Long-Term Survival after Extended Sleeve Lobectomy (ESL) for Central Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis with Reconstructed Time-to-Event Data
Abstract
1. Introduction
2. Materials and Methods
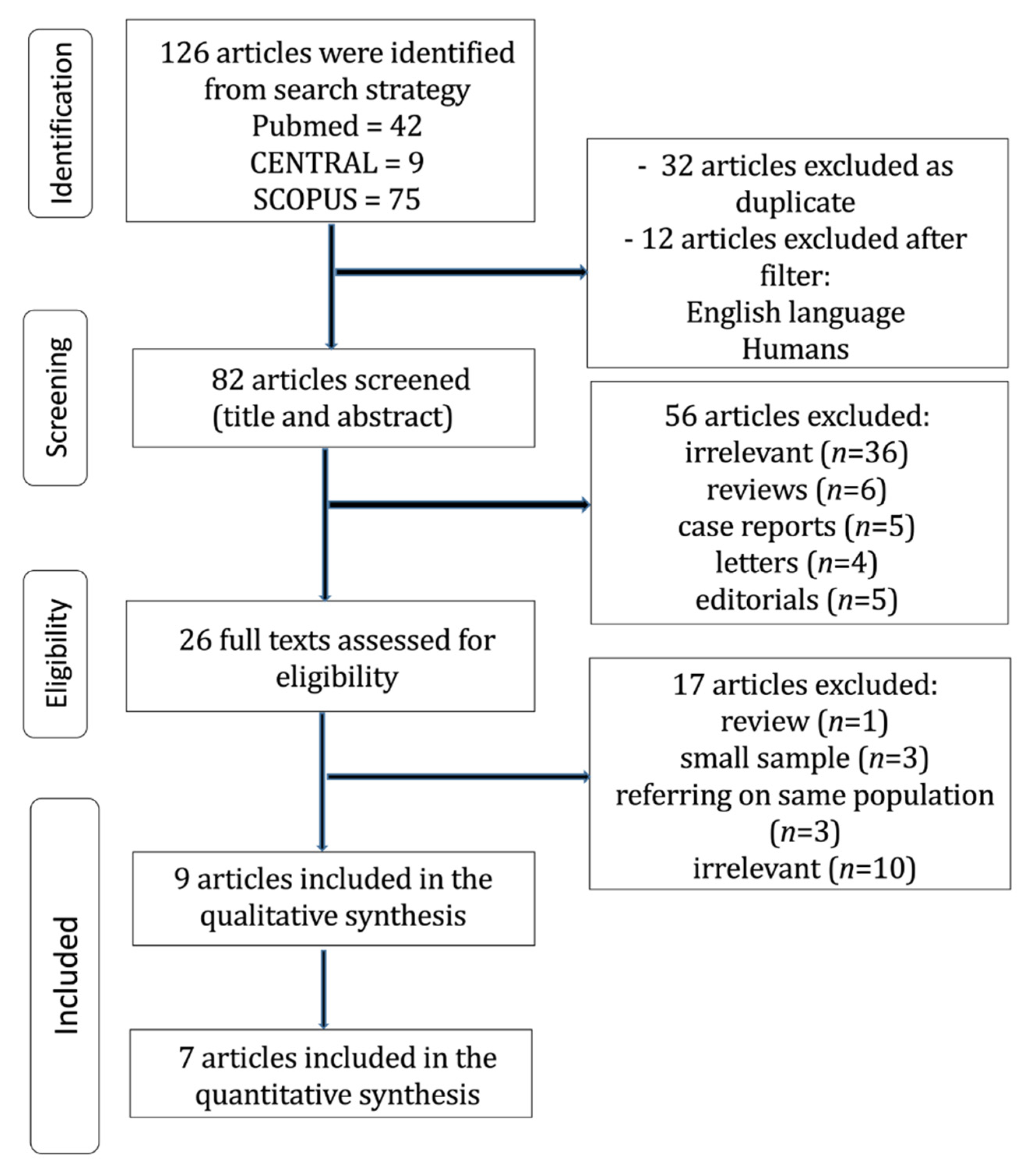
2.1. Search and Articles Selection Strategy
2.2. Data Extraction and Endpoints
2.3. Sensitivity Analysis on Survival Endpoints
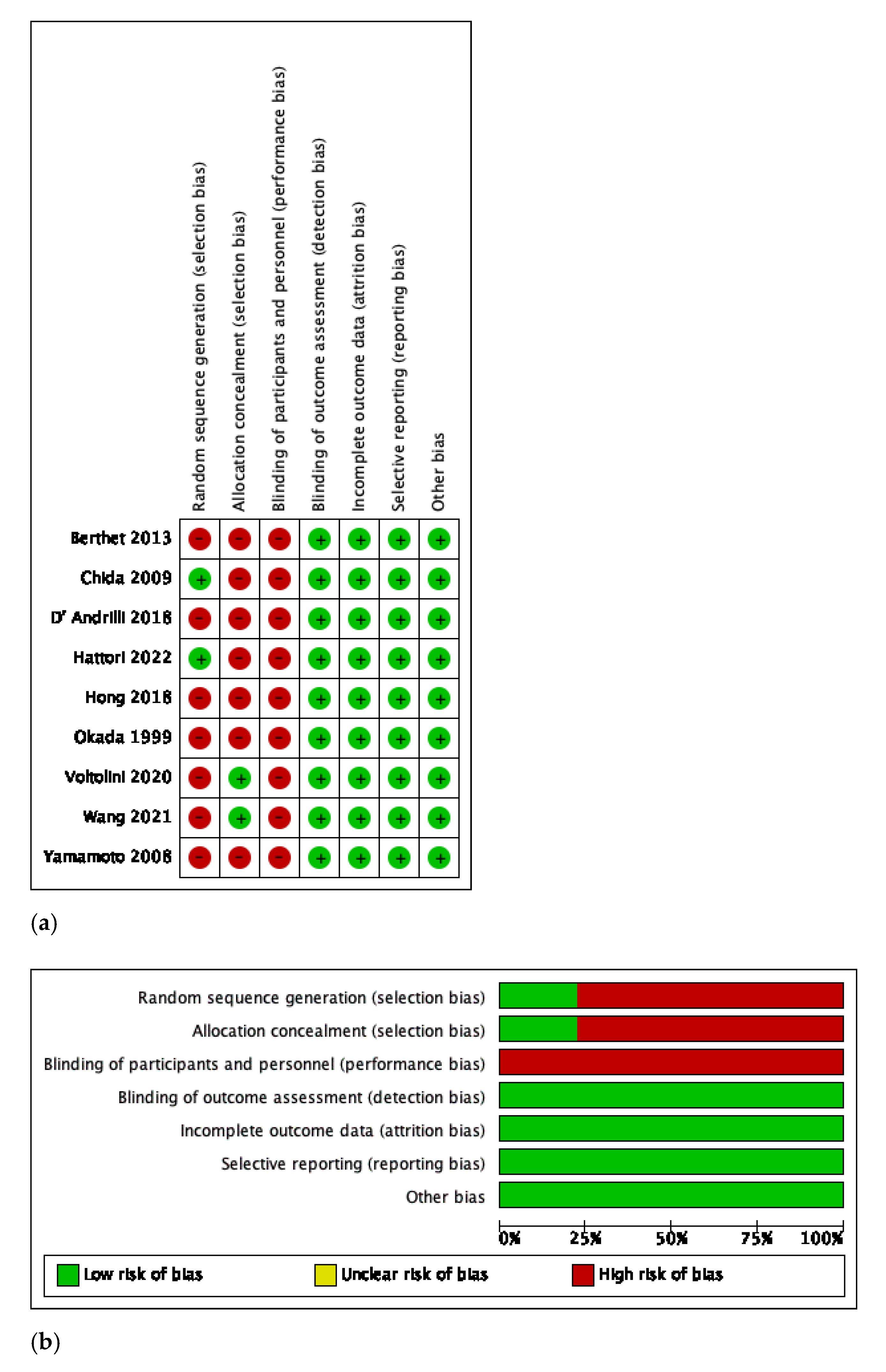
2.4. Quality and Publication Bias Assessment
3. Results
3.1. Search Strategy and Patient Demographics
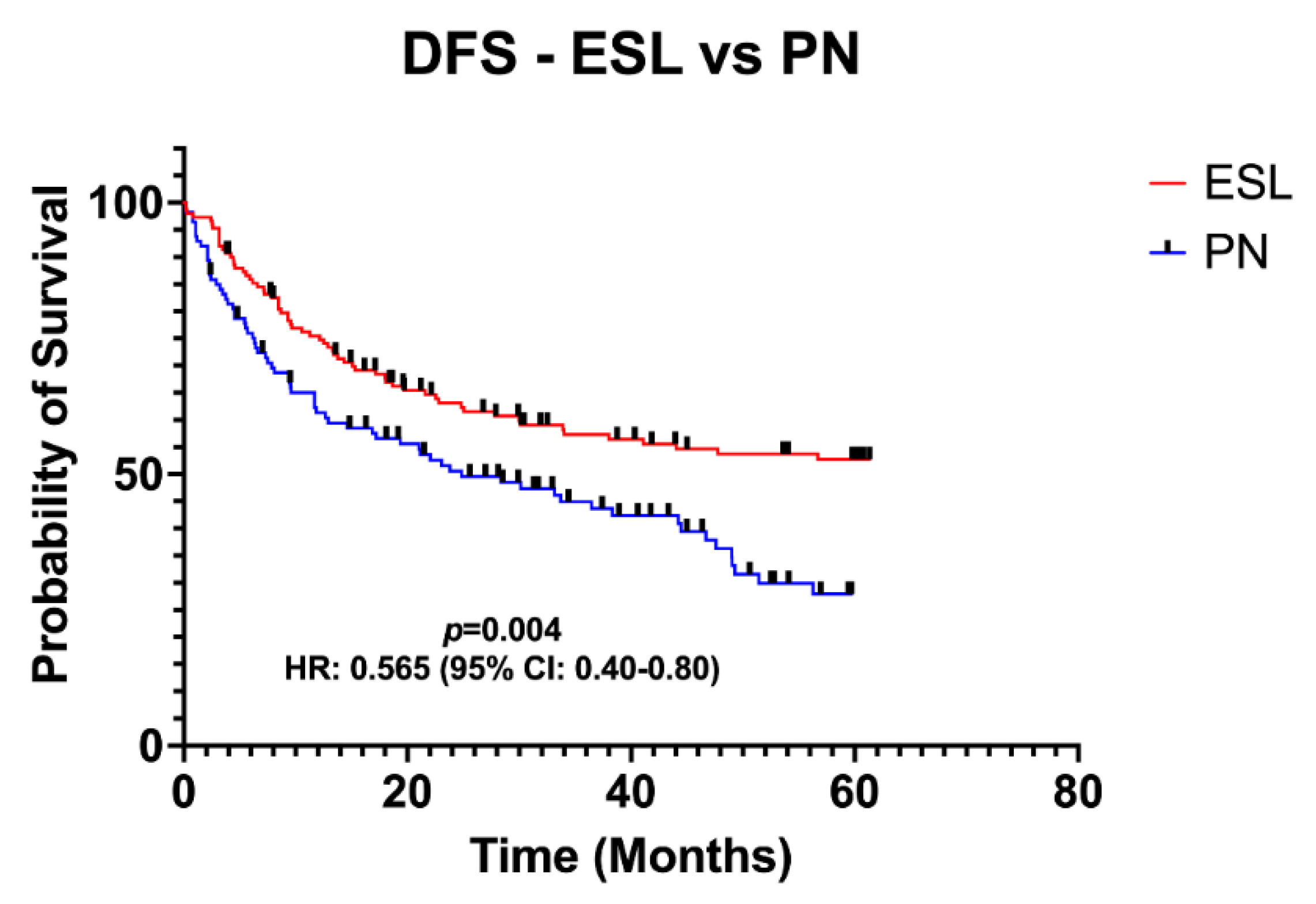
3.2. Primary Endpoints: OS and DFS
3.3. Secondary Endpoints: Complications, Operative Mortality, and Adjuvant Treatment
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Deslauriers, J.; Gregoire, J.; Jacques, L.F.; Piraux, M.; Guojin, L.; Lacasse, Y. Sleeve lobectomy versus pneumonectomy for lung cancer: A comparative analysis of survival and sites or recurrences. Ann. Thorac. Surg. 2004, 77, 1152–1156; discussion 1156. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Caro, A.; Garcia, S.; Reguart, N.; Cladellas, E.; Arguis, P.; Sanchez, M.; Gimferrer, J.M. Determining the appropriate sleeve lobectomy versus pneumonectomy ratio in central non-small cell lung cancer patients: An audit of an aggressive policy of pneumonectomy avoidance. Eur. J. Cardiothorac. Surg. 