Abstract
Left main (LM) percutaneous coronary interventions (PCI) are challenging and highly invasive procedures. Periprocedural myocardial injury (Troponin (Tn) elevation > 99th percentile) is frequently detected after LM PCI, being identified even in up to 67% of patients. However, the prognostic implications of periprocedural Tn elevation after LM PCI remain controversial. We aim to assess the impact and prognostic significance of the periprocedural troponin elevation on long-term outcomes in patients undergoing LM PCI in a real-world setting. Consecutive 673 patients who underwent LM PCI in our department between January 2015 to February 2021 were included in a prospective registry. The first group consisted of 323 patients with major cardiac Troponin I elevation defined as an elevation of Tn values > 5× the 99th percentile in patients with normal baseline values or post-procedure Tn rise by >20% in patients with elevated pre-procedure Tn in whom the Tn level was stable or falling (based on the fourth universal definition of myocardial infarction). The second group consisted of patients without major cardiac Troponin I elevation. Seven-year long-term all-cause mortality was not higher in the group with major Tn elevation (36.9% vs. 40.6%; p = 0.818). Naturally, periprocedural myocardial infarction was diagnosed only in patients from groups with major Tn elevation (4.9% of all patients). In-hospital death and other periprocedural complications did not differ significantly between the two study groups. The adjusted HRs for mortality post-PCI in patients with a periprocedural myocardial infarction were not significant. Long-term mortality subanalysis for the group with criteria for cardiac procedural myocardial injury showed no significant differences (39.5% vs. 38.8%; p = 0.997). The occurrence of Tn elevation (>1×; >5×; >35× and >70× URL) after LM PCI was not associated with adverse long-term outcomes. The results of the study suggest that the isolated periprocedural troponin elevation is not clinically significant.
1. Introduction
The left main coronary artery (LM) is crucial for maintaining blood flow to most of the left ventricular (LV) myocardium, therefore significant LM narrowing puts this cohort at great risk [1,2]. Decisions regarding the choice of the revascularization method i.e., percutaneous coronary interventions (PCI) vs. coronary artery bypass graft (CABG) remain in the heart team’s tasks and are individualized for each patient. Advances in PCI, such as adequate patient selection, development in device technology, stenting techniques, enhanced interventional cardiologist experience, and modern post-procedure therapy, have made PCI a safe and efficient alternative to CABG surgery for LM coronary artery disease [3,4,5]. Despite the great efficiency and high safety, it should be emphasized that LM PCI are challenging and highly invasive procedure. Periprocedural myocardial injury (Troponin (Tn) > 99th percentile) is frequently discovered after LM PCI, being recognized even up to 67% of patients using a standard Tn assay [6].
Myocardial infarction (MI) is a frequently utilized endpoint in cardiology scientific studies, indicating irreversible myocardial necrosis mostly due to acute myocardial ischemia [7]. There are various types of MI with different mechanisms involved. Periprocedural myocardial infarction (PMI) refers to MI that arises during PCI or CABG. Interventional cardiologists, under the patronage of the Society for Cardiac Angiography and Intervention (SCAI), generally concurred on a definition of a clinically significant MI based on an increase of creatine kinase-myocardial band (CK-MB) >10 times or troponin >70 times the upper limit of normal (ULN) as an independent criterion [8]. Nevertheless, upon consideration, the specialists developing the latest Fourth Universal Definition of MI (UDMI) have decided to preserve the previous (Third UDMI) definition. Fourth UDMI defines percutaneous coronary intervention-related MI (MI type 4a) as an elevation of cardiac troponin (Tn) values more than five times the 99th percentile upper reference limit (URL) in patients with normal baseline values [9]. In patients with elevated pre-procedure Tn in whom the Tn level is stable (≤20% variation) or falling, the post-procedure Tn must rise by >20% [9]. However, the absolute post-procedural value must still be at least five times the 99th percentile ULN [9]. The prognostic implications of significant periprocedural Tn elevation after percutaneous coronary intervention are still controversial [10,11]. In addition, a lower troponin elevation (>5 times the 99th percentile) in PCI compared to CABG (>10× ULN) is required to diagnose peri-operative myocardial infarction [9]. No established agreement amongst cardiology societies and scientific groups has led to a variety of definitions with different cardiac biomarkers (CK-MB or Tn), deliberations on whether the multiplicity of ULN should change after PCI or CABG, and whether clinical characteristics such as electrocardiogram changes, new artery occlusions, new regional wall kinetic abnormalities, or loss of viable myocardium should be considered [4,8,9,12,13,14,15,16,17,18]. Most importantly, the influence of PMIs definition on mortality is various. Since an appropriate definition of PMI has not been established, and patients’ survival differs depending on the different definitions used, perhaps PMI should be removed from primary composite endpoints [19]. Therefore, the optimal PMI definition and the consequences of this selection on the results should be further explored. A summary of all PMI definitions is provided in Table 1.

Table 1.
