Reliability of Endolymphatic Hydrops Qualitative Assessment in Magnetic Resonance Imaging
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
2.2. Study Group Description
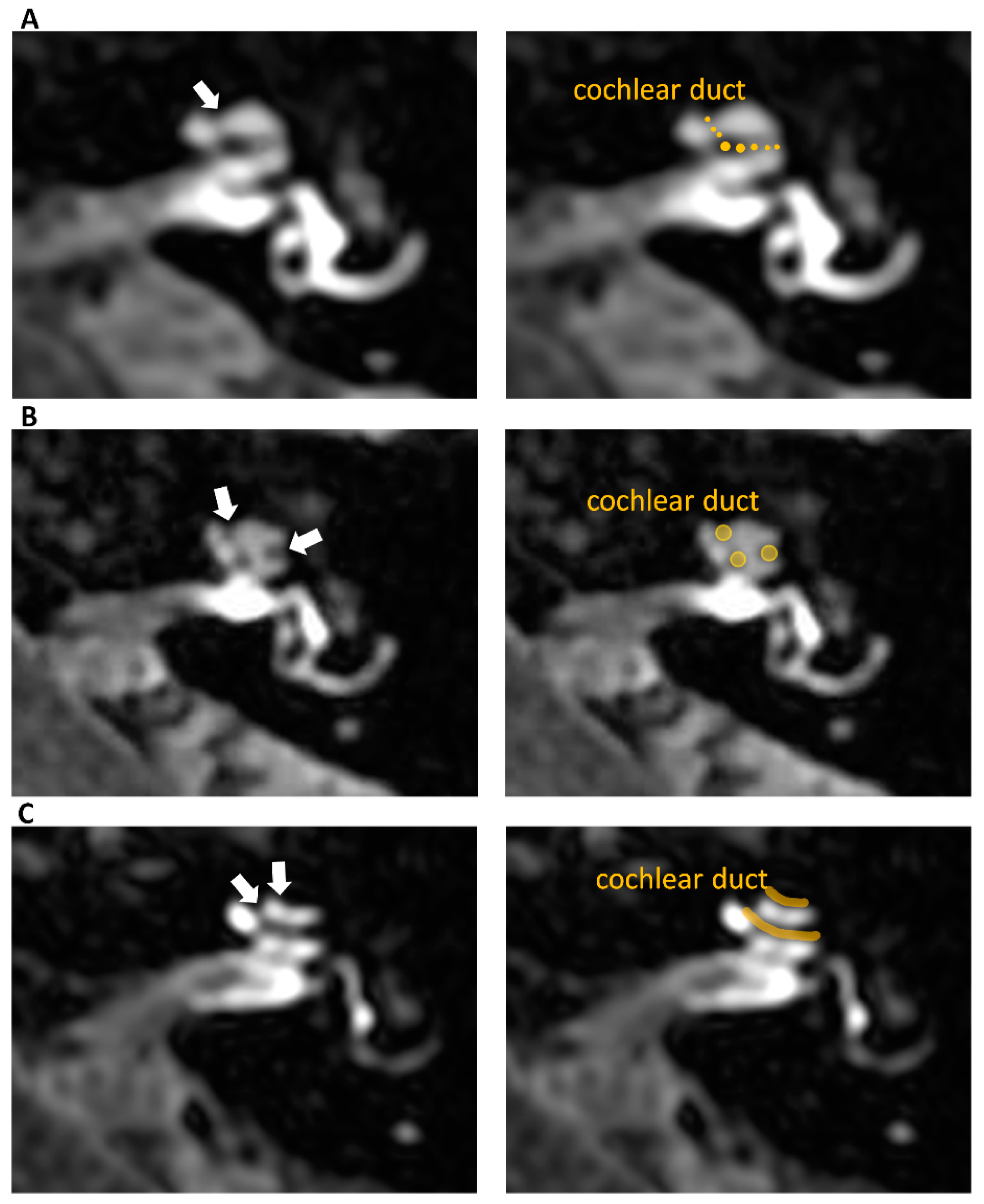
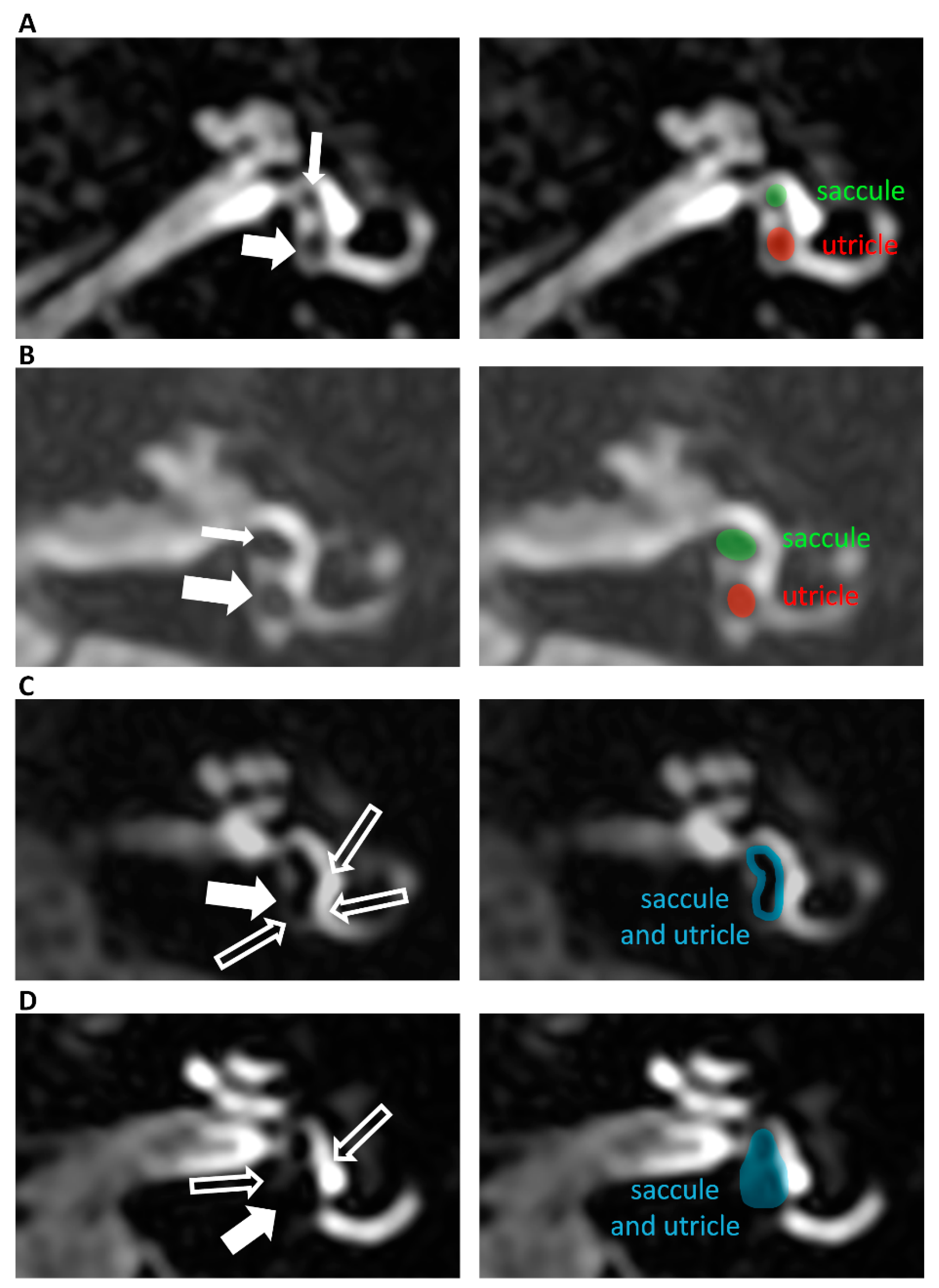
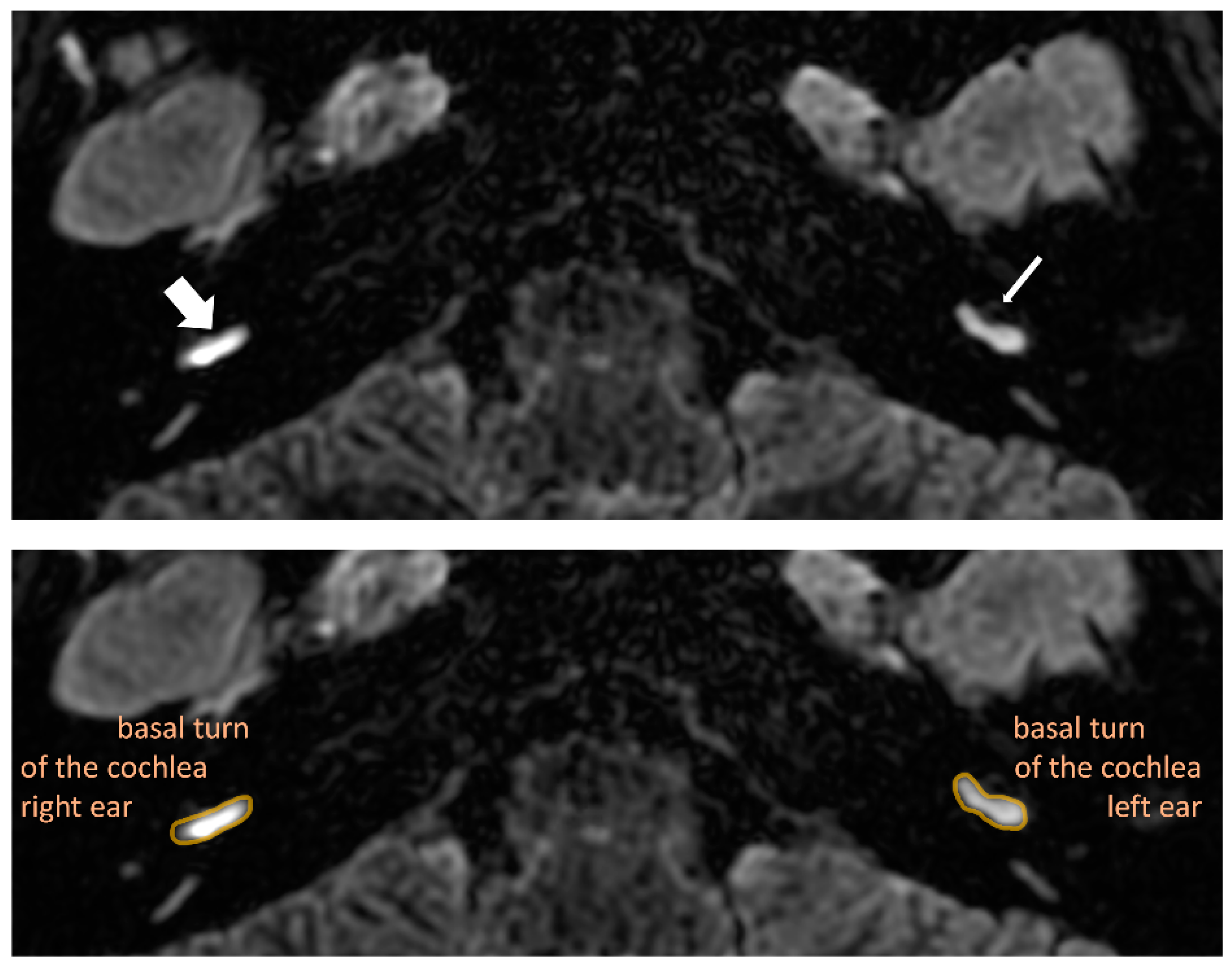
2.3. Magnetic Resonance Imaging Procedure and Analysis
2.4. Statistical Analysis
