Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review
Abstract
1. Introduction
2. Materials and Methods
3. Safety of MPLT
4. Efficacy of Subthreshold Micropulse Laser and Intravitreal Administration
5. Comparison of Subthreshold Micropulse and Conventional Laser Treatment
6. Subthreshold Micropulse Laser Treatment and Intravitreal Therapy
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gale, R.; Scanlon, P.H.; Evans, M.; Ghanchi, F.; Yang, Y.; Silvestri, G.; Freeman, M.; Maisey, A.; Napier, J. Action on Diabetic Macular Oedema: Achieving Optimal Patient Management in Treating Visual Impairment Due to Diabetic Eye Disease. Eye 2017, 31 (Suppl. S1), S1–S20. [Google Scholar] [CrossRef] [PubMed]
- Teo, Z.L.; Tham, Y.C.; Yu, M.; Chee, M.L.; Rim, T.H.; Cheung, N.; Bikbov, M.M.; Wang, Y.X.; Tang, Y.; Lu, Y.; et al. Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045: Systematic Review and Meta-Analysis. Ophthalmology 2021, 128, 1580–1591. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Garcia-Arumi, J.; Bandello, F.; Berg, K.; Chakravarthy, U.; Gerendas, B.S.; Jonas, J.; Larsen, M.; Tadayoni, R.; Loewenstein, A. Guidelines for the Management of Diabetic Macular Edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica 2017, 237, 185–222. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.K.; Jampol, L.M. The Diabetic Retinopathy Clinical Research Network (DRCR.Net) and Its Contributions to the Treatment of Diabetic Retinopathy Keywords Diabetic Retinopathy Clinical Research Network Proliferative Diabetic Retinopathy Panretinal Photocoagulation Diabetic Macular Edema. Ophthalmic Res. 2019, 62, 225–230. [Google Scholar] [CrossRef]
- Virgili, G.; Parravano, M.; Evans, J.R.; Gordon, I.; Lucenteforte, E. Anti-Vascular Endothelial Growth Factor for Diabetic Macular Oedema: A Network Meta-Analysis. Cochrane Database Syst. Rev. 2017, 6. [Google Scholar] [CrossRef]
- Sędziak-Marcinek, B.; Teper, S.; Chełmecka, E.; Wylęgała, A.; Marcinek, M.; Bas, M.; Wylęgała, E. Diabetic Macular Edema Treatment with Bevacizumab Does Not Depend on the Retinal Nonperfusion Presence. J. Diabetes Res. 2021, 2021, 1–15. [Google Scholar] [CrossRef]
- Moshfeghi, A.A.; Rosenfeld, P.J.; Flynn, H.W.; Schwartz, S.G.; Davis, J.L.; Murray, T.G.; Smiddy, W.E.; Berrocal, A.M.; Dubovy, S.R.; Lee, W.H.; et al. Endophthalmitis after Intravitreal Vascular [Corrected] Endothelial Growth Factor Antagonists: A Six-Year Experience at a University Referral Center. Retina 2011, 31, 662–668. [Google Scholar] [CrossRef]
- Grzybowski, A.; Markeviciute, A.; Zemaitiene, R. Treatment of Macular Edema in Vascular Retinal Diseases: A 2021 Update. J. Clin. Med. 2021, 10, 5300. [Google Scholar] [CrossRef]
- Elhamid, A.H.A. Combined Intravitreal Dexamethasone Implant And Micropulse Yellow Laser For Treatment Of Anti-VEGF Resistant Diabetic Macular Edema. Open Ophthalmol. J. 2017, 11, 164–172. [Google Scholar] [CrossRef]
- Everett, L.A.; Paulus, Y.M. Laser Therapy in the Treatment of Diabetic Retinopathy and Diabetic Macular Edema. Curr. Diab Rep. 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Photocoagulation for Diabetic Macular Edema. Early Treatment Diabetic Retinopathy Study Report Number 1. Early Treatment Diabetic Retinopathy Study Research Group. Available online: https://pubmed.ncbi.nlm.nih.gov/2866759/ (accessed on 22 October 2022).
- Sivaprasad, S.; Elagouz, M.; McHugh, D.; Shona, O.; Dorin, G. Micropulsed Diode Laser Therapy: Evolution and Clinical Applications. Surv. Ophthalmol. 2010, 55, 516–530. [Google Scholar] [CrossRef] [PubMed]
- Luttrull, J.K.; Dorin, G. Subthreshold Diode Micropulse Laser Photocoagulation (SDM) as Invisible Retinal Phototherapy for Diabetic Macular Edema: A Review. Curr. Diabetes Rev. 2012, 8, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Luttrull, J.K.; Sinclair, S.H. Safety of Transfoveal Subthreshold Diode Micropulse Laser for Fovea-Involving Diabetic Macular Edema in Eyes with Good Visual Acuity. Retina 2014, 34, 2010–2020. [Google Scholar] [CrossRef] [PubMed]
- Gawęcki, M. Micropulse Laser Treatment of Retinal Diseases. J. Clin. Med. 2019, 8, 242. [Google Scholar] [CrossRef] [PubMed]
- Donati, M.C.; Murro, V.; Mucciolo, D.P.; Giorgio, D.; Cinotti, G.; Virgili, G.; Rizzo, S. Subthreshold Yellow Micropulse Laser for Treatment of Diabetic Macular Edema: Comparison between Fixed and Variable Treatment Regimen. Eur. J. Ophthalmol. 2021, 31, 1254–1260. [Google Scholar] [CrossRef]
- Zas, M.; Cotic, M.; Wu, M.; Wu, A.; Wu, L. Macular Laser Photocoagulation in the Management of Diabetic Macular Edema: Still Relevant in 2020? Taiwan J. Ophthalmol. 2020, 10, 87–94. [Google Scholar] [CrossRef]
- Inagaki, K.; Ohkoshi, K.; Ohde, S.; Deshpande, G.A.; Ebihara, N.; Murakami, A. Comparative Efficacy of Pure Yellow (577-Nm) and 810-Nm Subthreshold Micropulse Laser Photocoagulation Combined with Yellow (561–577-Nm) Direct Photocoagulation for Diabetic Macular Edema. Jpn. J. Ophthalmol. 2015, 59, 21–28. [Google Scholar] [CrossRef]
- Kikushima, W.; Shijo, T.; Furuhata, Y.; Sakurada, Y.; Kashiwagi, K. Comparison of the 1-Year Visual and Anatomical Outcomes between Subthreshold Red (670 Nm) and Yellow (577 Nm) Micro-Pulse Laser Treatment for Diabetic Macular Edema. Pharmaceuticals 2021, 14, 1100. [Google Scholar] [CrossRef]
- Scholz, P.; Altay, L.; Fauser, S. A Review of Subthreshold Micropulse Laser for Treatment of Macular Disorders. Adv. Ther. 2017, 34, 1528–1555. [Google Scholar] [CrossRef]
- Moore, S.M.; Chao, D.L. Application of Subthreshold Laser Therapy in Retinal Diseases: A Review. Expert Rev. Ophthalmol. 2018, 13, 311–320. [Google Scholar] [CrossRef]
- Su, D.; Hubschman, J.P. A Review of Subthreshold Micropulse Laser and Recent Advances in Retinal Laser Technology. Ophthalmol. Ther. 2017, 6, 1–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brader, H.S.; Young, L.H.Y. Subthreshold Diode Micropulse Laser: A Review. Semin. Ophthalmol. 2016, 31, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Jorge, E.C.; Jorge, E.N.; Botelho, M.; Farat, J.G.; Virgili, G.; el Dib, R. Monotherapy Laser Photocoagulation for Diabetic Macular Oedema. Cochrane Database Syst. Rev. 2018, 2018, CD010859. [Google Scholar] [CrossRef]
