Biomarkers of Hypercoagulability in COVID-19
Conclusions
Conflicts of Interest
References
- Bagautdinova, D.; Bacharz, K.C.; Bylund, C.L.; Sae-Hau, M.; Weiss, E.S.; Rajotte, M.; Lincoln, G.; Vasquez, T.S.; Parker, N.D.; Wright, K.B.; et al. Understanding the Impact of COVID-19 on Chronic Lymphocytic Leukemia (CLL) Caregiving and Related Resource Needs. J. Clin. Med. 2023, 12, 1648. [Google Scholar] [CrossRef] [PubMed]
- Citu, C.; Burlea, B.; Gorun, F.; Motoc, A.; Gorun, O.M.; Malita, D.; Ratiu, A.; Margan, R.; Grigoras, M.L.; Bratosin, F.; et al. Predictive Value of Blood Coagulation Parameters in Poor Outcomes in COVID-19 Patients: A Retrospective Observational Study in Romania. J. Clin. Med. 2022, 11, 2831. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Mora, S.; Corona, M.; Torres, M.; Casado-Fernández, G.; García-Pérez, J.; Ramos-Martín, F.; Vigón, L.; Manzanares, M.; Mateos, E.; Martín-Moro, F.; et al. Early Cellular and Humoral Responses Developed in Oncohematological Patients after Vaccination with One Dose against COVID-19. J. Clin. Med. 2022, 11, 2803. [Google Scholar] [CrossRef] [PubMed]
- Mackiewicz-Milewska, M.; Sakwińska, K.; Cisowska-Adamiak, M.; Szymkuć-Bukowska, I.; Ratuszek-Sadowska, D.; Mackiewicz-Nartowicz, H. Bleeding into the Abdominal and Ilio-Lumbar Muscles—A Rare Complication in the Course of COVID-19: Analysis of Four Cases and a Literature Review. J. Clin. Med. 2022, 11, 4712. [Google Scholar] [CrossRef] [PubMed]
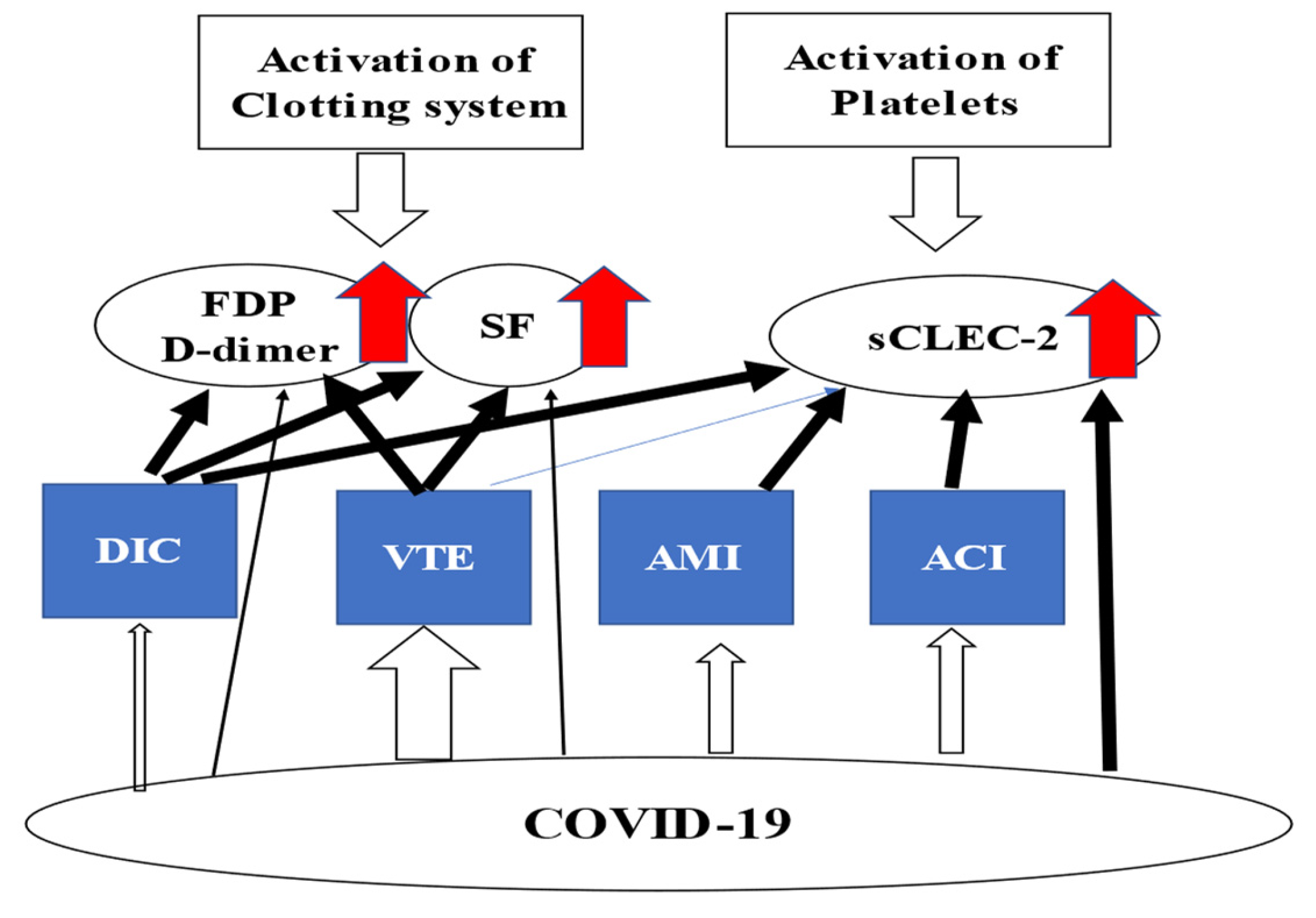
- Yamamoto, A.; Wada, H.; Ichikawa, Y.; Mizuno, H.; Tomida, M.; Masuda, J.; Makino, K.; Kodama, S.; Yoshida, M.; Fukui, S.; et al. Evaluation of Biomarkers of Severity in Patients with COVID-19 Infection. J. Clin. Med. 2021, 10, 3775. [Google Scholar] [CrossRef] [PubMed]
- Wada, H.; Ichikawa, Y.; Ezaki, M.; Yamamoto, A.; Tomida, M.; Yoshida, M.; Fukui, S.; Moritani, I.; Shiraki, K.; Shimaoka, M.; et al. Elevated Plasma Soluble C-Type Lectin-like Receptor 2 Is Associated with the Worsening of Coronavirus Disease 2019. J. Clin. Med. 2022, 11, 985. [Google Scholar] [CrossRef] [PubMed]