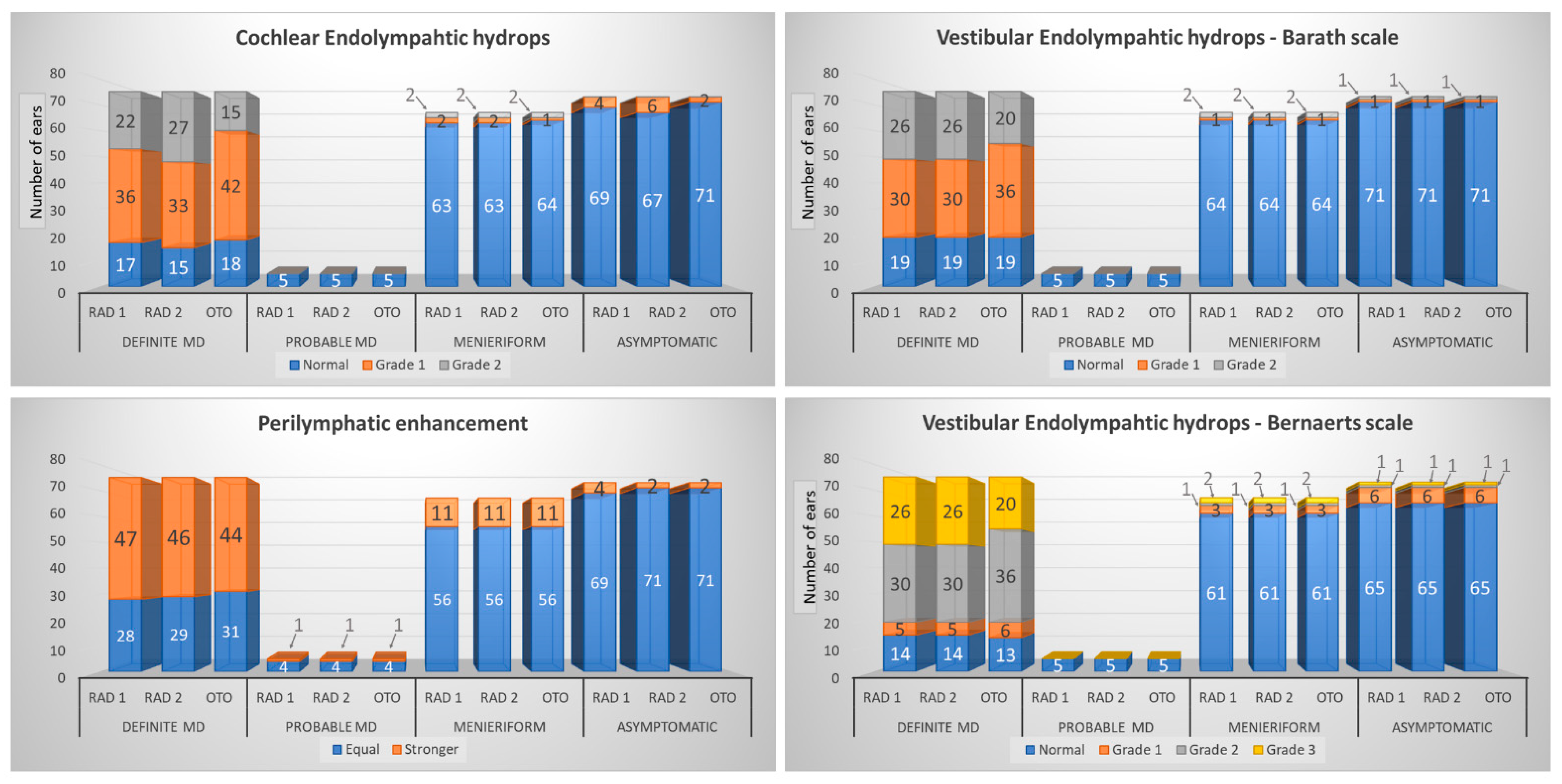
3. Results
3.1. Results
3.1.1. Patients’ Characteristics
3.1.2. MRI Findings—Radiological Features Analysis
4. Discussion
5. Conclusions
- Visualization of endolymphatic structures is possible.
- Endolymphatic hydrops is present more often in Ménière’s disease ears than in other inner diseases and much more frequent than in asymptomatic ears, so it might be used as a diagnostic criterion to support the diagnosis of Ménière’s disease for clinically unclear cases.
- Increased perilymphatic enhancement is not difficult to assess and is present more often in Ménière’s disease than in other inner ear pathologies.
- Quick diagnosis of endolymphatic hydrops on MRI is not difficult, even for quickly trained observers, that is, otorhinolaryngologists after a short period of training.
- The assessment of vestibular hydrops on the two scales mentioned above is easy to learn. The modified scale increases the sensitivity and specificity of the method to diagnose Ménière’s disease ears, so it can be used for diagnosing and staging vestibular endolymphatic hydrops.