2011, 39, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Committee for Scientific Affairs; The Japanese Association for Thoracic Surgery; Shimizu, H.; Okada, M.; Toh, Y.; Doki, Y.; Endo, S.; Fukuda, H.; Hirata, Y.; Iwata, H.; et al. Thoracic and cardiovascular surgeries in Japan during 2018: Annual report by the Japanese Association for Thoracic Surgery. Gen. Thorac. Cardiovasc. Surg. 2021, 69, 179–212. [Google Scholar] [PubMed]
- Okada, M.; Tsubota, N.; Yoshimura, M.; Miyamoto, Y.; Matsuoka, H.; Satake, S.; Yamagishi, H. Extended sleeve lobectomy for lung cancer: The avoidance of pneumonectomy. J. Thorac. Cardiovasc. Surg. 1999, 118, 710–713; discussion 713–714. [Google Scholar] [CrossRef] [PubMed]
- Rendina, E.A.; Venuta, F.; de Giacomo, T.; Rossi, M.; Coloni, G.F. Parenchymal sparing operations for bronchogenic carcinoma. Surg. Clin. N. Am. 2002, 82, 589–609. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Zhou, Y.; Lee, J.J. IPD from KM: Reconstruct individual patient data from published Kaplan-Meier survival curves. BMC Med. Res. Methodol. 2021, 21, 111. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hern an, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Berthet, J.P.; Paradela, M.; Jimenez, M.J.; Molins, L.; Gómez-Caro, A. Extended sleeve lobectomy: One more step toward avoiding pneumonectomy in centrally located lung cancer. Ann. Thorac. Surg. 2013, 96, 1988–1997. [Google Scholar] [CrossRef] [PubMed]