- Ohkoshi, K.; Tsuiki, E.; Kitaoka, T.; Yamaguchi, T. Visualization of Subthreshold Micropulse Diode Laser Photocoagulation by Scanning Laser Ophthalmoscopy in the Retro Mode. Am. J. Ophthalmol. 2010, 150, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Luttrull, J.K.; Sramek, C.; Palanker, D.; Spink, C.J.; Musch, D.C. Long-Term Safety, High-Resolution Imaging, and Tissue Temperature Modeling of Subvisible Diode Micropulse Photocoagulation for Retinovascular Macular Edema. Retina 2012, 32, 375–386. [Google Scholar] [CrossRef]
- Vujosevic, S.; Martini, F.; Longhin, E.; Convento, E.; Cavarzeran, F.; Midena, E. Subthreshold Micropulse Yellow Laser Versus Subthreshold Micropulse Infrared Laser in Center-Involving Diabetic Macular Edema. Morphologic and Functional Safety. Retina 2015, 35, 1594–1603. [Google Scholar] [CrossRef]
- Wells-Gray, E.M.; Doble, N.; Ohr, M.P.; Choi, S.S. Structural Integrity of Individual Cone Photoreceptors after Short-Wavelength Subthreshold Micropulse Laser Therapy for Diabetic Macular Edema. Ophthalmic Surg. Lasers Imaging 2018, 49, 946–954. [Google Scholar] [CrossRef]
- Midena, E.; Bini, S.; Frizziero, L.; Pilotto, E.; Esposito, G.; Micera, A. Aqueous Humour Concentrations of PEDF and Erythropoietin Are Not Influenced by Subthreshold Micropulse Laser Treatment of Diabetic Macular Edema. Biosci. Rep. 2019, 39, BSR20190328. [Google Scholar] [CrossRef]
- Midena, E.; Micera, A.; Frizziero, L.; Pilotto, E.; Esposito, G.; Bini, S. Sub-Threshold Micropulse Laser Treatment Reduces Inflammatory Biomarkers in Aqueous Humour of Diabetic Patients with Macular Edema. Sci. Rep. 2019, 9, 10034. [Google Scholar] [CrossRef]
- Chang, D.B.; Luttrull, J.K. Comparison of Subthreshold 577 and 810 Nm Micropulse Laser Effects on Heat-Shock Protein Activation Kinetics: Implications for Treatment Efficacy and Safety. Transl. Vis. Sci. Technol. 2020, 9, 23. [Google Scholar] [CrossRef]
- Midena, E.; Bini, S. Changes of Aqueous Humor Müller Cells’ Biomarkers in Human Patients Affected by Diabetic Macular Edema after Subthreshold Micropulse Laser Treatment. Retina 2020, 40, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Shiraya, T.; Araki, F.; Nakagawa, S.; Ueta, T.; Totsuka, K.; Abe, H.; Naito, Y.; Toyama, T.; Sugimoto, K.; Kato, S. Differential Gene Expression Analysis Using RNA Sequencing: Retinal Pigment Epithelial Cells after Exposure to Continuous-Wave and Subthreshold Micropulse Laser. Jpn. J. Ophthalmol. 2022, 66, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.K.; Merrill, K.D.; Truong, S.N.; Forward, K.M.; Morse, L.S.; Telander, D.G. The Comparative Histologic Effects of Subthreshold 532- and 810-Nm Diode Micropulse Laser on the Retina. Investig. Ophthalmol. Vis. Sci. 2013, 54, 2216–2224. [Google Scholar] [CrossRef] [PubMed]
- de Cillà, S.; Vezzola, D.; Farruggio, S.; Vujosevic, S.; Clemente, N.; Raina, G.; Mary, D.; Casini, G.; Rossetti, L.; Avagliano, L.; et al. The Subthreshold Micropulse Laser Treatment of the Retina Restores the Oxidant/Antioxidant Balance and Counteracts Programmed Forms of Cell Death in the Mice Eyes. Acta Ophthalmol. 2019, 97, e559–e567. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, K.; Kakihara, S.; Tanaka, M.; Shindo, T.; Murata, T. Investigation of the Therapeutic Mechanism of Subthreshold Micropulse Laser Irradiation in Retina. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Funatsu, H.; Yamashita, H.; Noma, H.; Mimura, T.; Nakamura, S.; Sakata, K.; Hori, S. Aqueous Humor Levels of Cytokines Are Related to Vitreous Levels and Progression of Diabetic Retinopathy in Diabetic Patients. Arch. Clin. Exp. Ophthalmol. 2005, 243, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Mitamura, Y.; Ogata, K.; Arai, M.; Takatsuna, Y.; Yamamoto, S. Functional and Morphological Changes of Macula after Subthreshold Micropulse Diode Laser Photocoagulation for Diabetic Macular Oedema. Eye 2010, 24, 784–788. [Google Scholar] [CrossRef]
- Işık, M.U.; Değirmenci, M.F.K.; Sağlık, A. Factors Affecting the Response to Subthreshold Micropulse Laser Therapy Used in Center-Involved Diabetic Macular Edema. Lasers Med. Sci. 2022, 37, 1865–1871. [Google Scholar] [CrossRef]
- Ueda, K.; Shiraya, T.; Araki, F.; Hashimoto, Y.; Yamamoto, M.; Yamanari, M.; Ueta, T.; Minami, T.; Aoki, N.; Sugiyama, S.; et al. Changes in Entropy on Polarized-Sensitive Optical Coherence Tomography Images after Therapeutic Subthreshold Micropulse Laser for Diabetic Macular Edema: A Pilot Study. PLoS ONE 2021, 16, e0257000. [Google Scholar] [CrossRef]
- Valera-Cornejo, D.A.; García-Roa, M.; Quiroz-Mendoza, J.; Arias-Gómez, A.; Ramírez-Neria, P.; Villalpando-Gómez, Y.; Romero-Morales, V.; García-Franco, R. Micropulse Laser in Patients with Refractory and Treatment-Naïve Center–Involved Diabetic Macular Edema: Short Terms Visual and Anatomic Outcomes. Ther. Adv. Ophthalmol. 2021, 13, 251584142097911. [Google Scholar] [CrossRef]
- Passos, R.M.; Malerbi, F.K.; Rocha, M.; Maia, M.; Farah, M.E. Real-Life Outcomes of Subthreshold Laser Therapy for Diabetic Macular Edema. Int. J. Retina Vitr. 2021, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Frizziero, L.; Calciati, A.; Torresin, T.; Midena, G.; Parrozzani, R.; Pilotto, E.; Midena, E. Diabetic Macular Edema Treated with 577-Nm Subthreshold Micropulse Laser: A Real-Life, Long-Term Study. J. Pers. Med. 2021, 11, 405. [Google Scholar] [CrossRef]
- Vujosevic, S.; Gatti, V.; Muraca, A.; Brambilla, M.; Villani, E.; Nucci, P.; Rossetti, L.; de Cilla, S. Optical Coherence Tomography Angiography Changes after Subthreshold Micropulse Yellow Laser in Diabetic Macular Edema. Retina 2020, 40, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Toma, C.; Villani, E.; Brambilla, M.; Torti, E.; Leporati, F.; Muraca, A.; Nucci, P.; de Cilla, S. Subthreshold Micropulse Laser in Diabetic Macular Edema: 1-Year Improvement in OCT/OCT-Angiography Biomarkers. Transl. Vis. Sci. Technol. 2020, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Vesela, S.; Hejsek, L.; Stepanov, A.; Dusova, J.; Marak, J.; Jiraskova, N.; Studnicka, J. Use of Micropulse Laser in Patients with Diabetic Macular Edema at the Department of Ophthalmology, University Hospital Hradec Kralove. Ceská A Slov. Oftalmol. Cas. Ceské Oftalmol. Spol. A Slov. Oftalmol. Spol. 2018, 75, 53–58. [Google Scholar] [CrossRef]
