Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis
Abstract
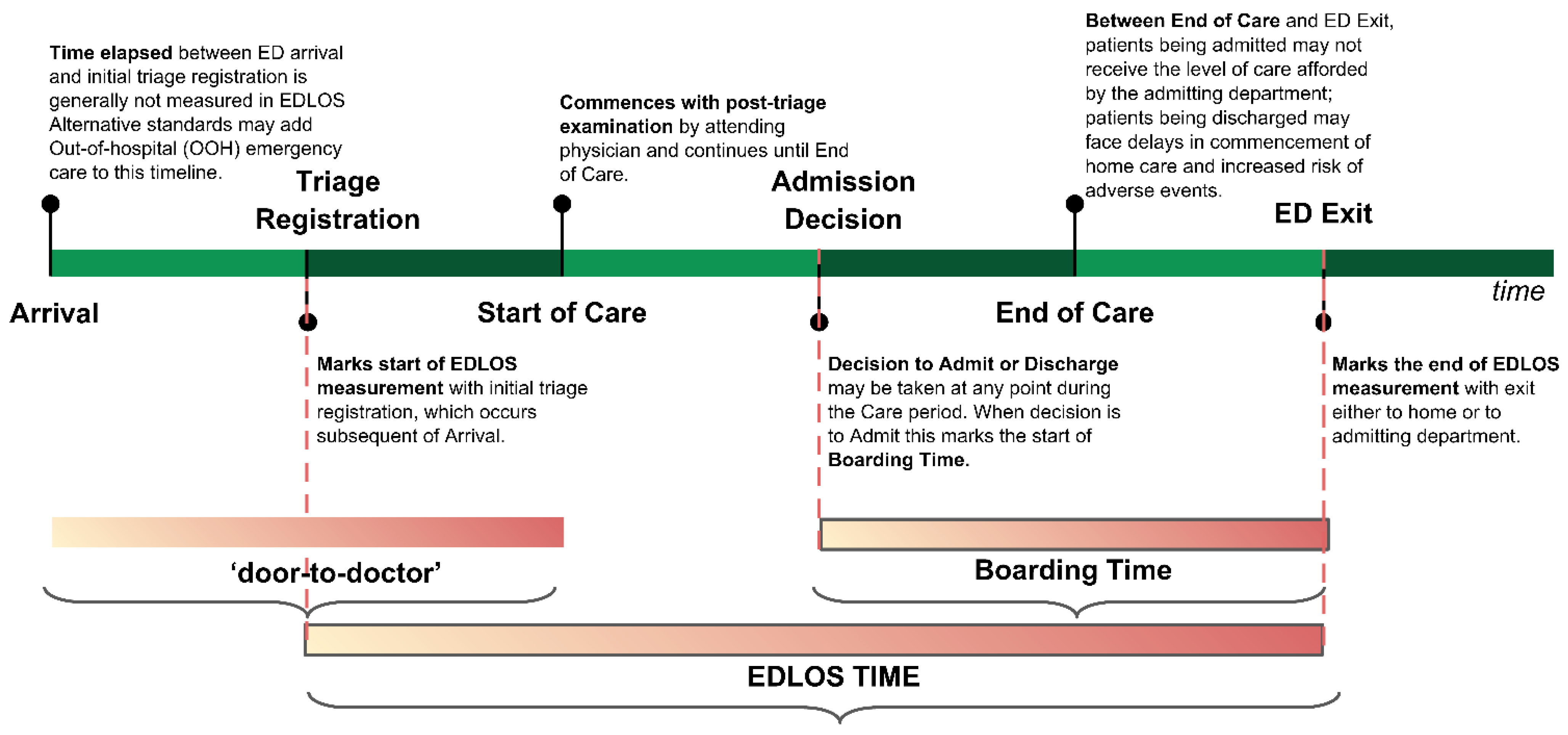
1. Introduction
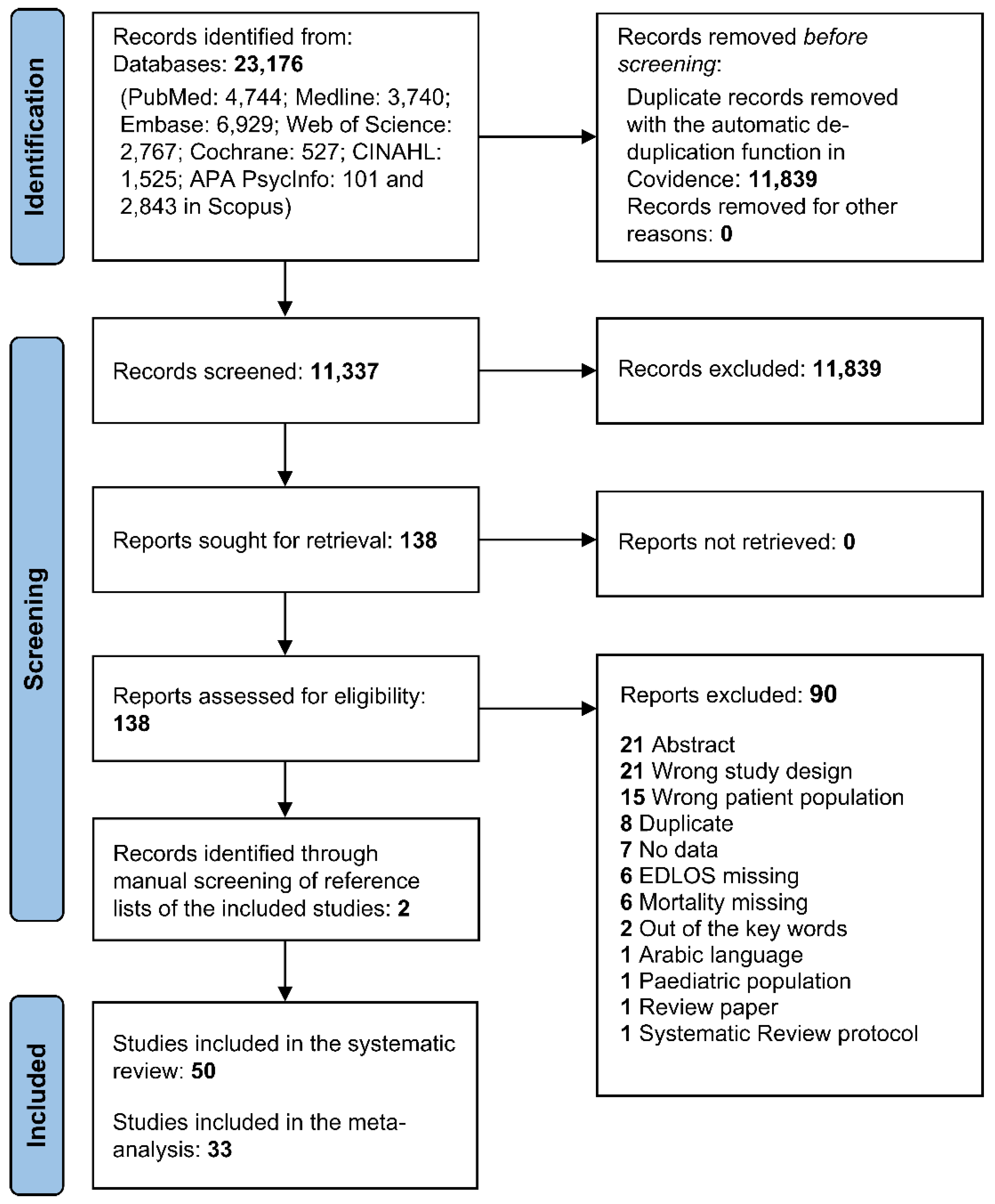
2. Materials and Methods
2.1. Data Sources and Searches
2.2. Inclusion Criteria and Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Analysis
3. Results
3.1. Systematic Review
3.1.1. Characteristics of the Selected Studies
3.1.2. Non-Intensive Care Unit-Admitted Population
3.1.3. Intensive Care Unit-Admitted Emergency Department Population
3.1.4. Quality of the Selected Studies
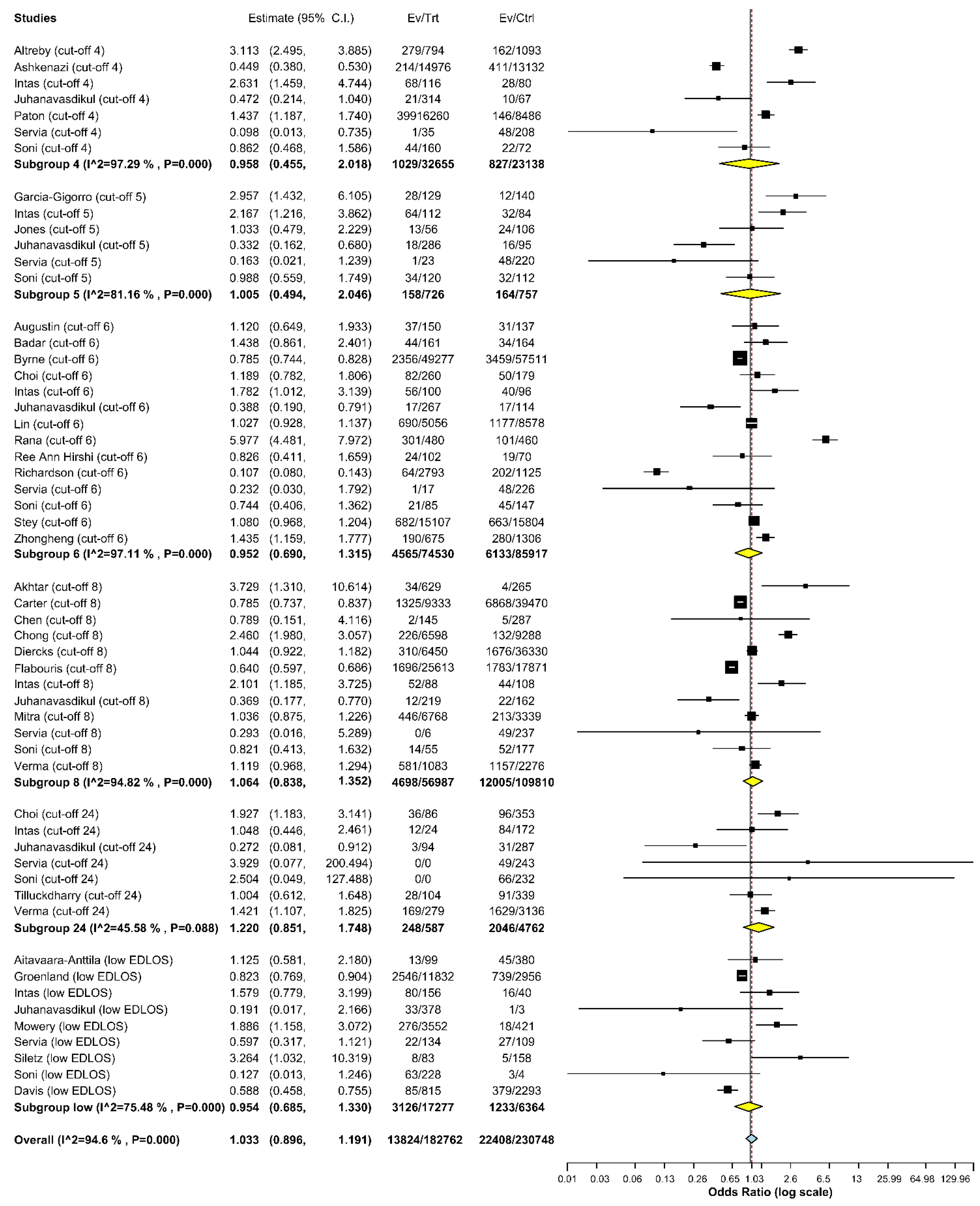
3.2. Meta-analysis
3.2.1. Random-Effects Models
3.2.2. Funnel Plots
3.2.3. Cross-validation (Leave-one-out)
3.2.4. Inverse Variance Heterogeneity Model
3.2.5. Subgroup Meta-Analyses and Univariate Meta-Regression Analysis
4. Discussion
4.1. Study Strengths
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIS | Abbreviated Injury Score |
| ACS | American College of Surgeons |
| APACH | Acute Physiology and Chronic Health Evaluation |
| BT | Boarding time |
| CRRT | Continuous renal replacement therapy |
| CI | Confidence interval |
| ED | Emergency department |
| EDLOS | Emergency department length of stay |
| GCS | Glasgow Coma Scale |
| ICD | International Classification of Diseases |
| ICU | Intensive care unit |
| IHM | In-hospital mortality |
| ISS | Injury Severity Score |
| KTAS | Korean Triage and Acuity Scale |
| LOS | Length of stay |
| MAP | Mean arterial blood pressure |
| MV | Mechanical ventilation |
