Safety of Sirolimus in Patients with Tuberous Sclerosis Complex under Two Years of Age—A Bicenter Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
- Clinical or genetic diagnosis of TSC;
- Treatment with oral sirolimus before the age of two years;
- A follow-up at least three months after the initiation of treatment.
- Genetic analysis results: TSC1 or TSC2 gene mutation;
- Sex;
- Age at the initiation of mTOR inhibitor treatment;
- Age at the onset of epileptic seizures;
- Reason for mTOR inhibitor treatment;
- Whether antiepileptic drugs (ASMs) were included;
- If the ASM treatment was preventive.
- Age: from birth to 6 months of age, 6–12 months, 12–24 months, and 24–36 months of age.
- Treatment duration (months).
2.2. Study Outcomes
- Grade 1: Mild
- Grade 2: Moderate
- Grade 3: Severe, of medical significance
- Grade 4: Life-threatening consequences
- Grade 5: Death related to AE
2.3. Statistical Analysis
3. Results
3.1. Reasons for mTOR Inhibitor Treatment
3.2. Sirolimus Dosing
3.3. Data Collection
3.4. Long-Term mTOR Inhibitor Continuation
3.5. Additional Therapies
3.6. The Safety Profile of Sirolimus Therapy
4. Discussion
4.1. Hyperlipidemia
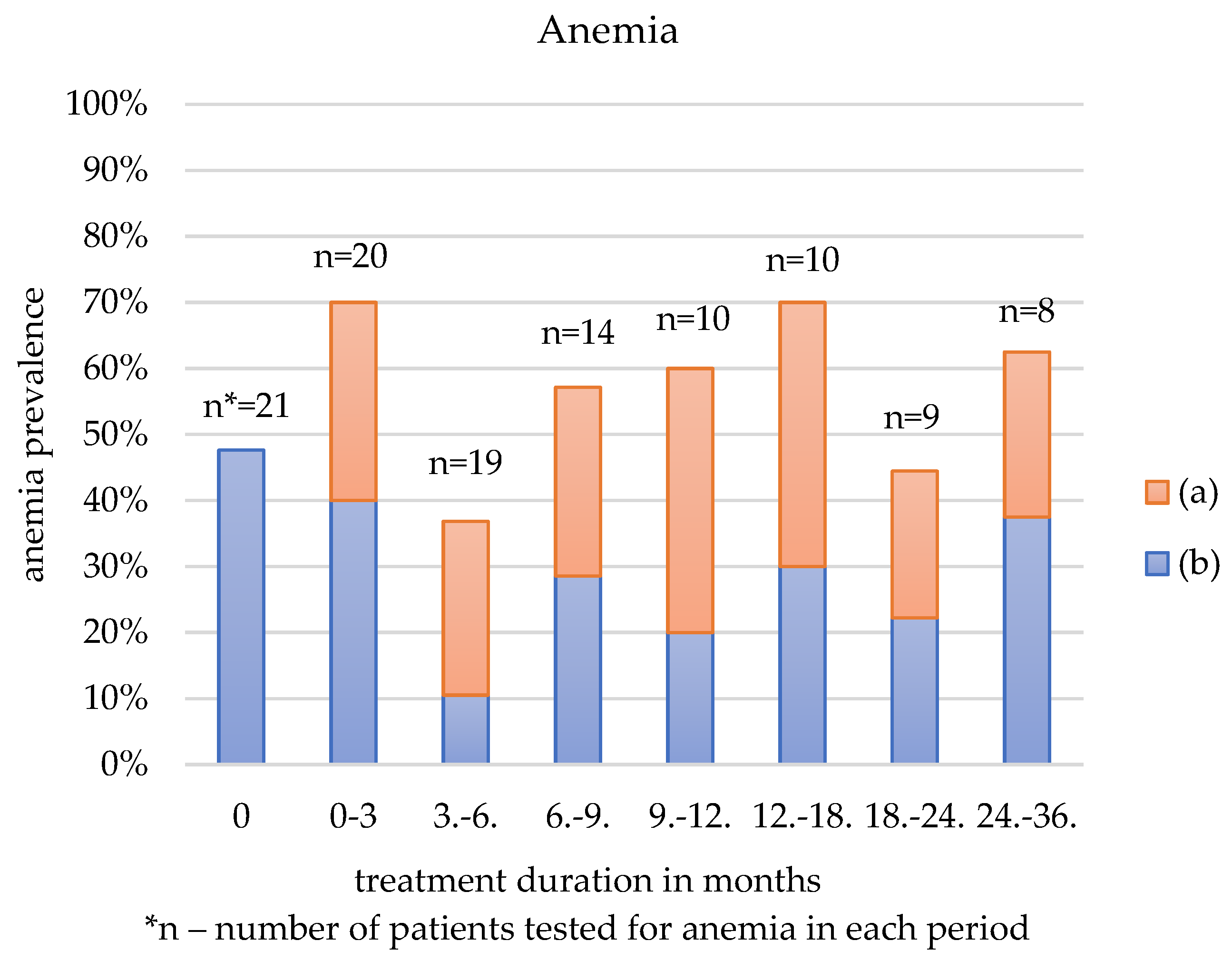
4.2. Anemia
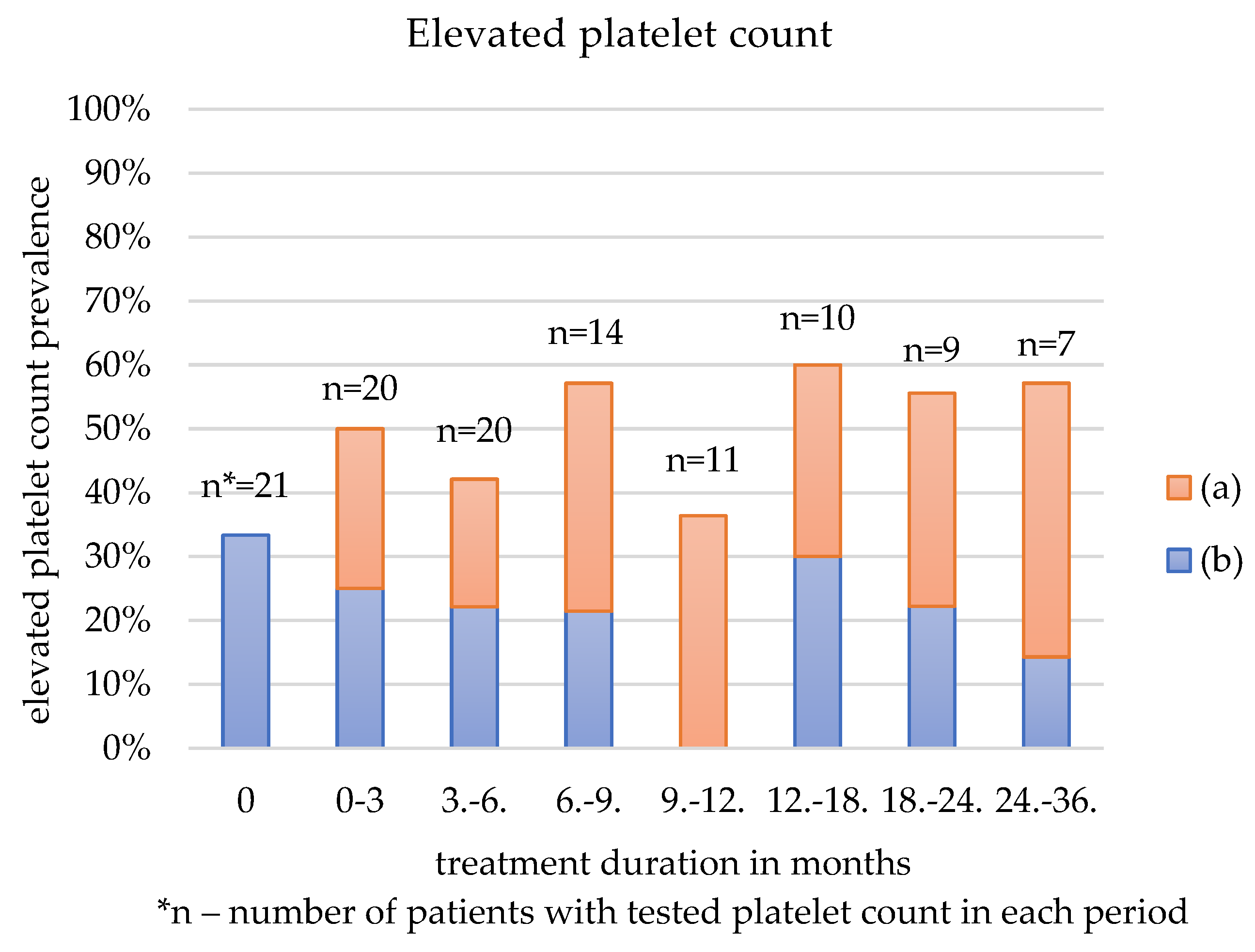
4.3. Thrombocytosis
4.4. Infections
4.5. Discontinuation
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Curatolo, P.; Bombardieri, R.; Jozwiak, S. Tuberous Sclerosis. Lancet 2008, 372, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Holmes, G.L.; Stafstrom, C.E.; Baraban, S.C.; Bertram, E.; Bolton, P.; Brooks-Kayal, A.; Chugani, H.T.; Coulter, D.; Crino, P.; Delanerolle, N.C.; et