Prevalence of Hyperuricemia and Its Association with Cardiovascular Risk Factors and Subclinical Target Organ Damage
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Selection of Patients
2.3. Variables Recorded
2.4. Statistical Analysis
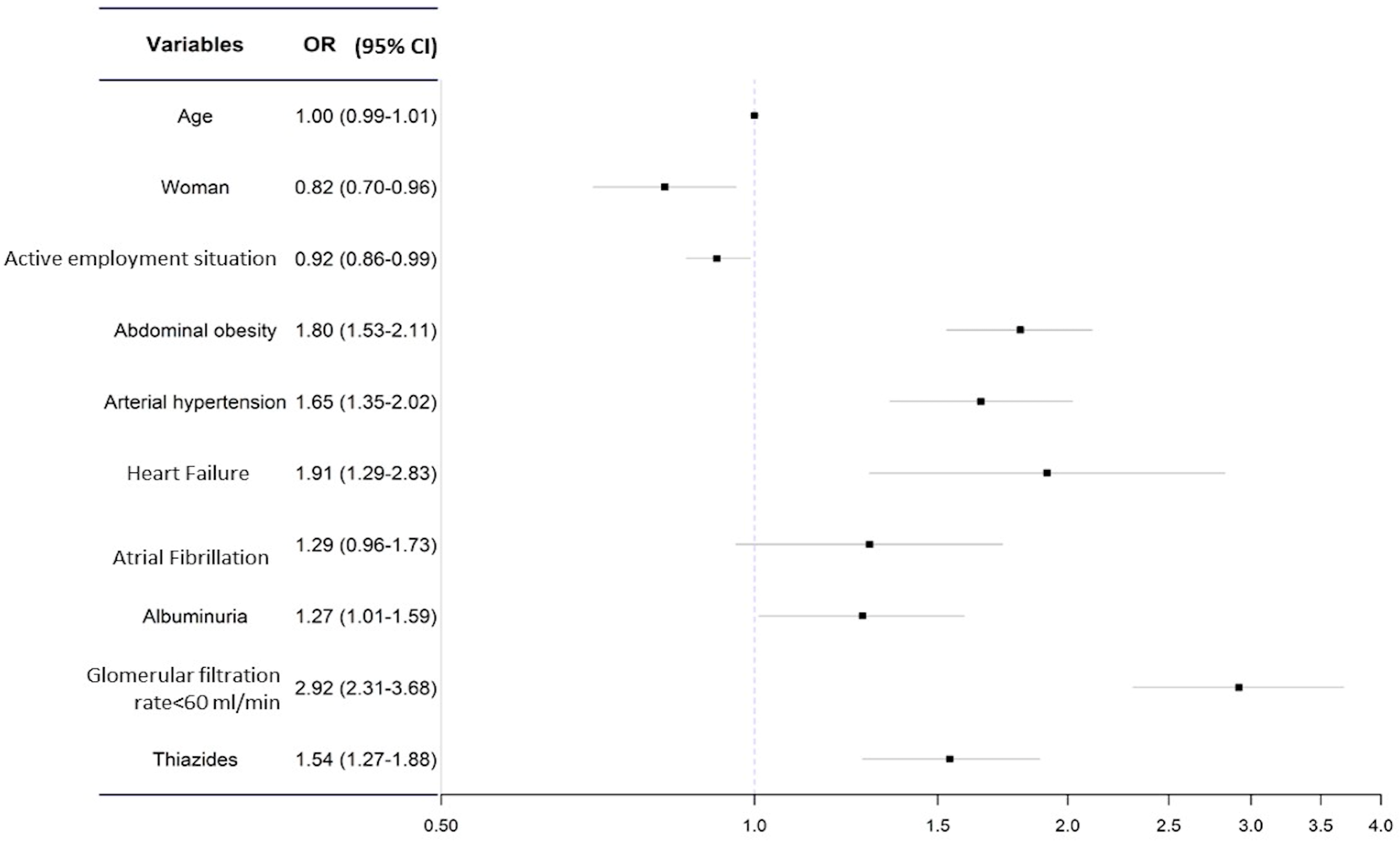
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. The Investigators of the IBERICAN Study and of the Spanish Society of Primary Care Physicians (SEMERGEN) Foundation
References
- Instituto Nacional de Estadística (INE). Defunciones Según La Causa de Muerte. In Enero-Mayo 2019 y 2020; Instituto Nacional de Estadística: Madrid, Spain, 2020. [Google Scholar]
- Soriano, J.B.; Rojas-Rueda, D.; Alonso, J.; Antó, J.M.; Cardona, P.-J.; Fernández, E.; Garcia-Basteiro, A.L.; Benavides, F.G.; Glenn, S.D.; Krish, V.; et al. La Carga de Enfermedad En España: Resultados Del Estudio de La Carga Global de Las Enfermedades 2016. Med. Clin. 2018, 151, 171–190. [Google Scholar] [CrossRef] [PubMed]
- O’Flaherty, M.; Buchan, I.; Capewell, S. Contributions of Treatment and Lifestyle to Declining CVD Mortality: Why Have CVD Mortality Rates Declined so Much since the 1960s? Heart 2013, 99, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Ridker, P.M.; Maseri, A. Inflammation and Atherosclerosis. Circulation 2002, 105, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Corry, D.B.; Tuck, M.L. Uric Acid and the Vasculature. Curr. Hypertens. Rep. 2006, 8, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Bagnati, M.; Perugini, C.; Cau, C.; Bordone, R.; Albano, E.; Bellomo, G. When and Why a Water-Soluble Antioxidant Becomes pro-Oxidant during Copper-Induced Low-Density Lipoprotein Oxidation: A Study Using Uric Acid. Biochem. J. 1999, 340, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Corry, D.B.; Eslami, P.; Yamamoto, K.; Nyby, M.D.; Makino, H.; Tuck, M.L. Uric Acid Stimulates Vascular Smooth Muscle Cell Proliferation and Oxidative Stress via the Vascular Renin–Angiotensin System. J. Hypertens. 2008, 26, 269–275. [Google Scholar] [CrossRef]
- Kanellis, J.; Watanabe, S.; Li, J.H.; Kang, D.H.; Li, P.; Nakagawa, T.; Wamsley, A.; Sheikh-Hamad, D.; Lan, H.Y.; Feng, L.; et al. Uric Acid Stimulates Monocyte Chemoattractant Protein-1 Production in Vascular Smooth Muscle Cells Via Mitogen-Activated Protein Kinase and Cyclooxygenase-2. Hypertension 2003, 41, 1287–1293. [Google Scholar] [CrossRef]
- Patetsios, P.; Rodino, W.; Wisselink, W.; Bryan, D.; Kirwin, J.D.; Panetta, T.F. Identification of Uric Acid in AorticAneurysms and Atherosclerotic Artery. Ann. N. Y. Acad. Sci. 1996, 800, 243–245. [Google Scholar] [CrossRef]