Periprocedural myocardial infarction definitions.
We aim to assess the impact and prognostic significance of the periprocedural troponin elevation on long-term results in patients undergoing LM PCI in a real-world setting.
2. Materials and Methods
This manuscript is a part of a series of scientific articles on LM disease. The design of the registry has been previously reported [20,21,22]. In brief, subsequent 673 LM PCI patients from the period between January 2015–February 2021 were included in the study. Patients with significant LM stenosis (≥50% diameter) engaging or not the ostial narrowing of the left anterior descending artery (LAD), circumflex coronary artery (LCx), or both were enrolled in the study. Moderate lesions were assessed with the use of intravascular ultrasound imaging (IVUS) (minimal lumen area of 6.0 mm for LM). Terminal patients (life expectancy below one year) were eliminated from the further analysis. All PCI interventions were performed by an experienced invasive cardiologist after the heart team sat with a cardiac surgeon.
LM patients were categorized into two groups. The first group was composed of 323 patients with major cardiac Troponin I elevation defined as an elevation of Tn values more than 5 times the 99th percentile URL in patients with normal baseline values or post-procedure Tn rise by >20% in patients with elevated pre-procedure Tn in whom the Tn level was stable or falling (however, the absolute post-procedural value still needs to be at least 5 times the 99th percentile URL). Tn elevation cut-off values were determined based on the criteria for PCI-associated MI ≤ 48 h after the PCI procedure (MI type 4a) from the most recent Fourth UDMI [9]. Patients at our facility had Troponin I levels measured prior to and after the PCI intervention as part of the routine clinical management. The second group consisted of patients without major cardiac Troponin I elevation (Figure 1).
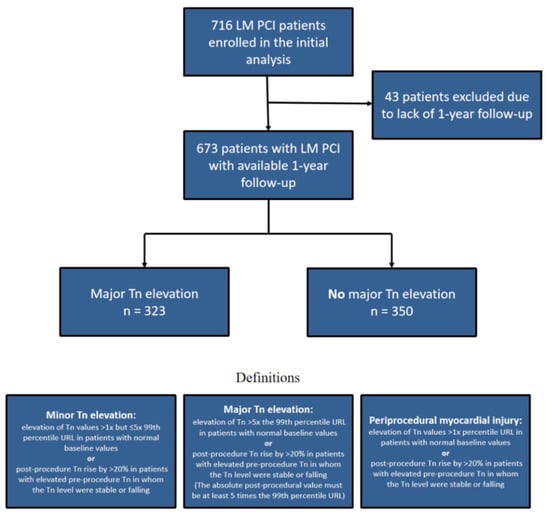
Figure 1.
Flowchart presenting population size and definitions.
Baseline clinical and angiographic characteristics, procedural information, in-hospital and follow-up outcome data were examined. Contrast-induced nephropathy was determined as the deterioration of kidney function, depicted as either a 25% or ≥0.5 mg/dL (44 μmol/L) serum creatinine elevation from baseline level within 48 h [23]. Chronic kidney disease was determined using the Cockcroft–Gault equation [24]. All coronary artery bifurcations were categorized using the Medina classification [25]. In-hospital death, in-hospital MI, and long-term all-cause death were established as a primary outcome. Secondary outcome of the study was Tn analysis according to various cutoffs of postprocedural Troponin levels.
Periprocedural MI type 4a diagnosis, in addition to Tn elevation, required proof of new myocardial ischaemia (i.e., new ECG abnormalities, cardiac imaging evidence, or PCI complications associated with reduction in coronary artery blood flow [9]. IVUS or optical coherence tomography (OCT) methods were used in 31.9% of patients and were not investigated thoroughly in this paper. The mean and median follow-up for the cohort were respectively 1385 and 1411 days (interquartile range: 938 days, max: 2553 days). Survival analysis data were gathered by telephone contact or with the use of National Health Fund documentation.
All analyses were performed with STATISTICA 13.7 (StatSoft, Inc., Tulsa, OK, USA). Continuous variables were shown as means ± SD or medians (IQR). Categorical variables were summarized as counts or percentages and were compared between groups using the test for proportions. The normality distribution was analyzed using the Shapiro–Wilk test. Differences between continuous variables were tested with Student’s t-test or nonparametric Mann-Whitney test. The survival probability at follow-up was calculated using the Kaplan–Meier method. Log-rank tests were used to compare survival between the different groups. A two-sided p < 0.05 was considered statistically significant.
