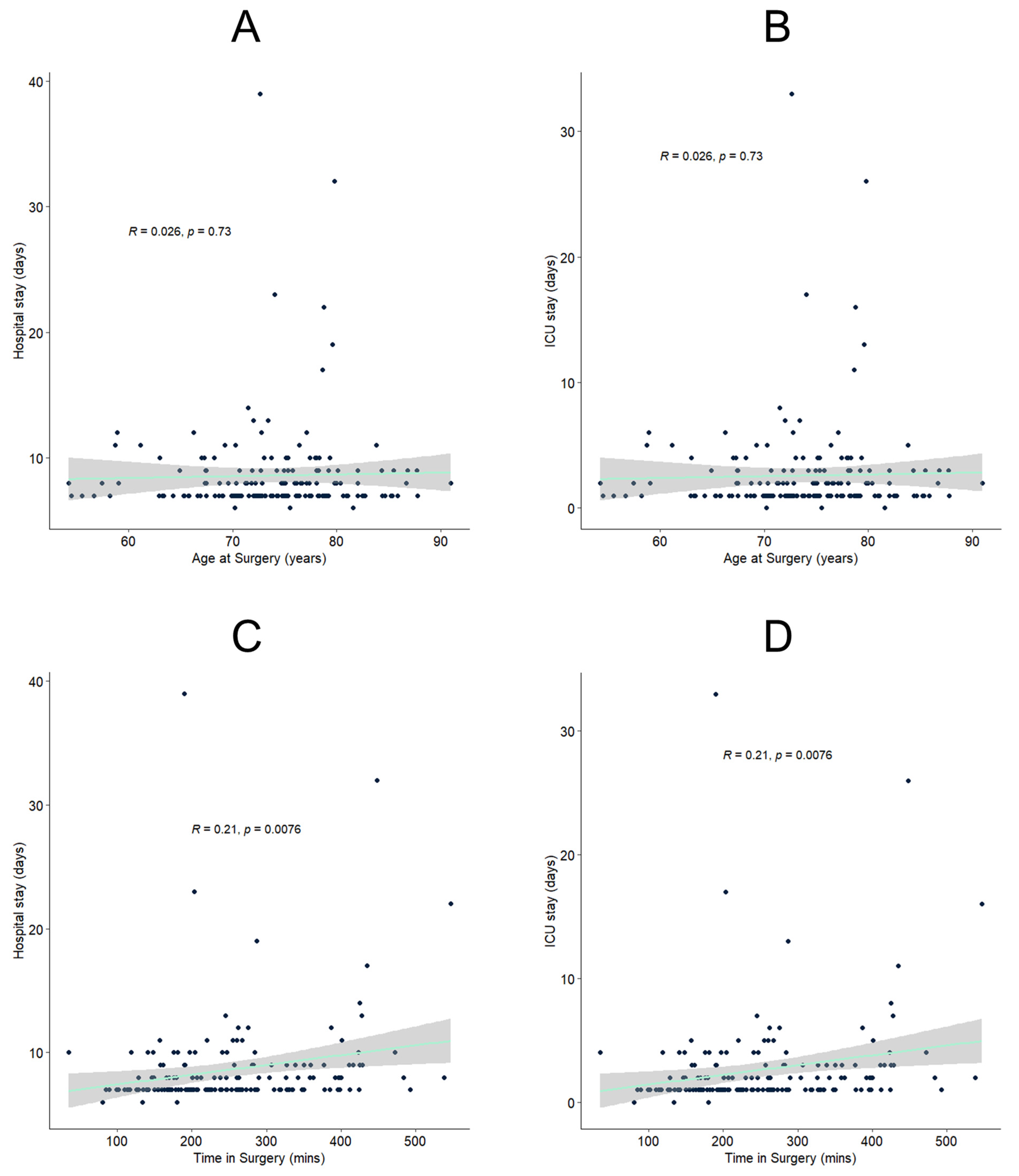
3.4. Factors Associated with Hospital and ICU Stay Length
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. World Report on Ageing and Health. 2015. Available online: https://www.who.int/publications/i/item/9789241565042 (accessed on 9 May 2023).