- Chida, M.; Minowa, M.; Miyoshi, S.; Kondo, T. Extended sleeve lobectomy for locally advanced lung cancer. Ann. Thorac. Surg. 2009, 87, 900–905. [Google Scholar] [CrossRef] [PubMed]
- D’Andrilli, A.; Maurizi, G.; Ciccone, A.M.; Andreetti, C.; Ibrahim, M.; Menna, C.; Vanni, C.; Venuta, F.; Rendina, E.A. Long-segment pulmonary artery resection to avoid pneumonectomy: Long-term results after prosthetic replacement. Eur. J. Cardiothorac. Surg. 2018, 53, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Hattori, A.; Matsunaga, T.; Fukui, M.; Takamochi, K.; Oh, S.; Suzuki, K. Surgical Outcome After Extended Sleeve Lobectomy in Centrally Located Non-small Cell Lung Cancer. Ann. Thorac. Surg. 2022, 114, 1853–1862. [Google Scholar] [CrossRef] [PubMed]
- Hong, T.H.; Cho, J.H.; Shin, S.; Kim, H.K.; Choi, Y.S.; Zo, J.I.; Shim, Y.M.; Kim, J. Extended sleeve lobectomy for centrally located non-small-cell lung cancer: A 20-year single-centre experience. Eur. J. Cardiothorac. Surg. 2018, 54, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Voltolini, L.; Gonfiotti, A.; Viggiano, D.; Borgianni, S.; Farronato, A.; Bongiolatti, S. Extended sleeve-lobectomy for centrally located locally advanced non-small cell lung cancer is a feasible approach to avoid pneumonectomy. J. Thorac Dis. 2020, 12, 4090–4098. