Fear-Avoidance Beliefs Are Associated with Pain Intensity and Shoulder Disability in Adults with Chronic Shoulder Pain: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Aspects
2.2. Participants and Setting
2.3. Outcome Measures
2.3.1. Fear-Avoidance Beliefs
2.3.2. Shoulder Pain Intensity and Disability
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Relation between Age, Fear-Avoidance Beliefs, and Shoulder Pain Intensity and Disability
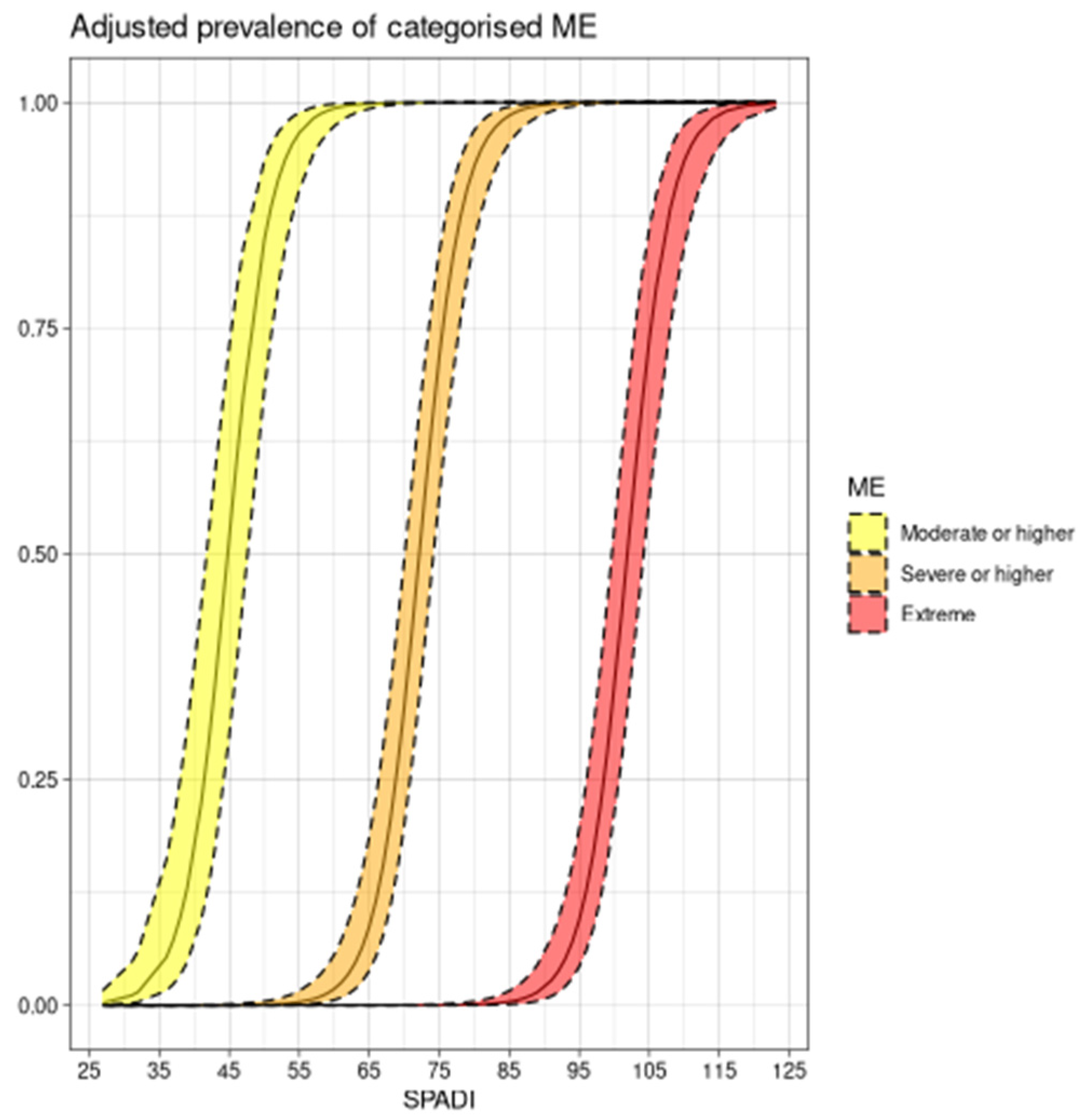
3.3. The Association between Fear-Avoidance Beliefs and Shoulder Pain Intensity and Disability
4. Discussion
4.1. Clinical Implications
4.2. Methodological Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Groenewald, C.B.; Essner, B.S.; Wright, D.; Fesinmeyer, M.D.; Palermo, T.M. The Economic Costs of Chronic Pain among a Cohort of Treatment-Seeking Adolescents in the United States. J. Pain 2014, 15, 925–933. [Google Scholar] [CrossRef]
- Dansie, E.J.; Turk, D.C.; Martin, K.R.; Van Domelen, D.R.; Patel, K.V. Association of Chronic Widespread Pain with Objectively Measured Physical Activity in Adults: Findings from the National Health and Nutrition Examination Survey. J. Pain 2014, 15, 507–515. [Google Scholar] [CrossRef]
- Jordan, K.P.; Kadam, U.T.; Hayward, R.; Porcheret, M.; Young, C.; Croft, P. Annual Consultation Prevalence of Regional Musculoskeletal Problems in Primary Care: An Observational Study. BMC Musculoskelet. Disord. 2010, 11, 144. [Google Scholar] [CrossRef]
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.M.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A.N. Prevalence and Incidence of Shoulder Pain in the General Population; a Systematic Review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef]
- Pribicevic, M. The Epidemiology of Shoulder Pain: A Narrative Review of the Literature; IntechOpen: London, UK, 2012. [Google Scholar] [CrossRef]
- Ackerman, I.N.; Fotis, K.; Pearson, L.; Schoch, P.; Broughton, N.; Brennan-Olsen, S.L.; Bucknill, A.; Cross, E.; Bunting-Frame, N.; Page, R.S. Impaired Health-Related Quality of Life, Psychological Distress, and Productivity Loss in Younger People with Persistent Shoulder Pain: A Cross-Sectional Analysis. Disabil. Rehabil. 2022, 44, 3785–3794. [Google Scholar] [CrossRef]
- Clausen, M.B.; Nielsen, M.F.; Merrild, M.B.; Hölmich, P.; Thorborg, K. High Incidence of Lost Workdays in Patients with Subacromial Impingement Syndrome. Dan. Med. J. 2021, 68, A07200496. [Google Scholar]
- Imagama, S.; Ando, K.; Kobayashi, K.; Seki, T.; Hamada, T.; Machino, M.; Ota, K.; Tanaka, S.; Morozumi, M.; Kanbara, S.; et al. Shoulder Pain Has Most Impact on Poor Quality of Life among Various Types of Musculoskeletal Pain in Middle-Aged and Elderly People: Yakumo Study. Mod. Rheumatol. 2020, 30, 568–572. [Google Scholar] [CrossRef]
