Potential Hepatic Lipid Markers Associated with Nonalcoholic Steatohepatitis and Fibrosis in Morbid Obesity Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Protocol
2.2. Noninvasive Serum Markers
2.3. Ultrasonographic and Transient Elastography Examination
2.4. Liver Sample Preparation
2.5. Ultrahigh-Performance Liquid Chromatography–Tandem Mass Spectrometer
2.6. Untargeted Lipidomic Analysis
2.7. Statistical Analysis
3. Results
3.1. Characteristics of Patients in NASH with Mild Liver Fibrosis and NASH with Significant Liver Fibrosis Groups
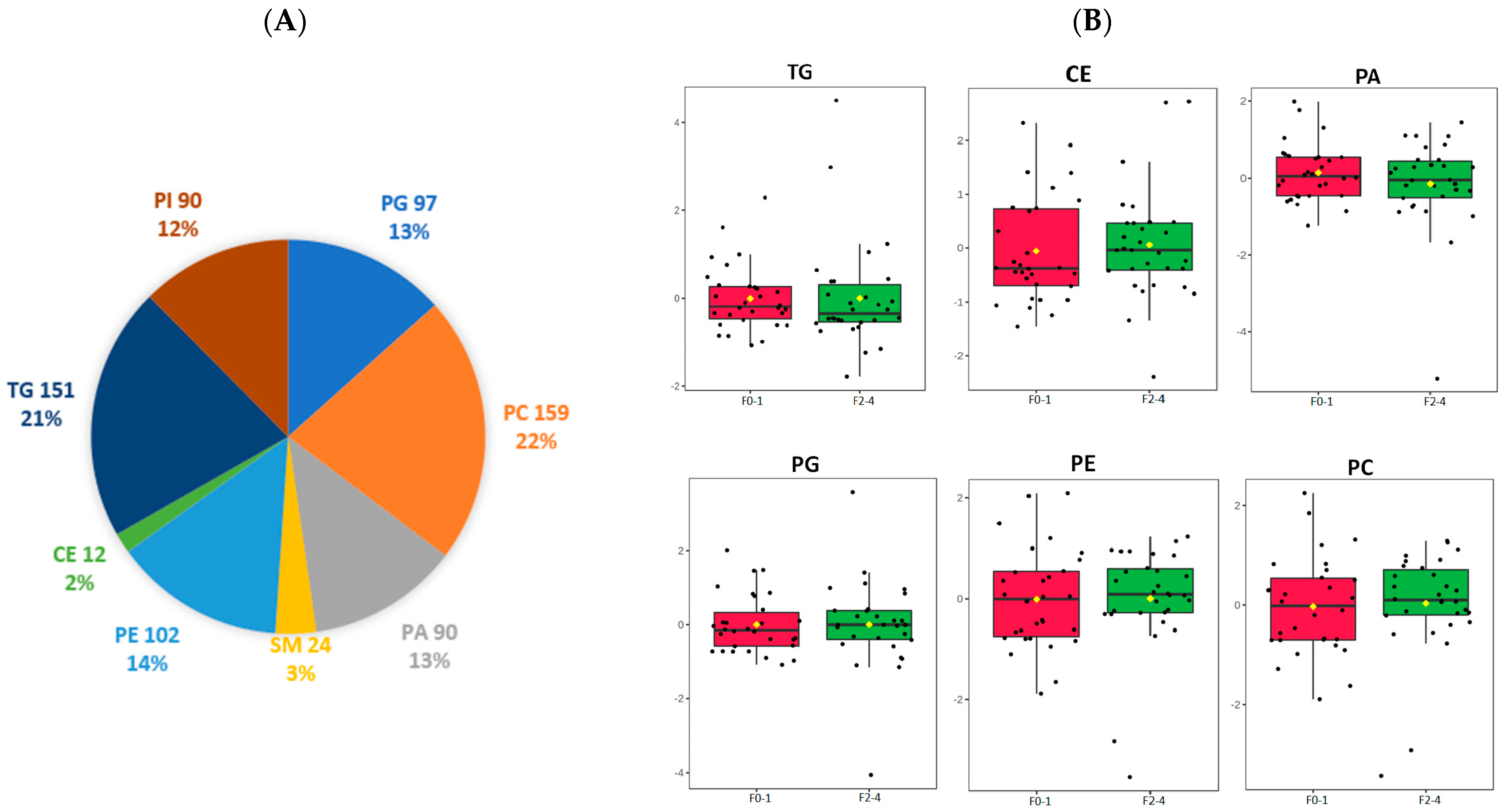
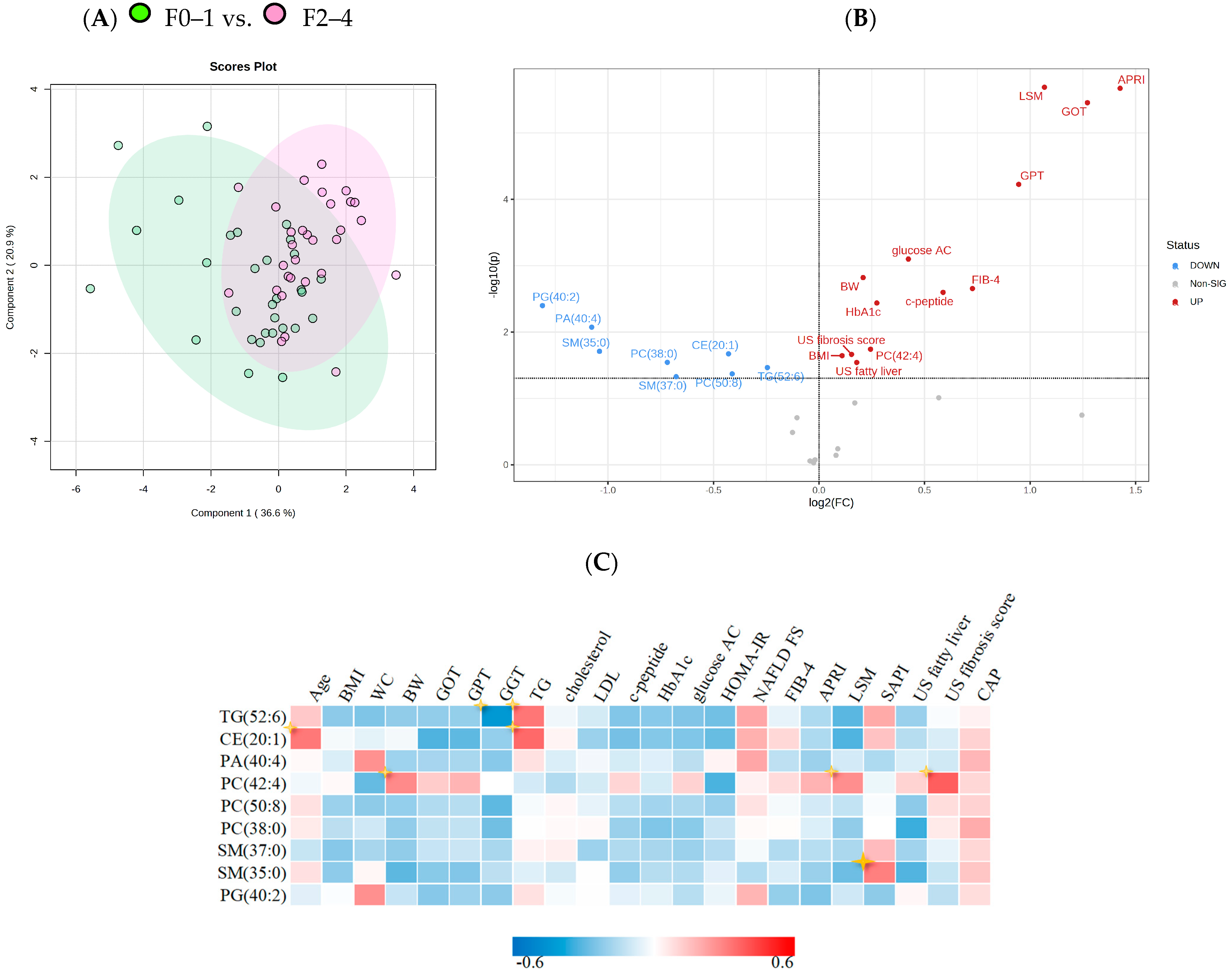
3.2. Lipidomic Profile Differentiation between NASH Stages
3.3. Association of Lipid Metabolites and NAFLD Parameters among Patients with NASH
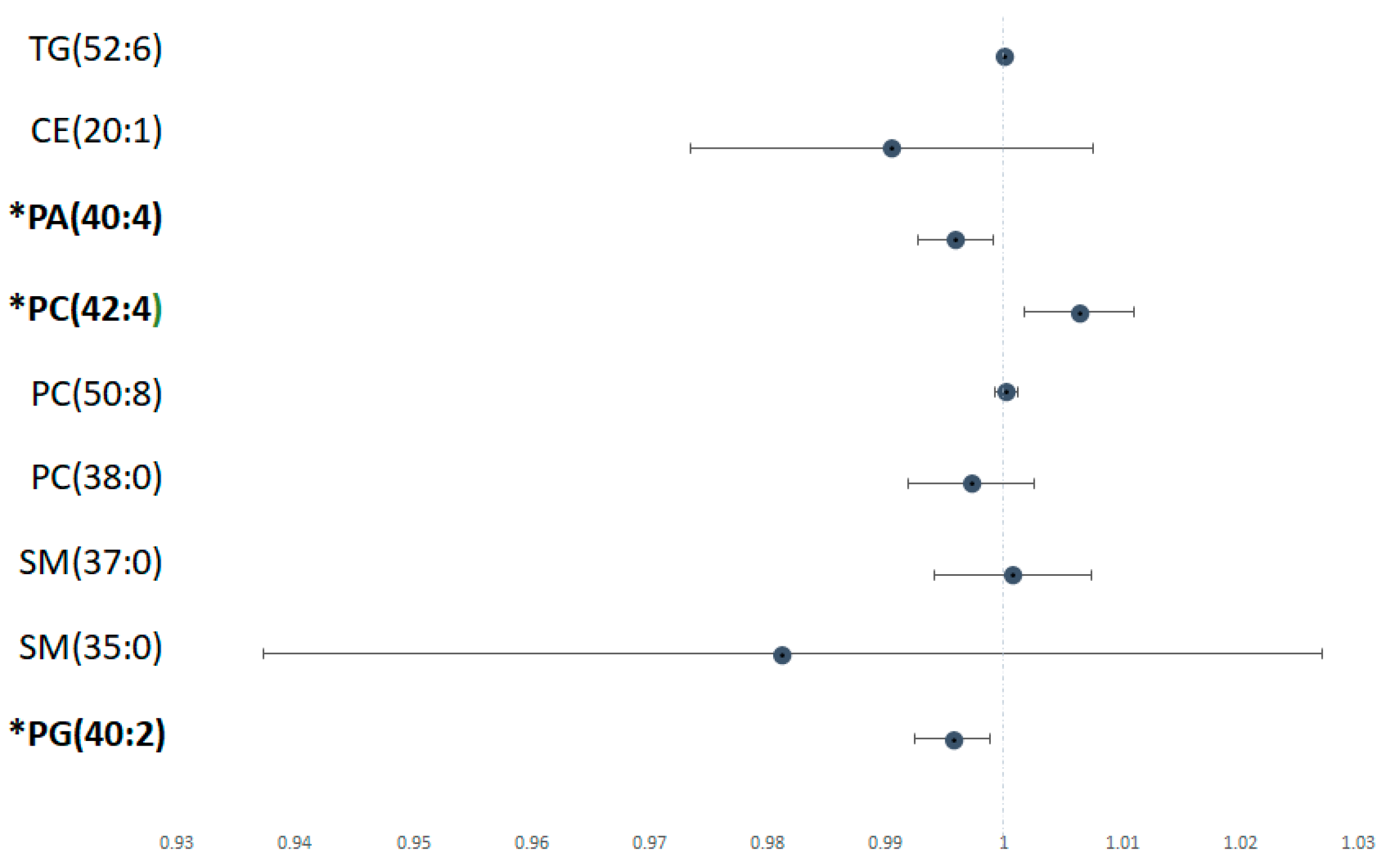
3.4. Predictive Models of NASH Fibrosis in Terms of Levels of Lipid Metabolites
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Association for the Study of the Liver; European Association for the Study of Diabetes; European Association for the Study of Obesity. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.-C.; Wu, C.-Y.; Wang, Y.-J.; Hung, H.-H.; Yang, H.-I.; Kao, W.-Y.; Su, C.-W.; Wu, J.-C.; Chan, W.-L.; Lin, H.-C.; et al. Updated thresholds for serum alanine aminotransferase level in a large-scale population study composed of 34,346 subjects. Aliment. Pharmacol. Ther. 2012, 36, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.-L.; Wang, Y.-J.; Kao, W.-Y.; Chen, P.-H.; Huo, T.-I.; Huang, Y.-H.; Lan, K.-H.; Su, C.-W.; Chan, W.-L.; Lin, H.-C.; et al. Inverse Association between Hepatitis B Virus Infection and Fatty Liver Disease: A Large-Scale Study in Populations Seeking for Check-Up. PLoS ONE 2013, 8, e72049. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.-J.; Yang, Y.-W.; You, S.-L.; Lai, M.-S.; Chen, C.-J. Thirty-Year Outcomes of the National Hepatitis B Immunization Program in Taiwan. JAMA 2013, 310, 974–976. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Recommendations on Treatment of Hepatitis C 2018. J. Hepatol. 2018, 69, 461–511. [Google Scholar] [CrossRef]
- Simon, T.G.; Roelstraete, B.; Khalili, H.; Hagström, H.; Ludvigsson, J.F. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: Results from a nationwide cohort. Gut 2021, 70, 1375–1382. [Google Scholar] [CrossRef]