al. Tuberous Sclerosis Complex and Epilepsy: Recent Developments and Future Challenges. Epilepsia 2007, 48, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Manning, B.D. The TSC1-TSC2 Complex: A Molecular Switchboard Controlling Cell Growth. Biochem. J. 2008, 412, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Franz, D.N. Everolimus: An MTOR Inhibitor for the Treatment of Tuberous Sclerosis. Expert. Rev. Anticancer Ther. 2011, 11, 1181–1192. [Google Scholar] [CrossRef] [PubMed]
- Chu-Shore, C.J.; Major, P.; Montenegro, M.; Thiele, E. Cyst-like Tubers Are Associated with TSC2 and Epilepsy in Tuberous Sclerosis Complex. Neurology 2009, 72, 1165–1169. [Google Scholar] [CrossRef] [PubMed]
- Miszewska, D.; Sugalska, M.; Jóźwiak, S. Risk Factors Associated with Refractory Epilepsy in Patients with Tuberous Sclerosis Complex: A Systematic Review. J. Clin. Med. 2021, 10, 5495. [Google Scholar] [CrossRef]
- Jozwiak, S.; Słowińska, M.; Borkowska, J.; Sadowski, K.; Łojszczyk, B.; Domańska-Pakieła, D.; Chmielewski, D.; Kaczorowska-Frontczak, M.; Głowacka, J.; Sijko, K.; et al. Preventive Antiepileptic Treatment in Tuberous Sclerosis Complex: A Long-Term, Prospective Trial. Pediatr. Neurol. 2019, 101, 18–25. [Google Scholar] [CrossRef]
- Northrup, H.; Aronow, M.E.; Bebin, E.M.; Bissler, J.; Darling, T.N.; de Vries, P.J.; Frost, M.D.; Fuchs, Z.; Gosnell, E.S.; Gupta, N.; et al. Updated International Tuberous Sclerosis Complex Diagnostic Criteria and Surveillance and Management Recommendations. Pediatr. Neurol. 2021, 123, 50–66. [Google Scholar] [CrossRef]