- Desideri, G.; Castaldo, G.; Lombardi, A.; Mussap, M.; Testa, A.; Pontremoli, R.; Punzi, L.; Borghi, C. Is It Time to Revise the Normal Range of Serum Uric Acid Levels? Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 1295–1306. [Google Scholar]
- Verdecchia, P.; Schillaci, G.; Reboldi, G.; Santeusanio, F.; Porcellati, C.; Brunetti, P. Relation Between Serum Uric Acid and Risk of Cardiovascular Disease in Essential Hypertension. Hypertension 2000, 36, 1072–1078. [Google Scholar] [CrossRef]
- Liu, L.; Gu, Y.; Li, C.; Zhang, Q.; Meng, G.; Wu, H.; Du, H.; Shi, H.; Xia, Y.; Guo, X.; et al. Serum Uric Acid Is an Independent Predictor for Developing Prehypertension: A Population-Based Prospective Cohort Study. J. Hum. Hypertens. 2017, 31, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Kao, T.W.; Yang, H.F.; Chou, C.W.; Wu, C.J.; Lai, C.H.; Sun, Y.S.; Wang, C.C.; Chen, W.L. The Association of Uric Acid with the Risk of Metabolic Syndrome, Arterial Hypertension or Diabetes in Young Subjects—An Observational Study. Clin. Chim. Acta 2018, 478, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Lurbe, E.; Torro, M.I.; Alvarez-Pitti, J.; Redon, J.; Borghi, C.; Redon, P. Uric Acid Is Linked to Cardiometabolic Risk Factors in Overweight and Obese Youths. J. Hypertens. 2018, 36, 1840–1846. [Google Scholar] [CrossRef] [PubMed]
- Rocha, E.P.A.A.; Vogel, M.; Stanik, J.; Pietzner, D.; Willenberg, A.; Körner, A.; Kiess, W. Serum Uric Acid Levels as an Indicator for Metabolically Unhealthy Obesity in Children and Adolescents. Horm. Res. Paediatr. 2018, 90, 19–27. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Grandi, E.; Rosticci, M.; D’Addato, S.; Borghi, C. Serum Uric Acid Predicts Incident Metabolic Syndrome in the Elderly in an Analysis of the Brisighella Heart Study. Sci. Rep. 2018, 8, 11529. [Google Scholar] [CrossRef]
- Franssen, W.M.A.; Beyens, M.; Al Hatawe, T.; Frederix, I.; Verboven, K.; Dendale, P.; Eijnde, B.O.; Massa, G.; Hansen, D. Cardiac Function in Adolescents with Obesity: Cardiometabolic Risk Factors and Impact on Physical Fitness. Int. J. Obes. 2019, 43, 1400–1410. [Google Scholar] [CrossRef]
- Chang, H.-Y.; Lee, P.-H.; Lei, C.-C.; Tung, C.-W.; Hsu, Y.-C.; Huang, T.-J.; Lu, L.; Lin, C.-L. Hyperuricemia Is an Independent Risk Factor for New Onset Micro-Albuminuria in a Middle-Aged and Elderly Population: A Prospective Cohort Study in Taiwan. PLoS ONE 2013, 8, e61450. [Google Scholar] [CrossRef]