- Angulo, P.; Kleiner, D.E.; Dam-Larsen, S.; Adams, L.A.; Björnsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Keach, J.C.; Lafferty, H.D.; Stahler, A.; et al. Liver Fibrosis, but No Other Histologic Features, Is Associated with Long-term Outcomes of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology 2015, 149, 389–397.e10. [Google Scholar] [CrossRef]
- Dulai, P.S.; Singh, S.; Patel, J.; Soni, M.; Prokop, L.J.; Younossi, Z.; Sebastiani, G.; Ekstedt, M.; Hagstrom, H.; Nasr, P.; et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology 2017, 65, 1557–1565. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62 (Suppl. S1), S47–S64. [Google Scholar] [CrossRef]
- Gutiérrez-Cuevas, J.; Santos, A.; Armendariz-Borunda, J. Pathophysiological Molecular Mechanisms of Obesity: A Link between MAFLD and NASH with Cardiovascular Diseases. Int. J. Mol. Sci. 2021, 22, 11629. [Google Scholar] [CrossRef]
- Morita, S.; Neto, D.D.S.; Morita, F.H.A.; Morita, N.K.; Lobo, S.M.A. Prevalence of Non-alcoholic Fatty Liver Disease and Steatohepatitis Risk Factors in Patients Undergoing Bariatric Surgery. Obes. Surg. 2015, 25, 2335–2343. [Google Scholar] [CrossRef] [PubMed]
- Seki, Y.; Kakizaki, S.; Horiguchi, N.; Hashizume, H.; Tojima, H.; Yamazaki, Y.; Sato, K.; Kusano, M.; Yamada, M.; Kasama, K. Prevalence of nonalcoholic steatohepatitis in Japanese patients with morbid obesity undergoing bariatric surgery. J. Gastroenterol. 2016, 51, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.-J.; Wang, H.-H.; Lee, W.-J.; Liew, P.-L.; Lin, J.-T.; Wu, M.-S. Diagnostic Value of Ultrasonographic Examination for Nonalcoholic Steatohepatitis in Morbidly Obese Patients Undergoing Laparoscopic Bariatric Surgery. Obes. Surg. 2007, 17, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Tai, C.-M.; Huang, C.-K.; Tu, H.-P.; Hwang, J.-C.; Chang, C.-Y.; Yu, M.-L. PNPLA3 genotype increases susceptibility of nonalcoholic steatohepatitis among obese patients with nonalcoholic fatty liver disease. Surg. Obes. Relat. Dis. 2015, 11, 888–894. [Google Scholar] [CrossRef]
- Tai, C.-M.; Huang, C.-K.; Tu, H.-P.; Hwang, J.-C.; Yeh, M.-L.; Huang, C.-F.; Huang, J.-F.; Dai, C.-Y.; Yu, M.-L. Interactions of a PPARGC1A Variant and a PNPLA3 Variant Affect Nonalcoholic Steatohepatitis in Severely Obese Taiwanese Patients. Medicine 2016, 95, e3120. [Google Scholar] [CrossRef]
- Kao, W.-Y.; Chang, I.-W.; Chen, C.-L.; Su, C.-W.; Fang, S.U.; Tang, J.-H.; Chang, C.-C.; Chang, Y.-J.; Wang, W. Fibroscan-Based Score to Predict Significant Liver Fibrosis in Morbidly Obese Patients with Nonalcoholic Fatty Liver Disease. Obes. Surg. 2020, 30, 1249–1257. [Google Scholar] [CrossRef]