- Kuijpers, T.; van der Windt, D.A.W.M.; van der Heijden, G.J.M.G.; Bouter, L.M. Systematic Review of Prognostic Cohort Studies on Shoulder Disorders. Pain 2004, 109, 420–431. [Google Scholar] [CrossRef]
- Lewis, J. Rotator Cuff Related Shoulder Pain: Assessment, Management and Uncertainties. Man. Ther. 2016, 23, 57–68. [Google Scholar] [CrossRef]
- Dunn, W.R.; Kuhn, J.E.; Sanders, R.; An, Q.; Baumgarten, K.M.; Bishop, J.Y.; Brophy, R.H.; Carey, J.L.; Holloway, G.B.; Jones, G.L.; et al. Symptoms of Pain Do Not Correlate with Rotator Cuff Tear Severity: A Cross-Sectional Study of 393 Patients with a Symptomatic Atraumatic Full-Thickness Rotator Cuff Tear. J. Bone Joint Surg. Am. 2014, 96, 793–800. [Google Scholar] [CrossRef]
- Navarro-Ledesma, S.; Struyf, F.; Labajos-Manzanares, M.T.; Fernandez-Sanchez, M.; Morales-Asencio, J.M.; Luque-Suarez, A. Does the Acromiohumeral Distance Matter in Chronic Rotator Cuff Related Shoulder Pain? Musculoskelet. Sci. Pract. 2017, 29, 38–42. [Google Scholar] [CrossRef]
- Ratcliffe, E.; Pickering, S.; McLean, S.; Lewis, J. Is There a Relationship between Subacromial Impingement Syndrome and Scapular Orientation? A Systematic Review. Br. J. Sports Med. 2014, 48, 1251–1256. [Google Scholar] [CrossRef]
- MOON Shoulder Group. The Duration of Symptoms Does Not Correlate with Rotator Cuff Tear Severity or Other Patient-Related Features: A Cross-Sectional Study of Patients with Atraumatic, Full-Thickness Rotator Cuff Tears. J. Shoulder Elbow Surg. 2014, 23, 1052–1058. [Google Scholar] [CrossRef]
- Thorpe, A.M.; O’Sullivan, P.B.; Mitchell, T.; Hurworth, M.; Spencer, J.; Booth, G.; Goebel, S.; Khoo, P.; Tay, A.; Smith, A. Are Psychologic Factors Associated with Shoulder Scores After Rotator Cuff Surgery? Clin. Orthop. 2018, 476, 2062–2073. [Google Scholar] [CrossRef]
- Sheikhzadeh, A.; Wertli, M.M.; Weiner, S.S.; Rasmussen-Barr, E.; Weiser, S. Do Psychological Factors Affect Outcomes in Musculoskeletal Shoulder Disorders? A Systematic Review. BMC Musculoskelet. Disord. 2021, 22, 560. [Google Scholar] [CrossRef]
- Adams, R. The Biology of Fear. Curr. Biol. 2013, 23, R79–R93. [Google Scholar] [CrossRef]
- Davidson, P.; Carlsson, I.; Jönsson, P.; Johansson, M. Sleep and the Generalization of Fear Learning. J. Sleep Res. 2016, 25, 88–95. [Google Scholar] [CrossRef]
- Meulders, A.; Vlaeyen, J.W.S. The Acquisition and Generalization of Cued and Contextual Pain-Related Fear: An Experimental Study Using a Voluntary Movement Paradigm. Pain 2013, 154, 272–282. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S. Learning to Predict and Control Harmful Events: Chronic Pain and Conditioning. Pain 2015, 156, S86–S93. [Google Scholar] [CrossRef]