- Culleton, B.F.; Larson, M.G.; Kannel, W.B.; Levy, D. Serum Uric Acid and Risk for Cardiovascular Disease and Death: The Framingham Heart Study. Ann. Intern. Med. 1999, 131, 7. [Google Scholar] [CrossRef]
- Maloberti, A.; Giannattasio, C.; Bombelli, M.; Desideri, G.; Cicero, A.F.G.; Muiesan, M.L.; Rosei, E.A.; Salvetti, M.; Ungar, A.; Rivasi, G.; et al. Hyperuricemia and Risk of Cardiovascular Outcomes: The Experience of the URRAH (Uric Acid Right for Heart Health) Project. High Blood Press. Cardiovasc. Prev. 2020, 27, 121–128. [Google Scholar] [CrossRef]
- Maloberti, A.; Bombelli, M.; Facchetti, R.; Barbagallo, C.M.; Bernardino, B.; Rosei, E.A.; Casiglia, E.; Cicero, A.F.G.; Cirillo, M.; Cirillo, P.; et al. Relationships between Diuretic-Related Hyperuricemia and Cardiovascular Events: Data from the URic Acid Right for HeArt Health Study. J. Hypertens. 2021, 39, 333–340. [Google Scholar] [CrossRef]
- de Leeuw, P.W.; Thijs, L.; Birkenhäger, W.H.; Voyaki, S.M.; Efstratopoulos, A.D.; Fagard, R.H.; Leonetti, G.; Nachev, C.; Petrie, J.C.; Rodicio, J.L.; et al. Prognostic Significance of Renal Function in Elderly Patients with Isolated Systolic Hypertension: Results from the Syst-Eur Trial. J. Am. Soc. Nephrol. 2002, 13, 2213–2222. [Google Scholar] [CrossRef] [PubMed]
- Ndrepepa, G.; Braun, S.; Haase, H.U.; Schulz, S.; Ranftl, S.; Hadamitzky, M.; Mehilli, J.; Schömig, A.; Kastrati, A. Prognostic Value of Uric Acid in Patients with Acute Coronary Syndromes. Am. J. Cardiol. 2012, 109, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Qin, J.; Deng, X.; Luo, G.; Yu, D.; Zhang, M.; Zhou, S.; Wang, L. Prognostic Value of Serum Uric Acid in Patients with Acute Heart Failure: A Meta-Analysis. Medicine 2019, 98, e14525. [Google Scholar] [CrossRef] [PubMed]
- Cinza Sanjurjo, S.; Llisterri Caro, J.L.; Barquilla García, A.; Polo García, J.; Velilla Zancada, S.; Rodríguez Roca, G.C.; Micó Pérez, R.M.; Martín Sánchez, V.; Prieto Díaz, M.Á. Descripción de La Muestra, Diseño y Métodos Del Estudio Para La Identificación de La Población Española de Riesgo Cardiovascular y Renal (IBERICAN). Med. Fam. Semer. 2020, 46, 4–15. [Google Scholar] [CrossRef]
- Matsushita, K.; Mahmoodi, B.K.; Woodward, M.; Emberson, J.R.; Jafar, T.H.; Jee, S.H.; Polkinghorne, K.R.; Shankar, A.; Smith, D.H.; Tonelli, M.; et al. Comparison of Risk Prediction Using the CKD-EPI Equation and the MDRD Study Equation for Estimated Glomerular Filtration Rate. JAMA 2012, 307, 1941–1951. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the Management of Arterial Hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 2284–2309. [Google Scholar] [CrossRef]