3. Results
A total of 673 consecutive LM PCI patients (mean age: 68.8 ± 9.2 years, 76.4% males) were divided into two groups according to cardiac Troponin I elevation as defined above. The first group was composed of 323 patients with major cardiac Troponin I elevation and the second group consisted of patients without major cardiac Troponin I elevation. Patients’ baseline clinical characteristics are presented in Table 2. There were no significant differences in the incidence of major cardiovascular risk factors. On admission, stable coronary artery disease was found in a smaller percentage in the group with major Tn elevation (51.7% vs. 62.3%; p = 0.006), the tendency towards the higher occurrence of unstable CAD (27.2% vs. 21.4%; p = 0.078) and NSTEMI (17.0% vs. 12.3%; p = 0.081) was visible. Prior PCI LAD was found to be more frequent in groups without Tn elevation (19.5% vs. 26.6%; p = 0.030). Left ventricular ejection fraction (LVEF) (49.1 ± 11.4% vs. 50.4 ± 11.3%; p = 0.150) and left ventricular end-diastolic diameter (LVEDD) (52.0 ± 7.1 mm vs. 51.1 ± 7.3 mm; p = 0.151) was similar in both groups.

Table 2.
Baseline characteristics by treatment group.
Baseline angiographic characteristics are shown in Table 3. Localization of the LM lesions was similar in both groups. Not-ostial LAD (57.6% vs. 50.3%; p = 0.058) and LCX (41.5% vs. 34.6%; p = 0.065) lesions were found more often in groups with major Tn elevation, however, this difference was not significant. The trend toward a higher frequency of LM plus two-vessel disease (30.7% vs. 24.9%; p = 0.093) and LM plus three-vessel disease (14.2% vs. 10.0%; p = 0.091) was observed. There was no significant difference in the frequency of Medina bifurcation types between both groups. Syntax Score was significantly higher in patients with major Tn elevation (26.2 ± 10.2 vs. 24.3 ± 9.9; p = 0.011). The EuroScore II value was non-significantly higher in Group with Tn elevation (2.35 ± 1.99 vs. 2.24 ± 1.83; p = 0.788).

Table 3.
Baseline angiographic characteristics.
Procedural characteristics are presented in Table 4. A procedure success ratio was high in both patient fractions. The number of stents (1.9 ± 0.9 vs. 1.7 ± 0.8; p < 0.001) and the total length (45.1 ± 24.9 mm vs. 37.5 ± 21.8 mm; p < 0.001) were notably higher in the group with major Tn elevation. Periprocedural fluoroscopy time did not differ significantly, however, a dose of radiation was significantly higher in the group with Tn elevation (1500 ± 896 vs. 1317 ± 822; p = 0.010). Artery access did not differ in both groups, and radial access was used more frequently. Only second-generation drug-eluting stents were used in this study. All stenting techniques are summarized in Table 4. Two-stent techniques were performed more frequently in groups with major Tn elevation (27.2% vs. 19.4%; p = 0.016). The crushing technique constituted 38.5% of two-stent techniques.

Table 4.
Procedural characteristics.
Procedural clinical results are summarized at the end of Table 4. Naturally, PMI type 4a was diagnosed only in patients from group with major Tn elevation (4.9% of all patients). Contrast induced nephropathy was found more frequently in the group with major Tn elevation (5.6% vs. 3.1%; p = 0.121), but the difference was not significant. Frequency of other periprocedural complications were on the similar levels in two groups. There was no significant difference in the seven-year long-term all-cause mortality between groups with and without major Tn elevation (36.9% vs. 40.6%; p = 0.818) (Figure 2).
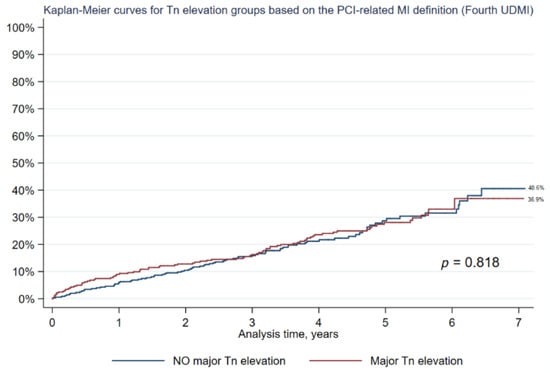
Figure 2.
Kaplan-Meier analysis of all-cause mortality: major Tn elevation vs. NO major Tn elevation (based on PCI-related myocardial infarction definition from the fourth universal definition of myocardial infarction).
3.1. Subanalysis: Patients with Periprocedural Myocardial Infarction
At seven years, the adjusted HRs for mortality after LM PCI in patients with a periprocedural myocardial infarction were not significant (21.2% vs. 25.5%; HR: 0.833; 95% CI: 0.426 to 1.629; p = 0.593).
3.2. Subanalysis: Patients with Criteria for Cardiac Procedural Myocardial Injury
In a subanalysis, we decided to examine the criteria for cardiac procedural myocardial injury. Cardiac procedural myocardial injury is arbitrarily defined by increases in Tn values (>99th percentile URL) in patients with normal baseline values (≤99th percentile URL) or a rise of Tn values > 20% of the baseline value when it is above the 99th percentile URL but it is stable or falling [9]. In terms of troponin elevation, the difference is that the criteria for cardiac procedural myocardial injury elevation do not require a five-fold increase compared to the 99th percentile URL (in comparison to periprocedural MI criteria). In our group, the criteria for cardiac procedural myocardial injury were met in 56.0% of patients. Long-term mortality in that subanalysis showed no significant differences (39.5% vs. 38.8%; p = 0.997) between the groups (Figure 3).