- Musso, G.; Cassader, M.; Paschetta, E.; Gambino, R. Bioactive Lipid Species and Metabolic Pathways in Progression and Resolution of Nonalcoholic Steatohepatitis. Gastroenterology 2018, 155, 282–302.e8. [Google Scholar] [CrossRef]
- Régnier, M.; Polizzi, A.; Guillou, H.; Loiseau, N. Sphingolipid metabolism in non-alcoholic fatty liver diseases. Biochimie 2019, 159, 9–22. [Google Scholar] [CrossRef]
- Caussy, C.; Ajmera, V.H.; Puri, P.; Hsu, C.L.-S.; Bassirian, S.; Mgdsyan, M.; Singh, S.; Faulkner, C.; Valasek, M.A.; Rizo, E.; et al. Serum metabolites detect the presence of advanced fibrosis in derivation and validation cohorts of patients with non-alcoholic fatty liver disease. Gut 2019, 68, 1884–1892. [Google Scholar] [CrossRef]
- Chiappini, F.; Coilly, A.; Kadar, H.; Gual, P.; Tran, A.; Desterke, C.; Samuel, D.; Duclos-Vallée, J.-C.; Touboul, D.; Bertrand-Michel, J.; et al. Metabolism dysregulation induces a specific lipid signature of nonalcoholic steatohepatitis in patients. Sci. Rep. 2017, 7, 46658. [Google Scholar] [CrossRef]
- Wang, Z.-H.; Zheng, K.I.; Wang, X.-D.; Qiao, J.; Li, Y.-Y.; Zhang, L.; Zheng, M.-H.; Wu, J. LC-MS-based lipidomic analysis in distinguishing patients with nonalcoholic steatohepatitis from nonalcoholic fatty liver. Hepatobiliary Pancreat. Dis. Int. 2021, 20, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Ooi, G.J.; Meikle, P.J.; Huynh, K.; Earnest, A.; Roberts, S.K.; Kemp, W.; Parker, B.L.; Brown, W.; Burton, P.; Watt, M.J. Hepatic lipidomic remodeling in severe obesity manifests with steatosis and does not evolve with non-alcoholic steatohepatitis. J. Hepatol. 2021, 75, 524–535. [Google Scholar] [CrossRef]
- Gutiérrez-Cuevas, J.; Lucano-Landeros, S.; López-Cifuentes, D.; Santos, A.; Armendariz-Borunda, J. Epidemiologic, Genetic, Pathogenic, Metabolic, Epigenetic Aspects Involved in NASH-HCC: Current Therapeutic Strategies. Cancers 2022, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Kasama, K.; Mui, W.; Lee, W.J.; Lakdawala, M.; Naitoh, T.; Seki, Y.; Sasaki, A.; Wakabayashi, G.; Sasaki, I.; Kawamura, I.; et al. IFSO-APC Consensus Statements 2011. Obes. Surg. 2012, 22, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Bedossa, P.; Poitou, C.; Veyrie, N.; Bouillot, J.-L.; Basdevant, A.; Paradis, V.; Tordjman, J.; Clement, K. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology 2012, 56, 1751–1759. [Google Scholar] [CrossRef]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef]