- Cinza-Sanjurjo, S.; Micó-Pérez, R.M.; Velilla-Zancada, S.; Prieto-Díaz, M.A.; Rodríguez-Roca, G.C.; Barquilla García, A.; Polo García, J.; Martín Sánchez, V.; Llisterri Caro, J.L. Factores Asociados al Riesgo Cardiovascular y Enfermedad Cardiovascular y Renal En El Estudio IBERICAN (Identificación de La PoBlación Española de RIesgo CArdiovascular y ReNal): Resultados Definitivos. Med. Fam. Semer. 2020, 46, 368–378. [Google Scholar] [CrossRef]
- Maloberti, A.; Maggioni, S.; Occhi, L.; Triglione, N.; Panzeri, F.; Nava, S.; Signorini, S.; Falbo, R.; Casati, M.; Grassi, G.; et al. Sex-Related Relationships between Uric Acid and Target Organ Damage in Hypertension. J. Clin. Hypertens. 2018, 20, 193–200. [Google Scholar] [CrossRef]
- Miao, Z.; Li, C.; Chen, Y.; Zhao, S.; Wang, Y.; Wang, Z.; Chen, X.; Xu, F.; Wang, F.; Sun, R.; et al. Dietary and Lifestyle Changes Associated with High Prevalence of Hyperuricemia and Gout in the Shandong Coastal Cities of Eastern China. J. Rheumatol. 2008, 35, 1859–1864. [Google Scholar]
- Huang, X.-B.; Zhang, W.-Q.; Tang, W.-W.; Liu, Y.; Ning, Y.; Huang, C.; Liu, J.-X.; Yi, Y.-J.; Xu, R.-H.; Wang, T.-D. Prevalence and Associated Factors of Hyperuricemia among Urban Adults Aged 35–79 Years in Southwestern China: A Community-Based Cross-Sectional Study. Sci. Rep. 2020, 10, 15683. [Google Scholar] [CrossRef]
- Zitt, E.; Fischer, A.; Lhotta, K.; Concin, H.; Nagel, G. Sex- and Age-Specific Variations, Temporal Trends and Metabolic Determinants of Serum Uric Acid Concentrations in a Large Population-Based Austrian Cohort. Sci. Rep. 2020, 10, 7578. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, M.; Kuwabara, R.; Niwa, K.; Hisatome, I.; Smits, G.; Roncal-Jimenez, C.; MacLean, P.; Yracheta, J.; Ohno, M.; Lanaspa, M.; et al. Different Risk for Hypertension, Diabetes, Dyslipidemia, and Hyperuricemia According to Level of Body Mass Index in Japanese and American Subjects. Nutrients 2018, 10, 1011. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Girerd, N.; Machu, J.-L.; Bozec, E.; Duarte, K.; Boivin, J.-M.; Wagner, S.; Ferreira, J.P.; Zannad, F.; Rossignol, P. Impact of Uric Acid on Hypertension Occurrence and Target Organ Damage: Insights From the STANISLAS Cohort With a 20-Year Follow-Up. Am. J. Hypertens. 2020, 33, 869–878. [Google Scholar] [CrossRef]