- Evaluation of cochlear hydrops is more complicated than vestibular. However, the main concern is not to diagnose pathology but to grade it properly (which means to answer the question “is it 1st or 2nd grade endolymphatic hydrops?”) rather than to diagnose it (“is it normal = 0 or abnormal = 1st or 2nd grade?”). Therefore, it should be used for the diagnosis of endolymphatic hydrops, not for grading it.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopez-Escamez, J.A.; Carey, J.; Chung, W.H.; Goebel, J.A.; Magnusson, M.; Mandala, M.; Newman-Toker, D.E.; Strupp, M.; Suzuki, M.; Trabalzini, F.; et al. Diagnostic criteria for Meniere’s disease. J. Vestib. Res. 2015, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Goebel, J.A. 2015 Equilibrium Committee Amendment to the 1995 AAO-HNS Guidelines for the Definition of Meniere’s Disease. Otolaryngol. Head Neck. Surg. 2016, 154, 403–404. [Google Scholar] [CrossRef] [PubMed]
- Hallpike, C.S.; Cairns, H. Observations on the Pathology of Meniere’s Syndrome: (Section of Otology). Proc. R. Soc. Med. 1938, 31, 1317–1336. [Google Scholar]
- Nakashima, T.; Naganawa, S.; Sugiura, M.; Teranishi, M.; Sone, M.; Hayashi, H.; Nakata, S.; Katayama, N.; Ishida, I.M. Visualization of endolymphatic hydrops in patients with Meniere’s disease. Laryngoscope 2007, 117, 415–420. [Google Scholar] [CrossRef]
- Nakashima, T.; Naganawa, S.; Pyykko, I.; Gibson, W.P.; Sone, M.; Nakata, S.; Teranishi, M. Grading of endolymphatic hydrops using magnetic resonance imaging. Acta Otolaryngol. Suppl. 2009, 129, 5–8. [Google Scholar] [CrossRef]
- Barath, K.; Schuknecht, B.; Naldi, A.M.; Schrepfer, T.; Bockisch, C.J.; Hegemann, S.C. Detection and grading of endolymphatic hydrops in Meniere disease using MR imaging. AJNR Am. J. Neuroradiol. 2014, 35, 1387–1392. [Google Scholar] [CrossRef]
- Attye, A.; Eliezer, M.; Boudiaf, N.; Tropres, I.; Chechin, D.; Schmerber, S.; Dumas, G.; Krainik, A. MRI of endolymphatic hydrops in patients with Meniere’s disease: A case-controlled study with a simplified classification based on saccular morphology. Eur. Radiol. 2017, 27, 3138–3146. [Google Scholar] [CrossRef]
- Bernaerts, A.; Vanspauwen, R.; Blaivie, C.; van Dinther, J.; Zarowski, A.; Wuyts, F.L.; Vanden Bossche, S.; Offeciers, E.; Casselman, J.W.; De Foer, B. The value of four stage vestibular hydrops grading and asymmetric perilymphatic enhancement in the diagnosis of Meniere’s disease on MRI. Neuroradiology 2019, 61, 421–429. [Google Scholar] [CrossRef]
- Naganawa, S.; Kawai, H.; Sone, M.; Nakashima, T. Increased sensitivity to low concentration gadolinium contrast by optimized heavily T2-weighted 3D-FLAIR to visualize endolymphatic space. Magn. Reson. Med. Sci. 2010, 9, 73–80. [Google Scholar] [CrossRef]
- Jasinska, A.; Lachowska, M.; Wnuk, E.; Pierchala, K.; Rowinski, O.; Niemczyk, K. Correlation between magnetic resonance imaging classification of endolymphatic hydrops and clinical manifestations and audiovestibular test results in patients with definite Meniere’s disease. Auris Nasus Larynx 2022, 49, 34–45. [Google Scholar] [CrossRef]