- Ahrens, M.; Ammerpohl, O.; von Schönfels, W.; Kolarova, J.; Bens, S.; Itzel, T.; Teufel, A.; Herrmann, A.; Brosch, M.; Hinrichsen, H.; et al. DNA Methylation Analysis in Nonalcoholic Fatty Liver Disease Suggests Distinct Disease-Specific and Remodeling Signatures after Bariatric Surgery. Cell Metab. 2013, 18, 296–302. [Google Scholar] [CrossRef]
- Yang, B.-L.; Wu, W.-C.; Fang, K.-C.; Wang, Y.-C.; Huo, T.-I.; Huang, Y.-H.; Yang, H.-I.; Su, C.-W.; Lin, H.-C.; Lee, F.-Y.; et al. External Validation of Fatty Liver Index for Identifying Ultrasonographic Fatty Liver in a Large-Scale Cross-Sectional Study in Taiwan. PLoS ONE 2015, 10, e0120443. [Google Scholar] [CrossRef]
- Abul-Husn, N.S.; Cheng, X.; Li, A.H.; Xin, Y.; Schurmann, C.; Stevis, P.; Liu, Y.; Kozlitina, J.; Stender, S.; Wood, G.C.; et al. A Protein-Truncating HSD17B13 Variant and Protection from Chronic Liver Disease. N. Engl. J. Med. 2018, 378, 1096–1106. [Google Scholar] [CrossRef]
- Kao, W.Y.; Chiou, Y.Y.; Hung, H.H.; Chou, Y.H.; Su, C.W.; Wu, J.C.; Huo, T.I.; Huang, Y.H.; Lin, H.C.; Lee, S.D. Risk factors for long-term prognosis in hepatocellular carcinoma after radiofrequency ablation therapy: The clinical implication of aspartate aminotransferase-platelet ratio index. Eur. J. Gastroenterol. Hepatol. 2011, 23, 528–536. [Google Scholar] [CrossRef]
- Wong, V.W.-S.; Adams, L.A.; de Lédinghen, V.; Wong, G.L.-H.; Sookoian, S. Noninvasive biomarkers in NAFLD and NASH—Current progress and future promise. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 461–478. [Google Scholar] [CrossRef]
- Wang, C.-C.; Liu, C.-H.; Lin, C.-L.; Wang, P.-C.; Tseng, T.-C.; Lin, H.H.; Kao, J.-H. Fibrosis index based on four factors better predicts advanced fibrosis or cirrhosis than aspartate aminotransferase/platelet ratio index in chronic hepatitis C patients. J. Formos. Med. Assoc. 2015, 114, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Saleh, T.; Ahmed, E.; Yu, L.; Song, S.; Park, K.; Kwak, H.; Woo, H. Conjugating homogenized liver-extracellular matrix into decellularized hepatic scaffold for liver tissue engineering. J. Biomed. Mater. Res. Part A 2020, 108, 1991–2004. [Google Scholar] [CrossRef] [PubMed]
- Folch, J.; Lees, M.; Sloane Stanley, G.H. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar] [CrossRef]
- Mopuri, R.; Kalyesubula, M.; Rosov, A.; Edery, N.; Moallem, U.; Dvir, H. Improved Folch Method for Liver-Fat Quantification. Front. Vet. Sci. 2021, 7, 594853. [Google Scholar] [CrossRef]
