Prognostic Impact of Sarcopenia in Patients with Advanced Prostate Carcinoma: A Systematic Review
Abstract
1. Introduction
2. Evidence Acquisition
2.1. Information Sources and Search Strategy
2.2. Study Selection Process
2.3. Study Selection Process
2.4. Data Collection Process
2.5. Risk of Bias Assessment
2.6. Assessment of Publication Bias
2.7. Analysis and Synthesis of Results
2.8. Certainty of Evidence Assessment
3. Evidence Synthesis
3.1. Description of Included Studies
3.2. Risk of Bias in Included Studies
3.3. Synthesis of Results
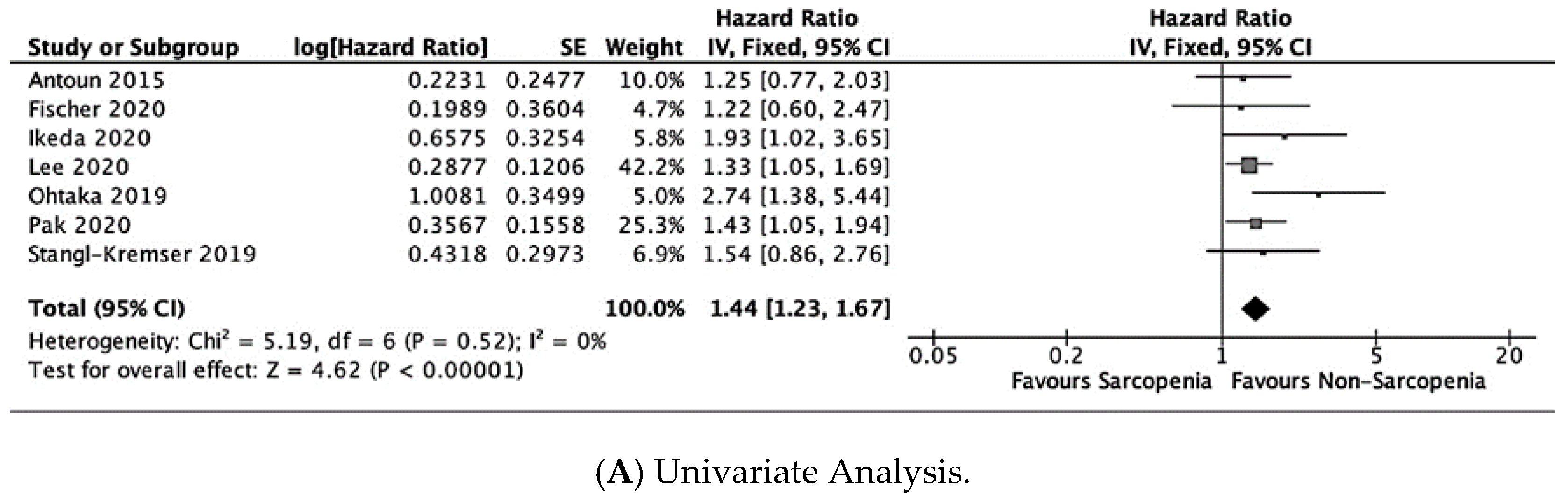
3.3.1. Overall Survival
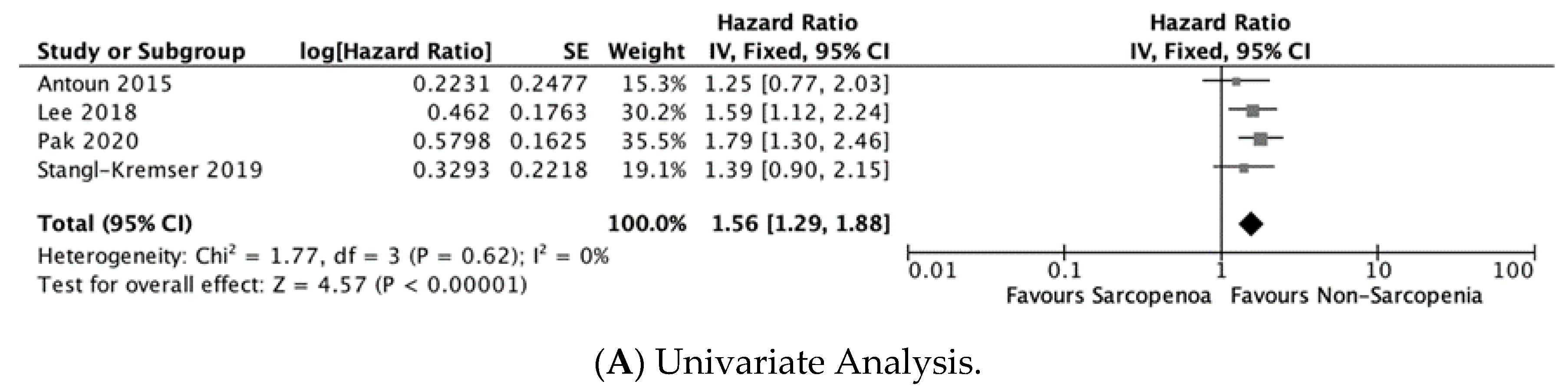
3.3.2. Cancer-Specific Survival
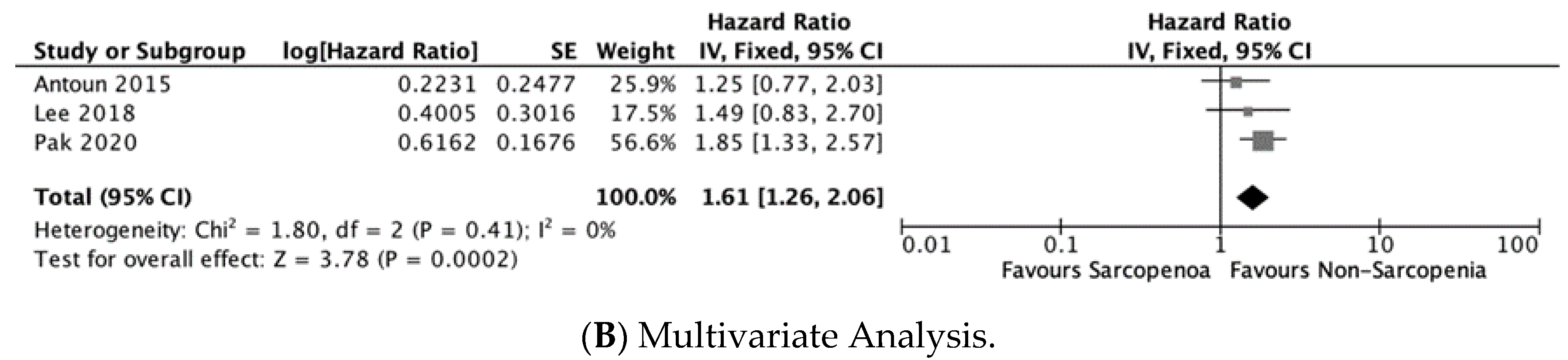
3.3.3. Progression-Free Survival
4. Discussion
5. Take Home Message
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global Cancer Incidence and Mortality Rates and Trends—An Update. Cancer Epidemiol. Biomark. Prev. 2016, 25, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Wilson, D.; Jackson, T.; Sapey, E.; Lord, J.M. Frailty and sarcopenia: The potential role of an aged immune system. Ageing Res. Rev. 2017, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.R.; Saad, F.; Egerdie, B.; Sieber, P.R.; Tammela, T.L.; Ke, C.; Leder, B.Z.; Goessl, C. Sarcopenia During Androgen-Deprivation Therapy for Prostate Cancer. J. Clin. Oncol. 2012, 30, 3271–3276. [Google Scholar] [CrossRef]
- Ubachs, J.; Ziemons, J.; Minis-Rutten, I.J.G.; Kruitwagen, R.F.P.M.; Kleijnen, J.; Lambrechts, S.; Olde Damink, S.W.M.; Rensen, S.S.; Van Gorp, T. Sarcopenia and ovarian cancer survival: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 1165–1174. [Google Scholar] [CrossRef]
- Zhang, X.-M.; Dou, Q.-L.; Zeng, Y.; Yang, Y.; Cheng, A.S.K.; Zhang, W.-W. Sarcopenia as a predictor of mortality in women with breast cancer: A meta-analysis and systematic review. BMC Cancer 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Yang, M.; Shen, Y.; Tan, L.; Li, W. Prognostic Value of Sarcopenia in Lung Cancer. Chest 2019, 156, 101–111. [Google Scholar] [CrossRef]
- Sun, G.; Li, Y.; Peng, Y.; Lu, D.; Zhang, F.; Cui, X.; Zhang, Q.; Li, Z. Can sarcopenia be a predictor of prognosis for patients with non-metastatic colorectal cancer? A systematic review and meta-analysis. Int. J. Color. Dis. 2018, 33, 1419–1427. [Google Scholar] [CrossRef]