- Sugalska, M.; Tomik, A.; Jóźwiak, S.; Werner, B. Treatment of Cardiac Rhabdomyomas with Mtor Inhibitors in Children with Tuberous Sclerosis Complex—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4907. [Google Scholar] [CrossRef]
- Saffari, A.; Brösse, I.; Wiemer-Kruel, A.; Wilken, B.; Kreuzaler, P.; Hahn, A.; Bernhard, M.K.; van Tilburg, C.M.; Hoffmann, G.F.; Gorenflo, M.; et al. Safety and Efficacy of MTOR Inhibitor Treatment in Patients with Tuberous Sclerosis Complex under 2 Years of Age—A Multicenter Retrospective Study. Orphanet J. Rare Dis. 2019, 14, 96. [Google Scholar] [CrossRef]
- Tomoto, K.; Fujimoto, A.; Inenaga, C.; Okanishi, T.; Imai, S.; Ogai, M.; Fukunaga, A.; Nakamura, H.; Sato, K.; Obana, A.; et al. Experience Using MTOR Inhibitors for Subependymal Giant Cell Astrocytoma in Tuberous Sclerosis Complex at a Single Facility. BMC Neurol. 2021, 21, 139. [Google Scholar] [CrossRef] [PubMed]
- Sagiv, E.; Chikkabyrappa, S.; Conwell, J.; Lewin, M.; Chun, T. Use of Everolimus to Treat Cardiac Rhabdomyomas and Incessant Arrhythmias in a Newborn: Benefits and Complications. Ann. Pediatr. Cardiol. 2022, 15, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Hinton, R.B.; Prakash, A.; Romp, R.L.; Krueger, D.A.; Knilans, T.K. Cardiovascular Manifestations of Tuberous Sclerosis Complex and Summary of the Revised Diagnostic Criteria and Surveillance and Management Recommendations from the International Tuberous Sclerosis Consensus Group. J. Am. Heart Assoc. 2014, 3, e001493. [Google Scholar] [CrossRef] [PubMed]