- Ortman, J.M.; Velkoff, V.A.; Hogan, H. An aging nation: The older population in the United States. Econ. Stat. Adm. US Dep. Commer. 2014, 1964, 1–28. [Google Scholar]
- Savji, N.; Rockman, C.B.; Skolnick, A.H.; Guo, Y.; Adelman, M.A.; Riles, T.; Berger, J.S. Association between advanced age and vascular disease in different arterial territories: A population database of over 3.6 million subjects. J. Am. Coll. Cardiol. 2013, 61, 1736–1743. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.W.; Sedrakyan, A.; Mao, J.; Venermo, M.; Faizer, R.; Debus, S.; Behrendt, C.-A.; Scali, S.T.; Altreuther, M.; Schermerhorn, M.; et al. Variations in Abdominal Aortic Aneurysm Care: A Report From the International Consortium of Vascular Registries. Circulation 2016, 134, 1948–1958. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.R.; Jackson, C.R.; Helenowski, I.B.; Verta, M.J.; Wilkinson, J.B.; Kim, S.; Hoel, A.W. A comparison of results of carotid endarterectomy in octogenarians and nonagenarians to younger patients from the Mid-America Vascular Study Group and the Society for Vascular Surgery Vascular Quality Initiative. J. Vasc. Surg. 2017, 65, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Halandras, P.M. Vascular Surgery and Geriatric Patients. Clin. Geriatr. Med. 2019, 35, 93–101. [Google Scholar] [CrossRef]
- Schwarze, M.L.; Shen, Y.; Hemmerich, J.; Dale, W. Age-related trends in utilization and outcome of open and endovascular repair for abdominal aortic aneurysm in the United States, 2001–2006. J. Vasc. Surg. 2009, 50, 722–729.e2. [Google Scholar] [CrossRef]
- Han, Y.; Zhang, S.; Zhang, J.; Ji, C.; Eckstein, H.-H. Outcomes of Endovascular Abdominal Aortic Aneurysm Repair in Octogenarians: Meta-analysis and Systematic Review. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 454–463. [Google Scholar] [CrossRef]
- Hahl, T.; Protto, S.; Järvenpää, V.; Uurto, I.; Väärämäki, S.; Suominen, V. Long-term outcomes of endovascular aneurysm repair according to instructions for use adherence status. J. Vasc. Surg. 2022, 76, 699–706.e2. [Google Scholar] [CrossRef]
- Oliveira-Pinto, J.; Oliveira, N.; Bastos-Gonçalves, F.; Hoeks, S.; Van Rijn, M.J.; Raa, S.T.; Mansilha, A.; Verhagen, H.J. Long-term results of outside “instructions for use” EVAR. J. Cardiovasc. Surg. 2017, 58, 252–260. [Google Scholar] [CrossRef]
- Taher, F.; Falkensammer, J.; McCarte, J.; Strassegger, J.; Uhlmann, M.; Schuch, P.; Assadian, A. The influence of prototype testing in three-dimensional aortic models on fenestrated endograft design. J. Vasc. Surg. 2017, 65, 1591–1597. [Google Scholar] [CrossRef]
- Kliewer, M.E.; Bordet, M.; Chavent, B.; Reijnen, M.M.P.J.; Frisch, N.; Midy, D.; Feugier, P.; Millon, A.; Lardenoije, J.-W.; Assadian, A.; et al. Assessment of fenestrated Anaconda stent graft design by numerical simulation: Results of a European prospective multicenter study. J. Vasc. Surg. 2022, 75, 99–108.e2. [Google Scholar] [CrossRef]
- Kliewer, M.; Pelanek-Völk, E.; Plimon, M.; Taher, F.; Assadian, A.; Falkensammer, J. Exclusion of complex aortic aneurysm with chimney endovascular aortic repair is applicable in a minority of patients treated with fenestrated endografts. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 460–466. [Google Scholar] [CrossRef]
- Oderich, G.S.; Farber, M.A.; Schneider, D.; Makaroun, M.; Sanchez, L.A.; Schanzer, A.; Beck, A.W.; Starnes, B.W.; Fillinger, M.; Tenorio, E.R.; et al. Final 5-year results of the United States Zenith Fenestrated prospective multicenter study for juxtarenal abdominal aortic aneurysms. J. Vasc. Surg. 2021, 73, 1128–1138.e2. [Google Scholar] [CrossRef]