- Jia, Z.; Zhang, X.; Kang, S.; Wu, Y. Serum Uric Acid Levels and Incidence of Impaired Fasting Glucose and Type 2 Diabetes Mellitus: A Meta-Analysis of Cohort Studies. Diabetes Res. Clin. Pract. 2013, 101, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Liu, J.; Solomon, D.H. Risk of Incident Diabetes in Patients with Gout: A Cohort Study. Arthritis Rheumatol. 2015, 67, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Fan, Y.; Liu, Q.; Liu, K.; Chen, F.; Tang, X.; Li, G.; Hu, D.; Song, G. Sex-Specific Association of Serum Uric Acid Dynamics with the Incidence of Metabolic Syndrome in a Health Check-up Chinese Population: A Prospective Cohort Study. BMJ Open 2020, 10, e035289. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Jiang, Y.; Huang, Y.; Song, W.; Li, X.; Huang, Y.; Ou, J.; Wei, Q.; Gu, J. The Comparison of Dyslipidemia and Serum Uric Acid in Patients with Gout and Asymptomatic Hyperuricemia: A Cross-Sectional Study. Lipids Health Dis. 2020, 19, 31. [Google Scholar] [CrossRef] [PubMed]
- de Magalhães, E.L.G.; Juvanhol, L.L.; da Silva, D.C.G.; Ferreira, F.G.; Roberto, D.M.T.; Hinnig, P.D.F.; Longo, G.Z. Uric Acid: A New Marker for Metabolic Syndrome? Results of a Population-Based Study with Adults. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2077–2080. [Google Scholar] [CrossRef]
- Baldwin, W.; McRae, S.; Marek, G.; Wymer, D.; Pannu, V.; Baylis, C.; Johnson, R.J.; Sautin, Y.Y. Hyperuricemia as a Mediator of the Proinflammatory Endocrine Imbalance in the Adipose Tissue in a Murine Model of the Metabolic Syndrome. Diabetes 2011, 60, 1258–1269. [Google Scholar] [CrossRef]
- Visco, V.; Pascale, A.V.; Virtuoso, N.; Mongiello, F.; Cinque, F.; Gioia, R.; Finelli, R.; Mazzeo, P.; Manzi, M.V.; Morisco, C.; et al. Serum Uric Acid and Left Ventricular Mass in Essential Hypertension. Front. Cardiovasc. Med. 2020, 7, 1–10. [Google Scholar] [CrossRef]
- Chernatska, O.M.; Prystupa, L.N.; Fadieieva, H.A.; Liashenko, A.V.; Smiianova, Y.O. Arterial Hypertension Associated with Hyperuricemia: Features of Heart Damage. Wiad. Lek. 2020, 73, 943–946. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, C.; Yan, Y.; Yuan, Y.; Wang, K.K.; Chu, C.; Hu, J.W.; Ma, Q.; Liao, Y.Y.; Fu, B.W.; et al. Association of Uric Acid in Serum and Urine with Subclinical Renal Damage: Hanzhong Adolescent Hypertension Study. PLoS ONE 2019, 14, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Muiesan, M.L.; Agabiti-Rosei, C.; Paini, A.; Salvetti, M. Uric Acid and Cardiovascular Disease: An Update. Eur. Cardiol. 2016, 11, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Kawada, T. Risk of cardiovascular and all-cause events in hyperuricemia patients with special reference to diuretic use. J. Hypertens. 2022, 40, 409. [Google Scholar] [CrossRef] [PubMed]