- Cai, X.; Liang, N.; Wang, H.; Gao, A.; Xiao, R.; Yu, H. Lipidomic profiles of maternal blood at the earlier stage of gestation and umbilical venous blood in response to supraphysiological hypercholesterolemia versus physiological hypercholesterolemia: An evidence of potential biomarkers and early intervention. Biochim. Biophys. Acta-Mol. Cell Biol. Lipids 2020, 1865, 158587. [Google Scholar] [CrossRef] [PubMed]
- Puri, P.; Baillie, R.A.; Wiest, M.M.; Mirshahi, F.; Choudhury, J.; Cheung, O.; Sargeant, C.; Contos, M.J.; Sanyal, A.J. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology 2007, 46, 1081–1090. [Google Scholar] [CrossRef]
- McGlinchey, A.J.; Govaere, O.; Geng, D.; Ratziu, V.; Allison, M.; Bousier, J.; Petta, S.; de Oliviera, C.; Bugianesi, E.; Schattenberg, J.M.; et al. Metabolic signatures across the full spectrum of non-alcoholic fatty liver disease. JHEP Rep. 2022, 4, 100477. [Google Scholar] [CrossRef]
- Gorden, D.; Myers, D.S.; Ivanova, P.T.; Fahy, E.; Maurya, M.R.; Gupta, S.; Min, J.; Spann, N.J.; McDonald, J.G.; Kelly, S.L.; et al. Biomarkers of NAFLD progression: A lipidomics approach to an epidemic. J. Lipid Res. 2015, 56, 722–736. [Google Scholar] [CrossRef]
- Alamri, H.; Patterson, N.H.; Yang, E.; Zoroquiain, P.; Lazaris, A.; Chaurand, P.; Metrakos, P. Mapping the triglyceride distribution in NAFLD human liver by MALDI imaging mass spectrometry reveals molecular differences in micro and macro steatosis. Anal. Bioanal. Chem. 2019, 411, 885–894. [Google Scholar] [CrossRef]
- Wouters, K.; van Bilsen, M.; van Gorp, P.J.; Bieghs, V.; Lütjohann, D.; Kerksiek, A.; Staels, B.; Hofker, M.H.; Shiri-Sverdlov, R. Intrahepatic cholesterol influences progression, inhibition and reversal of non-alcoholic steatohepatitis in hyperlipidemic mice. FEBS Lett. 2010, 584, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Quehenberger, O.; Armando, A.; Dennis, E.A. Polyunsaturated fatty acid metabolites as novel lipidomic biomarkers for noninvasive diagnosis of nonalcoholic steatohepatitis. J. Lipid Res. 2015, 56, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Yang, L.; McCall, S.; Huang, J.; Yu, X.X.; Pandey, S.K.; Bhanot, S.; Monia, B.P.; Li, Y.-X.; Diehl, A.M. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology 2007, 45, 1366–1374. [Google Scholar] [CrossRef] [PubMed]
- Morgan, A.E.; Mc Auley, M.T. Cholesterol Homeostasis: An In Silico Investigation into How Aging Disrupts Its Key Hepatic Regulatory Mechanisms. Biology 2020, 9, 314. [Google Scholar] [CrossRef]