- Meulders, A. From Fear of Movement-Related Pain and Avoidance to Chronic Pain Disability: A State-of-the-Art Review. Curr. Opin. Behav. Sci. 2019, 26, 130–136. [Google Scholar] [CrossRef]
- Meulders, A.; Vlaeyen, J.W.S. Mere Intention to Perform Painful Movements Elicits Fear of Movement-Related Pain: An Experimental Study on Fear Acquisition beyond Actual Movements. J. Pain 2013, 14, 412–423. [Google Scholar] [CrossRef]
- Meulders, A.; Harvie, D.S.; Lorimer Moseley, G.; Vlaeyen, J.W.S. Generalization of Pain-Related Fear Using a Left-Right Hand Judgment Conditioning Task. Behav. Ther. 2015, 46, 699–716. [Google Scholar] [CrossRef]
- Jepma, M.; Wager, T.D. Conceptual Conditioning: Mechanisms Mediating Conditioning Effects on Pain. Psychol. Sci. 2015, 26, 1728–1739. [Google Scholar] [CrossRef]
- Koban, L.; Jepma, M.; Geuter, S.; Wager, T.D. What’s in a Word? How Instructions, Suggestions, and Social Information Change Pain and Emotion. Neurosci. Biobehav. Rev. 2017, 81, 29–42. [Google Scholar] [CrossRef]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.S.; Karoly, P. Fear-Avoidance Model of Chronic Pain: The next Generation. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef]
- Leeuw, M.; Goossens, M.E.J.B.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W.S. The Fear-Avoidance Model of Musculoskeletal Pain: Current State of Scientific Evidence. J. Behav. Med. 2007, 30, 77–94. [Google Scholar] [CrossRef]
- Steimer, T. The Biology of Fear- and Anxiety-Related Behaviors. Dialogues Clin. Neurosci. 2002, 4, 231–249. [Google Scholar] [CrossRef]
- Turk, D.C.; Wilson, H.D. Fear of Pain as a Prognostic Factor in Chronic Pain: Conceptual Models, Assessment, and Treatment Implications. Curr. Pain Headache Rep. 2010, 14, 88–95. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-Avoidance Model of Chronic Musculoskeletal Pain: 12 Years On. Pain 2012, 153, 1144–1147. [Google Scholar] [CrossRef]
- Sieben, J.M.; Vlaeyen, J.W.S.; Portegijs, P.J.M.; Verbunt, J.A.; van Riet-Rutgers, S.; Kester, A.D.M.; Von Korff, M.; Arntz, A.; Knottnerus, J.A. A Longitudinal Study on the Predictive Validity of the Fear-Avoidance Model in Low Back Pain. Pain 2005, 117, 162–170. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Struyf, F.; Meeus, M.; Luque-Suarez, A. The Association between Pain Beliefs and Pain Intensity and/or Disability in People with Shoulder Pain: A Systematic Review. Musculoskelet. Sci. Pract. 2018, 37, 29–57. [Google Scholar] [CrossRef]
- De Baets, L.; Matheve, T.; Meeus, M.; Struyf, F.; Timmermans, A. The Influence of Cognitions, Emotions and Behavioral Factors on Treatment Outcomes in Musculoskeletal Shoulder Pain: A Systematic Review. Clin. Rehabil. 2019, 33, 980–991. [Google Scholar] [CrossRef]