- Eun, Y.; Han, K.-D.; Kim, D.H.; Kim, I.Y.; Park, E.-J.; Lee, S.; Cha, H.-S.; Koh, E.-M.; Lee, J.; Kim, H. Increased Overall Heart Rate Irregularity Risk by Hyperuricemia in the General Population: Results from the Korean National Health and Nutrition Examination Survey. Medicina 2020, 56, 501. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Kuwabara, M.; Johnson, R.; Bove, M.; Fogacci, F.; Rosticci, M.; Giovannini, M.; D’Addato, S.; Borghi, C. LDL-Oxidation, Serum Uric Acid, Kidney Function and Pulse-Wave Velocity: Data from the Brisighella Heart Study Cohort. Int. J. Cardiol. 2018, 261, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Oh, T.R.; Choi, H.S.; Kim, C.S.; Bae, E.H.; Ma, S.K.; Sung, S.-A.; Kim, Y.-S.; Oh, K.H.; Ahn, C.; Kim, S.W. Hyperuricemia Has Increased the Risk of Progression of Chronic Kidney Disease: Propensity Score Matching Analysis from the KNOW-CKD Study. Sci. Rep. 2019, 9, 6681. [Google Scholar] [CrossRef]
- Russo, E.; Verzola, D.; Leoncini, G.; Cappadona, F.; Esposito, P.; Pontremoli, R.; Viazzi, F. Treating Hyperuricemia: The Last Word Hasn’t Been Said Yet. J. Clin. Med. 2021, 10, 819. [Google Scholar] [CrossRef]
- Moriel, P.; Sevanian, A.; Ajzen, S.; Zanella, M.T.; Plavnik, F.L.; Rubbo, H.; Abdalla, D.S.P. Nitric Oxide, Cholesterol Oxides and Endothelium-Dependent Vasodilation in Plasma of Patients with Essential Hypertension. Braz. J. Med. Biol. Res. 2002, 35, 1301–1309. [Google Scholar] [CrossRef]
- Forman, J.P.; Choi, H.; Curhan, G.C. Uric Acid and Insulin Sensitivity and Risk of Incident Hypertension. Arch. Intern. Med. 2009, 169, 155. [Google Scholar] [CrossRef]
- Tsushima, Y.; Nishizawa, H.; Tochino, Y.; Nakatsuji, H.; Sekimoto, R.; Nagao, H.; Shirakura, T.; Kato, K.; Imaizumi, K.; Takahashi, H.; et al. Uric Acid Secretion from Adipose Tissue and Its Increase in Obesity. J. Biol. Chem. 2013, 288, 27138–27149. [Google Scholar] [CrossRef] [PubMed]
- Akbari, P.; Khorasani-Zadeh, A. Thiazide Diuretics; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
| Variable | N | n | % | OR 95% CI | aOR 95% CI | |
|---|---|---|---|---|---|---|
| Sex | Man | 3188 | 597 | 18.7 | 0.72 [0.63–0.81] | 0.73 [0.64–0.84] |
| Female | 3739 | 529 | 14.1 | |||
| Race | White | 6678 | 1097 | 16.4 | ||
| Others | 249 | 29 | 11.6 | 0.67 [0.45–0.99] | 0.78 [0.52–1.16] | |