- Latalska, M.; Prokopiuk, A.; Wróbel-Dudzińska, D.; Mackiewicz, J. Subthreshold Micropulse Yellow 577 Nm Laser Therapy of Diabetic Macular Oedema in Rural and Urban Patients of South-Eastern Poland. Ann. Agric. Environ. Med. 2017, 24, 96–99. [Google Scholar] [CrossRef]
- Abouhussein, M. Micropulse Laser for Diabetic Macular Edema. Delta J. Ophthalmol. 2016, 17, 167. [Google Scholar] [CrossRef]
- Nicolò, M.; Musetti, D.; Traverso, C.E. Yellow Micropulse Laser in Diabetic Macular Edema: A Short-Term Pilot Study. Eur. J. Ophthalmol. 2014, 24, 885–889. [Google Scholar] [CrossRef]
- Mansouri, A.; Sampat, K.M.; Malik, K.J.; Steiner, J.N.; Glaser, B.M. Efficacy of Subthreshold Micropulse Laser in the Treatment of Diabetic Macular Edema Is Influenced by Pre-Treatment Central Foveal Thickness. Eye 2014, 28, 1418–1424. [Google Scholar] [CrossRef]
- Kwon, Y.H.; Lee, D.K.; Kwon, O.W. The Short-Term Efficacy of Subthreshold Micropulse Yellow (577-Nm) Laser Photocoagulation for Diabetic Macular Edema. Korean J. Ophthalmol. 2014, 28, 379–385. [Google Scholar] [CrossRef][Green Version]
- Takatsuna, Y.; Yamamoto, S.; Nakamura, Y.; Tatsumi, T.; Arai, M.; Mitamura, Y. Long-Term Therapeutic Efficacy of the Subthreshold Micropulse Diode Laser Photocoagulation for Diabetic Macular Edema. Jpn. J. Ophthalmol. 2011, 55, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Ohkoshi, K.; Yamaguchi, T. Subthreshold Micropulse Diode Laser Photocoagulation for Diabetic Macular Edema in Japanese Patients. Am. J. Ophthalmol. 2010, 149, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Değirmenci, M.F.K.; Demirel, S.; Batıoğlu, F.; Özmert, E. Short-Term Efficacy of Micropulse Yellow Laser in Non-Center-Involving Diabetic Macular Edema: Preliminary Results. Turk. J. Ophthalmol. 2018, 48, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Friberg, T.R.; Karatza, E.C. The Treatment of Macular Disease Using a Micropulsed and Continuous Wave 810-Nm Diode Laser. Ophthalmology 1997, 104, 2030–2038. [Google Scholar] [CrossRef]
- Citirik, M. The Impact of Central Foveal Thickness on the Efficacy of Subthreshold Micropulse Yellow Laser Photocoagulation in Diabetic Macular Edema. Lasers Med. Sci. 2019, 34, 907–912. [Google Scholar] [CrossRef]
- Frizziero, L.; Calciati, A.; Midena, G.; Torresin, T.; Parrozzani, R.; Pilotto, E.; Midena, E. Subthreshold Micropulse Laser Modulates Retinal Neuroinflammatory Biomarkers in Diabetic Macular Edema. J. Clin. Med. 2021, 10, 3134. [Google Scholar] [CrossRef]
- Nowacka, B.; Mozolewska-Piotrowska, K.; Lubiński, W.; Machalińska, A.; Grabowicz, A. Macular Function and Structure in Patients with Center-Involved Diabetic Macular Edema before and after Micropulse Laser Therapy. Klin. Oczna. 2021, 123, 90–95. [Google Scholar] [CrossRef]
- Marashi, A.; Zazo, A. Hybrid Threshold Laser to Treat Diabetic Macular Edema: A Retrospective Analysis Single Center Cohort Study. Ann. Med. Surg. 2022, 80, 104222. [Google Scholar] [CrossRef]
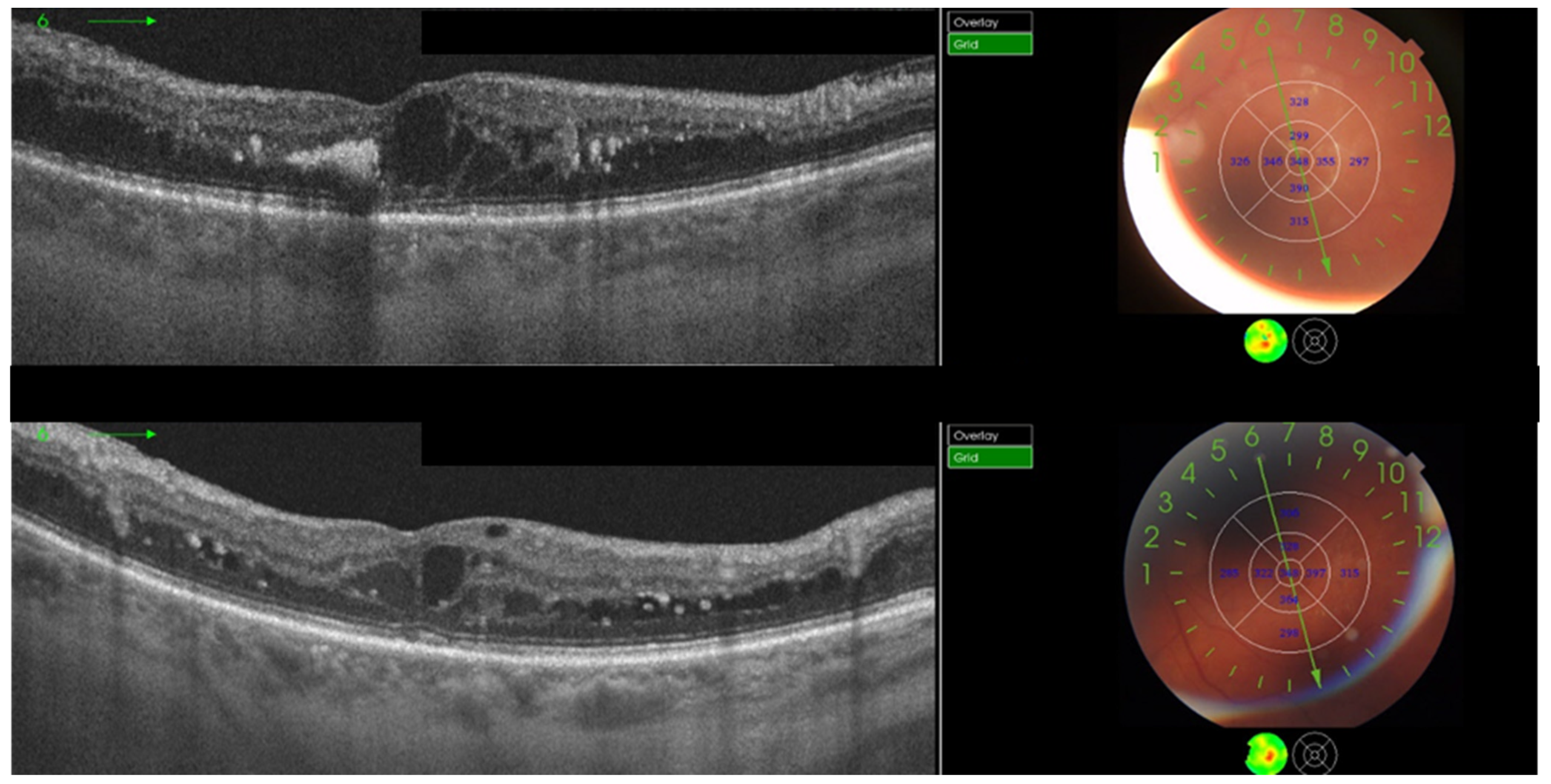
- Hunt, M.; Teper, S.; Wylęgała, A.; Wylęgała, E. Response to 1-Year Fixed-Regimen Bevacizumab Therapy in Treatment-Naïve DME Patients: Assessment by OCT Angiography. J. Diabetes Res. 2022, 2022, 3547461. [Google Scholar] [CrossRef]
- Vujosevic, S.; Bottega, E.; Casciano, M.; Pilotto, E.; Convento, E.; Midena, E. Microperimetry and Fundus Autofluorescence in Diabetic Macular Edema: Subthreshold Micropulse Diode Laser Versus Modified Early Treatment Diabetic Retinopathy Study Laser Photocoagulation. Retina 2010, 30, 908–916. [Google Scholar] [CrossRef]
- Lavinsky, D.; Cardillo, J.A.; Melo, L.A.S.; Dare, A.; Farah, M.E.; Belfort, R. Randomized Clinical Trial Evaluating METDRS versus Normal or High-Density Micropulse Photocoagulation for Diabetic Macular Edema. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4314–4323. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, P.; Ramanjulu, R.; Azad, R.; Vohra, R.; Garg, S. Subthreshold Micropulse Diode Laser and Double Frequency Neodymium: YAG Laser in Treatment of Diabetic Macular Edema: A Prospective, Randomized Study Using Multifocal Electroretinography. Photomed. Laser Surg. 2011, 29, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, K.; Ohkoshi, K.; Ohde, S. Spectral-Domain Optical Coherence Tomography Imaging of Retinal Changes After Conventional Multicolor Laser, Subthreshold Micropulse Diode Laser, or Pattern Scanning Laser Therapy in Japanese with Macular Edema. Retina 2012, 32, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Xie, T.Y.; Guo, Q.Q.; Wang, Y.; Wang, Q.; Chen, X.Y. Randomized, Controlled Clinical Trial Comparison of SDM Laser versus Argon Ion Laser in Diabetic Macular Edema. International. Eye Sci. 2013, 13, 2370–2372. [Google Scholar] [CrossRef]
- Othman, I.S.; Eissa, S.A.; Skotb, M.; Sadek, S.H. Subthreshold Diode-Laser Micropulse Photocoagulation as a Primary and Secondary Line of Treatment in Management of Diabetic Macular Edema. Clin. Ophthalmol. 2014, 8, 653–659. [Google Scholar] [CrossRef]
- Fazel, F.; Bagheri, M.; Golabchi, K.; Jahanbani Ardakani, H. Comparison of Subthreshold Diode Laser Micropulse Therapy versus Conventional Photocoagulation Laser Therapy as Primary Treatment of Diabetic Macular Edema. J. Curr. Ophthalmol. 2016, 28, 206–211. [Google Scholar] [CrossRef]
- Chhablani, J.; Alshareef, R.; Kim, D.T.; Narayanan, R.; Goud, A.; Mathai, A. Comparison of Different Settings for Yellow Subthreshold Laser Treatment in Diabetic Macular Edema. BMC Ophthalmol. 2018, 18, 168. [Google Scholar] [CrossRef]
- Bougatsou, P.; Panagiotopoulou, E.K.; Gkika, M.; Dardabounis, D.; Konstantinidis, A.; Sideroudi, H.; Perente, I.; Labiris, G. Comparison of Subthreshold 532 Nm Diode Micropulse Laser with Conventional Laser Photocoagulation in the Treatment of Non-Centre Involved Clinically Significant Diabetic Macular Edema. Acta Med. 2020, 63, 25–30. [Google Scholar] [CrossRef]
- Al-Barki, A.; Al-Hijji, L.; High, R.; Schatz, P.; Do, D.; Nguyen, Q.D.; Luttrull, J.K.; Kozak, I. Comparison of Short-Pulse Subthreshold (532 Nm) and Infrared Micropulse (810 Nm) Macular Laser for Diabetic Macular Edema. Sci. Rep. 2021, 11, 14. [Google Scholar] [CrossRef]