- Pinart, M.; German Prostate Cancer Consortium (DPKK); Kunath, F.; Lieb, V.; Tsaur, I.; Wullich, B.; Schmidt, S. Prognostic models for predicting overall survival in metastatic castration-resistant prostate cancer: A systematic review. World J. Urol. 2020, 38, 613–635. [Google Scholar] [CrossRef]
- Moons, K.G.; Hooft, L.; Williams, K.; Hayden, J.A.; Damen, J.A.; Riley, R.D. Implementing systematic reviews of prognosis studies in Cochrane. Cochrane Database Syst. Rev. 2018, 10, ED000129. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hayden, J.A.; Van Der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Grooten, W.J.A.; Tseli, E.; Äng, B.O.; Boersma, K.; Stålnacke, B.-M.; Gerdle, B.; Enthoven, P. Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS—Aspects of interrater agreement. Diagn. Progn. Res. 2019, 3, 1–11. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, version 6.3 (updated February 2022); Cochrane: London, UK, 2022. [Google Scholar]
- Foroutan, F.; Guyatt, G.; Zuk, V.; Vandvik, P.O.; Alba, A.C.; Mustafa, R.; Vernooij, R.; Arevalo-Rodriguez, I.; Munn, Z.; Roshanov, P.; et al. GRADE Guidelines 28: Use of GRADE for the assessment of evidence about prognostic factors: Rating certainty in identification of groups of patients with different absolute risks. J. Clin. Epidemiology 2020, 121, 62–70. [Google Scholar] [CrossRef]
- Antoun, S.; Bayar, A.; Ileana, E.; Laplanche, A.; Fizazi, K.; di Palma, M.; Escudier, B.; Albiges, L.; Massard, C.; Loriot, Y. High subcutaneous adipose tissue predicts the prognosis in metastatic castration-resistant prostate cancer patients in post chemotherapy setting. Eur. J. Cancer 2015, 51, 2570–2577. [Google Scholar] [CrossRef]
- Fischer, S.; Clements, S.; McWilliam, A.; Green, A.; Descamps, T.; Oing, C.; Gillessen, S. Influence of abiraterone and enzalutamide on body composition in patients with metastatic castration resistant prostate cancer. Cancer Treat. Res. Commun. 2020, 25, 100256. [Google Scholar] [CrossRef]
- Ikeda, T.; Ishihara, H.; Iizuka, J.; Hashimoto, Y.; Yoshida, K.; Kakuta, Y.; Takagi, T.; Okumi, M.; Ishida, H.; Kondo, T.; et al. Prognostic impact of sarcopenia in patients with metastatic hormone-sensitive prostate cancer. Jpn. J. Clin. Oncol. 2020, 50, 933–939. [Google Scholar] [CrossRef]
- Lee, J.; Lee, H.S.; Ha, J.S.; Han, K.S.; Rha, K.H.; Hong, S.J.; Chung, B.H.; Koo, K.C. Subcutaneous Fat Distribution is a Prognostic Biomarker for Men with Castration Resistant Prostate Cancer. J. Urol. 2018, 200, 114–120. [Google Scholar] [CrossRef]