- Struyf, F.; Geraets, J.; Noten, S.; Meeus, M.; Nijs, J. A Multivariable Prediction Model for the Chronification of Non-Traumatic Shoulder Pain: A Systematic Review. Pain Physician 2016, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; Walsworth, M.K.; Doukas, W.C.; Murphy, K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Arch. Phys. Med. Rehabil. 2009, 90, 1898–1903. [Google Scholar] [CrossRef] [PubMed]
- Calis, M.; Demir, H.; Ulker, S.; Kirnap, M.; Duygulu, F.; Calis, H.T. Is Intraarticular Sodium Hyaluronate Injection an Alternative Treatment in Patients with Adhesive Capsulitis? Rheumatol. Int. 2006, 26, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; Neblett, R.; Gatchel, R.J.; Roldán-Jiménez, C. Cross-Cultural Adaptation and Validity of the Spanish Fear-Avoidance Components Scale and Clinical Implications in Primary Care. BMC Fam. Pract. 2020, 21, 44. [Google Scholar] [CrossRef]
- Kamonseki, D.H.; Haik, M.N.; Ribeiro, L.P.; de Almeida, R.F.; de Almeida, L.A.; Fonseca, C.L.; Camargo, P.R. Measurement Properties of the Brazilian Versions of Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in Individuals with Shoulder Pain. PloS ONE 2021, 16, e0260452. [Google Scholar] [CrossRef]
- Torres-Lacomba, M.; Sánchez-Sánchez, B.; Prieto-Gómez, V.; Pacheco-da-Costa, S.; Yuste-Sánchez, M.J.; Navarro-Brazález, B.; Gutiérrez-Ortega, C. Spanish Cultural Adaptation and Validation of the Shoulder Pain and Disability Index, and the Oxford Shoulder Score after Breast Cancer Surgery. Health Qual. Life Outcomes 2015, 13, 63. [Google Scholar] [CrossRef]
- Baliki, M.N.; Mansour, A.R.; Baria, A.T.; Apkarian, A.V. Functional Reorganization of the Default Mode Network across Chronic Pain Conditions. PLoS ONE 2014, 9, e106133. [Google Scholar] [CrossRef]
- Davis, K.D.; Moayedi, M. Central Mechanisms of Pain Revealed Through Functional and Structural MRI. J. Neuroimmune Pharmacol. 2013, 8, 518–534. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.G.; Oliveira, L.; Erthal, F.; Joffily, M.; Mocaiber, I.F.; Volchan, E.; Pessoa, L. Emotion Affects Action: Midcingulate Cortex as a Pivotal Node of Interaction between Negative Emotion and Motor Signals. Cogn. Affect. Behav. Neurosci. 2010, 10, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Dodson, C.C.; Cordasco, F.A. Anterior Glenohumeral Joint Dislocations. Orthop. Clin. N. Am. 2008, 39, 507–518. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex Differences in Pain: A Brief Review of Clinical and Experimental Findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Kreddig, N.; Hasenbring, M.I. Pain Anxiety and Fear of (Re) Injury in Patients with Chronic Back Pain: Sex as a Moderator. Scand. J. Pain 2017, 16, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Konietzny, K.; Chehadi, O.; Streitlein-Böhme, I.; Rusche, H.; Willburger, R.; Hasenbring, M.I. Mild Depression in Low Back Pain: The Interaction of Thought Suppression and Stress Plays a Role, Especially in Female Patients. Int. J. Behav. Med. 2018, 25, 207–214. [Google Scholar] [CrossRef]