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Jiang, S.; You, X.; Aramini, B.; Shabaturov, L.; Jiang, G.; Zhu, Y.; Fan, J. Extended Sleeve Lobectomy is an Alternative for Centrally Located Lung Cancer with Superior Short- and Long-term Outcomes. Clin. Lung Cancer. 2021, 22, e621–e628. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Miyamoto, Y.; Ohsumi, A.; Kojima, F.; Imanishi, N.; Matsuoka, K.; Ueda, M.; Hamada, C. Sleeve lung resection for lung cancer: Analysis according to the type of procedure. J. Thorac. Cardiovasc. Surg. 2008, 136, 1349–1356. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Waseda, R.; Iwasaki, A. Extended sleeve lobectomy: Its place in surgical therapy for centrally located non-small cell lung cancer and a review of technical aspects. J. Thorac. Dis. 2018, 10 (Suppl. S26), S3103–S3108. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, C.; Stoelben, E. A new classification of bronchial anastomosis after sleeve lobectomy. J. Thorac. Cardiovasc. Surg. 2012, 144, 808–812. [Google Scholar] [CrossRef] [PubMed]

| Study ID, Year | Country | Study Design | Patients, n | Mean Age, y ± SD | Histology, n (%) | Pathologic Stage, n (%) | Neoadjuvant Therapy, n (%) | Type of Procedure, n (%) | Combined Angioplasty, n (%) | Follow-up, m | NOS | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