- Sato, A. MTOR, a Potential Target to Treat Autism Spectrum Disorder. CNS Neurol. Disord.-Drug Targets 2016, 15, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Qin, Y.; Wu, Q.; Li, X.; Xie, D.; Zhao, Z.; Duan, S. MTOR Signaling Pathway Regulates the Release of Proinflammatory Molecule CCL5 Implicated in the Pathogenesis of Autism Spectrum Disorder. Front. Immunol. 2022, 13, 818518. [Google Scholar] [CrossRef]
- Jóźwiak, S.; Kotulska, K.; Berkowitz, N.; Brechenmacher, T.; Franz, D.N. Safety of Everolimus in Patients Younger than 3 Years of Age: Results from EXIST-1, a Randomized, Controlled Clinical Trial. J. Pediatr. 2016, 172, 151–155.e1. [Google Scholar] [CrossRef]
- Krueger, D.A.; Care, M.M.; Holland, K.; Agricola, K.; Tudor, C.; Mangeshkar, P.; Wilson, K.A.; Byars, A.; Sahmoud, T.; Neal Franz, D.; et al. Everolimus for Subependymal Giant-Cell Astrocytomas in Tuberous Sclerosis From the Departments of Pediatrics and Neurology. N. Engl. J. Med. 2010, 363, 1801–1811. [Google Scholar] [CrossRef]
- Hatano, T.; Endo, K.; Tamari, M. Efficacy and Safety of Low-Dose Everolimus Treatment for Renal Angiomyolipoma Associated with Tuberous Sclerosis Complex. Int. J. Clin. Oncol. 2021, 26, 163–168. [Google Scholar] [CrossRef]
- Dame, C. Thrombocytosis. In Pediatric Hematology, 3rd ed.; Arceci, R.J., Hann, I.M., Smith, O.P., Eds.; Wiley: Hoboken, NJ, USA, 2006; pp. 548–561. [Google Scholar] [CrossRef]
- Cancer Institute, N. Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) v5.0; U.S. Department of Health and Human Services: Washington, DC, USA, 2017.