- Hornibrook, J.; Flook, E.; Greig, S.; Babbage, M.; Goh, T.; Coates, M.; Care, R.; Bird, P. MRI Inner Ear Imaging and Tone Burst Electrocochleography in the Diagnosis of Meniere’s Disease. Otol. Neurotol. 2015, 36, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Jerin, C.; Floerke, S.; Maxwell, R.; Gurkov, R. Relationship Between the Extent of Endolymphatic Hydrops and the Severity and Fluctuation of Audiovestibular Symptoms in Patients with Meniere’s Disease and MRI Evidence of Hydrops. Otol. Neurotol. 2018, 39, e123–e130. [Google Scholar] [CrossRef] [PubMed]
- Fukuoka, H.; Takumi, Y.; Tsukada, K.; Miyagawa, M.; Oguchi, T.; Ueda, H.; Kadoya, M.; Usami, S. Comparison of the diagnostic value of 3 T MRI after intratympanic injection of GBCA, electrocochleography, and the glycerol test in patients with Meniere’s disease. Acta Otolaryngol. 2012, 132, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Dai, C.; Zhao, M.; Sha, Y. The correlation between symptoms of definite Meniere’s disease and endolymphatic hydrops visualized by magnetic resonance imaging. Laryngoscope 2016, 126, 974–979. [Google Scholar] [CrossRef]
- Yamazaki, M.; Naganawa, S.; Kawai, H.; Nihashi, T.; Nakashima, T. Signal alteration of the cochlear perilymph on 3 different sequences after intratympanic Gd-DTPA administration at 3 tesla: Comparison of 3D-FLAIR, 3D-T1-weighted imaging, and 3D-CISS. Magn. Reson. Med. Sci. 2010, 9, 65–71. [Google Scholar] [CrossRef]
- Bykowski, J.; Harris, J.P.; Miller, M.; Du, J.; Mafee, M.F. Intratympanic Contrast in the Evaluation of Meniere Disease: Understanding the Limits. AJNR Am. J. Neuroradiol. 2015, 36, 1326–1332. [Google Scholar] [CrossRef]
- Fang, Z.M.; Chen, X.; Gu, X.; Liu, Y.; Zhang, R.; Cao, D.R.; He, H.G. A new magnetic resonance imaging scoring system for perilymphatic space appearance after intratympanic gadolinium injection, and its clinical application. J. Laryngol. Otol. 2012, 126, 454–459. [Google Scholar] [CrossRef]
- Nakashima, T.; Naganawa, S.; Teranishi, M.; Tagaya, M.; Nakata, S.; Sone, M.; Otake, H.; Kato, K.; Iwata, T.; Nishio, N. Endolymphatic hydrops revealed by intravenous gadolinium injection in patients with Meniere’s disease. Acta Otolaryngol. 2010, 130, 338–343. [Google Scholar] [CrossRef]
- Sepahdari, A.R.; Ishiyama, G.; Vorasubin, N.; Peng, K.A.; Linetsky, M.; Ishiyama, A. Delayed intravenous contrast-enhanced 3D FLAIR MRI in Meniere’s disease: Correlation of quantitative measures of endolymphatic hydrops with hearing. Clin. Imaging 2015, 39, 26–31. [Google Scholar] [CrossRef]
- Sano, R.; Teranishi, M.; Yamazaki, M.; Isoda, H.; Naganawa, S.; Sone, M.; Hiramatsu, M.; Yoshida, T.; Suzuki, H.; Nakashima, T. Contrast enhancement of the inner ear in magnetic resonance images taken at 10 minutes or 4 hours after intravenous gadolinium injection. Acta Otolaryngol. 2012, 132, 241–246. [Google Scholar] [CrossRef]
- Van Steekelenburg, J.M.; van Weijnen, A.; de Pont, L.M.H.; Vijlbrief, O.D.; Bommelje, C.C.; Koopman, J.P.; Verbist, B.M.; Blom, H.M.; Hammer, S. Value of Endolymphatic Hydrops and Perilymph Signal Intensity in Suspected Meniere Disease. AJNR Am. J. Neuroradiol. 2020, 41, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, M.; Naganawa, S.; Tagaya, M.; Kawai, H.; Ikeda, M.; Sone, M.; Teranishi, M.; Suzuki, H.; Nakashima, T. Comparison of contrast effect on the cochlear perilymph after intratympanic and intravenous gadolinium injection. AJNR Am. J. Neuroradiol. 2012, 33, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Naganawa, S.; Yamazaki, M.; Kawai, H.; Bokura, K.; Sone, M.; Nakashima, T. Imaging of Meniere’s disease after intravenous administration of single-dose gadodiamide: Utility of subtraction images with different inversion time. Magn. Reson. Med. Sci. 2012, 11, 213–219. [Google Scholar] [CrossRef]