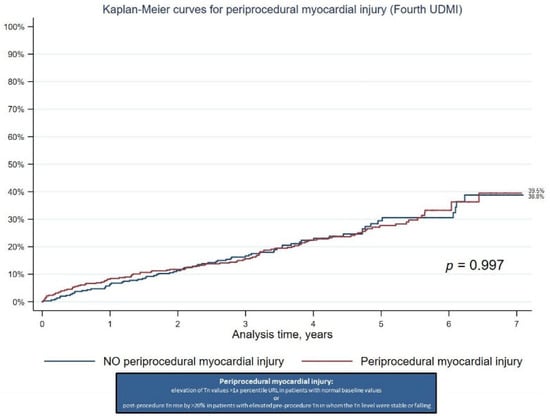
Figure 3.
Kaplan-Meier analysis of all-cause mortality: Periprocedural myocardial injury vs. NO periprocedural myocardial injury (Fourth Universal Definition of Myocardial Infarction).
3.3. Subanalysis: Different Postprocedural Troponin Levels Cutoffs
Moreover, the graph presenting Kaplan-Meier curves for all-cause death according to different cutoffs of postprocedural Tn levels is provided. There is no significant difference in long-term mortality although the highest mortality in patients with >70× Tn elevation is visible (49.5%; p = 0.142) (Figure 4).
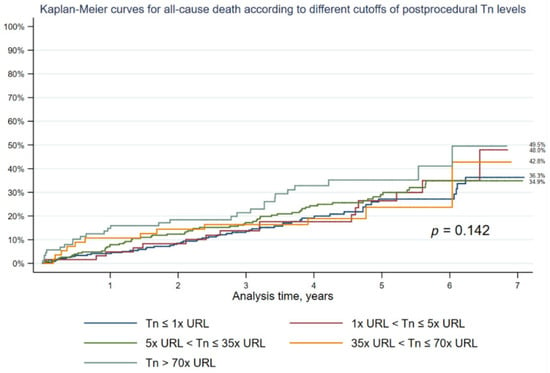
Figure 4.
Kaplan-Meier curves for all-cause mortality according to different cutoffs of postprocedural Troponin levels.
3.4. Subanalysis: Different Postprocedural CK-MB Mass Levels Cutoffs
Forty-eight percent (323 patients) of patients from our group had CK-MB mass levels measured before and after the LM PCI procedure. Additionally, we decided to investigate the association of CK-MB mass with long-term all-cause mortality in a subanalysis. The Kaplan-Meier curves for all-cause mortality according to different cutoffs of postprocedural CK-MB levels are provided. There is no significant difference in long-term mortality (p = 0.560) (Figure 5).
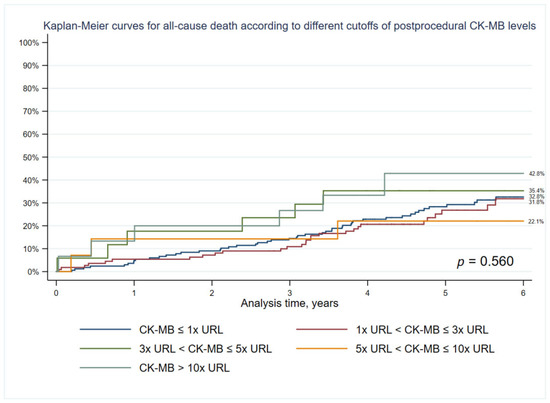
Figure 5.
Kaplan-Meier curves for all-cause mortality according to different cutoffs of postprocedural CK-MB mass levels.
4. Discussion
Clinically relevant PMI should be determined as those leading to major cardiovascular events, especially death. Periprocedural myocardial injury is frequently detected after LM PCI, recognized in the present study in over 50% of patients using a standard Tn assay. Nevertheless, the threshold for post-PCI biomarker elevations representing clinically significant periprocedural myocardial injury in LM PCI patients remains controversial. In recent years, this topic has been gaining more and more attention [6,26].
To the best of our knowledge, based on the literature review, this is the first paper to compare the groups of patients with significant Tn I elevation after LM PCI with patients without post-procedure Tn I elevation in a real-world setting. The aim of the present study was to assess the impact and prognostic significance of the periprocedural troponin elevation on long-term outcomes in patients undergoing PCI of LM CAD.