- Ezaki, M.; Wada, H.; Ichikawa, Y.; Ikeda, N.; Shiraki, K.; Yamamoto, A.; Moritani, I.; Shimaoka, M.; Shimpo, H. Plasma Soluble Fibrin Is Useful for the Diagnosis of Thrombotic Diseases. J. Clin. Med. 2023, 12, 2597. [Google Scholar] [CrossRef] [PubMed]
- Wada, H.; Yamamoto, A.; Tomida, M.; Ichikawa, Y.; Ezaki, M.; Masuda, J.; Yoshida, M.; Fukui, S.; Moritani, I.; Inoue, H.; et al. Proposal of Quick Diagnostic Criteria for Disseminated Intravascular Coagulation. J. Clin. Med. 2022, 11, 1028. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, A.; Wada, H.; Ichkawa, Y.; Tanaka, M.; Tashiro, H.; Shiraki, K.; Shimpo, H.; Yamashita, Y.; Mastumoto, T.; Shimaoka, M.; et al. Soluble C-Type Lectin-Like Receptor 2 Is a Biomarker for Disseminated Intravascular Coagulation. J. Clin. Med. 2021, 10, 2860. [Google Scholar] [CrossRef] [PubMed]
- Nishigaki, A.; Ichikawa, Y.; Ezaki, E.; Yamamoto, A.; Suzuki, K.; Tachibana, K.; Kamon, T.; Horie, S.; Masuda, J.; Makino, K.; et al. Soluble C-type lectin-like receptor 2 elevation in patients with acute cerebral infarction. J. Clin. Med. 2021, 10, 3408. [Google Scholar] [CrossRef] [PubMed]
- Suzuki-Inoue, K.; Fuller, G.L.; Garcia, A.; Eble, J.A.; Pohlmann, S.; Inoue, O.; Gartner, T.K.; Hughan, S.C.; Pearce, A.C.; Laing, G.D.; et al. A novel Syk-dependent mechanism of platelet activation by the C-type lectin receptor sCLEC-2. Blood 2006, 107, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Wada, H.; Shiraki, K.; Shimpo, H.; Shimaoka, M.; Iba, T.; Suzuki-Inoue, K. Thrombotic Mechanism Involving Platelet Activation, Hypercoagulability and Hypofibrinolysis in Coronavirus Disease 2019. Int. J. Mol. Sci. 2023, 24, 7975. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wada, H. Biomarkers of Hypercoagulability in COVID-19. J. Clin. Med. 2023, 12, 3525. https://doi.org/10.3390/jcm12103525
Wada H. Biomarkers of Hypercoagulability in COVID-19. Journal of Clinical Medicine. 2023; 12(10):3525. https://doi.org/10.3390/jcm12103525
Chicago/Turabian StyleWada, Hideo. 2023. "Biomarkers of Hypercoagulability in COVID-19" Journal of Clinical Medicine 12, no. 10: 3525. https://doi.org/10.3390/jcm12103525
APA StyleWada, H. (2023). Biomarkers of Hypercoagulability in COVID-19. Journal of Clinical Medicine, 12(10), 3525. https://doi.org/10.3390/jcm12103525