- Ishay, Y.; Nachman, D.; Khoury, T.; Ilan, Y. The role of the sphingolipid pathway in liver fibrosis: An emerging new potential target for novel therapies. Am. J. Physiol. Physiol. 2020, 318, C1055–C1064. [Google Scholar] [CrossRef] [PubMed]
- Montefusco, D.J.; Allegood, J.C.; Spiegel, S.; Cowart, L.A. Non-alcoholic fatty liver disease: Insights from sphingolipidomics. Biochem. Biophys. Res. Commun. 2018, 504, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Molina, B.; Castellano-Castillo, D.; Pastor, O.; Ocaña-Wilhelmi, L.; Fernández-García, D.; Romero-Gómez, M.; Cardona, F.; Tinahones, F.J. A Pilot Study of Serum Sphingomyelin Dynamics in Subjects with Severe Obesity and Non-alcoholic Steatohepatitis after Sleeve Gastrectomy. Obes. Surg. 2019, 29, 983–989. [Google Scholar] [CrossRef]
- Xuan, Q.; Hu, C.; Zhang, Y.; Wang, Q.; Zhao, X.; Liu, X.; Wang, C.; Jia, W.; Xu, G. Serum lipidomics profiles reveal potential lipid markers for prediabetes and type 2 diabetes in patients from multiple communities. Front. Endocrinol. 2022, 13, 966823. [Google Scholar] [CrossRef]
- Vvedenskaya, O.; Rose, T.D.; Knittelfelder, O.; Palladini, A.; Wodke, J.A.H.; Schuhmann, K.; Ackerman, J.M.; Wang, Y.; Has, C.; Brosch, M.; et al. Nonalcoholic fatty liver disease stratification by liver lipidomics. J. Lipid Res. 2021, 62, 100104. [Google Scholar] [CrossRef]
- van der Veen, J.N.; Kennelly, J.P.; Wan, S.; Vance, J.E.; Vance, D.E.; Jacobs, R.L. The critical role of phosphatidylcholine and phosphatidylethanolamine metabolism in health and disease. Biochim. Biophys. Acta (BBA)-Biomembr. 2017, 1859 Pt B, 1558–1572. [Google Scholar] [CrossRef]
- Payne, F.; Lim, K.; Girousse, A.; Brown, R.J.; Kory, N.; Robbins, A.; Xue, Y.; Sleigh, A.; Cochran, E.; Adams, C.; et al. Mutations disrupting the Kennedy phosphatidylcholine pathway in humans with congenital lipodystrophy and fatty liver disease. Proc. Natl. Acad. Sci. USA 2014, 111, 8901–8906. [Google Scholar] [CrossRef]
- Enomoto, H. Liver fibrosis markers of nonalcoholic steatohepatitis. World J. Gastroenterol. 2015, 21, 7427–7435. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Hui, J.M.; Marchesini, G.; Bugianesi, E.; George, J.; Farrell, G.C.; Enders, F.; Saksena, S.; Burt, A.D.; Bida, J.P.; et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007, 45, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Yip, T.C.-F.; Lee, H.W.; Chan, W.K.; Wong, G.L.-H.; Wong, V.W.-S. Asian perspective on NAFLD-associated HCC. J. Hepatol. 2021, 76, 726–734. [Google Scholar] [CrossRef] [PubMed]