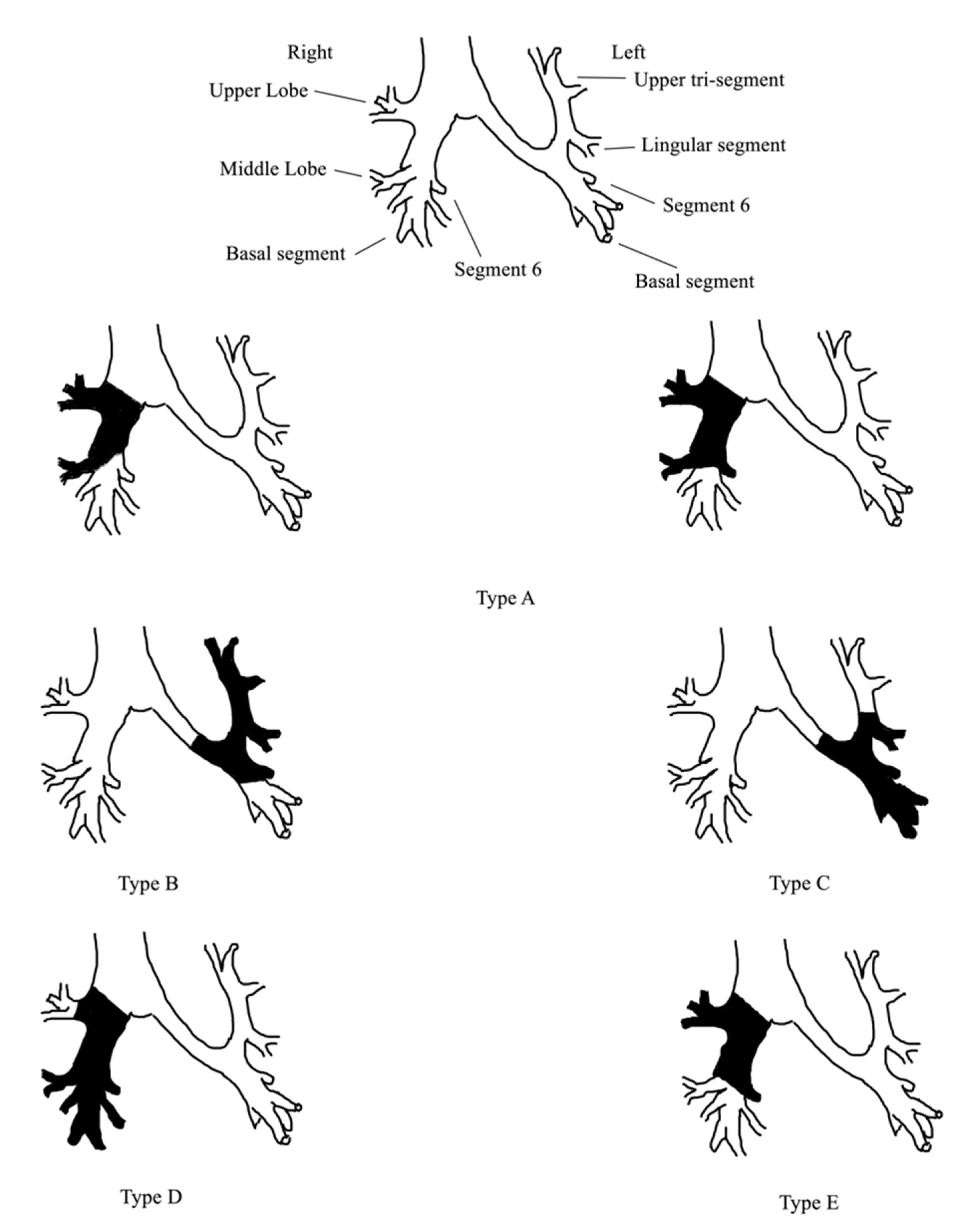
| ESL | PN | ESL | PN | ESL | PN | ESL | PN | ESL | PN | |||||||
| Berthet 2013 [10] | France | P | 27 | - | 62.7 ± 8.2 | - | ADC: 12 (44) SCC: 15 (56) | - | I: 7 (26) II: 14 (52) III: 6 (22) | - | 7 (25.9) | - | A:11 (41), B:7 (26), C:2 (7), D:2 (7), E:5 (19) | 11 (40.7) | 7–69 | 7 |
| Chida 2009 [11] | Japan | R | 23 | 15 | 65.36 ± 7.9 | - | ADC: 4 (17) SCC: 18 (78) O: 1 (5) | - | I: 4 (17) II: 6 (26) III: 13 (57) | NR | 7 (25.9) | - | - | 11 (40.7) | 3–36 | 6 |
| D’ Andrilli 2018 [12] | Italy | P | 24 | - | 60.4 ± 9.8 | - | ADC: 12 (50) SCC: 8 (33) O: 4 (17) | - | I: 7 (29) II: 8 (33) III: 9 (38) | - | 8 (33.3) | - | N/R | N/R | 6–72 | 6 |
| Hattori 2022 [13] | Japan | R | 43 | 76 | 66.5 ± 10.1 | N/R | ADC: 16 (37) SCC: 22 (51) O: 5 (12) | ADC: 21 (28) SCC: 45 (59) O: 10 (13) | I: 1 (2) II: 19 (44) III: 23 (54) | I: 1 (1) II: 25 (33) III: 50 (66) | 5 (12) | 13 (17) | A: 10 (23), B: n=8 (19), C: n=16 (37), D: n=9 (21) | 20 (47) | 6-222 | 6 |
| Hong 2018 [14] | Korea | R | 63 | - | 60 ± 10 | - | ADC: 2 (3) SCC: 54 (86) O: 7 (11) | - | I: 19 (30) II: 30 (48) III: 14 (23) | - | 4 (5.7) | - | A: 14 (22), B: 4 (6), C: 8 (13), D: 37 (59) | 13 (20.6) | 48 | 6 |