| Habitat | Urban | 4061 | 683 | 16.8 | ||
| Semi-urban | 1474 | 237 | 16.1 | 0.95 [0.81–1.11] | 0.97 [0.82–1.15] | |
| Rural | 1390 | 206 | 14.8 | 0.86 [0.73–1.02] | 0.82 [0.68–0.97] | |
| Education | Uneducated | 627 | 136 | 21.7 | ||
| Primary | 3814 | 622 | 16.3 | 0.70 [0.57–0.87] | 0.80 [0.64–0.99] | |
| Secondary | 1561 | 251 | 16.1 | 0.69 [0.55–0.87] | 0.88 [0.67–1.14] | |
| Tertiary | 925 | 117 | 12.6 | 0.52 [0.40–0.69] | 0.70 [0.51–0.96] | |
| Employment | Employed | 2914 | 404 | 13.9 | ||
| Unemployed | 569 | 69 | 12.1 | 0.86 [0.65–1.13] | 0.88 [0.66–1.17] | |
| Retired | 2485 | 514 | 20.7 | 1.62 [1.04–1.87] | 0.93 [0.76–1.14] | |
| Student | 76 | 6 | 7.9 | 0.53 [0.23–1.23] | 0.95 [0.40–2.24] | |
| Domestic chores | 861 | 131 | 15.2 | 1.11 [0.90–1.38] | 0.92 [0.71–1.18] | |
| Salary (EUR/year) | <18,000 | 2920 | 490 | 16.8 | ||
| ≥18,000 | 4007 | 636 | 15.9 | 0.94 [0.82–1.06] | 1.01 [0.87–1.16] | |
| Age, mean (SD) | HU | 62.7 (13.3) | 1.02 [1.02–1.03] | 1.02 [1.02–1.03] | ||
| No HU | 57.9 (14.7) | |||||
| Variable | N | n | % | OR 95% CI | aOR 95% CI | ||
|---|---|---|---|---|---|---|---|
| CVRF | Abdominal Obesity | No | 4691 | 573 | 12.2 | 2.25 [1.97–2.58] | 1.56 [1.09–2.24] |
| Yes | 2074 | 513 | 24.7 | ||||
| Obesity | No | 4445 | 531 | 11.9 | 2.20 [1.92–2.52] | 1.29 [0.90–1.84] | |
| Yes | 2320 | 555 | 23.9 | ||||
| HTN | No | 3469 | 340 | 9.8 | 2.31 [1.97–2.70] | 1.95 [1.66–2.30] | |
| Yes | 3292 | 746 | 22.7 | ||||
| Hypercholesterolemia | No | 3319 | 422 | 12.7 | 1.32 [1.15–1.52] | 1.19 [1.03–1.37] | |
| Yes | 3443 | 664 | 19.3 | ||||
| Sedentary | No | 4795 | 713 | 14.9 | 1.31 [1.14–1.51] | 1.12 [0.97–1.30] | |
| Yes | 1970 | 373 | 18.9 | ||||
| DM | No | 5406 | 804 | 14.9 | 1.19 [1.02–1.39] | 0.93 [0.79–1.10] | |
| Yes | 1359 | 282 | 20.8 | ||||
| Smoking | No | 5591 | 928 | 16.6 | 0.91 [0.75–1.10] | 0.94 [0.79–1.15] | |
| Yes | 1174 | 158 | 13.5 | ||||
| TOD | PP > 60 | No | 5602 | 829 | 14.8 | 1.13 [0.94–1.36] | 1.1 [0.92–1.32] |
| Yes | 1163 | 257 | 22.1 | ||||
| Left ventricular hypertrophy | No | 6516 | 1022 | 15.7 | 1.44 [1.07–1.94] | 1.36 [1.00–1.83] | |
| Yes | 249 | 64 | 25.7 | ||||
| ABI < 0.9 | No | 6636 | 1060 | 16 | 1.14 [0.73–1.77] | 1.06 [0.68–1.66] | |
| Yes | 129 | 26 | 20.2 | ||||
| History of cardiovascular disease | Stroke | No | 6491 | 1030 | 15.9 | 1.10 [0.81–1.5] | 1.00 [0.73–1.37] |
| Yes | 274 | 56 | 20.4 | ||||
| Ischemic heart disease | No | 6277 | 996 | 15.9 | 0.96 [0.75–1.22] | 0.89 [0.69–1.14] | |
| Yes | 488 | 90 | 18.4 | ||||