- Naganawa, S.; Yamazaki, M.; Kawai, H.; Bokura, K.; Sone, M.; Nakashima, T. Imaging of Meniere’s disease by subtraction of MR cisternography from positive perilymph image. Magn. Reson. Med. Sci. 2012, 11, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Naganawa, S.; Suzuki, K.; Nakamichi, R.; Bokura, K.; Yoshida, T.; Sone, M.; Homann, G.; Nakashima, T.; Ikeda, M. Semi-quantification of endolymphatic size on MR imaging after intravenous injection of single-dose gadodiamide: Comparison between two types of processing strategies. Magn. Reson. Med. Sci. 2013, 12, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wu, Q.; Sha, Y.; Dai, C.; Zhang, R. Gadolinium-enhanced MRI reveals dynamic development of endolymphatic hydrops in Meniere’s disease. Braz. J. Otorhinolaryngol. 2020, 86, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Suarez Vega, V.M.; Dominguez, P.; Caballeros Lam, F.M.; Leal, J.I.; Perez-Fernandez, N. Comparison between high-resolution 3D-IR with real reconstruction and 3D-flair sequences in the assessment of endolymphatic hydrops in 3 tesla. Acta Otolaryngol. 2020, 140, 883–888. [Google Scholar] [CrossRef]
- Ito, T.; Kitahara, T.; Inui, H.; Miyasaka, T.; Kichikawa, K.; Ota, I.; Nario, K.; Matsumura, Y.; Yamanaka, T. Endolymphatic space size in patients with Meniere’s disease and healthy controls. Acta Otolaryngol. 2016, 136, 879–882. [Google Scholar] [CrossRef]
- Paskoniene, A.; Baltagalviene, R.; Lengvenis, G.; Beleskiene, V.; Ivaska, J.; Markeviciute, V.; Mickeviciene, V.; Lesinskas, E. The Importance of the Temporal Bone 3T MR Imaging in the Diagnosis of Meniere’s Disease. Otol. Neurotol. 2020, 41, 235–241. [Google Scholar] [CrossRef]
- Pai, I.; Mendis, S.; Murdin, L.; Touska, P.; Connor, S. Magnetic resonance imaging of Meniere’s disease: Early clinical experience in a UK centre. J. Laryngol. Otol. 2020, 134, 302–310. [Google Scholar] [CrossRef]
- Quatre, R.; Attye, A.; Karkas, A.; Job, A.; Dumas, G.; Schmerber, S. Relationship between Audio-Vestibular Functional Tests and Inner Ear MRI in Meniere’s Disease. Ear. Hear 2019, 40, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Zhou, F.; Wang, W. 3D-real IR MRI of Meniere’s disease with partial endolymphatic hydrops. Am. J. Otolaryngol. 2019, 40, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Guo, P.; Wang, W. Magnetic Resonance Imaging of Meniere’s Disease After Intravenous Administration of Gadolinium. Ann. Otol. Rhinol. Laryngol. 2018, 127, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Sugimoto, S.; Teranishi, M.; Otake, H.; Yamazaki, M.; Naganawa, S.; Nakashima, T.; Sone, M. Imaging of the endolymphatic space in patients with Meniere’s disease. Auris Nasus Larynx 2018, 45, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Conlon, B.J.; Gibson, W.P. Meniere’s disease: The incidence of hydrops in the contralateral asymptomatic ear. Laryngoscope 1999, 109, 1800–1802. [Google Scholar] [CrossRef]
- Perez-Carpena, P.; Lopez-Escamez, J.A. Current Understanding and Clinical Management of Meniere’s Disease: A Systematic Review. Semin Neurol 2020, 40, 138–150. [Google Scholar] [CrossRef]