In this paper, groups were created based on Tn elevation values more than five times the 99th percentile URL in patients with normal baseline values or post-procedure Tn rise by >20% in patients with elevated pre-procedure Tn. These categories were used as the basal groups in tables, because these criteria are believed to have the greatest clinical implications and are used in clinical practice more often than the criteria for cardiac procedural myocardial injury. The main findings of this real-life large study examining the prognostic implications of periprocedural myocardial injury and troponin elevations in more than 600 consecutive patients undergoing LM PCI is that the (1) occurrence of Tn elevation (>1× URL (minor); >5× URL (major); >35× URL and >70× URL) after LM PCI is not associated with adverse long-term outcomes and does not affect the prognosis, (2) LM PCI is an invasive procedure and the troponin increase occurs in more than 50% of PCI LM patients population, (3) PMI according to fourth UDMI following LM PCI are not associated with an increase in all-cause mortality at seven years, (4) a subanalysis of 323 patients showed that the occurrence of CK-MB elevation (>1× URL; >3× URL; >5× URL and >10× URL) after LM PCI is also not associated with adverse long-term outcomes.
Whether isolated elevation of Troponin level after PCI delivers long-term prognostic information data about mortality is an important issue. Circulating troponin after PCI composed of two groups: a pre-PCI or baseline fraction and a fraction that corresponds to PCI-associated Tn increase. Continuous microscopic cardiomyocyte loss during everyday life and cardiomyocyte renewal are two processes that contribute to physiological baseline circulating troponin levels [27,28]. The articles describing the effects of post-PCI biomarkers elevation on major adverse cardiac effects and mortality differ in terms of the biomarkers assessed, their influence, and cut-off values [29,30,31,32,33]. Some of these articles stated that the Tn elevation was not associated with increased mortality and did not offer prognostic data beyond that provided by the baseline level of the biomarker [18,34,35]. Therefore, the significance of change and factors that predispose to an elevation of post-PCI Tn levels after LM PCI remain unclear.
Recent analysis from the EXCEL trial stated that both peak CK-MB ≥ 10× URL and Tn ≥ 70× URL were independently predictive of five-year all-cause and cardiovascular mortality [14,26]. In the Excel study, confusion is associated with the PMI definition: PMI by study protocol definition correlates with increased 5-year all-cause and cardiovascular mortality after PCI and CABG, but the fourth UDMI definition PMI is related only to increased mortality in the CABG group [14]. Similar results were obtained, in the SYNTAX where CK-MB ≥ 10× URL post-PCI was related to 30-day and a 10-year increase in all-cause mortality, SYNTAX trial did not report troponin levels analysis [13]. In the study by Hao-Yu et al., only post-procedural CK-MB levels elevations: ≥3× and ≥10× URL independently predicted increased 3-year cardiovascular and all-cause mortality, whereas different Tn I cutoff levels did not show such correlations [6]. Moreover, only the SCAI definition of PMI (but not ARC-2 and Fourth UDMI) was associated with higher cardiovascular (HR: 4.93; 95% CI: 1.92–12.69) and all-cause (HR: 3.11; 95% CI: 1.33–7.27) mortality after LM PCI [6]. The influence of differing definitions of PMI was also investigated in the ISCHEMIA study, wherein a primary definition used CK-MB and a second one used Tn. PMIs were not related to all-cause death (HR: 1.14 [95% CI: 0.42–3.08] and 1.06 [95% CI: 0.56–2.02]) or cardiovascular death (HR: 1.99 [95% CI: 0.73–5.43] and 1.24 [95% CI: 0.57–2.68]) using either definition [16], ISCHEMIA had a median follow-up of 3.2 years.
In our study, unlike most of the trials above, none of the Tn elevation cutoffs was related to the increase in the seven-year all-cause mortality (p = 0.142). An identical situation, with no effect on long-term death rates, occurs in terms of CK-MB elevations (p = 0.560). Moreover, the adjusted HRs for the seven-year all-cause mortality post-PCI in patients with a PMI by Fourth UDMI were not significant (HR: 0.833; 95% CI: 0.426 to 1.629; p = 0.593). PMI type 4a in our study was found in 4.9% of all patients, these results are in line with other real-world LM studies, in the DELTA 2 registry PMI was diagnosed in 4.0% of patients who underwent LM PCI [36]. It should be noted that the Tn elevation by Fourth UDMI for PMI was met in 48% of patients and the criteria for periprocedural myocardial injury in 56% of the patients. Earlier trials exposed that the three-year mortality in patients with unprotected LM CAD who received drug-only treatment was up to 50% [37,38,39], post-procedure elevation in Tn levels should not come as a surprise after life-saving LM PCI.
In patients with major Tn I elevation Syntax score, a number of implanted stents, radiation time, and radiation dose were higher and two-stent techniques were used more often. Therefore, it can be assumed that the PCI procedures performed on these patients were more complex. However, the procedure success ratio was high and similar in both study groups. It should be emphasized that patients qualified for PCI of LM often have severe comorbidities that disqualify them from CABG. For these patients, LM PCI is the only option, and the question that should be asked is whether it is possible to perform PCI on patients who could potentially undergo CABG without a periprocedural rise in Tn levels. Especially, that diagnosis of CABG-related MI (type 5 MI) requires a greater rise of Tn levels (>10× URL) than PCI-related MI type 4a (>5× URL) [9].