- Wise, E.A.; Price, D.D.; Myers, C.D.; Heft, M.W.; Robinson, M.E. Gender Role Expectations of Pain: Relationship to Experimental Pain Perception. Pain 2002, 96, 335–342. [Google Scholar] [CrossRef]
- Lee, K.-C.; Chiu, T.T.W.; Lam, T.-H. The Role of Fear-Avoidance Beliefs in Patients with Neck Pain: Relationships with Current and Future Disability and Work Capacity. Clin. Rehabil. 2007, 21, 812–821. [Google Scholar] [CrossRef]
- Woby, S.R.; Watson, P.J.; Roach, N.K.; Urmston, M. Adjustment to Chronic Low Back Pain—The Relative Influence of Fear-Avoidance Beliefs, Catastrophizing, and Appraisals of Control. Behav. Res. Ther. 2004, 42, 761–774. [Google Scholar] [CrossRef]
- Janela, D.; Costa, F.; Molinos, M.; Moulder, R.G.; Lains, J.; Scheer, J.K.; Bento, V.; Yanamadala, V.; Cohen, S.P.; Correia, F.D. Fear Avoidance Beliefs in Upper-Extremity Musculoskeletal Pain Conditions: Secondary Analysis of a Prospective Clinical Study on Digital Care Programs. Pain Med. Malden Mass 2022, pnac149. [Google Scholar] [CrossRef]
- Riley, S.P.; Tafuto, V.; Cote, M.; Brismée, J.-M.; Wright, A.; Cook, C. Reliability and Relationship of the Fear-Avoidance Beliefs Questionnaire with the Shoulder Pain and Disability Index and Numeric Pain Rating Scale in Patients with Shoulder Pain. Physiother. Theory Pract. 2019, 35, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Lemaster, N.G.; Hettrich, C.M.; Jacobs, C.A.; Heebner, N.; Westgate, P.M.; Mair, S.; Montgomery, J.R.; Uhl, T.L. Which Risk Factors Are Associated with Pain and Patient-Reported Function in Patients with a Rotator Cuff Tear? Clin. Orthop. 2021, 479, 1982–1992. [Google Scholar] [CrossRef] [PubMed]
- Kamonseki, D.H.; Pott-Junior, H.; Haik, M.N.; de Almeida, L.A.; Camargo, P.R. Pain-Related Fear Phenotypes Are Associated with Function of the Upper Limbs in Individuals with Shoulder Pain. Musculoskelet. Sci. Pract. 2021, 55, 102416. [Google Scholar] [CrossRef] [PubMed]
- Sh, K. Kinesiophobia: A New View of Chronic Pain Behavior. Pain Manag. 1990, 3, 35–43. [Google Scholar]
- Luque-Suarez, A.; Martinez-Calderon, J.; Navarro-Ledesma, S.; Morales-Asencio, J.M.; Meeus, M.; Struyf, F. Kinesiophobia Is Associated with Pain Intensity and Disability in Chronic Shoulder Pain: A Cross-Sectional Study. J. Manipulative Physiol. Ther. 2020, 43, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Lentz, T.A.; Barabas, J.A.; Day, T.; Bishop, M.D.; George, S.Z. The Relationship of Pain Intensity, Physical Impairment, and Pain-Related Fear to Function in Patients with Shoulder Pathology. J. Orthop. Sports Phys. Ther. 2009, 39, 270–277. [Google Scholar] [CrossRef]