| Okada 1999 [4] | Japan | R | 15 | - | 64 ± 6 | - | ADC: 2 (13) SCC: 13 (87) | - | I: 0 (0) II: 9 (60) III: 6 (40) | - | 4 (27) | - | A: 6 (40), B: 4 (27), C: 5 (33) | 8 (53.3) | 9–106 | 6 |
| Voltolini 2020 [15] | Italy | P | 22 | 38 | 68 (51-79) | 67 (51-83) | ADC: 8 (36.4) SCC: 14 (63.6) | N/R | I: 1 (4.5) II: 8 (36.3) III: 13 (59.1) IV: 0 (0) | I: 2 (5.2) II: 12 (31.6) III: 23 (60.5) IV: 1 (2.6) | 7 (31.8) | 12 (31.6) | A: 8 (36), B: 1 (5), C: 13 (59) | 7 (31.8) | 4-57 | 7 |
| Wang 2021 [16] | China-Italy | P | 22 | 43 | 54 ± 10 | 54 ± 9 | SCC: 15 (68) O: 7 (32) | SCC: 31 (72) O: 12 (28) | *N0: 11 (50) N1: 6 (27) N2: 5 (23) | *N0: 22 (51) N1: 13 (30) N2: 8 (19) | 9 (41) | 18 (42) | A: 7 B: 10 C:2 D: 3 | - | 11-58 | 7 |
| Yamamoto 2008 [17] | Japan | R | 20 | - | N/R | - | N/R | - | N/R | - | N/R | - | A: 2 (10), B: 8 (40), C: 7 (35), E: 3 (15) | 9 (45) | 13–113 | 5 |
| Complications | Number of Patients (259) n, (%) |
|---|---|
| Sputum retention | 12 (4.6) |
| Pneumonia | 20 (7.7) |
| Prolonged air leakage | 19 (7.3) |
| Chylothorax | 2 (0.8) |
| AF | 16 (6.2) |
| BPF | 12 (4.6) |
| Stricture | 8 (3.1) |
| PVT | 4 (1.5) |
| Reoperation | 4 (1.5) |