- Lois, N.; Gardner, E.; Waugh, N.; Azuara-Blanco, A.; Mistry, H.; McAuley, D.; Acharya, N.; Aslam, T.M.; Bailey, C.; Chong, V.; et al. Diabetic Macular Oedema and Diode Subthreshold Micropulse Laser (DIAMONDS): Study Protocol for a Randomised Controlled Trial. Trials 2019, 20, 122. [Google Scholar] [CrossRef]
- Lois, N.; Campbell, C.; Waugh, N.; Azuara-Blanco, A.; Maredza, M.; Mistry, H.; McAuley, D.; Acharya, N.; Aslam, T.M.; Bailey, C.; et al. DIAbetic Macular Oedema aNd Diode Subthreshold Micropulse Laser (DIAMONDS): A Randomized Double-Masked Non-Inferiority Clinical Trial. Ophthalmology 2022, 20, 122. [Google Scholar] [CrossRef]
- Jhingan, M.; Goud, A.; Peguda, H.K.; Khodani, M.; Luttrull, J.K.; Chhablani, J. Subthreshold Microsecond Laser for Proliferative Diabetic Retinopathy: A Randomized Pilot Study. Clin. Ophthalmol. 2018, 12, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.J.; Xiao, J.H.; Zeng, P.; Zeng, R.; Gao, X.; Zhang, Y.C.; Lan, Y.Q. Optical Coherence Tomography Angiography Assessment of 577 Nm Laser Effect on Severe Non-Proliferative Diabetic Retinopathy with Diabetic Macular Edema. Int. J. Ophthalmol. 2020, 45, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, K.; Hamada, M.; Ohkoshi, K. Minimally Invasive Laser Treatment Combined with Intravitreal Injection of Anti-Vascular Endothelial Growth Factor for Diabetic Macular Oedema. Sci. Rep. 2019, 9, 7585. [Google Scholar] [CrossRef] [PubMed]
- Akkaya, S.; Açikalin, B.; Dogan, Y.E.; Çoban, F. Subthreshold Micropulse Laser versus Intravitreal Anti- VEGF for Diabetic Macular Edema Patients with Relatively Better Visual Acuity. Int. J. Ophthalmol. 2020, 13, 1606–1611. [Google Scholar] [CrossRef]
- Akhlaghi, M.; Dehghani, A.; Pourmohammadi, R.; Asadpour, L.; Pourazizi, M. Effects of Subthreshold Diode Micropulse Laser Photocoagulation on Treating Patients with Refractory Diabetic Macular Edema. J. Curr. Ophthalmol. 2019, 31, 157–160. [Google Scholar] [CrossRef]
- Altınel, G.M.; Acikalin, B.; Guler Alis, M.; Demir, G.; Mert Mutibayraktaroglu, K.; Melike Gedar Totuk, O.; Ardagil, A. Comparison of the Efficacy and Safety of Anti-VEGF Monotherapy versus Anti-VEGF Therapy Combined with Subthreshold Micropulse Laser Therapy for Diabetic Macular Edema. Lasers Med. Sci. 2021, 36, 1545–1553. [Google Scholar] [CrossRef]
- el Matri, L.; Chebil, A.; el Matri, K.; Falfoul, Y.; Chebbi, Z. Subthreshold Micropulse Laser Adjuvant to Bevacizumab versus Bevacizumab Monotherapy in Treating Diabetic Macular Edema: One- Year- Follow-Up. Ther. Adv. Ophthalmol. 2021, 13, 251584142110408. [Google Scholar] [CrossRef]
- Moisseiev, E.; Abbassi, S.; Thinda, S.; Yoon, J.; Yiu, G.; Morse, L.S. Subthreshold Micropulse Laser Reduces Anti-VEGF Injection Burden in Patients with Diabetic Macular Edema. Eur. J. Ophthalmol. 2018, 28, 68–73. [Google Scholar] [CrossRef]
- Abdelrahman, A.; Massoud, W.; Elshafei, A.M.K.; Genidy, M.; Abdallah, R.M.A. Anatomical and Functional Outcomes of Subthreshold Micropulse Laser versus Intravitreal Ranibizumab Injection in Treatment of Diabetic Macular Edema. Int. J. Retina Vitreous 2020, 6, 63. [Google Scholar] [CrossRef]
- Furashova, O.; Strassburger, P.; Becker, K.A.; Engelmann, K. Efficacy of Combining Intravitreal Injections of Ranibizumab with Micropulse Diode Laser versus Intravitreal Injections of Ranibizumab Alone in Diabetic Macular Edema (ReCaLL): A Single Center, Randomised, Controlled, Non-Inferiority Clinical Trial. BMC Ophthalmol. 2020, 20, 308. [Google Scholar] [CrossRef] [PubMed]
- Bıçak, F.; Kayıkçıoğlu, Ö.R.; Altınışık, M.; Doğruya, S.; Kurt, E. Efficacy of Subthreshold Micropulse Laser Combined with Ranibizumab in the Treatment of Diabetic Macular Edema. Int. Ophthalmol. 2022, 42, 3829–3836. [Google Scholar] [CrossRef] [PubMed]
- Mi, X.; Gu, X.; Yu, X. The Efficacy of Micropulse Laser Combined with Ranibizumab in Diabetic Macular Edema Treatment: Study Protocol for a Randomized Controlled Trial. Trials 2022, 23, 736. [Google Scholar] [CrossRef] [PubMed]
- Khattab, A.M.; Hagras, S.M.; AbdElhamid, A.H.; Torky, M.A.; Awad, E.A.; Abdelhameed, A.G. Aflibercept with Adjuvant Micropulsed Yellow Laser versus Aflibercept Monotherapy in Diabetic Macular Edema. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 1373–1380. [Google Scholar] [CrossRef]
- Abouhussein, M.A.; Gomaa, A.R. Aflibercept plus Micropulse Laser versus Aflibercept Monotherapy for Diabetic Macular Edema: 1-Year Results of a Randomized Clinical Trial. Int. Ophthalmol. 2020, 40, 1147–1154. [Google Scholar] [CrossRef]
- Kanar, H.; Arsan, A.; Altun, A.; Aki, S.; Hacisalihoglu, A. Can Subthreshold Micropulse Yellow Laser Treatment Change the Anti-Vascular Endothelial Growth Factor Algorithm in Diabetic Macular Edema? A Randomized Clinical Trial. Indian J. Ophthalmol. 2020, 68, 145–151. [Google Scholar] [CrossRef]
- Lai, F.H.P.; Chan, R.P.S.; Lai, A.C.H.; Tsang, S.; Woo, T.T.Y.; Lam, R.F.; Yuen, C.Y.F. Comparison of Two-Year Treatment Outcomes between Subthreshold Micropulse (577 Nm) Laser and Aflibercept for Diabetic Macular Edema. Jpn. J. Ophthalmol. 2021, 65, 680–688. [Google Scholar] [CrossRef]
- Koushan, K.; Eshtiaghi, A.; Fung, P.; Berger, A.R.; Chow, D.R. Treatment of Diabetic Macular Edema with Aflibercept and Micropulse Laser (DAM Study). Clin. Ophthalmol. 2022, 16, 1109–1115. [Google Scholar] [CrossRef]
- Toto, L.; D’Aloisio, R.; Quarta, A.; Libertini, D.; D’Onofrio, G.; de Nicola, C.; Romano, A.; Mastropasqua, R. Intravitreal Dexamethasone Implant (IDI) Alone and Combined with Navigated 577 Nm Subthreshold Micropulse Laser (SML) for Diabetic Macular Oedema. J. Clin. Med. 2022, 11, 5200. [Google Scholar] [CrossRef]
- Bonfiglio, V.; Rejdak, R.; Nowomiejska, K.; Zweifel, S.A.; Justus Wiest, M.R.; Romano, G.L.; Bucolo, C.; Gozzo, L.; Castellino, N.; Patane, C.; et al. Efficacy and Safety of Subthreshold Micropulse Yellow Laser for Persistent Diabetic Macular Edema After Vitrectomy: A Pilot Study. Front. Pharmacol. 2022, 13, 832448. [Google Scholar] [CrossRef]
- Chen, G.; Tzekov, R.; Li, W.; Jiang, F.; Mao, S.; Tong, Y. Subthreshold Micropulse Diode Laser Versus Conventional Laser Photocoagulation for Diabetic Macular Edema: A Meta-Analysis of Randomized Controlled Trials. Retina 2016, 36, 2059–2065. [Google Scholar] [CrossRef] [PubMed]