- Suer, M.; Philips, N.; Kliethermes, S.; Scerpella, T.; Sehgal, N. Baseline Kinesiophobia and Pain Catastrophizing Scores Predict Prolonged Postoperative Shoulder Pain. Pain Physician 2022, 25, E285–E292. [Google Scholar]
- Henschke, N.; Ostelo, R.W.; van Tulder, M.W.; Vlaeyen, J.W.; Morley, S.; Assendelft, W.J.; Main, C.J. Behavioural Treatment for Chronic Low-Back Pain. Cochrane Database Syst. Rev. 2010, 2010, CD002014. [Google Scholar] [CrossRef]
- Harvie, D.; Moseley, G.L. ‘Pain-Related Fear: Exposure-Based Treatment of Chronic Pain’ Editors: Edited by Johan W.S. Vlaeyen, Stephen, J. Morley, Steven, J. Linton, Katja Boersma, and Jeroen de Jong, 1st Ed., IASP-Press, 196 Pages, 2012. Eur. J. Pain 2013, 17, 787–788. [Google Scholar] [CrossRef]
- Schemer, L.; Schroeder, A.; Ørnbøl, E.; Glombiewski, J.A. Exposure and Cognitive-Behavioural Therapy for Chronic Back Pain: An RCT on Treatment Processes. Eur. J. Pain Lond. Engl. 2019, 23, 526–538. [Google Scholar] [CrossRef]
- Hanel, J.; Owen, P.J.; Held, S.; Tagliaferri, S.D.; Miller, C.T.; Donath, L.; Belavy, D.L. Effects of Exercise Training on Fear-Avoidance in Pain and Pain-Free Populations: Systematic Review and Meta-Analysis. Sports Med. 2020, 50, 2193–2207. [Google Scholar] [CrossRef] [PubMed]
| Variables | Mean and SD |
|---|---|
| Age | 48.45 ± 6.05 |
| SPADI | 76.97 ± 20.91 |
| FAB | 63.4 ± 14.6 |
| FABm | 63.3 ± 14.7 |
| FABs | 63.4 ± 14.6 |
| FABe | 63.9 ± 15 |
| Variables | Age | SPADI Total Score | FACS Total Score |
|---|---|---|---|
| Age | 1.00 | 0.02 | 0.02 |
| SPADI total score | 0.02 | 1.00 | 0.97 |
| FACS total score | 0.02 | 0.97 * | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González Aroca, J.; Díaz, Á.P.; Navarrete, C.; Albarnez, L. Fear-Avoidance Beliefs Are Associated with Pain Intensity and Shoulder Disability in Adults with Chronic Shoulder Pain: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 3376. https://doi.org/10.3390/jcm12103376
González Aroca J, Díaz ÁP, Navarrete C, Albarnez L. Fear-Avoidance Beliefs Are Associated with Pain Intensity and Shoulder Disability in Adults with Chronic Shoulder Pain: A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(10):3376. https://doi.org/10.3390/jcm12103376
Chicago/Turabian StyleGonzález Aroca, Joaquín, Álvaro Puelles Díaz, Carlos Navarrete, and Loreto Albarnez. 2023. "Fear-Avoidance Beliefs Are Associated with Pain Intensity and Shoulder Disability in Adults with Chronic Shoulder Pain: A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 10: 3376. https://doi.org/10.3390/jcm12103376
APA StyleGonzález Aroca, J., Díaz, Á. P., Navarrete, C., & Albarnez, L. (2023). Fear-Avoidance Beliefs Are Associated with Pain Intensity and Shoulder Disability in Adults with Chronic Shoulder Pain: A Cross-Sectional Study. Journal of Clinical Medicine, 12(10), 3376. https://doi.org/10.3390/jcm12103376