- Lee, J.; Park, J.S.; Heo, J.E.; Ahn, H.K.; Jang, W.S.; Ham, W.S.; Rha, K.H.; Choi, Y.D. Muscle Characteristics Obtained Using Computed Tomography as Prognosticators in Patients with Castration-Resistant Prostate Cancer. Cancers 2020, 12, 1864. [Google Scholar] [CrossRef]
- Muñoz-Rodríguez, J.; Domínguez, A.; Rosado, M.A.; Centeno, C.; Parejo, V.; Costa-Trachsel, I.; Gallardo, E.; Bonfill, T.; García-Rojo, D.; De Verdonces, L.; et al. Efecto de la densidad muscular en pacientes con cáncer de próstata metastásico tratados con terapia de privación androgénica. Endocrinol. Diabet. Nutr. 2021, 68, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Ohtaka, A.; Aoki, H.; Nagata, M.; Kanayama, M.; Shimizu, F.; Ide, H.; Tsujimura, A.; Horie, S. Sarcopenia is a poor prognostic factor of castration-resistant prostate cancer treated with docetaxel therapy. Prostate Int. 2019, 7, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Pak, S.; Kim, M.S.; Park, E.Y.; Kim, S.H.; Lee, K.H.; Joung, J.Y. Association of Body Composition With Survival and Treatment Efficacy in Castration-Resistant Prostate Cancer. Front. Oncol. 2020, 10, 558. [Google Scholar] [CrossRef] [PubMed]
- Stangl-Kremser, J.; Suarez-Ibarrola, R.; Andrea, D.D.; Korn, S.M.; Pones, M.; Kramer, G.; Marhold, M.; Krainer, M.; Enikeev, D.; Glybochko, P.; et al. Assessment of body composition in the advanced stage of castration-resistant prostate cancer: Special focus on sarcopenia. Prostate Cancer Prostatic Dis. 2020, 23, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.-J.; Wienke, A.; Surov, A. CT-defined low-skeletal muscle mass as a prognostic marker for survival in prostate cancer: A systematic review and meta-analysis. Urol. Oncol. Semin. Orig. Investig. 2022, 40, 103.e9–103.e16. [Google Scholar] [CrossRef]
- Jahrreiss, V.; Laukhtina, E.; D’Andrea, D.; Shariat, S.F. The prognostic value of sarcopenia in patients with prostate cancer: A systematic review. Curr. Opin. Urol. 2021, 31, 315–323. [Google Scholar] [CrossRef]
- Pamoukdjian, F.; Bouillet, T.; Lévy, V.; Soussan, M.; Zelek, L.; Paillaud, E. Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: A systematic review. Clin. Nutr. 2018, 37, 1101–1113. [Google Scholar] [CrossRef]
- Del Fabbro, E.; Parsons, H.; Warneke, C.L.; Pulivarthi, K.; Litton, J.K.; Dev, R.; Palla, S.L.; Brewster, A.; Bruera, E. The Relationship Between Body Composition and Response to Neoadjuvant Chemotherapy in Women with Operable Breast Cancer. Oncologist 2012, 17, 1240–1245. [Google Scholar] [CrossRef]