| MA | Meta-analysis |
| MEWS | Modified Early Warning Score |
| NOS | Newcastle–Ottawa Quality Assessment Scale |
| NEWS | National Early Warning Score |
| NIH-SS | NIH Stroke Scale |
| OR | Odds ratio |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RTS | Revised Trauma Score |
| SAPS | Simplified Acute Physiology Score |
| SOFA | Sequential Organ Failure Assessment |
| TRISS | Therapeutic Intervention Scoring System |
| TISSS | Therapeutic Intervention Scoring System Score |
References
- Mohr, N.M.; Wessman, B.T.; Bassin, B.; Elie-Turenne, M.C.; Ellender, T.; Emlet, L.L.; Ginsberg, Z.; Gunnerson, K.; Jones, K.M.; Kram, B.; et al. Boarding of critically III patients in the emergency department. J. Am. Coll. Emerg. Physicians Open 2020, 1, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Australasian College for Emergency Medicine: Policy on Standard Terminology (Revised 2014). Available online: https://acem.org.au (accessed on 19 June 2017).
- Rose, L.; Scales, D.C.; Atzema, C.; Burns, K.E.; Gray, S.; Doing, C.; Kiss, A.; Rubenfeld, G.; Lee, J.S. Emergency department length of stay for critical care admissions. A population-based study. Ann. Am. Thorac. Soc. 2016, 13, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Canadian Association of Emergency Physicians, CAEP. Position Statement on Emergency Department Overcrowding. 2009. Available online: http://caep.ca/sites/caep.ca/files/caep/files/edoc_position_statement_board_approved_june_2009_gl.pdf (accessed on 1 January 2020).