| Atrial fibrillation | No | 6386 | 973 | 15.2 | 1.76 [1.39–2.23] | 1.53 [1.19–1.98] | |
| Yes | 379 | 113 | 29.8 | ||||
| Heart failure | No | 6582 | 1021 | 15.5 | 2.31 [1.68–3.18] | 2.02 [1.44–2.83] | |
| Yes | 183 | 65 | 35.5 | ||||
| Peripheral Artery Disease | No | 6548 | 1045 | 16 | 0.98 [0.69–1.39] | 0.88 [0.62–1.27] | |
| Yes | 217 | 41 | 18.9 | ||||
| Kidney disease | eGFR < 60 mL/min | No | 6212 | 859 | 13.8 | 3.66 [3.01–4.46] | 3.01 [2.40–3.78] |
| Yes | 548 | 226 | 41.2 | ||||
| Albuminuria | No | 4500 | 687 | 15.3 | 1.70 [1.38–2.11] | 1.43 [1.14–1.78] | |
| Yes | 546 | 143 | 26.2 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antelo-Pais, P.; Prieto-Díaz, M.Á.; Micó-Pérez, R.M.; Pallarés-Carratalá, V.; Velilla-Zancada, S.; Polo-García, J.; Barquilla-García, A.; Ginel-Mendoza, L.; Segura-Fragoso, A.; Vitelli-Storelli, F.; et al. Prevalence of Hyperuricemia and Its Association with Cardiovascular Risk Factors and Subclinical Target Organ Damage. J. Clin. Med. 2023, 12, 50. https://doi.org/10.3390/jcm12010050
Antelo-Pais P, Prieto-Díaz MÁ, Micó-Pérez RM, Pallarés-Carratalá V, Velilla-Zancada S, Polo-García J, Barquilla-García A, Ginel-Mendoza L, Segura-Fragoso A, Vitelli-Storelli F, et al. Prevalence of Hyperuricemia and Its Association with Cardiovascular Risk Factors and Subclinical Target Organ Damage. Journal of Clinical Medicine. 2023; 12(1):50. https://doi.org/10.3390/jcm12010050
Chicago/Turabian StyleAntelo-Pais, Paula, Miguel Ángel Prieto-Díaz, Rafael M. Micó-Pérez, Vicente Pallarés-Carratalá, Sonsoles Velilla-Zancada, José Polo-García, Alfonso Barquilla-García, Leovigildo Ginel-Mendoza, Antonio Segura-Fragoso, Facundo Vitelli-Storelli, and et al. 2023. "Prevalence of Hyperuricemia and Its Association with Cardiovascular Risk Factors and Subclinical Target Organ Damage" Journal of Clinical Medicine 12, no. 1: 50. https://doi.org/10.3390/jcm12010050
APA StyleAntelo-Pais, P., Prieto-Díaz, M. Á., Micó-Pérez, R. M., Pallarés-Carratalá, V., Velilla-Zancada, S., Polo-García, J., Barquilla-García, A., Ginel-Mendoza, L., Segura-Fragoso, A., Vitelli-Storelli, F., Martín-Sánchez, V., Hermida-Ameijerias, Á., & Cinza-Sanjurjo, S., on behalf of the Investigators of the IBERICAN Study and of the Spanish Society of Primary Care Physicians (SEMERGEN) Foundation. (2023). Prevalence of Hyperuricemia and Its Association with Cardiovascular Risk Factors and Subclinical Target Organ Damage. Journal of Clinical Medicine, 12(1), 50. https://doi.org/10.3390/jcm12010050