- Martin, L.; Birdsell, L.; MacDonald, N.; Reiman, T.; Clandinin, M.T.; McCargar, L.J.; Murphy, R.; Ghosh, S.; Sawyer, M.B.; Baracos, V.E. Cancer Cachexia in the Age of Obesity: Skeletal Muscle Depletion Is a Powerful Prognostic Factor, Independent of Body Mass Index. J. Clin. Oncol. 2013, 31, 1539–1547. [Google Scholar] [CrossRef]
- Shachar, S.S.; Williams, G.R.; Muss, H.B.; Nishijima, T.F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer 2016, 57, 58–67. [Google Scholar] [CrossRef]
- Antoun, S.; Borget, I.; Lanoy, E. Impact of sarcopenia on the prognosis and treatment toxicities in patients diagnosed with cancer. Curr. Opin. Support. Palliat. Care 2013, 7, 383–389. [Google Scholar] [CrossRef]
- Kondrup, J. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin. Nutr. 2002, 21, 461–468. [Google Scholar] [CrossRef]
- da Silva, F.C.; da Silva, F.M.C.; Gonçalves, F.; Santos, A.; Kliment, J.; Whelan, P.; Oliver, T.; Antoniou, N.; Pastidis, S.; Queimadelos, A.M.; et al. Locally Advanced and Metastatic Prostate Cancer Treated with Intermittent Androgen Monotherapy or Maximal Androgen Blockade: Results from a Randomised Phase 3 Study by the South European Uroncological Group. Eur. Urol. 2014, 66, 232–239. [Google Scholar] [CrossRef]
- Niraula, S.; Le, L.W.; Tannock, I.F. Treatment of Prostate Cancer with Intermittent Versus Continuous Androgen Deprivation: A Systematic Review of Randomized Trials. J. Clin. Oncol. 2013, 31, 2029–2036. [Google Scholar] [CrossRef]
- Mottet, N.; Cornford, P.; van den Bergh, R.C.N.; Briers, E.; De Santis, M.; Gillessen, S.; Grummet, J.; Henry, A.M.; van der Kwast, T.H.; Lam, T.B.; et al. EAU-EANM-ESTRO-ESUR-ISUP_SIOG Guidelines on Prostate Cancer; European Association of Urology: Arnhem, The Netherlands, 2022. [Google Scholar]
- Higano, C.; Shields, A.; Wood, N.; Brown, J.; Tangen, C. Bone mineral density in patients with prostate cancer without bone metastases treated with intermittent androgen suppression. Urology 2004, 64, 1182–1186. [Google Scholar] [CrossRef]
- Dawson, J.K.; Dorff, T.B.; Schroeder, E.T.; Lane, C.J.; Gross, M.E.; Dieli-Conwright, C.M. Impact of resistance training on body composition and metabolic syndrome variables during androgen deprivation therapy for prostate cancer: A pilot randomized controlled trial. BMC Cancer 2018, 18, 368. [Google Scholar] [CrossRef]