- Horwitz, L.I.; Green, J.; Bradley, E.H. US Emergency Department performance on wait time and length of visit. Ann. Emerg. Med. 2010, 55, 133–141.e5. [Google Scholar] [CrossRef] [PubMed]
- Forero, R.; Man, N.; Ngo, H.; Mountain, D.; Mohsin, M.; Fatovich, D.; Toloo, G.; Celenza, A.; FitzGerald, G.; McCarthy, S.; et al. Impact of the four-hour National Emergency Access Target on 30-day mortality, access block and chronic emergency department overcrowding in Australian emergency departments. Emerg. Med. Australas. 2019, 31, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Sri-On, J.; Chang, Y.; Curley, D.P.; Camargo, C.A., Jr.; Weissman, J.S.; Singer, S.J.; Liu, S.W. Boarding is associated with higher rates of medication delays and adverse events but fewer laboratory-related delays. Am. J. Emerg. Med. 2014, 32, 1033–1036. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.J.; Thode, H.C., Jr.; Viccellio, P.; Pines, J.M. The association between length of emergency department boarding and mortality. Acad. Emerg. Med. 2011, 18, 1324–1329. [Google Scholar] [CrossRef]
- Derose, S.F.; Gabayan, G.Z.; Chiu, V.Y.; Yiu, S.C.; Sun, B.C. Emergency department crowding predicts admission length-of-stay but not mortality in a large health system. Med. Care 2014, 52, 602–611. [Google Scholar] [CrossRef]
- Liu, S.; Milne, L.; Yun, B.; Walsh, K. The boarding experience from the patient perspective: The wait. Emerg. Med. J. 2015, 32, 854–859. [Google Scholar] [CrossRef]
- Gabayan, G.Z.; Derose, S.F.; Chiu, V.Y.; Yiu, S.C.; Sarkisian, C.A.; Jones, J.P.; Sun, B.C. Emergency department crowding and outcomes after emergency department discharge. Ann. Emerg. Med. 2015, 66, 483–492.e5. [Google Scholar] [CrossRef]
- Sprivulis, P.C.; Da Silva, J.A.; Jacobs, I.G.; Jelinek, G.A.; Frazer, A.R. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med. J. Aust. 2006, 184, 208–212. [Google Scholar] [CrossRef]
- Sun, B.C.; Hsia, R.Y.; Weiss, R.E.; Zingmond, D.; Liang, L.J.; Han, W.; McCreath, H.; Asch, S.M. Effect of emergency department crowding on outcomes of admitted patients. Ann. Emerg. Med. 2013, 61, 605–611.e6. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Hollander, J.E. Emergency department crowding is associated with poor care for patients with severe pain. Ann. Emerg. Med. 2008, 51, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Pollack, C.V., Jr.; Diercks, D.B.; Chang, A.M.; Shofer, F.S.; Hollander, J.E. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad. Emerg. Med. 2009, 16, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Arkun, A.; Briggs, W.M.; Patel, S.; Datillo, P.A.; Bove, J.; Birkhahn, R.H. Emergency department crowding: Factors influencing flow. West J. Emerg. Med. 2010, 11, 10–15. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20411067 (accessed on 1 January 2020). [PubMed]
- Warner, L.S.H.; Pines, J.M.; Chambers, J.G.; Schuur, J.D. The most crowded US hospital emergency departments did not adopt effective interventions to improve flow, 2007–2010. Health Aff. 2015, 34, 2151–2159. [Google Scholar] [CrossRef]
- Mason, S.; Mountain, G.; Turner, J.; Arain, M.; Weber, E.J. Innovations to reduce demand and crowding in emergency care; a review study. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 10–15. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomised Studies in Meta-Analyses [Internet]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 29 June 2016).
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 Updated Mar 2011; (Cited 1 October 2011). Available online: http://www.cochrane-handbook.org (accessed on 1 January 2020).
- Stuck, A.E.; Rubenstein, L.Z.; Wieland, D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ 1998, 316, 469, author reply 470-1. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Doi, S.A.; Barendregt, J.J.; Khan, S.; Thalib, L.; Williams, G.M. Advances in the meta-analysis of heterogeneous clinical trials I: The inverse variance heterogeneity model. Contemp. Clin. Trials 2015, 45, 130–138. [Google Scholar] [CrossRef]
- Carter, A.W.; Pilcher, D.; Bailey, M.; Cameron, P.; Duke, G.J.; Cooper, J. Is ED length of stay before ICU admission related to patient mortality? Emerg. Med. Australas. 2010, 22, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Mitra, B.; Cameron, P.A.; Archer, P.; Bailey, M.; Pielage, P.; Mele, G.; Smit, D.V.; Newnham, H. The association between time to disposition plan in the emergency department and in-hospital mortality of general medical patients. Intern. Med. J. 2012, 42, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.P.; Haywood, C.; Barker, A.; Lim, W.K. Is emergency department length of stay associated with inpatient mortality? Australas J. Ageing 2013, 32, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Flabouris, A.; Jeyadoss, J.; Field, J.; Soulsby, T. Association between emergency department length of stay and outcome of patients admitted either to a ward, intensive care or high dependency unit. Emerg. Med. Australas. 2013, 25, 46–54. [Google Scholar] [CrossRef]
- Akhtar, N.; Kamran, S.; Singh, R.; Cameron, P.; Bourke, P.; Khan, R.; Joseph, S.; Santos, M.; Deleu, D.; Own, A. Prolonged stay of stroke patients in the emergency department may lead to an increased risk of complications, poor recovery, and increased mortality. J. Stroke Cerebrovasc. Dis. 2016, 25, 672–678. [Google Scholar] [CrossRef]
- Diercks, D.B.; Roe, M.T.; Chen, A.Y.; Peacock, W.F.; Kirk, J.D.; Pollack, C.V., Jr.; Gibler, W.B.; Smith, S.C., Jr.; Ohman, M.; Peterson, E.D. Prolonged emergency department stays of non–ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann. Emerg. Med. 2007, 50, 489–496. [Google Scholar] [CrossRef]
- Chen, H.C.; Lee, W.C.; Chen, Y.L.; Fang, H.Y.; Chen, C.J.; Yang, C.H.; Hang, C.L.; Fang, C.Y.; Yip, H.K.; Wu, C.J. The impacts of prolonged emergency department length of stay on clinical outcomes of patients with ST-segment elevation myocardial infarction after reperfusion. Intern. Emerg. Med. 2016, 11, 107–114. [Google Scholar] [CrossRef]
- Jones, E.M.; Boehme, A.K.; Aysenne, A.; Chang, T.; Albright, K.C.; Burns, C.; Beasley, T.M.; Martin-Schild, S. Prolonged emergency department length of stay as a predictor of adverse outcomes in patients with intracranial hemorrhage. J. Crit. Care Med. 2015, 2015, 526319. [Google Scholar] [CrossRef]
- Mowery, N.T.; Dougherty, S.D.; Hildreth, A.N.; Holmes, J.H.; Chang, M.C.; Martin, R.S.; Hoth, J.J.; Meredith, J.W.; Miller, P.R. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J. Trauma 2011, 70, 1317–1325. [Google Scholar] [CrossRef]
- Serviá, L.; Badia, M.; Baeza, I.; Montserrat, N.; Justes, M.; Cabré, X.; Valdrés, P.; Trujillano, J. Time spent in the emergency department and mortality rates in severely injured patients admitted to the intensive care unit: An observational study. J. Crit. Care 2012, 27, 58–65. [Google Scholar] [CrossRef]
- Tilluckdharry, L.; Tickoo, S.; Amoateng-Adjepong, Y.; Manthous, C.A. Outcomes of critically ill patients. Am. J. Emerg. Med. 2005, 23, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Weant, K.A.; Hirschy, R.; Sterk, E.; Dobersztyn, R.; Rech, M.A. Time spent in the emergency department and outcomes in patients with severe sepsis and septic shock. Adv. Emerg. Nurs. J. 2018, 40, 94–103. [Google Scholar] [CrossRef]