| All (n = 60) | NASH with F0–F1 (n = 30) | NASH with F2–F4 (n = 30) | p Value | |
|---|---|---|---|---|
| Age, years * | 35.9 ± 7.7 | 37.2 ± 8.5 | 34.6 ± 6.8 | 0.168 |
| Sex (M/F) (%) | 26/34 (43.3/56.7) | 8/22 (26.7/73.3) | 18/12 (60.0/40.0) | 0.009 |
| Smoking (yes/no) (%) | 9/51 (15.0/85.0) | 7/23 (23.3/76.7) | 2/28 (6.7/93.3) | 0.590 |
| BMI, kg/m2 * | 40.8 ± 5.3 | 39.2 ± 4.7 | 42.3 ± 5.5 | 0.011 |
| WC, cm * | 120.9 ± 11.8 | 118.7 ± 11.4 | 123.5 ± 11.8 | 0.166 |
| HTN (yes/no) (%) | 19/41 (31.7/68.3) | 8/22 (26.7/73.3) | 11/19 (36.7/63.3) | 0.405 |
| HTN under medication (yes/no) | 10/9 (52.6/47.4) | 5/3 (62.5/37.5) | 4/7 (57.1/42.9) | - |
| DM (yes/no) (%) | 14/46 (23.3/76.7) | 2/28 (6.7/93.3) | 12/18 (40.0/60.0) | 0.002 |
| DM under medication (yes/no) | 7/7 (50/50) | 1/1 (50/50) | 6/6 (50/50) | - |
| Biochemical data | ||||
| Fasting glucose, mg/Dl * | 118.7 ± 38.7 | 102.9 ± 18.5 | 134.0 ± 46.7 | 0.009 |
| HOMA-IR * | 6.1 ± 11.4 | 3.2 ± 3.3 | 9.99 ± 16.4 | 0.046 |
| C-peptide, ng/mL | 4.6 ± 2.1 | 3.8 ± 1.2 | 5.3 ± 2.4 | 0.025 |
| Cholesterol, mg/dL * | 195.6 ± 41.7 | 200.3 ± 49.4 | 191.1 ± 32.8 | 0.097 |
| LDL, mg/dL * | 134.3 ± 34.0 | 135.0 ± 41.1 | 133.6 ± 26.5 | 0.729 |
| TG, mg/dL * | 187.4 ± 152.2 | 192.1 ± 110.3 | 182.8 ± 185.9 | 0.255 |
| Total bilirubin, mg/dL * | 0.7 ± 0.3 | 0.6 ± 0.2 | 0.8 ± 0.8 | 0.101 |
| AST, U/L * | 44.2 ± 33.0 | 25.9 ± 9.7 | 62.5 ± 37.9 | <0.001 |
| ALT, U/L * | 66.1 ± 42.7 | 45.1 ± 21.4 | 90.0 ± 48.4 | <0.001 |
| GGT, U/L * | 50.6 ± 23.1 | 41.4 ± 22.3 | 59.3 ± 2075 | 0.008 |
| Creatinine, mg/dL * | 0.7 ± 0.2 | 0.7 ± 0.1 | 0.7 ± 0.2 | 0.273 |
| Albumin, g/dL * | 4.5 ± 0.3 | 4.5 ± 0.3 | 4.4 ± 0.3 | 0.351 |
| Platelet, 1000/mm3 * | 279.8 ± 64.0 | 297.0 ± 59.5 | 262.6 ± 64.8 | 0.054 |
| Non-invasive serum markers | ||||
| APRI * | 0.42 ± 0.34 | 0.23 ± 0.11 | 0.62 ± 0.39 | <0.001 |
| NAFLD-FS * | 2.44 ± 1.31 | 2.25 ± 1.37 | 2.64 ± 1.23 | 0.190 |
| FIB-4 score * | 0.72 ± 0.43 | 0.52 ± 0.22 | 0.95 ± 0.49 | <0.001 |
| FLI * | 84.13 ± 31.38 | 89.96 ± 10.36 | 78.3 ± 38.6 | 0.242 |
| Imaging techniques | ||||
| LSM (E score) *, kPa | 9.7 ± 6.4 | 6.9 ± 3.3 | 12.5 ± 7.5 | <0.001 |
| CAP, dB/m | 323.2 ± 66.6 | 320.2 ± 36.2 | 326.4 ± 89.0 | 0.111 |
| US fatty score * | 7.3 ± 1.6 | 6.8 ± 1.7 | 7.7 ± 1.4 | 0.046 |
| US fibrosis score * | 5.0 ± 0.7 | 5.0 ± 0.7 | 5.6 ± 1.1 | 0.035 |
| SAPI | 0.80 ± 0.24 | 0.80 ± 0.22 | 0.90 ± 0.26 | 0.082 |
| Lipid Class | Lipid Species | p Value | Fold Change |
|---|---|---|---|