- Hanson, E.D.; Sheaff, A.K.; Sood, S.; Ma, L.; Francis, J.D.; Goldberg, A.P.; Hurley, B.F. Strength Training Induces Muscle Hypertrophy and Functional Gains in Black Prostate Cancer Patients Despite Androgen Deprivation Therapy. Journals Gerontol. Ser. A 2013, 68, 490–498. [Google Scholar] [CrossRef]
- Inglis, J.E.; Culakova, E.; Dunne, R.F.; Janelsins, M.C.; Lin, P.-J.; Mustian, K.M.; Peppone, L.J. Impact of high-dose vitamin d supplementation on short physical performance battery and bioelectrical impedance analysis in older patients with prostate cancer on ADT. J. Clin. Oncol. 2019, 37, e23106. [Google Scholar] [CrossRef]
- Inglis, J.E.; Fernandez, I.D.; van Wijngaarden, E.; Culakova, E.; Reschke, J.E.; Kleckner, A.S.; Lin, P.-J.; Mustian, K.M.; Peppone, L.J. Effects of High-Dose Vitamin D Supplementation on Phase Angle and Physical Function in Patients with Prostate Cancer on ADT. Nutr. Cancer 2021, 73, 1882–1889. [Google Scholar] [CrossRef]
- Kiwata, J.L.; Dorff, T.B.; Schroeder, E.T.; Salem, G.J.; Lane, C.J.; Rice, J.C.; Gross, M.E.; Dieli-Conwright, C.M. A pilot randomised controlled trial of a periodised resistance training and protein supplementation intervention in prostate cancer survivors on androgen deprivation therapy. BMJ Open 2017, 7, e016910. [Google Scholar] [CrossRef]
- Fairman, C.M.; Kendall, K.L.; Newton, R.U.; Hart, N.H.; Taaffe, D.R.; Chee, R.; Tang, C.I.; Galvão, D.A. Examining the effects of creatine supplementation in augmenting adaptations to resistance training in patients with prostate cancer undergoing androgen deprivation therapy: A randomised, double-blind, placebo-controlled trial. BMJ Open 2019, 9, e030080. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, D.; Maki, T.; Herningtyas, E.H.; Ms, N.I.; Ms, H.S.; Sugiyama, Y.; Bs, S.N.; Iida, K.; Iguchi, G.; Takahashi, Y.; et al. Branched-chain amino acids protect against dexamethasone-induced soleus muscle atrophy in rats. Muscle Nerve 2010, 41, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-J.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, 2009, CD002759. [Google Scholar] [CrossRef] [PubMed]
- Bozzetti, F. Forcing the vicious circle: Sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann. Oncol. 2017, 28, 2107–2118. [Google Scholar] [CrossRef]
- Cushen, S.J.; Power, D.G.; Murphy, K.P.; McDermott, R.; Griffin, B.T.; Lim, M.; Daly, L.; MacEneaney, P.; Sullivan, K.O.; Prado, C.M.; et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin. Nutr. ESPEN 2016, 13, e39–e45. [Google Scholar] [CrossRef]