- Plunkett, P.K.; Byrne, D.G.; Breslin, T.; Bennett, K.; Silke, B. Increasing wait times predict increasing mortality for emergency medical admissions. Eur. J. Emerg. Med. 2011, 18, 192–196. [Google Scholar] [CrossRef] [PubMed]
- García-Gigorro, R.; de la Cruz Vigo, F.; Andrés-Esteban, E.M.; Chacón-Alves, S.; Varas, G.M.; Sánchez-Izquierdo, J.A.; González, J.M. Impact on patient outcome of emergency department length of stay prior to ICU admission. Med. Intensiva 2017, 41, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Agustin, M.; Price, L.L.; Andoh-Duku, A.; LaCamera, P. Impact of delayed admission to the intensive care unit from the emergency department upon sepsis outcomes and sepsis protocol compliance. Crit. Care Res. Pract. 2017, 2017, 9616545. [Google Scholar] [CrossRef]
- Siletz, A.; Jin, K.; Cohen, M.; Lewis, C.; Tillou, A.; Cryer, H.M.; Cheaito, A. Emergency department length of stay in critical nonoperative trauma. J. Surg. Res. 2017, 214, 102–108. [Google Scholar] [CrossRef]
- Junhasavasdikul, D.; Theerawit, P.; Kiatboonsri, S. Association between admission delay and adverse outcome of emergency medical patients. Emerg. Med. J. 2013, 30, 320–323. [Google Scholar] [CrossRef]
- Soni, K.D.; Kaushik, G.; Gupta, A.; Singh, V.; Kumar, S.; Sagar, S. From emergency department to intensive care unit, does the delay matter to trauma patients? J. Emerg. Trauma Shock 2018, 11, 189–192. [Google Scholar] [CrossRef]
- Paton, A.; Mitra, B.; Considine, J. Longer time to transfer from the emergency department after bed request is associated with worse outcomes. Emerg. Med. Australas. 2019, 31, 211–215. [Google Scholar] [CrossRef]
- Zhang, Z.; Bokhari, F.; Guo, Y.; Goyal, H. Prolonged length of stay in the emergency department and increased risk of hospital mortality in patients with sepsis requiring ICU admission. Emerg. Med. J. 2019, 36, 82–87. [Google Scholar] [CrossRef]
- Intas, G.; Stergiannis, P.; Chalari, E.; Tsoumakas, K.; Fildissis, G. The impact of ED boarding time, severity of illness, and discharge destination on outcomes of critically ill ED patients. Adv. Emerg. Nurs. J. 2012, 34, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.D.; Franklin, G.; Santos, A.; Harbrecht, B.; Danzl, D.; Coleman, R.; Smith, J.; Miller, F.; McMasters, K. Effective triage can ameliorate the deleterious effects of delayed transfer of trauma patients from the emergency department to the ICU. J. Am. Coll. Surg. 2009, 208, 671–678, discussion 678. [Google Scholar] [CrossRef] [PubMed]
- Aitavaara-Anttila, M.; Liisanantti, J.H.; Raatiniemi, L.; Ohtonen, P.; Ala-Kokko, T. Factors related to delayed intensive care unit admission from emergency department-A retrospective cohort study. Acta Anaesthesiol. Scand. 2019, 63, 939–946. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Shakeel, N.; Siddiqui, E.U.; Kazi, G.; Khan, I.Q.; Khursheed, M.; Feroze, A.; Ejaz, K.; Khan, S.T.; Adel, H. Impact of delay in admission on the outcome of critically ill patients presenting to the emergency department of a tertiary care hospital from low income country. J. Pak. Med. Assoc. 2016, 66, 509–516. [Google Scholar] [PubMed]
- Byrne, D.; Browne, J.G.; Conway, R.; Cournane, S.; O’Riordan, D.; Silke, B. Mortality outcomes and emergency department wait times—The paradox in the capacity limited system. Acute Med. 2018, 17, 130–136. [Google Scholar] [CrossRef]
- Groenland, C.N.; Termorshuizen, F.; Rietdijk, W.J.; van den Brule, J.; Dongelmans, D.A.; de Jonge, E.; de Lange, D.W.; de Smet, A.M.G.; de Keizer, N.F.; Weigel, J.D.; et al. Emergency department to ICU time is associated with hospital mortality: A registry analysis of 14,788 patients from six university hospitals in the Netherlands. Crit. Care Med. 2019, 47, 1564–1571. [Google Scholar] [CrossRef]
- Haji, K.; Haji, D.; Tiruvoipati, R.; Bailey, M.; Le Blanc, V.; Botha, J.A. Impact of length of stay in emergency department on the outcome in patients with severe sepsis. Crit. Care Shock 2010, 13, 132–137. [Google Scholar]
- Santos, F.R.Q.; Machado, M.N.; Lobo, S.M.A. Adverse outcomes of delayed intensive care unit. Rev. Bras. Ter. Intensiv. 2020, 32, 92–98. [Google Scholar] [CrossRef]
- Mejaddam, A.Y.; Elmer, J.; Sideris, A.C.; Chang, Y.; Petrovick, L.; Alam, H.B.; Fagenholz, P.J. Prolonged emergency department length of stay is not associated with worse outcomes in traumatic brain injury. J. Emerg. Med. 2013, 45, 384–391. [Google Scholar] [CrossRef]
- Saukkonen, K.A.; Varpula, M.; Räsänen, P.; Roine, R.P.; Voipio-Pulkki, L.M.; Pettilä, V. The effect of emergency department delay on outcome in critically ill medical patients: Evaluation using hospital mortality and quality of life at 6 months. J. Intern. Med. 2006, 260, 586–591. [Google Scholar] [CrossRef]
- Hung, S.C.; Kung, C.T.; Hung, C.W.; Liu, B.M.; Liu, J.W.; Chew, G.; Chuang, H.Y.; Lee, W.H.; Lee, T.C. Determining delayed admission to the intensive care unit for mechanically ventilated patients in the emergency department. Crit. Care 2014, 18, 485. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, L.T.; Grion, C.; Matsuo, T.; Anami, E.H.; Kauss, I.A.; Seko, L.; Bonametti, A.M. Impact of delayed admission to intensive care units on mortality of critically ill patients: A cohort study. Crit. Care 2011, 15, R28. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, I.; Gefen, L.; Hochman, O.; Tannous, E. The 4-h target in the emergency department, in-hospital mortality, and length of hospitalization: A single center-retrospective study. Am. J. Emerg. Med. 2021, 47, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Stey, A.M.; Kanzaria, H.K.; Dudley, R.A.; Bilimoria, K.Y.; Knudson, M.M.; Callcut, R.A. Emergency department length of stay and mortality in critically injured patients. J. Intensive Care Med. 2022, 37, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.; Woo, S.H.; Kim, D.H.; Lee, J.Y.; Lee, W.J.; Jeong, S.; Cha, K.; Youn, C.S.; Park, S. Prolonged length of stay in the emergency department and mortality in critically ill elderly patients with infections: A retrospective multicenter study. Emerg. Med. Int. 2021, 2021, 9952324. [Google Scholar] [CrossRef]
- Lin, S.; Ge, S.; He, W.; Zeng, M. Association of delayed time in the emergency department with the clinical outcomes for critically ill patients. QJM 2021, 114, 311–317. [Google Scholar] [CrossRef]
- Aletreby, W.T.; Brindley, P.G.; Balshi, A.N.; Huwait, B.M.; Alharthy, A.M.; Madi, A.F.; Ramadan, O.E.; Noor, A.S.N.; Alzayer, W.S.; Alodat, M.A.; et al. Delayed intensive care unit admission from the emergency department: Impact on patient outcomes. a retrospective study. Rev. Bras. Ter. Intensiva 2021, 33, 125–137. [Google Scholar] [CrossRef]
- Wessman, T.; Ärnlöv, J.; Carlsson, A.C.; Ekelund, U.; Wändell, P.; Melander, O.; Ruge, T. The association between length of stay in the emergency department and short-term mortality. Intern. Emerg. Med. 2022, 17, 233–240. [Google Scholar] [CrossRef]
- Rana, M.A.; Bibi, T.; Qayyum, M.A.; Javed, M.; Zartash, S.; Lashari, A.A.; Hafeez, R.P.M.M. Association between time spent. In: Emergency Department and Outcome of Patients Admitted to Intensive Care Unit. PJMHS 2021, 15, 543–545. [Google Scholar]