- Oderich, G.S.; Greenberg, R.K.; Farber, M.; Lyden, S.; Sanchez, L.; Fairman, R.; Jia, F.; Bharadwaj, P. Results of the United States multicenter prospective study evaluating the Zenith fenestrated endovascular graft for treatment of juxtarenal abdominal aortic aneurysms. J. Vasc. Surg. 2014, 60, 1420–1428.e5. [Google Scholar] [CrossRef]
- Schanzer, A.; Beck, A.W.; Eagleton, M.; Farber, M.A.; Oderich, G.; Schneider, D.; Sweet, M.P.; Crawford, A.; Timaran, C. Results of fenestrated and branched endovascular aortic aneurysm repair after failed infrarenal endovascular aortic aneurysm repair. J. Vasc. Surg. 2020, 72, 849–858. [Google Scholar] [CrossRef]
- Taher, F.; Assadian, A.; Strassegger, J.; Duschek, N.; Koulas, S.; Senekowitsch, C.; Falkensammer, J. Pararenal Aortic Ulcer Repair. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 504–510. [Google Scholar] [CrossRef]
- Taher, F.; Falkensammer, J.; Nguyen, J.; Uhlmann, M.; Skrinjar, E.; Assadian, A. Assessing the institutional learning curve for pararenal aortic repair using the fenestrated Anaconda endograft. Vascular 2019, 27, 46–50. [Google Scholar] [CrossRef]
- Hertault, A.; Sobocinski, J.; Kristmundsson, T.; Maurel, B.; Dias, N.V.; Azzaoui, R.; Sonesson, B.; Resch, T.; Haulon, S. Results of F-EVAR in octogenarians. Ann. Vasc. Surg. 2014, 28, 1396–1401. [Google Scholar] [CrossRef]
- Motta, F.; Oderich, G.S.; Tenorio, E.R.; Schanzer, A.; Timaran, C.H.; Schneider, D.; Sweet, M.P.; Beck, A.W.; Eagleton, M.J.; Farber, M.A. Fenestrated-branched endovascular aortic repair is a safe and effective option for octogenarians in treating complex aortic aneurysm compared with nonoctogenarians. J. Vasc. Surg. 2021, 74, 353–362.e1. [Google Scholar] [CrossRef]
- Zil-E-Ali, A.; Aziz, F.; Medina, D.; Nejim, B.; Radtka, J.F. Fenestrated endovascular abdominal aortic aneurysm repair in octogenarians is associated with higher mortality and an increased incidence of nonhome discharge. J. Vasc. Surg. 2022, 75, 1846–1854.e7. [Google Scholar] [CrossRef]
- Kanasi, E.; Ayilavarapu, S.; Jones, J. The aging population: Demographics and the biology of aging. Periodontol. 2000 2016, 72, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Basa, C.D.; Kaya Bicer, E.; Aydogdu, S.; Sur, H. How Long Do Octogenarians Benefit From Knee Arthroplasty? Cureus 2021, 13, e14997. [Google Scholar] [CrossRef] [PubMed]
- Trigueros-Larrea, J.M.; Gonzalez-Bedia, M.A.; Lomo-Garrote, J.M.; Martin-de la Cal, O.; Martin-Ferrero, M.A. Total Knee Arthroplasty in Octogenarians: Should We Still Be so Restrictive? Geriatrics 2021, 6, 67. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.; Fu, H.; Cheung, M.H.; Chan, W.K.V.; Chan, P.K.; Yan, C.H.; Chiu, K.-Y. How well do elderly patients do after total knee arthroplasty in the era of fast-track surgery? Arthroplasty 2020, 2, 16. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Sun, X.; Zhang, X. Influence of Age-Related Complications on Clinical Outcome in Patients With Small Ruptured Cerebral Aneurysms. Front. Neurol. 2020, 11, 131. [Google Scholar] [CrossRef]
- Silva, N.A.; Shao, B.; Sylvester, M.J.; Eloy, J.A.; Gandhi, C.D. Unruptured aneurysms in the elderly: Perioperative outcomes and cost analysis of endovascular coiling and surgical clipping. Neurosurg. Focus 2018, 44, E4. [Google Scholar] [CrossRef]
- Massarweh, N.N.; Legner, V.J.; Symons, R.G.; McCormick, W.C.; Flum, D.R. Impact of advancing age on abdominal surgical outcomes. Arch. Surg. 2009, 144, 1108–1114. [Google Scholar] [CrossRef]
- Polanczyk, C.A.; Marcantonio, E.; Goldman, L.; Rohde, L.E.; Orav, J.; Mangione, C.M.; Lee, T.H. Impact of age on perioperative complications and length of stay in patients undergoing noncardiac surgery. Ann. Intern. Med. 2001, 134, 637–643. [Google Scholar] [CrossRef]