- Attard, G.; Merseburger, A.S.; Arlt, W.; Sternberg, C.N.; Feyerabend, S.; Berruti, A.; Joniau, S.; Géczi, L.; Lefresne, F.; Lahaye, M.; et al. Assessment of the Safety of Glucocorticoid Regimens in Combination With Abiraterone Acetate for Metastatic Castration-Resistant Prostate Cancer. JAMA Oncol. 2019, 5, 1159. [Google Scholar] [CrossRef]
- Tombal, B.; Borre, M.; Rathenborg, P.; Werbrouck, P.; Van Poppel, H.; Heidenreich, A.; Iversen, P.; Braeckman, J.; Heracek, J.; Baron, B.; et al. Long-Term Antitumor Activity and Safety of Enzalutamide Monotherapy in Hormone Naïve Prostate Cancer: 3-Year Open Label Followup Results. J. Urol. 2018, 199, 459–464. [Google Scholar] [CrossRef]

| First Author, Year (Country) | Design | N | Patient | Sarcopenia | Outcomes | Follow-Up Time (Months) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age a | Inclusion Criteria | Exclusion Criteria | Metastases (N) | Cancer Treatment (%) | Definition | Prevalence (%) | Diagnosis Method | |||||
| Antoun, 2015 [18] (France) | RRR | 127 | 69 (63–74) * | Metastatic CRPCa | NR | Visceral: 15 | 1. Enzalutamide + prednisolone: 62 2. Abiraterone + prednisolone: 24 | SMI < 43 cm2/m2 (BMI < 25 kg/m2) SMI < 53 cm2/m2 (BMI > 25 kg/m2) | 66.14 | At L3 by CT scan | OS | 16 (95% CI: 12–19) |
| PFS | Sarcopenia: 4 (95% CI: 3–6) Non-sarcopenia: 5 (95% CI: 3–6) | |||||||||||
| Fischer, 2020 [19] (UK) | RCS | 90 | 69 (NR) * | Starting treatment (enzalutamide or abiraterone) for metastatic CRPCa | No imaging data | Bone: 15 Bone and lymph node: 17 Lymph node: 10 Visceral: 1 | Previous ADT: 100% 1. Enzalutamide + prednisolone: 69% 2. Abiraterone + prednisolone: 31% | SMI < 52.4 cm2/m2 | NR | At L3 by CT scan | OS | NR |
| Ikeda, 2020 [20] (Japan) | RCS | 197 | 73 (66.0–78.0) * | 1. Metastatic hormone-sensitive PCa 2. No previous treatments | Missing clinical or imaging data at diagnosis | Bone: 127 Distant lymph node: 29 Other locations: 9 | Previous ADT:100% 1. Docetaxel: 39.6% 2. Cabazitaxel: 6.7% 3. Enzalutamide: 30.6% 4. Abiraterone: 34.3% 5. Other treatment: 17.1% | SMI < 33 cm2/m2 (BMI < 25 kg/m2) SMI < 53 cm2/m2 (BMI >25 kg/m2) | 82,74 | At L3 by CT scan | OS | Sarcopenia: 72 (IQR: 50–84) Non-sarcopenia: NR (IQR: 52-NR) |
| CSS | Sarcopenia: 77 (IQR: 62-NR) Non-sarcopenia: NR (IQR: 75-NR) | |||||||||||