- Wiemer-Kruel, A.; Nabbout, R.; Fan, P.-C.; Ruiz Falco, M.L.; Polster, T.; Curatolo, P.; Fan, J.; Herbst, F.; Ridolfi, A.; French, J. Outcomes among Adult Patients with Tuberous Sclerosis Complex (TSC)-Associated Treatment-Refractory Seizures Treated with Adjunctive Everolimus: Final Analysis of the Exist-3 Study. Epilepsia 2018, 59, S5. [Google Scholar] [CrossRef]
- Hertzberg, C.; Belousova, E.; Fan, P.; DeWaele, L.; Bjoernvold, M.; Nabbout, R.; de Vries, P.; Fan, J.; Jin, L.; Herbst, F.; et al. Long-Term Efficacy and Safety of Everolimus among Pediatric Patients with Tuberous Sclerosis Complex (TSC) and Treatment-Refractory Seizures: Final Analysis of the Exist-3 Study. Ann. Neurol. 2018, 84, S345. [Google Scholar] [CrossRef]
- Bissler, J.J.; Mccormack, F.X.; Young, L.R.; Elwing, J.M.; Chuck, G.; Leonard, J.M.; Schmithorst, V.J.; Laor, T.; Brody, A.S.; Bean, J.; et al. Sirolimus for Angiomyolipoma in Tuberous Sclerosis Complex or Lymphangioleiomyomatosis. N. Engl. J. Med. 2008, 358, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.M.; de Vries, P.J.; Johnson, S.R.; McCartney, D.L.; Cox, J.A.; Serra, A.L.; Watson, P.C.; Howe, C.J.; Doyle, T.; Pointon, K.; et al. Sirolimus Therapy for Angiomyolipoma in Tuberous Sclerosis and Sporadic Lymphangioleiomyomatosis: A Phase 2 Trial. Clin. Cancer Res. 2011, 17, 4071–4081. [Google Scholar] [CrossRef] [PubMed]
- Verhave, J.; Boucher, A.; Dandavino, R.; Collette, S.; Senécal, L.; Hebert, M.J.; Girardin, C.; Cardinal, H. The Incidence, Management, and Evolution of Rapamycin-Related Side Effects in Kidney Transplant Recipients. Clin. Transpl. 2014, 28, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Fidan, K.; Kandur, Y.; Sozen, H.; Gonul, I.I.; Dalgic, A.; Söylemezoǧlu, O. How Often Do We Face Side Effects of Sirolimus in Pediatric Renal Transplantation? Transpl. Proc. 2013, 45, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Maria, G.; Antonia, D.; Michael, A.; Kate, M.; Sian, E.; Sarah, F.E.; Mehul, D.; Pratik, S. Sirolimus: Efficacy and Complications in Children with Hyperinsulinemic Hypoglycemia: A 5-Year Follow-up Study. J. Endocr. Soc. 2019, 3, 699–713. [Google Scholar] [CrossRef]
- Krueger, D.A.; Capal, J.K.; Curatolo, P.; Devinsky, O.; Ess, K.; Tzadok, M.; Koenig, M.K.; Narayanan, V.; Ramos, F.; Jozwiak, S.; et al. Short-Term Safety of MTOR Inhibitors in Infants and Very Young Children with Tuberous Sclerosis Complex (TSC): Multicentre Clinical Experience. Eur. J. Paediatr. Neurol. 2018, 22, 1066–1073. [Google Scholar] [CrossRef]
- Freixo, C.; Ferreira, V.; Martins, J.; Almeida, R.; Caldeira, D.; Rosa, M.; Costa, J.; Ferreira, J. Efficacy and Safety of Sirolimus in the Treatment of Vascular Anomalies: A Systematic Review. J. Vasc. Surg. 2020, 71, 318–327. [Google Scholar] [CrossRef]