| Triglyceride (TG) | TG (52:6) | 0.034281 | 1.185 |
| Cholesterol ester (CE) | CE (20:1) | 0.021292 | 1.3462 |
| Phospholipid (PL) | PA (40:4) | 0.00844 | 2.1097 |
| PC (38:0) | 0.028609 | 1.6457 | |
| PC (42:4) | 0.018124 | 0.8443 | |
| PC (50:8) | 0.043317 | 1.3303 | |
| PG (40:2) | 0.003993 | 2.4802 | |
| Sphingolipid (SP) | SM (35:0) | 0.019529 | 2.0565 |
| SM (37:0) | 0.047131 | 1.5988 |
| Model | C Statistic 95%CI | p Value |
|---|---|---|
| APRI + LSM + US fibrosis score | 0.914 (0.846–0.982) | <0.0001 |
| APRI + LSM + US fibrosis score + PC (42:4) | 0.925 (0.856–0.995) | <0.0001 |
| APRI + LSM + US fibrosis score + PG (40:2) | 0.930 (0.869–0.991) | <0.0001 |
| APRI + LSM + US fibrosis score + PC (42:4) + PG (40:2) | 0.941 (0.88–1.003) | <0.0001 |
| Model | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| APRI + LSM + US fibrosis score | 93.1 | 76.7 | 79.3 | 76.7 |
| APRI + LSM + US fibrosis score + PC (42:4) | 79.3 | 93.3 | 86.2 | 80 |
| APRI + LSM + US fibrosis score + PG (40:2) | 86.2 | 87.7 | 89.7 | 80 |
| APRI + LSM + US fibrosis score + PC (42:4) + PG (40:2) | 79.3 | 100 | 82.8 | 83.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, H.-C.; Hsieh, Y.-R.; Wang, W.; Chang, C.-W.; Chang, I.-W.; Chen, C.-L.; Chang, C.-C.; Chang, C.-H.; Kao, W.-Y.; Huang, S.-Y. Potential Hepatic Lipid Markers Associated with Nonalcoholic Steatohepatitis and Fibrosis in Morbid Obesity Patients. J. Clin. Med. 2023, 12, 3730. https://doi.org/10.3390/jcm12113730
Wu H-C, Hsieh Y-R, Wang W, Chang C-W, Chang I-W, Chen C-L, Chang C-C, Chang C-H, Kao W-Y, Huang S-Y. Potential Hepatic Lipid Markers Associated with Nonalcoholic Steatohepatitis and Fibrosis in Morbid Obesity Patients. Journal of Clinical Medicine. 2023; 12(11):3730. https://doi.org/10.3390/jcm12113730
Chicago/Turabian StyleWu, Hua-Chien, Yin-Ru Hsieh, Weu Wang, Ching-Wen Chang, I-Wei Chang, Chi-Long Chen, Chun-Chao Chang, Chia-Hsuan Chang, Wei-Yu Kao, and Shih-Yi Huang. 2023. "Potential Hepatic Lipid Markers Associated with Nonalcoholic Steatohepatitis and Fibrosis in Morbid Obesity Patients" Journal of Clinical Medicine 12, no. 11: 3730. https://doi.org/10.3390/jcm12113730
APA StyleWu, H.-C., Hsieh, Y.-R., Wang, W., Chang, C.-W., Chang, I.-W., Chen, C.-L., Chang, C.-C., Chang, C.-H., Kao, W.-Y., & Huang, S.-Y. (2023). Potential Hepatic Lipid Markers Associated with Nonalcoholic Steatohepatitis and Fibrosis in Morbid Obesity Patients. Journal of Clinical Medicine, 12(11), 3730. https://doi.org/10.3390/jcm12113730