- Thibon, E.; Bobbia, X.; Blanchard, B.; Masia, T.; Palmier, L.; Tendron, L.; de La Coussaye, J.E.; Claret, P.G. Association between mortality and waiting time in emergency room among adults. Ann. Fr. Med. Urgence 2019, 9, 229–234. [Google Scholar] [CrossRef]
- Asheim, A.; Nilsen, S.M.; Carlsen, F.; Næss-Pleym, L.E.; Uleberg, O.; Dale, J.; Bjørnsen, L.P.B.W.; Bjørngaard, J.H. The effect of emergency department delays on 30-day mortality in Central Norway. Eur. J. Emerg. Med. 2019, 26, 446–452. [Google Scholar] [CrossRef]
- Cheng, T.; Peng, Q.; Jin, Y.Q.; Yu, H.J.; Zhong, P.S.; Gu, W.M.; Wang, X.S.; Lu, Y.M.; Luo, L. Access block and prolonged length of stay in the emergency department are associated with a higher patient mortality rate. World J. Emerg. Med. 2022, 13, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Crilly, J.; Sweeny, A.; O’Dwyer, J.; Richards, B.; Green, D.; Marshall, A.P. Patients admitted via the emergency department to the intensive care unit: An observational cohort study. Emerg. Med. Australas. 2019, 31, 225–233. [Google Scholar] [CrossRef]
- Davis, N.W.; Sheehan, T.O.; Guo, Y.; Kelly, D.L.; Horgas, A.L.; Yoon, S.L. Factors associated with emergency department length of stay and in-hospital mortality in intracerebral hemorrhage patients. J. Neurosci. Nurs. 2021, 53, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Elay, G.; Behcet, A. Thirty-day mortality in septic shock patients is directly associated with high disease severity score but not with the length of stay in the emergency department. Eurasian J. Emerg. Med. 2020, 19, 172–177. [Google Scholar] [CrossRef]
- Sabaz, M.S.; Asar, S.; Cukurova, Z.; Sabaz, N.; Dog, H.; Sertcakacilar, G. Effect of delayed admission to intensive care units from the emergency department on the mortality of critically ill patients. Iran Red Crescent Med. J. 2020, 22, e102425. [Google Scholar] [CrossRef]
- Verma, A.; Shishodia, S.; Jaiswal, S.; Sheikh, W.R.; Haldar, M.; Vishen, A.; Ahuja, R.; Khatai, A.A.; Khanna, P. Increased length of stay of critically ill patients in the emergency department associated with higher in-hospital mortality. Indian J. Crit. Care Med. 2021, 25, 1221–1225. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Damania, D.; Jain, A.R.; Kanthala, A.R.; Ganti, L.; Jahromi, B.S. Does prolonged length of stay in the emergency department affect outcome for stroke patients? West J. Emerg. Med. 2014, 15, 267–275. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Boudi, Z.; Lauque, D.; Alsabri, M.; Östlundh, L.; Oneyji, C.; Khalemsky, A.; Lojo Rial, C.; Liu, S.W.; Camargo, C.A., Jr.; Aburawi, E. Association between boarding in the emergency department and in-hospital mortality: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0231253. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G. Analysing Data and Undertaking Meta-Analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P., Green, S., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2008; pp. 243–296. [Google Scholar]
- Mantel, N. Chi-square tests with one degree of freedom; extensions of the Mantel-Haenszel procedure. J. Am. Stat. Assoc. 1963, 58, 690–700. [Google Scholar] [CrossRef]
- Hedges, L.V.; Vevea, J.L. Estimating effect size under publication bias: Small sample properties and robustness of a random effects selection model. J. Educ. Behav. Stat. 1996, 21, 299–332. [Google Scholar] [CrossRef]
- Rathlev, N.K.; Chessare, J.; Olshaker, J.; Obendorfer, D.; Mehta, S.D.; Rothenhaus, T.; Crespo, S.; Magauran, B.; Davidson, K.; Shemin, R.; et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann. Emerg. Med. 2007, 49, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Miro, O.; Sanchez, M.; Espinosa, G.; Coll-Vinent, B.; Bragulat, E.; Milla, J. Analysis of patient flow in the emergency department and the effect of an extensive reorganisation. Emerg. Med. J. 2003, 20, 143–148, discussion 148. [Google Scholar] [CrossRef]
- Chalfin, D.B.; Trzeciak, S.; Likourezos, A.; Baumann, B.M.; Dellinger, R.P.; Delay-Ed Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit. Care Med. 2007, 35, 1477–1483. [Google Scholar] [CrossRef]
- Wang, H.; Robinson, R.D.; Bunch, K.; Huggins, C.A.; Watson, K.; Jayswal, R.D.; White, N.C.; Banks, B.; Zenarosa, N.R. The inaccuracy of determining overcrowding status by using the national ED overcrowding study tool. Am. J. Emerg. Med. 2014, 32, 1230–1236. [Google Scholar] [CrossRef]
- Di Somma, S.; Paladino, L.; Vaughan, L.; Lalle, I.; Magrini, L.; Magnanti, M. Overcrowding in emergency department: An international issue. Intern. Emerg. Med. 2015, 10, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Hilton, J.A.; Weber, E.J.; Alkemade, A.J.; Al Shabanah, H.; Anderson, P.D.; Bernhard, M.; Bertini, A.; Gries, A.; Ferrandiz, S.; et al. International perspectives on emergency department crowding. Acad. Emerg. Med. 2011, 18, 1358–1370. [Google Scholar] [CrossRef] [PubMed]
- Trzeciak, S.; Rivers, E.P. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg. Med. J. 2003, 20, 402–405. [Google Scholar] [CrossRef]
- Weaver, W.D. Time to thrombolytic treatment: Factors affecting delay and their influence on outcome. J. Am. Coll. Cardiol. 1995, 25, 3S–9S. [Google Scholar] [CrossRef]
- Cowley, R.A. Resuscitation and stabilization of major multiple trauma patients in a trauma center Environment. Clin. MedIterr. 1976, 83, 16–22. [Google Scholar]
- Rivers, E.; Nguyen, B.; Havstad, S.; Ressler, J.; Muzzin, A.; Knoblich, B.; Peterson, E.; Tomlanovich, M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 2001, 345, 1368–1377. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, J.O.; Teres, D.A.; Lemeshow, S.T.; Harris, D. Timing of intensive care unit admission in relation to ICU outcome. Crit. Care Med. 1990, 18, 1231–1235. [Google Scholar] [CrossRef] [PubMed]
- Duke, G.; Green, J.; Briedis, J. Survival of critically ill medical patients is time-critical. Crit. Care Resusc. 2004, 6, 261–267. [Google Scholar] [PubMed]
- Arise, Anzics Apd Management Committee. The outcome of patients with sepsis and septic shock presenting to emergency departments in Australia and New Zealand. Crit. Care Resusc. 2007, 9, 8–18. [Google Scholar]
- Richardson, D.B. The access-block effect: Relationship between delay to reaching an inpatient bed and inpatient length of stay. Med. J. Aust. 2002, 177, 492–495. [Google Scholar] [CrossRef]
- Richardson, D.B. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med. J. Aust. 2006, 184, 213–216. [Google Scholar] [CrossRef]
- Liu, Y.; Phillips, M.; Codde, J. Factors influencing patients’ length of stay. Aust. Health Rev. 2001, 24, 63–70. [Google Scholar] [CrossRef]
- Xu, C.; Liu, Y.; Jia, P.L.; Li, L.; Liu, T.Z.; Cheng, L.L.; Deng, K.; Borhan, A.S.M.; Thabane, L.; Sun, X. The methodological quality of dose-response meta-analyses needed substantial improvement: A cross-sectional survey and proposed recommendations. J. Clin. Epidemiol. 2019, 107, 1–11. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| N | Author | Year | Journal | Country and ED Setting | EDLOS Cut-Off |
|---|---|---|---|---|---|
| 1 | Carter AW [25] | 2010 | Emerg Med Australas | 45 Australian hospitals | Qualitative (8 h) |
| 2 | Mitra B [26] | 2012 | Intern Med J | 3 Australian hospitals | Qualitative (8 h) |
| 3 | Chong CP [27] | 2013 | Australas J Ageing | 1 Australian hospital | Qualitative (8 h) |