| Lee, 2018 [21] (Republic of Korea) | RRR | 282 | 67.0 (61.0–72.0) * | CRPCa progression | 1. Incomplete clinical data 2. Loss to follow-up 3. Unknown cause of death | Bone: 155 Lymph node: 118 Visceral: 10 | Previous ADT: 100% 1. Docetaxel + prednisolone: NR 2. Enzalutamide + prednisolone: NR 3. Abiraterone + prednisolone: NR | SMI < 52.4 | NR | At L3 by CT scan) | CSS | 15 |
| PFS | 3.7 | |||||||||||
| Lee, 2020 [22] (Republic of Korea) | RRR | 411 | 70 (65–76) * | CRPCa progression | 1. Insufficient imaging data 2. Lost to follow-up 3. Unknown cause of death | Bone: 344 Lymph node: 199 Visceral:70 | Previous ADT:100% 1. Docetaxel + prednisolone: NR 2. Cabazitaxel + prednisolone: NR 3. Enzalutamide + prednisolone: NR 4. Abiraterone + prednisolone: NR | SMI < 45.2 cm2/m2 SMA < 32.4 HU | 50.36 | At L3 by CT scan | OS | Sarcopenia: 19 Non-sarcopenia: 24 |
| Muñoz-Rodríguez, 2021 [23] (Spain) | RRR | 59 | 72.74 (12.25) | Metastatic onset PCa + first-line ADT | No imaging data | Bone: 52 Retroperitoneal lymphadenopathy: 30 Visceral: 6 | 1. ADT: 100% | European Working Group on Sarcopenia in Older People criteria [5] | NR | CT scan | OS | 32.3 (95% CI: 17.1–47.16) |
| Ohtaka, 2019 [24] (Japan) | RRR | 77 | 70 (65–76) * | CRPCa + docetaxel chemotherapy | NR | Bone: 55 Lymph node: 34 Visceral: 12 | 1. Previous ADT + docetaxel+ prednisolone: 100% | Psoas muscle index < 5.7 cm2/m2 | 33.77 | At L3-psoas muscle by CT scan | OS | 16.41 (IQR: 10.85–25.97) |
| Pak, 2020 [25] (Republic of Korea) | RRR | 230 | 68.3 (9.1) | CRPCa + first-line therapy | 1. Insufficient imaging data before starting first-line treatment 2. Patients treated for <2 months 3. Patients followed-up for <6 months | Bone: 196 Lymph node: 122 Solid organ: 28 | Previous ADT: 100% 1. Docetaxel + prednisolone: 7.0% 2. Cabazitaxel + prednisolone: 24.3% 3. Enzalutamide + prednisolone: 10.0% 4. Abiraterone + prednisolone: 13.0% 5. Other treatment + prednisolone: 2.1% | SMI < 50 cm2/m2 | 51.30 | At L3 by CT scan | OS | Sarcopenia: 16.9 Non-sarcopenia: 24.1 |
| PFS | Sarcopenia: 9.1 Non-sarcopenia: 14.9 | |||||||||||
| Stangl-Kremser, 2019 [26] (Austria) | RRR | 186 | 68,8 (64.6–75.0) * | CRPCa + chemohormonal therapy | 1. Insufficient imaging data 2. Lost to follow-up | Bone: 146 Distant lymph node: 65 Liver: 16 Visceral (No liver): 19 | 1. Docetaxel + prednisolone: 100 | SMI < 55 cm2/m2 (men) | 82.80 | At L3 by CT scan | OS | 26.2 (IQR 13.7–42.4) |