Study Limitations
The presented article analyzes a real-life group of LM PCI interventions. One of the main constraints was the absence of a group that underwent a cardiac surgical procedure. Nevertheless, comparing that group to the coronary artery bypass graft cohort was from the beginning beyond the primary purpose of the analysis. Second, this research was conducted in a world setting, and LM disease is a highly diversified state. Therefore, the localization of the disease (ostial/shaft/bifurcation), the complexity of the coronary lesion, and coronary artery disease in distal branches could impact the results. Third, despite the introduced trial being a prospective registry, not entire clinically significant information was accessible. Next, all-cause mortality was evaluated based on the long-term outcomes, and a cardiovascular vs. non-cardiovascular death rates analysis could not be provided.
5. Conclusions
Elevated troponin concentrations after LM PCI in real-world settings are frequently observed. However, these findings are not associated with an increased risk of in-hospital death and all-cause mortality in a long-term follow-up. The results of the study suggest that the isolated periprocedural troponin elevation is not clinically significant. Moreover, the performed subanalysis implies no clinical significance of CK-MB elevation.
Author Contributions
Conceptualization, W.J.S., M.K.-O., W.S. and M.G.; methodology, W.J.S. and M.K.-O.; validation, M.L. and M.G.; formal analysis, W.J.S. and M.K.-O.; investigation, W.J.S., M.K.-O., P.M., W.S., S.G., M.P., A.A., M.L. and M.G.; resources, M.L.; data curation, W.J.S. and M.K.-O.; writing—original draft preparation, W.J.S. and M.K.-O.; writing—review and editing, M.K.-O. and M.G.; visualization, W.J.S. and M.K.-O.; supervision, M.K.-O. and M.G.; project administration, W.J.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Poznan University of Medical Sciences.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- El-Menyar, A.A.; Al Suwaidi, J.; Holmes, D.R. Left Main Coronary Artery Stenosis: State-of-the-Art. Curr. Probl. Cardiol. 2007, 32, 103–193. [Google Scholar] [CrossRef] [PubMed]
- Fajadet, J.; Capodanno, D.; Stone, G.W. Management of left main disease: An update. Eur. Heart J. 2019, 40, 1454–1466. [Google Scholar] [CrossRef] [PubMed]
- Morice, M.-C.; Serruys, P.W.; Kappetein, A.P.; Feldman, T.E.; Stahle, E.; Colombo, A.; Mack, M.J.; Holmes, D.R.; Torracca, L.; van Es, G.A.; et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation 2010, 121, 2645–2653. [Google Scholar] [PubMed]
- Park, S.-J.; Kim, Y.-H.; Park, D.-W.; Yun, S.-C.; Ahn, J.-M.; Song, H.G.; Lee, J.Y.; Kim, W.J.; Kang, S.J.; Lee, S.W.; et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N. Engl. J. Med. 2011, 364, 1718–1727. [Google Scholar] [CrossRef]
- Park, D.-W.; Ahn, J.-M.; Park, H.; Yun, S.-C.; Kang, D.-Y.; Lee, P.H.; Kim, Y.H.; Lim, D.S.; Rha, S.W.; Park, G.M.; et al. Ten-Year Outcomes After Drug-Eluting Stents Versus Coronary Artery Bypass Grafting for Left Main Coronary Disease: Extended Follow-Up of the PRECOMBAT Trial. Circulation 2020, 141, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.Y.; Xu, B.; Dou, K.; Guan, C.; Song, L.; Huang, Y.; Zhang, R.; Xie, L.; Zhang, M.; Yan, H.; et al. Implications of Periprocedural Myocardial Biomarker Elevations and Commonly Used MI Definitions After Left Main PCI. JACC Cardiovasc. Interv. 2021, 14, 1623–1634. [Google Scholar] [CrossRef] [PubMed]
- Alpert, J.S.; Thygesen, K.; Antman, E.; Bassand, J.P. Myocardial infarction redefined—A consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J. Am. Coll. Cardiol. 2000, 36, 959–969. [Google Scholar] [PubMed]
- Moussa, I.D.; Klein, L.W.; Shah, B.; Mehran, R.; Mack, M.J.; Brilakis, E.S.; Reilly, J.P.; Zoghbi, G.; Holper, E.; Stone, G.W. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: An expert consensus document from the Society for Cardiovascular Angiography and Interventions (SCAI). J. Am. Coll. Cardiol. 2013, 62, 1563–1570. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef]