| 4 | Flabouris A [28] | 2013 | Emerg Med Australas | 1 Australian hospital | Qualitative (8 h) and continuous |
| 5 | Akhtar N [29] | 2016 | J Stroke Cerebrovasc Dis | 1 Qatari hospital | Qualitative (8 h) |
| 6 | Diercks DB [30] | 2007 | Ann Emerg Med | 550 U.S. hospitals | Qualitative (<4 h, 4–8 h, >8 h) |
| 7 | Chen HC [31] | 2016 | Intern Emerg Med | 1 Chinese hospital | Qualitative (8 h) |
| 8 | Jones EM [32] | 2015 | J Crit Care Med | 1 U.S. hospital | Qualitative (5 h) |
| 9 | Mowery NT [33] | 2011 | J Trauma | The U.S. healthcare system | Qualitative (2 h) and continuous |
| 10 | Serviá L [34] | 2012 | J Crit Care | 1 Spanish hospital | Qualitative (2 h) |
| 11 | Tilluckdharry L [35] | 2005 | Am J Emerg Med | 1 U.S. hospital | Qualitative (24 h) |
| 12 | Hirshi RA [36] | 2018 | Adv Emerg Nurs J | 1 U.S. hospital | Quantitative, continuous No specific EDLOS cut-off |
| 13 | Plunkett PK [37] | 2010 | Eur J Em Med | 1 U.K. hospital | Qualitative with multiple cut-offs: 2.6 h, 3.9 h, 5.8 h, and 8.7 h No specific EDLOS cut-off |
| 14 | García-Gigorro R [38] | 2016 | Med Intensiva | 1 Spanish hospital | Qualitative (6 h) |
| 15 | Agustin M [39] | 2017 | Crit Care Res Pract | 1 U.S. hospital | Qualitative (6 h) |
| 16 | Siletz A [40] | 2017 | J Surg Res | 1 U.S. hospital | 1.5 h |
| 17 | Junhasavasdikul D [41] | 2013 | Em Med J | 1 Thailand hospital | No specific EDLOS cut-off |
| 18 | Soni KD [42] | 2018 | J Emerg Trauma Shock | 1 Indian hospital | No specific EDLOS cut-off |
| 19 | Paton A [43] | 2018 | Emerg Med Australas | 3 Australian hospitals | 4 h |
| 20 | Zhang Z [44] | 2019 | Em Med J | 1 Chinese hospital | Qualitative (<6 h, 6–12 h, 12–24 h, >24 h) |
| 21 | Intas G [45] | 2012 | Adv Emerg Nurs J | 1 Greek hospital | Qualitative (6 h) |
| 22 | Richardson JD [46] | 2009 | J Am Coll Surg | 1 U.S. hospital | 6 h |
| 23 | Aitavaara-Anttila M [47] | 2019 | Acta Anaesthesiol Scand | 1 Finnish hospital | 3 h |
| 24 | Khan BA [48] | 2016 | J Pak Med Assoc | 1 Pakistani hospital | 6 h |
| 25 | Byrne D [49] | 2018 | Acute Med | 1 U.K. hospital | 6 h |
| 26 | Groenland CN [50] | 2019 | Crit Care Med | 6 university hospitals in The Netherlands | 1.2 h |
| 27 | Haji K [51] | 2010 | Crit Care Shock | 1 Australian hospital | Continuous No specific EDLOS cut-off |
| 28 | Santos FR [52] | 2020 | Rev Bras Ter Intensiva | 1 Brazilian hospital | Continuous No specific EDLOS cut-off |
| 29 | Mejaddam AY [53] | 2013 | J Emerg Med | 1 U.S. hospital | Continuous No specific EDLOS cut-off |
| 30 | Saukonnen KA [54] | 2006 | J Intern Med | 1 Finnish hospital | Continuous No specific EDLOS cut-off |
| 31 | Hung SC [55] | 2014 | Crit Care | 1 Chinese hospital | 4 h |
| 32 | Cardoso LT [56] | 2011 | Crit Care | 1 Brazilian hospital | Continuous No specific EDLOS cut-off |
| 33 | Ashkenazi [57] | 2021 | Am J Em Med | 28 Israeli hospitals | 4 h |
| 34 | Stey [58] | 2021 | J Int Care Med | 4 U.S. hospitals | 6 h |
| 35 | Choi [59] | 2021 | Emerg Med Intern | 5 Korean hospitals | 6 h 12 h 24 h |
| 36 | Lin [60] | 2021 | QJM: An International Journal of Medicine | 2 U.S. hospitals | 6 h |
| 37 | Altreby [61] | 2021 | Rev Bras Ter Intensiva. | 1 Saudi Arabian hospital | 4 h |
| 38 | Wessman [62] | 2021 | Internal and Emergency Medicine | 1 Swedish hospital | No cut-off |
| 39 | Rana [63] | 2021 | Pakistan Journal of Medical and Health Sciences | 1 Pakistani hospital | 6 h |
| 40 | Thibon [64] | 2019 | Ann. Fr. Med. Urgence | 1 French hospital | No cut-off |
| 41 | Asheim [65] | 2019 | European Journal of Emergency Medicine | 1 Norwegian hospital | No cut-off |
| 42 | Cheng [66] | 2022 | World J Emerg Med | 1 Chinese hospital | No specific cut-off |
| 43 | Crilly [67] | 2019 | Emergency Medicine Australasia | 1 Australian hospital | No specific cut-off |
| 44 | Davis [68] | 2021 | Journal of Neuroscience Nursing | U.S. hospitals | 3 h |
| 45 | Elay [69] | 2020 | Eurasian J Emerg Med. | 1 Turkish hospital | No specific cut-off |
| 46 | Rose [3] | 2016 | Annals ATS | Canadian hospitals | 6 h |
| 47 | Sabaz [70] | 2020 | Iran Red Crescent Med J. | 1 Iranian hospital | No specific cut-off |
| 48 | Verma [71] | 2021 | Indian Journal of Critical Care Medicine | 1 Indian hospital | 8 h and 24 h |
| 49 | Derose [9] | 2014 | Med Care | 14 U.S. hospitals | No specific cut-off |
| 50 | Jain [72] | 2013 | Western J Emerg Med | 1 U.S. hospital | No specific cut off |
| N | Author | Type of ED Population | Study Group (n) | Statistics | Factors Analyzed | Association with IHM |
|---|---|---|---|---|---|---|
| 1 | Carter [25] | ICU | 48,803 | Logistic regression Adjusted | Age, comorbidity, source of admission, year of admission, number of admissions to ICU from ED per day, type of hospital, diagnosis, MV, acute renal failure | No |
| 2 | Mitra [26] | Non-ICU | 10,107 | Logistic regression Adjusted | Age, sex, triage category, time to disposition plan | Yes |
| 3 | Chong [27] | Non-ICU | 15,886 | Logistic regression adjusted | Age, sex, comorbidities | No |
| 4 | Flabouris [28] | Non-ICU | 43,484 | Backwards stepwise regression | Age, EDLOS, sex, admission source, admitting unit, ED arrival time and day of week, ED departure time, Australasian triage scale | No |
| 5 | Akhtar [29] | Non-ICU | 894 | Logistic regression Adjusted | Sex, Health Technology Assessment, atrial fibrillation, smoking, thrombolysis complications, urinary tract infection, bedsores, Foley’s catheter | Yes |
| 6 | Diercks [30] | Non-ICU | 42,780 | Logistic regression Adjusted | Age, sex, Body Mass Index, race, insurance, cardiac risk factor, past cardiac history | No |
| 7 | Chen [31] | Non-ICU | 432 | No logistic regression | Age, sex, comorbidities, renal function, cardiac biomarkers, systolic and diastolic blood pressure, heart rate, time of primary PCI, door to balloon, advanced heart failure, Killip score, TIMI risk score, respiratory failure, anterior wall STEMI, any post myocardial complications, left ventricular ejection | No |
| 8 | Jones [32] | ICU | 162 | Logistic regression Adjusted | Age, sex, Baseline Intracerebral Hemorrhage Score (age, GCS, intracerebral hemorrhage volume and location, intraventricular hemorrhage) | Yes |
| 9 | Mowery [33] | Non-ICU | 3973 | Logistic regression Adjusted | Age, sex, ISS, revised trauma score | Yes |
| 10 | Serviá [34] | ICU | 243 | Logistic regression Adjusted | Age, sex, mechanical ventilation, head injury with AIS ≥ 3, TRISS ≥ 20 | No |
| 11 | Tilluckdharry [35] | ICU | 443 | No logistic regression Not adjusted | Age, sex, disease, APACHE II score | No |
| 12 | Hirshi [36] | ICU | 294 | Logistic regression | Arrival by emergency medical services, septic shock, liver disease, baseline lactate, Sequential Organ Failure Assessment, time to antibiotics and fluids, number of vasopressors | No |
| 13 | Plunkett [37] | Non-ICU | 23,114 | Logistic regression Adjusted | Sex, Acute Illness Severity Score, triage score category, major disease by category, Charlson’s comorbidity index, ICU admission, blood transfusion, troponin elevation, door-to-team, and team-to-ward time | Yes |
| 14 | García-Gigorro [38] | ICU | 269 | Logistic regression | Age, sex, comorbidities, diagnostic category, APACH score | Yes |
| 15 | Agustin [39] | ICU | 287 | Logistic regression | SOFA, MAP, and lactate | No |
| 16 | Siletz [40] | ICU | 241 | Logistic regression | Age, ISS, number of comorbidities | No |