- Qiao, G.; Guo, H.K.; Dai, Y.; Wang, X.L.; Meng, Q.L.; Li, H.; Chen, X.H.; Chen, Z.L. Sub-Threshold Micro-Pulse Diode Laser Treatment in Diabetic Macular Edema: A Meta-Analysis of Randomized Controlled Trials. Int. J. Ophthalmol. 2016, 9, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Ai, P.; Ai, Z.; Xu, G. Subthreshold Diode Micropulse Laser versus Conventional Laser Photocoagulation Monotherapy or Combined with Anti-VEGF Therapy for Diabetic Macular Edema: A Bayesian Network Meta-Analysis. Biomed. Pharmacother. 2018, 97, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Gawęcki, M. Subthreshold Diode Micropulse Laser Combined with Intravitreal Therapy for Macular Edema—A Systematized Review and Critical Approach. J. Clin. Med. 2021, 10, 1394. [Google Scholar] [CrossRef]
- Blindbæk, S.L.; Peto, T.; Grauslund, J. How Do We Evaluate the Role of Focal/Grid Photocoagulation in the Treatment of Diabetic Macular Edema? Acta Ophthalmol. 2019, 97, 339–346. [Google Scholar] [CrossRef]
| Date of search | June 2022–November 2022 |
| Databases searched | PubMed Mendeley |
| Target items | Journal papers |
| Years covered by search | 2010–2022 |
| Language | English |
| Search terms used | (subthreshold laser OR micropulse laser) NOT transscleral AND (diabetic macular edema OR clinically significant macular edema) AND (anti-VEGF OR intravitreal steroid OR vitrectomy) AND (conventional photocoagulation OR ETDRS photocoagulation OR continuous-wave photocoagulation) AND combined therapy AND safety |
| Article | Design | Evaluated on | Results |
|---|---|---|---|
| Clinical Study | |||
| Ohkoshi et al., 2010 [25] | Interventional case series 810 nm MPLT 125–200 μm/200 ms/15% DC titrated to 2–3× CWL power | 8 eyes CS-DME; 1 eye BRVO | Dark spots in SLO (retro mode) were observed with a higher laser energy and could be related to the swelling of RPE. No laser scars on color fundus images and FAF. |
| Luttrull et al., 2012 [26] | Retrospective 810 nm MPLT computer modeling of tissue temperature 125 μm/300 ms/5% DC fixed 950 mW | 212 eyes DME; 40 eyes BRVO FU = 12 | The risk of thermal retinal damage was low and could be eliminated by 5% DC. Significant decreases in CRT and maximum macular thickness. |
| Vujosevic et al., 2015 [27] | Prospective, randomized 577 nm (100 μm/200 ms/5% DC/fixed 250 mW) vs. 810 nm (125 μm/200 ms/5% DC/fixed 750 mW) MPLT | 53 eyes untreated CI-DME ≤ 400 μm FU = 6 | No visible scars on FA and FAF in both groups. No statistically differences in CRT, BCVA, and microperimetry in both groups. Statistically improved macular sensitivity in both groups. |
| Wells-Gray et al., 2018 [28] | Observational 577 nm MPLT Evaluation of the integrity of cones 200 μm/200 ms/5% DC fixed 400 mW, 7 × 7 pattern | 4 eyes non-CI-DME | No signs of structural photoreceptors damage in adaptive optics imaging. |
| Midena et al., 2019 [29] | Prospective 577 nm MPLT AH concentration of RPE biomarkers 200 ms/5% DC/fixed 250 mW | 18 eyes naïve DME ≤ 400 μm; 10 healthy eyes FU = 12 | Significant difference in RPE biomarkers concentration in DME and healthy patients. No significant influence of MLPT on biomarkers. |
| Midena et al., 2019 [30] | Prospective 577 nm MPLT AH concentration of 58 inflammatory biomarkers 200 ms/5% DC/fixed 250 mW | 18 eyes naïve DME ≤ 400 μm; 10 healthy eyes FU = 12 | Significant decrease in proinflammatory cytokines produced by microglial cells after MPLT. |
| Chang et al., 2020 [31] | 577 nm vs. 810 nm MPLT Mathematical analysis of the kinetics of HSP activation Vujosevic et al. [27] laser parameters | n/a | Both lasers were equally effective. The 810 nm laser had a significantly wider safety margin. |
| Midena et al., 2020 [32] | Prospective 577 nm MPLT AH concentration of Müller cells biomarkers 200 ms/5% DC/fixed 250 mW | 10 eyes naïve DME ≤ 400 μm; 12 healthy eyes FU = 12 | Significant reduction in concentration of VEGF and Müller cell activation markers in AH after MPLT. Significantly higher level of biomarkers in AH in patients with DME. |
| Shiraya et al., 2022 [33] | 577 nm MPLT Transcriptome analysis using RNA sequencing MPLT vs. conventional 100 μm/200 ms/5% DC 100–300 mW, 5 × 5 pattern | Human pluripotent stem cell-derived RPE cells FU = 24 h | MPLT induced the expression of HSP and differentially expressed genes related to photoreceptors. |
| Animal study | |||
| Yu et al., 2013 [34] | Prospective 532 nm (130 μm/200 ms) vs. 810 nm (195 μm/300 ms) MPLT titrated to 1× CWL power DC = 5%, 10%, 20%, 40% | 14 rabbits FU = 1 | No significant differences in histologic changes and protein expression between 532 and 810 nm laser. Lower DCs were more selective and caused less retinal photocoagulation |
| De Cilla et al., 2019 [35] | Prospective 810 nm Changes in apoptotic proteins expression 500 μm/75 ms/5% DC titrated to 2× CWL power | 20 young mice and 20 old mice one treatment (n = 20) and three treatments (n = 20) FU = 6 | MPLT modulated balance between oxidant and antioxidant in retina; regulated activation of apoptosis and autophagia. |
| Hirabayashi et al., 2022 [36] | Prospective 577 nm MPLT RT-PCR analysis of retinal samples of the expression of aquaporin subtypes and angiogenesis-related factors 50 μm/150 ms/5% DC/fixed 50 mW | Mice Threshold (n = 6) MPLT (n = 6) control (n = 6) FU = 3 days | Elevated aquaporin 3 expression in MPLT in compared to control group. |
| Article | Design | Evaluated on | Results |
|---|---|---|---|
| Nakamura et al., 2010 [38] | Prospective 810 nm MPLT 200 μm/200 ms/15% DC titrated to 2× CWL power, without papillomacular bundle | 28 eyes diffuse DME FU = 3 | Significant improvement in BCVA; significant reduction in CRT (from 481 ± 110 to 388 ± 127 μm). Central retinal sensitivity did not improve significantly. |
| Ohkoshi et al., 2010 [53] | Prospective 810 nm MPLT 200 μm/200–300 ms/15% DC titrated to 2× CWL power | 43 eyes CS-DME < 600 μm FU = 3 | BCVA did not change significantly. Significant reduction in CRT (from 341.8 ± 119.0 to 289.5 ± 122.8 μm). |
| Takatsuna et al., 2011 [52] | Retrospective 810 nm MPLT 200 μm/100 ms/15% DC titrated to 2× CWL power | 56 eyes DME FU = 12 | BCVA did not change significantly. Significant reduction in CRT (from 504.3 ± 105.8 to 320.4 ± 134.9 μm). |