- Ogórek, B.; Hamieh, L.; Hulshof, H.M.; Lasseter, K.; Klonowska, K.; Kuijf, H.; Moavero, R.; Hertzberg, C.; Weschke, B.; Riney, K.; et al. TSC2 Pathogenic Variants Are Predictive of Severe Clinical Manifestations in TSC Infants: Results of the EPISTOP Study. Genet. Med. 2020, 22, 1489–1497. [Google Scholar] [CrossRef]
- Morrisett, J.D.; Abdel-Fattah, G.; Hoogeveen, R.; Mitchell, E.; Ballantyne, C.M.; Pownall, H.J.; Opekun, A.R.; Jaffe, J.S.; Oppermann, S.; Kahan, B.D. Effects of Sirolimus on Plasma Lipids, Lipoprotein Levels, and Fatty Acid Metabolism in Renal Transplant Patients. J. Lipid Res. 2002, 43, 1170–1180. [Google Scholar] [CrossRef]
- Burén, J.; Ericsson, M.; Damasceno, N.R.T.; Sjödin, A. A Ketogenic Low-carbohydrate High-fat Diet Increases Ldl Cholesterol in Healthy, Young, Normal-weight Women: A Randomized Controlled Feeding Trial. Nutrients 2021, 13, 814. [Google Scholar] [CrossRef]
- Fang, Y.; Li, D.; Wang, M.; Zhao, X.; Duan, J.; Gu, Q.; Li, B.; Zha, J.; Mei, D.; Bian, G.; et al. Ketogenic Diet Therapy for Drug-Resistant Epilepsy and Cognitive Impairment in Children With Tuberous Sclerosis Complex. Front. Neurol. 2022, 13, 863826. [Google Scholar] [CrossRef] [PubMed]
- Sofroniadou, S.; Kassimatis, T.; Goldsmith, D. Anaemia, Microcytosis and Sirolimus-Is Iron the Missing Link? Nephrol. Dial. Transplant. 2010, 25, 1667–1675. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Widness, J.A. Pathophysiology of Anemia during the Neonatal Period, Including Anemia of Prematurity. Neoreviews 2008, 9, e520–e525. [Google Scholar] [CrossRef]
- Hartford, C.M.; Ratain, M.J. Rapamycin: Something Old, Something New, Sometimes Borrowed and Now Renewed. Clin. Pharmacol. Ther. 2007, 82, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Bevacqua, M.; Baldo, F.; Pastore, S.; Valencic, E.; Tommasini, A.; Maestro, A.; Rabusin, M.; Arbo, A.; Barbi, E. Off-Label Use of Sirolimus and Everolimus in a Pediatric Center: A Case Series and Review of the Literature. Pediatr. Drugs 2019, 21, 185–193. [Google Scholar] [CrossRef]
- Nguyen, L.S.; Vautier, M.; Allenbach, Y.; Zahr, N.; Benveniste, O.; Funck-Brentano, C.; Salem, J.E. Sirolimus and MTOR Inhibitors: A Review of Side Effects and Specific Management in Solid Organ Transplantation. Drug Saf. 2019, 42, 813–825. [Google Scholar] [CrossRef]
- Busca, A.; Locatelli, F.; Moscato, D.; Falda, M. Sirolimus-Related Toxicity in Stem Cell Transplantation. Biol. Blood Marrow Transplant. 2005, 11, 647–649. [Google Scholar] [CrossRef][Green Version]
- Xie, W.; Ji, L.; Zhang, Z. Sirolimus Monotherapy for Thrombocytopenia in Primary Antiphospholipid Syndrome: A Pilot Study From a Tertiary Referral Center. Front. Immunol. 2022, 13, 857424. [Google Scholar] [CrossRef]
- Fisher, A.; Seguel, J.M.; de la Torre, A.N.; Wilson, D.; Merchant, A.; Arora, R.K.; Koneru, B. Effect of Sirolimus on Infection Incidence in Liver Transplant Recipients. Liver Transplant. 2004, 10, 193–198. [Google Scholar] [CrossRef]