| Operative mortality | 3 (1.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magouliotis, D.E.; Zotos, P.-A.; Karamolegkou, A.P.; Tatsios, E.; Spiliopoulos, K.; Athanasiou, T. Long-Term Survival after Extended Sleeve Lobectomy (ESL) for Central Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis with Reconstructed Time-to-Event Data. J. Clin. Med. 2023, 12, 204. https://doi.org/10.3390/jcm12010204
Magouliotis DE, Zotos P-A, Karamolegkou AP, Tatsios E, Spiliopoulos K, Athanasiou T. Long-Term Survival after Extended Sleeve Lobectomy (ESL) for Central Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis with Reconstructed Time-to-Event Data. Journal of Clinical Medicine. 2023; 12(1):204. https://doi.org/10.3390/jcm12010204
Chicago/Turabian StyleMagouliotis, Dimitrios E., Prokopis-Andreas Zotos, Anna P. Karamolegkou, Evangelos Tatsios, Kyriakos Spiliopoulos, and Thanos Athanasiou. 2023. "Long-Term Survival after Extended Sleeve Lobectomy (ESL) for Central Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis with Reconstructed Time-to-Event Data" Journal of Clinical Medicine 12, no. 1: 204. https://doi.org/10.3390/jcm12010204
APA StyleMagouliotis, D. E., Zotos, P.-A., Karamolegkou, A. P., Tatsios, E., Spiliopoulos, K., & Athanasiou, T. (2023). Long-Term Survival after Extended Sleeve Lobectomy (ESL) for Central Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis with Reconstructed Time-to-Event Data. Journal of Clinical Medicine, 12(1), 204. https://doi.org/10.3390/jcm12010204