| Luttrull et al., 2014 [14] | Retrospective 810 nm MPLT 125–200 μm/300 ms/5% DC fixed 780 mW or 950 mW | 39 eyes CI-DME, V > 20/40 FU = 12 | Significant improvement in BCVA (logMAR from 0.19 ± 0.11 to 0.16 ± 0.09); significant reduction in CRT for eyes with CRT < 300 μm (from 248.3 ± 27.8 to 229.4 ± 34.3 μm). No evidence of MPLT injury to RPE. |
| Kwon et al., 2014 [51] | Retrospective 577 nm MPLT 100 μm/20 ms/15% DC titrated to immediately below CWL power 3 × 3 pattern, 1.5 widths | 14 eyes DME > 260 μm FU = 8 | Significant improvement of BCVA (logMAR from 0.51 ± 0.42 to 0.40 ± 0.35). Nonsignificant decrease in CRT. No laser scars detected in color photographs, FAF, IR, and FA. |
| Mansouri et al., 2014 [50] | Retrospective 810 nm MPLT CRT ≤ 400 μm vs. CRT > 400 μm 125 μm/300 ms/5% DC fixed 950 mW | 63 eyes DME FU = 12 | Significant reduction in CRT and gain in BCVA in patients with CRT ≤ 400 μm, stable CRT and BCVA in patients with CRT > 400 μm. No adverse effect from MPLT. |
| Nicolò et al., 2014 [49] | Retrospective 577 nm MPLT Naïve vs. previously treated DME 200 μm/200 ms/5% DC fixed 200 mW | 22 eyes DME FU = 6 | Significant improvement in BCVA (logMAR from 0.39 ± 0.19 to 0.27 ± 0.17) and CRT (from 350.9 ± 74.7 to 311.2 ± 49.43 μm) only in naïve patients. No evidence of RPE damage in FAF. |
| Inagaki et al., 2015 [18] | Prospective 810 nm MPLT + 561 nm focal laser of microaneurysms vs. 577 nm MPLT + 577 nm focal laser of microaneurysms 200 μm/200 ms/15% DC titrated to 2× CWL power, up to 500 μm from fovea | 53 eyes CS-DME FU = 12 | Similar significant reduction in CRT on both groups. Stable BCVA in both groups. Retreatment rate higher in 810 nm group (16.7% vs. 3.4%). Mean power lower in 577 nm group (204.1 vs. 954.1 mW). |
| Abouhussein et al., 2016 [48] | Prospective 577 nm MPLT previously treated 200 μm/200 ms/5% DC fixed 400 mW | 20 eyes CI-DME ≤ 400 μm FU = 6 | Significant improvement in BCVA (logMAR from 0.42 ± 0.15 to 0.3 ± 0.26), significant reduction in CRT (from 354.3 ± 32.96 to 310.7 ± 52.62 μm). No evidence of retinal scars in fundus photography or FA. |
| Latalska et al., 2017 [47] | Prospective 577 nm MPLT Rural vs. urban patients 100 μm/20 ms/5% DC titrated to 2× CWL power | 75 eyes Diffuse DME FU = 6 | More significant treatment effects in rural patients. Significant improvement of reading visual acuity and decrease in CRT in both groups. BVCA remained stable. No retinal damage. |
| Değirmenci et al., 2018 [54] | Retrospective 577 nm MPLT 160 μm/200 ms/5% DC titrated to 0.5× visible MPLT power | 9 eyes non-FI-DME FU = 3 | Significant decrease in mean retinal thickness (from 470.6 to 416 μm). Nonsignificant improvement of BCVA. No evidence of laser scars in FAF. |
| Vesela et al., 2018 [46] | Retrospective 577 nm MLPT 160 μm/200 ms/5% DC titrated to 0.3–0.5× CWL power | 63 eyes DME FU = 12 | Significant decrease in CRT (from 442 to 379 μm). Stabilization of BCVA. |
| Citirik et al., 2019 [56] | Prospective 577 nm MPLT CRT 250–300 μm vs. 301–400 μm vs. > 400 μm vs. healthy control 160 μm/200 ms/5% DC titrated to 0.5× visible MPLT power | 80 eyes recurrent DME after injection FU = 6 | Significant reduction in CRT (from 276.0 ± 22.44 to 238.57 ± 25.87 μm) and gain in BCVA (logMAR from 0.52 ± 0.05 to 0.38 ± 0.04) only in patients with pretreatment CRT ≤ 300 μm. |
| Vujosevic et al., 2020 [44,45] | Prospective 577 nm MLPT vs. control 100 μm/200 ms/5% DC fixed 250 mW, 7 × 7 pattern | 52 eyes naïve DME ≤ 400 μm FU = 12 | Significant increase in BCVA (ETDRS score from 69.4 ± 12.0 to 76.0 ± 9.1). Significantly decrease in hyper-reflective retinal spots, microaneurysms, DRIL. CRT did not change. Stable parameters in control group. No need for rescue treatment. No changes in FAF. |
| Donati et al., 2021 [16] | Retrospective 577 nm MPLT fixed vs. variable treatment regimen 100 μm/200 ms/5% DC fixed 450 mW or titrated to 4× CWL power | 39 eyes DME < 400 μm FU = 12 | Equally significant decrease in CRT in both groups. No significant improvement in BCVA in both groups. |
| Frizziero et al., 2021 [57] | Retrospective 577 nm MPLT 100 μm/200 ms/5% DC/fixed 250 mW | 134 eyes naïve CI-DME CRT ≤ 400 μm FU = 12 | Significant improvement in BCVA (EDTRS score from 77.3 ± 4.5 to 79.4 ± 4.4). No significant CRT reduction. No adverse effects in FAF and OCT. |
| Kikushima et al., 2021 [19] | Retrospective 577 nm vs. 670 nm MPLT 200 μm/200 ms/10% DC titrated to immediately below CWL power | 43 eyes DME FU = 1 | Both lasers maintained BCVA. CRT equally significantly decreased in both groups. No changes in FAF. |
| Nowacka et al., 2021 [58] | Prospective 577 nm MPLT 5% DC, titrated, not exceeding 350 mW | 21 eyes CI-DME CRT < 400 μm FU = 6 | No significant change in BCVA, CRT, bioelectrical function of cones, and bipolar cells in mfERG. |
| Passos et al., 2021 [42] | Retrospective 577 nm MPLT 160 μm/200 ms/5% DC titrated to 0.5× CWL power | 56 eyes CI-DME FU = 3 | Significant improvement in BCVA (logMAR from 0.59 ± 0.32 to 0.43 ± 0.25). Different OCT instruments disabled CRT analysis. |
| Ueda et al., 2021 [40] | Prospective 577 nm MPLT Evaluation of the dynamics of retinal healing process 100 μm/200 ms/5% DC titrated to 0.5× CWL power, 7 × 7 pattern | 11 eyes DME FU = 6 | Decrease in RPE entropy after MPLT on polarization-sensitive OCT. No visible signs in color photography, FAF, and OCT. No significant changes in BCVA and CRT. |
| Valera-Cornejo et al., 2021 [41] | Prospective 577 nm MPLT naïve vs. previously treated DME 100–150 μm/200 ms/5% DC titrated to 0.5× CWL power, 8 × 8 pattern | 33 eyes CI-DME < 700 μm FU = 3 | No significant changes in BCVA for both groups. Significant reduction in CRT (from 420 ± 121 to 390 ± 130 μm) in naïve group. No adverse events in color photographs and FAF. |
| Işık et al., 2022 [39] | Retrospective 577 nm MPLT MPLT vs. healthy control 160 μm/200 ms/5% DC titrated to 0.5× visible MPLT power | 40 eyes CI-DME FU = 3 | Significant increase in BCVA; significant decrease in CRT. Area of central RPE measured in EDI-OCT was smaller in patients requiring retreatment. |
| Marashi et al., 2022 [59] | Retrospective 532 nm focal threshold laser of microaneurysms + 532 nm grid MPLT 125 μm/200 ms/5% DC titrated to 0.5× CWL power | 12 eyes DME CRT > 300 μm FU = 6 | Significant reduction in CRT (from 336.58 ± 86.36 to 264.33 ± 61.41 μm). Stable BCVA. Minimal scar formation. Four eyes required anti-VEGF injection. |