- Li, M.; Zhou, Y.; Chen, C.; Yang, T.; Zhou, S.; Chen, S.; Wu, Y.; Cui, Y. Efficacy and Safety of MTOR Inhibitors (Rapamycin and Its Analogues) for Tuberous Sclerosis Complex: A Meta-Analysis. Orphanet J. Rare Dis. 2019, 14, 39. [Google Scholar] [CrossRef]
- Rugo, H.S.; Pritchard, K.I.; Gnant, M.; Noguchi, S.; Piccart, M.; Hortobagyi, G.; Baselga, J.; Perez, A.; Geberth, M.; Csoszi, T.; et al. Incidence and Time Course of Everolimus-Related Adverse Events in Postmenopausal Women with Hormone Receptor-Positive Advanced Breast Cancer: Insights from BOLERO-2. Ann. Oncol. 2014, 25, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Rafii, S.; Roda, D.; Geuna, E.; Jimenez, B.; Rihawi, K.; Capelan, M.; Yap, T.A.; Molife, L.R.; Kaye, S.B.; de Bono, J.S.; et al. Higher Risk of Infections with PI3K-AKT-MTOR Pathway Inhibitors in Patients with Advanced Solid Tumors on Phase I Clinical Trials. Clin. Cancer Res. 2015, 21, 1869–1876. [Google Scholar] [CrossRef] [PubMed]
- French, J.A.; Lawson, J.A.; Yapici, Z.; Ikeda, H.; Polster, T.; Nabbout, R.; Curatolo, P.; de Vries, P.J.; Dlugos, D.J.; Berkowitz, N.; et al. Adjunctive Everolimus Therapy for Treatment-Resistant Focal-Onset Seizures Associated with Tuberous Sclerosis (EXIST-3): A Phase 3, Randomised, Double-Blind, Placebo-Controlled Study. Lancet 2016, 388, 2153–2163. [Google Scholar] [CrossRef] [PubMed]
- Krueger, D.A.; Care, M.M.; Agricola, K.; Tudor, C.; Mays, M.; David, B.S.; Franz, N. Everolimus Long-Term Safety and Efficacy in Subependymal Giant Cell Astrocytoma. Neurology 2013, 80, 574–580. [Google Scholar] [CrossRef]

| Variable | Value (%) |
|---|---|
| N = 21 | |
| Sex | |
| Female | 13 (61.9) |
| Male | 8 (38.1) |
| TSC mutation | |
| TSC1 | 0 (0) |
| TSC2 | 15 (71.4) |
| PKD1 | 3 (14.3) |
| Not studied | 6 (28.6) |
| Reason for mTORi 1 treatment | |
| Cardiac rhabdomyomas | 5 (28.6) |
| SEGA | 12 (57.1) |
| Renal AML | 1 (4.8) |
| Retinal hamartomas | 1 (4.8) |
| Epilepsy | 7 (33.3) |
| Age at the initiation of mTORi treatment (days) | |
| Mean (SD) | 211.9 (233.2) |
| Median [Min, Max] | 104 [3, 656] |
| mTORi treatment follow-up duration (months) | |
| Mean (SD) | 16 (8.7) |
| Median [Min, Max] | 22 [3, 24] |
| Antiepileptic treatment | |
| Yes | 19 (90.5) |
| No | 2 (9.5) |
| Number of ASM 2 | |
| Mean (SD) | 2.0 (1.1) |
| Median [Min, Max] | 2.0 [0, 3.0] |
| Preventive antiepileptic treatment | |
| Yes | 7 (33.3) |
| No | 14 (66.7) |
| Adverse Effect|Age | 0–6 Months | 6–12 Months | 12–24 Months | 24–36 Months |
|---|---|---|---|---|
| N 1 (%) | N (%) | N (%) | N (%) | |
| Hyperlipidemia | 10/12 (83.33) | 11/13 (84.62) | 13/13 (100) | 5/8 (62.5) |
| Hypercholesterolemia | 8/12 (66.67) | 5/12 (41.67) | 8/13 (61.54) | 3/8 (37.5) |
| Elevated LDL | 5/11 (45.45) | 5/12 (41.67) | 7/13 (53.85) | 2/7 (28.57) |
| Hypertrigliceridemia | 7/12 (58.33) | 8/12 (66.67) | 10/13 (76.92) | 3/7 (42.86) |