| 17 | Junhasavasdikul [41] | Non-ICU | 381 | Logistic regression | Age, sex, primary diagnosis, lead-time, severity triage score, MEWS | No |
| 18 | Soni [42] | ICU | 232 | Logistic regression | Age, sex, SpO2, GCS, ICU stay days, heart rate, referring, status, ISS | No |
| 19 | Paton [43] | Non-ICU | 24,746 | Logistic regression | Sex, age, triage, category, ambulance transport, residing at home | Yes |
| 20 | Zhang [44] | ICU | 1997 | Logistic regression | PaO2/FiO2, serum creatinine, age, SOFA, Body Mass Index, lactate, comorbidities and infection site | Yes |
| 21 | Intas [45] | ICU | 200 | Logistic regression | Age, sex, diagnostic category (e.g., medical, surgical), APACH score, SAOS II, GCS at the time of intubation, admission time | Yes |
| 22 | Richardson [46] | Non-ICU | 3918 | Logistic regression | Age, mechanism of injury, race, sex, GCS, computed tomography findings of the head, abdomen, and chest, ISS, | No |
| 23 | Aitavaara-Anttila [47] | ICU | 479 | Logistic regression | NEWS on ED admission, SOFA score, and APACH score on ICU admission, GCS, urine output, blood pressure, oxygen saturation, respiratory rate, pulse rate, body temperature, use of oxygen or form of mechanical ventilation, use of vasoactive medication, chronic illnesses, and medications | No |
| 24 | Khan [48] | ICU | 325 | Logistic regression | Age, sex, time of presentation, ED triage category, vital signs, presenting complaints, comorbid conditions, laboratory values, radiological studies, procedures, severity of illness scores | No |
| 25 | Byrne [49] | Non-ICU | 106,788 | Logistic regression | Age, sex, severity triage score, illness severity score, comorbidities, sepsis, disabilities | No |
| 26 | Groenland [50] | ICU | 14,788 | Logistic regression | Disease severity, APACH IV score, comorbidities, age, admission diagnosis, reason for ICU admission (medical, urgent, or elective) | Yes |
| 27 | Haji [51] | ICU | 117 | Logistic regression | Age, sex, APACH II score, physiological and biochemical data: heart rate, respiratory rate, temperature, systolic blood pressure, GCS, pH, partial pressure of carbon dioxide, serum bicarbonate, white cell count, time to resuscitation and time to antibiotics | No |
| 28 | Santos [52] | ICU | 6176 | Logistic regression | Age, sex, admission due to neurological disease, cancer, infectious disease, hypertension, level of dependency, chronic dialytic kidney disease, GCS on admission, SOFA score, dependency level, use of vasopressors, mechanical ventilation, need for renal replacement therapy | No |
| 29 | Mejaddam [53] | ICU | 224 | Logistic regression | Age, sex, time and date of presentation, mechanism of injury, current use of antithrombotic medications, timing of intubation, initial results of radiological imaging, head computed tomography results, GCS, initial pupil reactivity, administration of blood products, initial laboratory values, initial vital signs, intracranial pressure monitor placement, use of antiepileptic agents, hyperosmolar agents, and vasopressors, prolonged hypotension | No |
| 30 | Saukonnen [54] | ICU | 1675 | No logistic regression | Age, sex, place of admission, NYHA class, diagnoses according to the APACH II score, and ICD (Tenth Revision), SAPS II, SOFA, TISS score | No |
| 31 | Hung [55] | ICU | 1242 | Logistic regression | Age, sex, vital signs, triage results, chief complaints, laboratory findings, baseline comorbidities, hospital discharge condition, length of ventilator use, APACH II score, diagnostic categories | Yes |
| 32 | Cardoso [56] | ICU | 401 | Cox regression | Age, sex, APACH II score, comorbidities, need for mechanical ventilation and tracheal intubation, vasoactive drug use, TISS score, SOFA, hospital ward admission | Yes |
| 33 | Ashkenazi [57] | Non-ICU | 28,108 | Logistic regression | Age, sex, type of specialty ward admission | No |
| 34 | Stey [58] | ICU | 30,915 | Logistic regression | Age, sex, race, systolic blood pressure, oxygen saturation, GCS, comorbidities (diabetes, cerebrovascular accident, dementia, dependent functional status, cirrhosis, varices), injuries (intracerebral hemorrhage, contusion, lung injury) insurance, transfer status, emergency transport vehicle, admission year, teaching hospital status, ACS trauma center designation, number of orthopedic and trauma surgeons and number of trauma ICU beds. | No |
| 35 | Choi [59] | ICU | 439 | Logistic regression | Age, sex, comorbidities (hypertension, diabetes, chronic renal disease, cardiovascular disease, and malignancy status), initial vital signs (systolic blood pressure, diastolic blood pressure, pulse rate, respiratory rate, and body temperature), KTAS level in the ED, SOFA score. | Yes |
| 36 | Lin [60] | ICU | 13,634 | Logistic regression | Age, sex and SAPS II, covariates were adjusted for age, sex, ethnicity, marital status, length of ICU stay, length of hospital stay, ICU types, SAPS II, and diagnostic category. | Yes |
| 37 | Altreby [61] | ICU | 1887 | Logistic regression | Age, sex, diagnosis, and general diagnostic category (medical, surgical, and trauma), mechanical ventilation status, need for vasopressors, need for CRRT, insertion of a central venous line, measures of severity such as APACHE IV, SOFA score, MEWS, and sepsis status. | Yes |
| 38 | Wessman [62] | Non-ICU | 641,314 | Logistic regression | Age, sex, any of the ten most common chief complaints pre-defined (abdominal pain, chest pain, shortness of breath, painful or swollen extremity, malaise, dysrhythmia, allergic reaction, syncope, intoxication, fever and undefined), triage priority at arrival, if the patient was given prehospital care given by ambulance or not, if the patients were admitted to in-hospital care or not if the patient presented to the ED in the weekend or not. The chief complaints can be seen as a crude proxy for comorbidity and should eliminate some confounding associated with complaint. | Yes |
| 39 | Rana [63] | ICU | 460 | No logistic regression | Time of admission, primary diagnoses, co-morbidities, time spent in ED from presentation to reaching ICU, APACHE IV. | Yes |
| 40 | Thibon [64] | Non-ICU | 15,496 | No logistic regression | Age, sex, severity triage score, biology, imaging | Yes |
| 41 | Asheim [65] | Non-ICU | 165,183 | Logistic regression | Age, sex, cardiovascular disease, infection, medical specialty, arrival with ambulance | No |
| 42 | Cheng [66] | Non-ICU | 4972 | Logistic regression | Age, sex, time of arrival, arrival with ambulance, ward disposition, number of ED patients, disease categories, health insurance | Yes |
| 43 | Crilly [67] | ICU | 423 | Logistic regression | Age, sex, severity triage score, daytime, time to the ED, mode of arrival, diagnosis, APACHE score | No |
| 44 | Davis [68] | Non-ICU | 3108 | Logistic regression | Age, sex, NIH-SSS score, comorbidities | Yes |
| 45 | Elay [69] | ICU | 206 | No logistic regression | Age, sex, disease severity scores, comorbidities, antibiotic administration, blood culture results, length of hospital stay, and 30-day mortality. SOFA and APACHE II | No |
| 46 | Rose [3] | ICU | 314,836 | Logistic regression | Age, sex, severity triage score, diagnosis, comorbidities, ventilation, ED annual census, ED shift time, institution, specialized center, hospital occupancy, WE admission | No |