| PFS | 7.8 (IQR: 4.4–16.3) | |||||||||||
| Study | Study Participation | Study Attrition | Prognostic Factor Measurement | Outcome Measurement | Study Confounding | Statistical Analysis and Reporting | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|
| Antoun [18] | Low | Low | Low | Low | Low | Moderate | Low |
| Fischer [19] | Low | Low | Low | Low | High | High | High |
| Ikeda [20] | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Lee [21] | Low | Low | Low | Low | Low | Moderate | Low |
| Lee [22] | Low | Low | Low | Low | Low | Moderate | Low |
| Muñoz-Rodríguez [23] | Low | Low | Low | Low | Low | Moderate | Low |
| Ohtaka [24] | Low | Low | Low | Low | Low | Moderate | Low |
| Pak [25] | Low | Low | Low | Low | Low | Moderate | Low |
| Stangl-Kremser [26] | Low | High | High | Low | Moderate | Moderate | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Pablos-Rodríguez, P.; del Pino-Sedeño, T.; Infante-Ventura, D.; de Armas-Castellano, A.; Ramírez Backhaus, M.; Ferrer, J.F.L.; de Pablos-Velasco, P.; Rueda-Domínguez, A.; Trujillo-Martín, M.M. Prognostic Impact of Sarcopenia in Patients with Advanced Prostate Carcinoma: A Systematic Review. J. Clin. Med. 2023, 12, 57. https://doi.org/10.3390/jcm12010057
de Pablos-Rodríguez P, del Pino-Sedeño T, Infante-Ventura D, de Armas-Castellano A, Ramírez Backhaus M, Ferrer JFL, de Pablos-Velasco P, Rueda-Domínguez A, Trujillo-Martín MM. Prognostic Impact of Sarcopenia in Patients with Advanced Prostate Carcinoma: A Systematic Review. Journal of Clinical Medicine. 2023; 12(1):57. https://doi.org/10.3390/jcm12010057
Chicago/Turabian Stylede Pablos-Rodríguez, Pedro, Tasmania del Pino-Sedeño, Diego Infante-Ventura, Aythami de Armas-Castellano, Miguel Ramírez Backhaus, Juan Francisco Loro Ferrer, Pedro de Pablos-Velasco, Antonio Rueda-Domínguez, and María M. Trujillo-Martín. 2023. "Prognostic Impact of Sarcopenia in Patients with Advanced Prostate Carcinoma: A Systematic Review" Journal of Clinical Medicine 12, no. 1: 57. https://doi.org/10.3390/jcm12010057
APA Stylede Pablos-Rodríguez, P., del Pino-Sedeño, T., Infante-Ventura, D., de Armas-Castellano, A., Ramírez Backhaus, M., Ferrer, J. F. L., de Pablos-Velasco, P., Rueda-Domínguez, A., & Trujillo-Martín, M. M. (2023). Prognostic Impact of Sarcopenia in Patients with Advanced Prostate Carcinoma: A Systematic Review. Journal of Clinical Medicine, 12(1), 57. https://doi.org/10.3390/jcm12010057