- Bulluck, H.; Paradies, V.; Barbato, E.; Baumbach, A.; Bøtker, H.E.; Capodanno, D.; De Caterina, R.; Cavallini, C.; Davidson, S.M.; Feldman, D.N.; et al. Prognostically relevant periprocedural myocardial injury and infarction associated with percutaneous coronary interventions: A Consensus Document of the ESC Working Group on Cellular Biology of the Heart and European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur. Heart J. 2021, 42, 2630–2642. [Google Scholar]
- Koskinas, K.C.; Ndrepepa, G.; Räber, L.; Karagiannis, A.; Kufner, S.; Zanchin, T.; Hieber, J.; Hunziker, L.; Mayer, K.; Byrne, R.A.; et al. Prognostic Impact of Periprocedural Myocardial Infarction in Patients Undergoing Elective Percutaneous Coronary Interventions. Circ. Cardiovasc. Interv. 2018, 11, 006752. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, H.M.; McFadden, E.P.; Farb, A.; Mehran, R.; Stone, G.W.; Spertus, J.; Onuma, Y.; Morel, M.A.; van Es, G.A.; Zuckerman, B.; et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Eur. Heart J. 2018, 39, 2192–2207. [Google Scholar] [CrossRef] [PubMed]
- Hara, H.; Serruys, P.W.; Takahashi, K.; Kawashima, H.; Ono, M.; Gao, C.; Wang, R.; Mohr, F.W.; Holmes, D.R.; Davierwala, P.M.; et al. Impact of Peri-Procedural Myocardial Infarction on Outcomes After Revascularization. J. Am. Coll. Cardiol. 2020, 76, 1622–1639. [Google Scholar] [CrossRef] [PubMed]
- Gregson, J.; Stone, G.W.; Ben-Yehuda, O.; Redfors, B.; Kandzari, D.E.; Morice, M.C.; Leon, M.B.; Kosmidou, I.; Lembo, N.J.; Brown, W.M.; et al. Implications of Alternative Definitions of Peri-Procedural Myocardial Infarction After Coronary Revascularization. J. Am. Coll. Cardiol. 2020, 76, 1609–1621. [Google Scholar] [CrossRef]
- Mäkikallio, T.; Holm, N.R.; Lindsay, M.; Spence, M.S.; Erglis, A.; Menown, I.B.; Trovik, T.; Eskola, M.; Romppanen, H.; Kellerth, T.; et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): A prospective, randomised, open-label, non-inferiority trial. Lancet 2016, 388, 2743–2752. [Google Scholar] [CrossRef]
- Chaitman, B.R.; Alexander, K.P.; Cyr, D.D.; Berger, J.S.; Reynolds, H.R.; Bangalore, S.; Boden, W.E.; Lopes, R.D.; Demkow, M.; Piero Perna, G.; et al. Myocardial Infarction in the ISCHEMIA Trial: Impact of Different Definitions on Incidence, Prognosis, and Treatment Comparisons. Circulation 2021, 143, 790–804. [Google Scholar] [CrossRef]
- Cho, M.S.; Ahn, J.M.; Lee, C.H.; Kang, D.Y.; Lee, J.B.; Lee, P.H.; Kang, S.J.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; et al. Differential Rates and Clinical Significance of Periprocedural Myocardial Infarction After Stenting or Bypass Surgery for Multivessel Coronary Disease According to Various Definitions. JACC Cardiovasc. Interv. 2017, 10, 1498–1507. [Google Scholar] [CrossRef]
- Ndrepepa, G.; Colleran, R.; Braun, S.; Cassese, S.; Hieber, J.; Fusaro, M.; Kufner, S.; Ott, I.; Byrne, R.A.; Husser, O.; et al. High-Sensitivity Troponin T and Mortality After Elective Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2016, 68, 2259–2268. [Google Scholar] [CrossRef]
- Cutlip, D.E. Procedural Myocardial Infarction. J. Am. Coll. Cardiol. 2020, 76, 1640–1643. [Google Scholar] [CrossRef]
- Skorupski, W.J.; Grygier, M.; Araszkiewicz, A.; Skorupski, W.; Grajek, S.; Pyda, M.; Siniawski, A.; Mitkowski, P.; Lesiak, M.; Kałużna-Oleksy, M. The impact of right coronary artery support on outcomes of patients with unprotected left main disease undergoing percutaneous coronary intervention. Kardiol. Pol. 2021, 79, 631–637. [Google Scholar] [CrossRef]
- Kałużna-Oleksy, M.; Skorupski, W.J.; Grygier, M.; Araszkiewicz, A.; Skorupski, W.; Grajek, S.; Mitkowski, P.; Pyda, M.; Lesiak, M. A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes? J. Pers. Med. 2021, 11, 581. [Google Scholar] [CrossRef] [PubMed]
- Skorupski, W.J.; Kałużna-Oleksy, M.; Lesiak, M.; Araszkiewicz, A.; Skorupski, W.; Grajek, S.; Mitkowski, P.; Pyda, M.; Grygier, M. Short- and Long-Term Outcomes of Left Main Coronary Artery Stenting in Patients Disqualified from Coronary Artery Bypass Graft Surgery. J. Pers. Med. 2022, 12, 348. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, N.M.A.; Mahfouz, A.; Achkar, K.; Rafie, I.M.; Hajar, R. Contrast-induced Nephropathy. Heart Views 2013, 14, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Siersbæk-Nielsen, K.; Hansen, J.M.; Kampmann, J.; Kristensen, M. Rapid evaluation of creatinine clearance. Lancet 1971, 297, 1133–1134. [Google Scholar] [CrossRef]