| Anemia | 11/12 (91.67) | 8/14 (57.14) | 9/14 (64.29) | 5/10 (50) |
| Thrombocytosis | 7/12 (58.33) | 5/14 (35.71) | 11/14 (78.57) | 7/10 (70) |
| Neutropenia | 5/12 (41.67) | 3/14 (21.43) | 5/14 (35.71) | 1/10 (10) |
| Elevated D-dimers | 2/2 (100) | 0/1 (0) | 1/2 (50) | 0/0 (0) |
| Elevated bilirubin | 3/7 (42.86) | 0/4 (0) | 0/4 (0) | 1/6 (16.67) |
| Low ALT | 4/12 (33.33) | 4/13 (30.77) | 6/12 (50) | 4/7 (57.14) |
| Elevated AST | 2/12 (16.67) | 1/13 (7.69) | 4/12 (25) | 2/7 (28.57) |
| Elevated fibrinogen | 0/6 (0) | 1/2 (50) | 1/3 (33.33) | 0/1 (0) |
| Infections | 2/12 (16.67) | 3/13 (23.08) | 5/13 (38.46) | 5/10 (50) |
| Mouth ulcers | 2/11 (18.18) | 0/14 (0) | 0/13 (0) | 1/10 (10) |
| Anemia | Elevated Platelet Count | Hyperlipidemia | ||||
|---|---|---|---|---|---|---|
| Duration of the Treatment (Months) | All Patients | No History of Anemia Prior to Sirolimus | All Patients | No History of Elevated PLT 1 Prior to Sirolimus | All Patients | No History of Hyperlipidemia Prior to Sirolimus |
| N 2 (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| 0 | 10/21 (47.62) | 0/11 (0) | 7/21 (33.33) | 0/14 (0) | 7/18 (38.89) | 0/11 (0) |
| 0–3 | 14/20 (70) | 6/11 (54.55) | 10/20 (50) | 5/13 (38.46) | 11/18 (61.11) | 7/11 (63.64) |
| 3–6 | 7/19 (36.84) | 5/10 (50) | 8/20 (42.11) | 4/11 (36.36) | 7/16 (43.75) | 4/10 (40) |
| 6–9 | 8/14 (57.14) | 4/8 (50) | 8/14 (57.14) | 5/7 (71.43) | 7/12 (58.33) | 4/7 (57.14) |
| 9–12 | 6/10 (60) | 4/6 (66.67) | 4/11 (36.36) | 4/6 (66.67) | 5/9 (55.56) | 2/5 (40) |
| 12–18 | 7/10 (70) | 4/5 (80) | 6/10 (60) | 3/3 (100) | 7/11 (63.64) | 4/6 (66.67) |
| 18–24 | 4/9 (44.44) | 2/5 (40) | 5/9 (55.56) | 3/4 (75) | 6/8 (75) | 4/6 (66.67) |
| 24–36 | 5/8 (62.50) | 2/4 (50) | 4/7 (57.14) | 3/3 (100) | 4/7 (57.14) | 2/4 (50) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Śmiałek, D.; Jóźwiak, S.; Kotulska, K. Safety of Sirolimus in Patients with Tuberous Sclerosis Complex under Two Years of Age—A Bicenter Retrospective Study. J. Clin. Med. 2023, 12, 365. https://doi.org/10.3390/jcm12010365
Śmiałek D, Jóźwiak S, Kotulska K. Safety of Sirolimus in Patients with Tuberous Sclerosis Complex under Two Years of Age—A Bicenter Retrospective Study. Journal of Clinical Medicine. 2023; 12(1):365. https://doi.org/10.3390/jcm12010365
Chicago/Turabian StyleŚmiałek, Dominika, Sergiusz Jóźwiak, and Katarzyna Kotulska. 2023. "Safety of Sirolimus in Patients with Tuberous Sclerosis Complex under Two Years of Age—A Bicenter Retrospective Study" Journal of Clinical Medicine 12, no. 1: 365. https://doi.org/10.3390/jcm12010365
APA StyleŚmiałek, D., Jóźwiak, S., & Kotulska, K. (2023). Safety of Sirolimus in Patients with Tuberous Sclerosis Complex under Two Years of Age—A Bicenter Retrospective Study. Journal of Clinical Medicine, 12(1), 365. https://doi.org/10.3390/jcm12010365