- Shepherd, S.J.; Creber, N.; Mansour, K.; Wiesenfeld, D.; Iseli, T.A.; Amott, D. Relationship between age, comorbidities and complications in head and neck cancer patients undergoing curative surgery. ANZ J. Surg. 2020, 90, 851–855. [Google Scholar] [CrossRef]
- Henstra, L.; Yazar, O.; de Niet, A.; Tielliu, I.F.J.; Schurink, G.W.H.; Zeebregts, C.J. Outcome of Fenestrated Endovascular Aneurysm Repair in Octogenarians: A Retrospective Multicentre Analysis. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 24–30. [Google Scholar] [CrossRef]
- Mahmood, D.N.; Forbes, S.M.; Rocha, R.; Tan, K.; Ouzounian, M.; Chung, J.C.-Y.; Lindsay, T.F. Outcomes in octogenarians after thoracoabdominal and juxtarenal aortic aneurysm repair using fenestrated-branched devices justifies treatment. J. Vasc. Surg. 2023, 77, 694–703.e3. [Google Scholar] [CrossRef]
- Makaloski, V.; Kölbel, T.; Rohlffs, F.; Behrendt, C.-A.; Law, Y.; Debus, E.S.; Tsilimparis, N. Early Outcomes After Branched and Fenestrated Endovascular Aortic Repair in Octogenarians. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 818–825. [Google Scholar] [CrossRef]
- Timaran, D.E.; Knowles, M.; Ali, T.; Timaran, C.H. Fenestrated endovascular aneurysm repair among octogenarians at high and standard risk for open repair. J. Vasc. Surg. 2017, 66, 354–359. [Google Scholar] [CrossRef]
- Locham, S.; Faateh, M.; Dakour-Aridi, H.; Nejim, B.; Malas, M. Octogenarians Undergoing Open Repair Have Higher Mortality Compared with Fenestrated Endovascular Repair of Intact Abdominal Aortic Aneurysms Involving the Visceral Vessels. Ann. Vasc. Surg. 2018, 51, 192–199. [Google Scholar] [CrossRef]

| Non-Octogenarians | Octogenarians | p-Value | |
|---|---|---|---|
| N | 191 (82.7%) | 40 (17.3%) | - |
| Age | 72.1 (5.8) | 83.3 (2.7) | - |
| Aneurysm diameter Missing | 61 (15) | 67 (13) | 0.041 |
| 48 (25.1%) | 14 (35.0%) | ||
| ASA | 0.040 | ||
| 1 | 1 (0.5%) | 0 (0%) | |
| 2 | 47 (24.6%) | 2 (5.0%) | |
| 3 | 132 (69.1%) | 33 (82.5%) | |
| 4 | 7 (3.7%) | 3 (7.5%) | |
| Hypertension | 92.2% | 94.6% | 0.868 |
| Diabetes | 31.2% | 12.9% | 0.065 |
| CHD | 48.9% | 54.5% | 0.792 |
| Time in surgery | 261 (107) | 244 (100) | 0.36 |
| Days in ICU | 2.8 (4.1) | 1.7 (1.1) | 0.004 |
| Days in hospital | 8.8 (4.1) | 7.7 (1.1) | 0.004 |
| Fenestrations | 0.426 | ||
| 1 | 11 (5.8%) | 6 (15.0%) | |
| 2 | 30 (15.7%) | 5 (12.5%) | |
| 3 | 30 (15.7%) | 7 (17.5%) | |
| 4 | 106 (55.5%) | 20 (50.0%) | |
| 5 | 13 (6.8%) | 1 (2.5%) |
| 30 Day Survival | + | − | Total |
|---|---|---|---|
| Non-octogenerians | 180 (94.8%) | 11 (5.2%) | 191 (100%) |
| Octogenerians | 38 (95.0%) | 2 (5.0%) | 40 (100%) |
| Unadjusted odds ratio (95% CI): 0.91 (0.13–3.64) | |||
| Acute Kidney Injury | Non-Octogenarians | Octogenarians |
|---|---|---|
| Yes | 26 (13.6%) | 4 (10.0%) |
| No | 165 (86.4%) | 36 (90.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hofmann, A.G.; Leinweber, M.E.; Assadian, A.; Falkensammer, J.; Taher, F. The Effect of Age on Peri-Operative Outcomes after FEVAR. J. Clin. Med. 2023, 12, 3858. https://doi.org/10.3390/jcm12113858
Hofmann AG, Leinweber ME, Assadian A, Falkensammer J, Taher F. The Effect of Age on Peri-Operative Outcomes after FEVAR. Journal of Clinical Medicine. 2023; 12(11):3858. https://doi.org/10.3390/jcm12113858
Chicago/Turabian StyleHofmann, Amun Georg, Maria Elisabeth Leinweber, Afshin Assadian, Juergen Falkensammer, and Fadi Taher. 2023. "The Effect of Age on Peri-Operative Outcomes after FEVAR" Journal of Clinical Medicine 12, no. 11: 3858. https://doi.org/10.3390/jcm12113858
APA StyleHofmann, A. G., Leinweber, M. E., Assadian, A., Falkensammer, J., & Taher, F. (2023). The Effect of Age on Peri-Operative Outcomes after FEVAR. Journal of Clinical Medicine, 12(11), 3858. https://doi.org/10.3390/jcm12113858