- Medina, A.; Suarez de Lezo, J.; Pan, M. A new classification of coronary bifurcation lesions. Rev. Esp. Cardiol. 2006, 59, 183. [Google Scholar] [CrossRef]
- Ben-Yehuda, O.; Chen, S.; Redfors, B.; McAndrew, T.; Crowley, A.; Kosmidou, I.; Kandzari, D.E.; Puskas, J.D.; Morice, M.C.; Taggart, D.P.; et al. Impact of large periprocedural myocardial infarction on mortality after percutaneous coronary intervention and coronary artery bypass grafting for left main disease: An analysis from the EXCEL trial. Eur. Heart J. 2019, 40, 1930–1941. [Google Scholar] [CrossRef]
- Bergmann, O.; Bhardwaj, R.D.; Bernard, S.; Zdunek, S.; Barnabé-Heider, F.; Walsh, S.; Zupicich, J.; Alkass, K.; Buchholz, B.A.; Druid, H.; et al. Evidence for cardiomyocyte renewal in humans. Science 2009, 324, 98–102. [Google Scholar] [CrossRef]
- Olivetti, G.; Giordano, G.; Corradi, D.; Melissari, M.; Lagrasta, C.; Gambert, S.R.; Anversa, P. Gender differences and aging: Effects on the human heart. J. Am. Coll. Cardiol. 1995, 26, 1068–1079. [Google Scholar] [CrossRef]
- Ellis, S.G.; Chew, D.; Chan, A.; Whitlow, P.L.; Schneider, J.P.; Topol, E.J. Death following creatine kinase-MB elevation after coronary intervention: Identification of an early risk period: Importance of creatine kinase-MB level, completeness of revascularization, ventricular function, and probable benefit of statin therapy. Circulation 2002, 106, 1205–1210. [Google Scholar] [CrossRef]
- Kong, T.Q.; Davidson, C.J.; Meyers, S.N.; Tauke, J.T.; Parker, M.A.; Bonow, R.O. Prognostic implication of creatine kinase elevation following elective coronary artery interventions. JAMA 1997, 277, 461–466. [Google Scholar] [CrossRef]
- Abdelmeguid, A.E.; Topol, E.J.; Whitlow, P.L.; Sapp, S.K.; Ellis, S.G. Significance of mild transient release of creatine kinase-MB fraction after percutaneous coronary interventions. Circulation 1996, 94, 1528–1536. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Mehran, R.; Dangas, G.; Lansky, A.J.; Kornowski, R.; Leon, M.B. Differential impact on survival of electrocardiographic Q-wave versus enzymatic myocardial infarction after percutaneous intervention: A device-specific analysis of 7147 patients. Circulation 2001, 104, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Saucedo, J.F.; Mehran, R.; Dangas, G.; Hong, M.K.; Lansky, A.; Kent, K.M.; Satler, L.F.; Pichard, A.D.; Stone, G.W.; Leon, M.B. Long-term clinical events following creatine kinase—Myocardial band isoenzyme elevation after successful coronary stenting. J. Am. Coll. Cardiol. 2000, 35, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.; Rihal, C.S.; Lennon, R.J.; Singh, M.; Jaffe, A.S.; Holmes, D.R.J. Significance of periprocedural myonecrosis on outcomes after percutaneous coronary intervention: An analysis of preintervention and postintervention troponin T levels in 5487 patients. Circ. Cardiovasc. Interv. 2008, 1, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.L.; Garratt, K.N.; Burritt, M.F.; Lennon, R.J.; Reeder, G.S.; Jaffe, A.S. Baseline troponin level: Key to understanding the importance of post-PCI troponin elevations. Eur. Heart J. 2006, 27, 1061–1069. [Google Scholar] [CrossRef]
- Chieffo, A.; Tanaka, A.; Giustino, G.; Briede, I.; Sawaya, F.J.; Daemen, J.; Kawamoto, H.; Meliga, E.; D’Ascenzo, F.; Cerrato, E.; et al. The DELTA 2 Registry. JACC Cardiovasc. Interv. 2017, 10, 2401–2410. [Google Scholar] [CrossRef]
- Conley, M.J.; Ely, R.L.; Kisslo, J.; Lee, K.L.; McNeer, J.F.; Rosati, R.A. The prognostic spectrum of left main stenosis. Circulation 1978, 57, 947–952. [Google Scholar] [CrossRef]
- Herrick, J.B. Clinical features of sudden obstruction of the coronary arteries. J. Am. Med. Assoc. 1912, 59, 2015–2022. [Google Scholar] [CrossRef]
- Favaloro, R.G. Saphenous Vein Autograft Replacement of Severe Segmental Coronary Artery Occlusion: Operative Technique. Ann. Thorac. Surg. 1968, 5, 334–339. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).