| Article | Design | Evaluated on | Results |
|---|---|---|---|
| Vujosevic et al., 2010 [61] | Prospective, randomized 810 nm MPLT (125 μm/200 ms/5% DC/fixed 750 mW) vs. 514 nm mETDRS photocoagulation (100 μm/100 ms/80–100 mW) | 62 eyes naïve CI-DME CRT ≥ 250 μm FU = 12 | Stable BCVA in both groups. Similarly significant decrease in CRT in both groups. Significant increase in central 12° retinal sensitivity in MPLT group and significant decrease in ETDRS group. Mean no. of treatment 2.03 ± 0.75 in MPLT vs. 2.1 ± 1 in mETDRS. |
| Lavinsky et al., 2011 [62] | Prospective, randomized, double-masked 810 nm ND-MPLT vs. 810 nm HD-MPLT (125 μm/300 ms/15% DC/titrated to 1.2× CWL power) vs. 532 nm mETDRS photocoagulation (75 μm/50 ms/barely visible) | 123 patients naïve CS-DME CRT ≥ 250 μm FU = 12 | Best improvement in BCVA in HD-MPLT group (logMAR 0.25); stable BCVA in ND-MPLT group. Significant progressive reduction in CRT in all groups; greatest in HD-MPLT group (154 μm). No statistical differences in BCVA and CRT in HD-MPLT and mETDRS group. No retreatment in 49% HD-MPLT, 44% mETDRS, and 2% ND-MPLT. |
| Venkatesh et al., 2011 [63] | Prospective, randomized 810 nm MPLT (125 μm/2000 ms/5% DC/titrated to 0.5× CWL power) vs. 532 nm conventional laser (50–100 μm/100 ms/90–180 mW) | 46 eyes CS-DME CRT < 400 μm FU = 6 | Stable BCVA, macular sensitivity, and contrast sensitivity in both groups. Similarly significant decrease in CRT in both groups. More regions with functional loss in mfERG detected after conventional laser. |
| Inagaki et al., 2012 [64] | Retrospective, case-series Grid photocoagulation 810 nm MPLT (200 μm/200 ms/15% DC, titrated to 2–3× CWL power) vs. multicolor (532, 561, or 569 nm) laser (100 μm, 100 ms, 50–100 mW) vs. 532 nm pattern scanning laser (100 μm, 20 ms, 120–320 mW) | 30 eyes CS-DME (n = 15) BRVO (n = 15) FU = 6 | No damage was identified after MPLT in OCT scans; fewer changes in outer retina after pattern scanning laser than after conventional laser. |
| Xie et al., 2013 [65] | Prospective, randomized 810 nm MPLT (125 μm/300 ms/5% DC, titrated to 0.5× visible MPLT power) vs. argon ion conventional laser | 99 eyes DME FU = 6 | Stable BCVA and significant decrease in CRT in both groups. No significant differences in BCVA and CRT between groups. |
| Othman et al., 2014 [66] | Prospective 810 nm MPLT (75–125 μm/15% DC/800–1000 mW) Primary treatment vs. secondary treatment after argon laser photocoagulation | 220 eyes CS-DME CRT > 210 μm FU = 14 ± 2.8 | Stable BCVA in both groups. Significant decrease in CRT in both groups. In primary treatment, 11.37% of eyes and 33% of them in secondary treatment required intravitreal triamcinolone; 3.2% of them in primary group required vitrectomy due to poor response. |
| Fazel et al., 2016 [67] | Prospective, randomized, single-blind 810 nm MPLT (75–125 μm/0.3 ms/15% DC/1000 mJ) vs. 810 nm focal + grid conventional laser | 68 eyes naïve CS-DME CRT 300–450 μm FU = 4 | Significant improvement in BCVA only in MPLT group. Significant decrease in CRT in both groups; more significant in MPLT group. |
| Chhablani et al., 2018 [68] | Prospective, randomized, double-masked 577 nm 5% DC vs. 577 nm 15% DC (100 μm/100 ms/titrated to 0.3× visible MPLT power) vs. 532 nm navigated mETDRS photocoagulation. | 30 eyes naïve non-CI-DME CRT < 350 μm FU = 3 | Stable BCVA and CRT in all groups. Significant reduction in retinal sensitivity in conventional group; similarly significant increase in 5% DC and 15% DC groups. |
| Bougatsou et al., 2020 [69] | Prospective, randomized 532 nm MPLT (50–100 μm/100 ms/15% DC/titrated to 2× CWL power) vs. 532 nm focal photocoagulation | 60 eyes non-CI-CS-DME naïve FU = 6 | Significantly reduced CRT in both groups; significantly better in MPLT group. Significant improvement in BCVA in MLPT group. |
| Al-Barki et al., 2021 [70] | Prospective short-pulse subthreshold 532 nm vs. micropulse 810 nm | 116 eyes CI-DME FU = 6 | Visual acuity significantly improved in MLPT group. Comparable anatomic results and need for rescue therapy in both groups. |
| Lois et al., 2022 [71,72] | Prospective, randomized, double-masked DIAMONDS trial 577 nm MPLT (125 μm/300 ms, 15% DC, titrated to 1× CWL power) vs. mETDRS photocoagulation | 266 eyes CI-DME CRT 301–399 μm FU = 24 | No difference in BCVA, CRT, or 10-2 visual field; need for additional rescue treatment. No. of laser treatments was higher in MPLT group (2.37 vs. 1.89). |
| Article | Design | Evaluated on | Results |
|---|---|---|---|
| Inagaki et al., 2019 [75] | Retrospective ranibizumab or aflibercept + 577 nm MPLT 100 μm/200 ms/5% DC titrated to 0.5–0.6× CWL power | 34 eyes DME FU = 12 | Significant improvement in BCVA (logMAR from 0.52 ± 0.34 to 0.43 ± 0.33). Significant decrease in CRT (from 491.1 to 354.8 μm). Mean no. of injections 3.6 ± 2.1. |
| Akkaya et al., 2020 [76] | Retrospective ranibizumab or aflibercept vs. 577 nm MPLT 100 μm/200 ms/10% DC titrated to 0.5× CWL power | 76 eyes CI-DMI ≤ 350 μm BCVA > 0.7 Snellen FU = 12 | BVCA significantly better in laser group (logMAR 0.054 ± 0.07 vs. 0.095 ± 0.08). The decrease in CRT was non-significant, but it was higher in laser group. Mean no. of injections 5.85 ± 1.38; mean no. of laser treatments 3.64 ± 0.76. |
| Bevacizumab | |||
| Akhlaghi et al., 2019 [77] | Prospective, randomized bevacizumab + 532 nm MPLT vs. bevacizumab 200 μm/5% DC titrated to 4× CWL power | 42 eyes refractory DME FU = 3 | Significant improvement in BCVA (logMAR 0.81 ± 0.33 to 0.62 ± 0.26) and significant decrease in CRT (from 513 ± 126.29 to 408.1 ± 95.28 μm) only in combination group. |
| Altınel et al., 2021 [78] | Retrospective bevacizumab + 577 nm MPLT vs. bevacizumab 160 μm/200 ms/5% DC titrated to 0.5 × visible MPLT power | 80 eyes CI-DME FU = 12 | Significant increase in BVCA in combined group. Significant decrease in CRT, which was similar in both groups. Mean no. of injections significantly lower in combined group (4.38 ± 0.81 vs. 5.65 ± 1.51). |
| El Matri et al., 2021 [79] | Retrospective bevacizumab + 577 nm MPLT vs. bevacizumab 200 μm/200 ms/5% DC fixed 400 mW, 2 × 2 or 4 × 4 pattern | 98 eyes naïve CI-DME ≤ 500 μm FU = 12 | Significant improvement in BCVA (logMAR from 0.692 ± 0.35 to 0.501 ± 0.37) and decrease in CRT (from 479.1 ± 14.3 to 289.6 ± 15) in combined group. The difference is not significant between groups. Significantly lower no. of injections in combined group (4.1 ± 1.5 vs. 7.2 ± 1.3) per year. |