| 47 | Sabaz [70] | ICU | 1297 | Logistic regression | Age, sex, length of hospital stay, length of ICU stay, ICU admission diagnosis, APACHE II score and comorbidities, APACHE II score, APACHE IV score, SAPS 3 score, SOFA score, TISS score, GSC score on the first day of ICU, results of blood samples taken on the first day of ICU, need for MV and tracheal intubation, vasoactive agents use, invasive procedures used, treatments | Yes |
| 48 | Verma [71] | ICU | 3429 | No logistic regression | Age, sex, diagnosis, severity triage score | Yes |
| 49 | Derose [9] | Non-ICU | 136,740 | Logistic regression | Age, sex, severity triage score, ambulance arrival, race, ED shift time, blood pressure, heart rate, ED system crowding | No |
| 50 | Jain [72] | Non-ICU | 190 | Logistic regression | Age, sex, NIH-SSS, disposition, hospital length of stay, comorbidity, thrombolysis | No |
| Author | Study Group (n) | Association with IHM | Quality Score of Studies | Confounding Factors | MA | |
|---|---|---|---|---|---|---|
| ICU | Carter [25] | 48,803 | No | 8 | Not analyzed | Yes |
| Jones [32] | 162 | Yes | 6 | Not analyzed | Yes | |
| Serviá [34] | 243 | No | 7 | Not analyzed Factors associated with mortality: age greater than 60 years, MV, head injuries with abbreviated injury scale scores of 4 or higher, and shock | Yes | |
| Tilluckdharry [35] | 443 | No | 8 | Not analyzed | Yes | |
| Hirshi [36] | 294 | No | 8 | Not analyzed Factors associated with mortality: liver disease | Yes | |
| García-Gigorro [38] | 269 | Yes | 5.5 | Not analyzed | Yes | |
| Agustin [39] | 287 | No | 5 | SOFA, mean arterial blood pressure, and lactate | Yes | |
| Siletz [40] | 241 | No | 6 | Age, ISS, number of comorbidities | Yes | |
| Soni [42] | 232 | No | 3.3 | Age, SpO2, GCS, referring status, ICU stay | Yes | |
| Zhang [44] | 1997 | Yes | 6 | PaO2/FiO2, serum creatinine, age, SOFA, Body Mass Index, lactate, comorbidities, and infection site | Yes | |
| Intas [45] | 200 | Yes | 6 | Reason for admission (surgical vs. medical), direct versus indirect ICU admission, time of admission, fever | Yes | |
| Aitavaara-Anttila M [47] | 479 | No | 8 | Not analyzed | Yes | |
| Khan [48] | 325 | No | 6 | Age, discharge diagnostic (renal, sepsis, malignancy, respiratory), CT scan result, triage category | Yes | |
| Groenland [50] | 14,788 | Yes | 8 | APACH IV, comorbidities, age, admission diagnosis, reason for ICU admission | Yes | |
| Haji [51] | 117 | No | 6 | Not analyzed | No | |
| Santos [52] | 6176 | No | 6 | Age, sex, neurological disease, infection/sepsis, cancer, arterial hypertension, need for assistance, chronic renal dialysis, GCS at admission | No | |
| Lin [60] | 13,634 | Yes | 6 | ICU types, length of hospital stay, length of ICU stay, SAP score II, diagnostic category | Yes | |
| Mejaddam [53] | 224 | No | 6 | Not analyzed No clear mortality data | No | |
| Saukonnen [54] | 1675 | No | 6 | No analyzed | No | |
| Hung [55] | 1242 | Yes | 6 | Higher APACHE II score, triage level as non-urgent, sex, diagnostic category | No | |
| Cardoso [56] | 401 | Yes | 6 | Sex, age, comorbidity, APS, SOFA, TISS, general hospital ward, sepsis diagnosis | No | |
| Stey [58] | 30,915 | No | 7 | ACS verification hospital level, adult beds, triage score, hospital teaching status, trauma ICU beds, number of neurosurgeons, number of orthopedic surgeons, number of trauma surgeons | Yes | |
| Choi [59] | 439 | Yes | 6.5 | Malignancy, systolic blood pressure, platelets, albumin, SOFA, septic shock, vasopressor at ED, ventilator at ED | Yes | |
| Altreby [61] | 1887 | Yes | 6.5 | Age, sex, mechanical ventilation, CRRT, vasopressors, central venous line, diagnosis, APACHE IV, SOFA, MEWS, sepsis, time to admission, ICU length of stay | Yes | |
| Rana [63] | 460 | Yes | 5.5 | Not analyzed | Yes | |
| Crilly [67] | 423 | No | 5.5 | Not analyzed | No | |
| Elay [69] | 206 | No | 5 | Not analyzed | No | |
| Rose [3] | 314,836 | Yes | 7 | Age, sex, comorbidity, trauma admission, ventilation, ED annual census, ED shift time, institution, specialized center, hospital occupancy, weekend admission, ICU census | No | |
| Sabaz [70] | 1297 | No | 6.5 | MV, lactate, APACH 2, SAP 3, APACH 4, SOFA, inotrope agent, septic shock warning, white blood count | No | |
| Verma [71] | 3429 | Yes | 6 | Not analyzed | Yes | |
| Non-ICU | Mitra [26] | 10,107 | Yes | 6 | Age, sex, triage category, hospital type | Yes |
| Chong [27] | 15,886 | No | 8 | Age, injuries, sepsis, stroke, pneumonia, renal diseases, COPD, liver diseases | Yes | |
| Flabouris [28] | 43,484 | No | 7 | Age, triage category, sex, admission source | Yes | |
| Akhtar [29] | 894 | Yes | 7 | Age, prior stroke, coronary artery disease, history of smoking, dysphagia present at admission | Yes | |
| Diercks DB [30] | 42,780 | No | 7 | Not analyzed | Yes | |
| Chen [31] | 432 | No | 7 | Not analyzed | Yes | |
| Mowery [33] | 3973 | Yes | 8 | RTS, age, ISS, | Yes | |
| Plunkett [37] | 23,114 | Yes | 6 | Sex, major disease by category, Charlson’s comorbidity index, ICU admission, blood transfusion, troponin elevation | No | |
| Junhasavasdikul [41] | 381 | No | 4 | MEWS, sepsis, Eastern Cooperative Oncology Group | Yes | |
| Paton [43] | 24,746 | Yes | 6 | Age, sex, triage category, ambulance transport, residing at home | Yes | |
| Richardson [46] | 3918 | No | 6 | Age, ISS, GCS, positive CT | Yes | |
| Byrne [49] | 106,788 | No | 8 | Not analyzed | Yes | |
| Ashkenazi [57] | 28,108 | No | 8 | Age, sex | Yes | |
| Wessman [62] | 641,314 | Yes | 7.5 | Age | No | |
| Thibon [64] | 15,496 | Yes | 6.5 | Not analyzed | No | |
| Asheim [65] | 165,183 | No | 7 | Age, sex, cardiovascular disease, infection, ambulance, medical specialty | No | |
| Cheng [66] | 4972 | Yes | 6.5 | Not analyzed | No | |
| Davis [68] | 3108 | Yes | 8 | Age, comorbidity | Yes | |
| Derose [9] | 136,740 | No | 5 | Sex, race/ethnicity, and pre-existing comorbidities, ambulance arrival, triage, blood pressure and pulse, triage score, diagnosis, day shift, weekend, month | No | |
| Jain [72] | 190 | No | 8 | SS, thrombolysis, hospital length of stay | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lauque, D.; Khalemsky, A.; Boudi, Z.; Östlundh, L.; Xu, C.; Alsabri, M.; Onyeji, C.; Cellini, J.; Intas, G.; Soni, K.D.; et al. Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 32. https://doi.org/10.3390/jcm12010032
Lauque D, Khalemsky A, Boudi Z, Östlundh L, Xu C, Alsabri M, Onyeji C, Cellini J, Intas G, Soni KD, et al. Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(1):32. https://doi.org/10.3390/jcm12010032
Chicago/Turabian StyleLauque, Dominique, Anna Khalemsky, Zoubir Boudi, Linda Östlundh, Chang Xu, Mohammed Alsabri, Churchill Onyeji, Jacqueline Cellini, Geroge Intas, Kapil Dev Soni, and et al. 2023. "Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 1: 32. https://doi.org/10.3390/jcm12010032
APA StyleLauque, D., Khalemsky, A., Boudi, Z., Östlundh, L., Xu, C., Alsabri, M., Onyeji, C., Cellini, J., Intas, G., Soni, K. D., Junhasavasdikul, D., Cabello, J. J. T., Rathlev, N. K., Liu, S. W., Camargo, C. A., Jr., Slagman, A., Christ, M., Singer, A. J., Houze-Cerfon, C.-H., ... Bellou, A. (2023). Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(1), 32. https://doi.org/10.3390/jcm12010032