| Ranibizumab | |||
| Moisseiev et al., 2018 [80] | Retrospective 577 nm MPLT vs. ranibizumab 200 μm/200 ms/5% DC/fixed 400 mW | 38 eyes DME FU = 12 | Comparable improvement in BCVA. Change in CRT greater in ranibizumab group. Significantly fewer injections required in MPLT group (1.7 ± 2.3 vs. 5.6 ± 2.1). |
| Abdelrahman et al., 2020 [81] | Prospective, randomized 532 nm MPLT vs. ranibizumab vs. control 200 μm/200 ms/5% DC fixed 400 mW, 7 × 7 pattern | 120 eyes naïve DME CRT ≤ 400 μm FU = 6 | Significant improvement in BCVA (93% vs. 31%) and decrease in CRT (34.66% vs. 11.69%) in both groups; significantly higher in ranibizumab group. Significant improvement in mfERG only in ranibizumab group. |
| Furashova et al., 2020 [82] | Prospective, randomized ReCaLL clinical trial 810 nm MPLT 200 ms/15% DC titrated to 2× CWL power, without fovea | 17 eyes DME CRT > 300 μm FU = 12 | Significant increase in BCVA with significant decrease in CRT in both groups. No significant differences between groups. Significantly lower no. of injections in combined group (7.5 vs. 9). |
| Bıçak et al., 2022 [83] | Retrospective ranibizumab + 577 nm MPLT vs. ranibizumab 165 μm/200 ms/5% DC titrated to 0.5× visible MPLT power, grid pattern | 97 eyes DME CRT ≤ 350 μm FU = 9 | Significant increase in BCVA in both groups with significant decrease in CRT. No significant differences between groups. Significantly lower no. of injections in combined group (4.19 ± 1.01 vs. 5.53 ± 1.14). |
| Mi et al., 2022 [84] | Prospective, randomized, double-blind ranibizumab + sham 577 nm MPLT vs. sham ranibizumab + 577 nm MPLT 200 μm/200 ms/5% DC fixed 400 mW, 7 × 7 pattern | 72 patients DME CRT > 300 μm | This study is currently recruiting participants. The results are not yet available. |
| Aflibercept | |||
| Khattab et al., 2019 [85] | Prospective, randomized aflibercept + 577 nm MPLT vs. aflibercept 200 μm/200 ms/5% DC fixed 400 mW, 7 × 7 pattern | 54 eyes DME CRT > 250 μm FU = 18 | Significant increase in BCVA and contrast sensitivity; significant decrease in CRT in both groups. No significant differences between groups. Significantly lower no. of injections in combined group (4.1 ± 1.1 vs. 7.3 ± 1.1). |
| Abouhussein et al., 2020 [86] | Prospective, randomized aflibercept + 577 nm MPLT vs. aflibercept 200 μm/200 ms/5% DC fixed 400 mW, 5 × 5 pattern | 40 eyes naïve DME CRT > 300 μm FU = 12 | Significant increase in BCVA and significant decrease in CRT in both groups. No significant differences between groups. Significantly lower no. of injections in combined group (4.5 ± 1.4 vs. 5.4 ± 1.7) after the loading dose of aflibercept. |
| Kanar et al., 2020 [87] | Prospective, randomized aflibercept + 577 nm MPLT vs. aflibercept 160 μm/200 ms/5% DC titrated to 0.5× visible MPLT power | 56 eyes naïve DME CRT > 300 μm FU = 12 | Significant increase in BCVA and significant decrease in CRT in both groups. No significant differences between groups. Significantly lower no. of injections in combined group (3.21 ± 0.41 vs. 5.39 ± 1.54). |
| Lai et al., 2021 [88] | Retrospective 577 nm MPLT + focal laser of microaneurysms vs. aflibercept 200 μm/200 ms/5% DC fixed 400 mW, 5 × 5 pattern, 0.25 spacing | 164 eyes DME CRT > 300 μm FU = 24 | Significant increase in BCVA and significant decrease in CRT in both groups. Significantly greater improvement in BCVA at 6 months, as well as in CTR at 6 and 12 months in aflibercept group; no significant differences between groups at 12 and 24 months. Rescue aflibercept required in 24% of MLPT eyes. |
| Koushan et al., 2022 [89] | Prospective, randomized, single-blind DAM Study aflibercept + 532 nm MPLT vs. aflibercept + sham 532 nm MPLT 200 μm/200 ms/10% DC titrated to 0.9× visible MPLT power, 3 × 3 pattern | 30 eyes CI-DME CRT ≥ 315 μm FU = 12 | Significant increase in BCVA and significant decrease in CRT in both groups. No significant differences between groups. Similar no. of injections in both groups. |
| Dexamethasone | |||
| Elhamid 2017 [9] | Prospective 577 nm MPLT + IDI 200 μm/200 ms/5% DC fixed 400 mW, 7 × 7 pattern | 20 eyes refractory CI-DME CRT ≥ 300 μm FU = 12 | Significant improvement in BCVA (Snellen from 0.45 ± 0.14 to 0.6 ± 0.1) and significant decrease in CRT (from 420.7 ± 38.74 to 285.2 ± 14.99 μm). Retreatment was performed in 40% of eyes. |
| Toto et al., 2022 [90] | Prospective 577 nm navigated MPLT + IDI vs. IDI 100 μm/100 ms/5% DC titrated to 0.3× visible MPLT power | 60 eyes naïve CI-DME CRT > 300 μm FU = 6 | Significant improvement in BCVA and decrease in CRT in both groups; significantly higher in MPLT+ IDI group. Significantly higher no. of second injections in IDI group (73.3% vs. 56.7% of patients). Shorter time before the second injection in IDI group (83.5 vs. 137.4 days). |
| Vitrectomy | |||
| Bonfiglio et al., 2022 [91] | Prospective PPV+ 577 nm MPLT vs. PPV 200 μm/200 ms/5% DC titrated to 2× CWL power, 7 × 7 pattern | 95 eyes Persistent DME CRT ≥ 300 μm FU = 6 | Significant improvement in BCVA (EDTRS letters from 51.54 ± 13.81 to 57.83 ± 13.95) and decrease in CRT (from 410.59 ± 129.91 to 283.39 ± 73.45 μm) in MPLT group. Second MPLT required in 67% of eyes. Parafoveal VD significantly higher and FAZ significantly smaller in OCTA in MPLT group. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sabal, B.; Teper, S.; Wylęgała, E. Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review. J. Clin. Med. 2023, 12, 274. https://doi.org/10.3390/jcm12010274
Sabal B, Teper S, Wylęgała E. Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review. Journal of Clinical Medicine. 2023; 12(1):274. https://doi.org/10.3390/jcm12010274
Chicago/Turabian StyleSabal, Barbara, Sławomir Teper, and Edward Wylęgała. 2023. "Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review" Journal of Clinical Medicine 12, no. 1: 274. https://doi.org/10.3390/jcm12010274
APA StyleSabal, B., Teper, S., & Wylęgała, E. (2023). Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review. Journal of Clinical Medicine, 12(1), 274. https://doi.org/10.3390/jcm12010274