- Tagaya, M.; Yamazaki, M.; Teranishi, M.; Naganawa, S.; Yoshida, T.; Otake, H.; Nakata, S.; Sone, M.; Nakashima, T. Endolymphatic hydrops and blood-labyrinth barrier in Meniere’s disease. Acta Otolaryngol. 2011, 131, 474–479. [Google Scholar] [CrossRef]
- Pakdaman, M.N.; Ishiyama, G.; Ishiyama, A.; Peng, K.A.; Kim, H.J.; Pope, W.B.; Sepahdari, A.R. Blood-Labyrinth Barrier Permeability in Meniere Disease and Idiopathic Sudden Sensorineural Hearing Loss: Findings on Delayed Postcontrast 3D-FLAIR MRI. AJNR Am. J. Neuroradiol. 2016, 37, 1903–1908. [Google Scholar] [CrossRef]
- Jasinska-Nowacka, A.; Lachowska, M.; Wnuk, E.; Niemczyk, K. Changes in endolymphatic hydrops after vestibular neurectomy observed in magnetic resonance imaging—A pilot study. Auris Nasus Larynx 2022, 49, 584–592. [Google Scholar] [CrossRef]
- Kim, T.Y.; Park, D.W.; Lee, Y.J.; Lee, J.Y.; Lee, S.H.; Chung, J.H.; Lee, S. Comparison of Inner Ear Contrast Enhancement among Patients with Unilateral Inner Ear Symptoms in MR Images Obtained 10 Minutes and 4 Hours after Gadolinium Injection. AJNR Am. J. Neuroradiol. 2015, 36, 2367–2372. [Google Scholar] [CrossRef]
- Pyykko, I.; Nakashima, T.; Yoshida, T.; Zou, J.; Naganawa, S. Meniere’s disease: A reappraisal supported by a variable latency of symptoms and the MRI visualisation of endolymphatic hydrops. BMJ Open 2013, 3, e001555. [Google Scholar] [CrossRef] [PubMed]
- Gurkov, R.; Flatz, W.; Louza, J.; Strupp, M.; Krause, E. In vivo visualization of endolyphatic hydrops in patients with Meniere’s disease: Correlation with audiovestibular function. Eur. Arch. Otorhinolaryngol. 2011, 268, 1743–1748. [Google Scholar] [CrossRef]
- Naganawa, S.; Nakashima, T. Visualization of endolymphatic hydrops with MR imaging in patients with Meniere’s disease and related pathologies: Current status of its methods and clinical significance. Jpn. J. Radiol. 2014, 32, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Kahn, L.; Hautefort, C.; Guichard, J.P.; Toupet, M.; Jourdaine, C.; Vitaux, H.; Herman, P.; Kania, R.; Houdart, E.; Attye, A.; et al. Relationship between video head impulse test, ocular and cervical vestibular evoked myogenic potentials, and compartmental magnetic resonance imaging classification in meniere’s disease. Laryngoscope 2020, 130, E444–E452. [Google Scholar] [CrossRef]
- Kato, K.; Yoshida, T.; Teranishi, M.; Sano, R.; Otake, H.; Sone, M.; Naganawa, S.; Nakashima, T. Peak width in multifrequency tympanometry and endolymphatic hydrops revealed by magnetic resonance imaging. Otol. Neurotol. 2012, 33, 912–915. [Google Scholar] [CrossRef]
- Katayama, N.; Yamamoto, M.; Teranishi, M.; Naganawa, S.; Nakata, S.; Sone, M.; Nakashima, T. Relationship between endolymphatic hydrops and vestibular-evoked myogenic potential. Acta Otolaryngol. 2010, 130, 917–923. [Google Scholar] [CrossRef]
- Gurkov, R.; Flatz, W.; Keeser, D.; Strupp, M.; Ertl-Wagner, B.; Krause, E. Effect of standard-dose Betahistine on endolymphatic hydrops: An MRI pilot study. Eur. Arch. Otorhinolaryngol. 2013, 270, 1231–1235. [Google Scholar] [CrossRef]
- Gurkov, R.; Flatz, W.; Ertl-Wagner, B.; Krause, E. Endolymphatic hydrops in the horizontal semicircular canal: A morphologic correlate for canal paresis in Meniere’s disease. Laryngoscope 2013, 123, 503–506. [Google Scholar] [CrossRef] [PubMed]
- Uno, A.; Imai, T.; Watanabe, Y.; Tanaka, H.; Kitahara, T.; Horii, A.; Kamakura, T.; Takimoto, Y.; Osaki, Y.; Nishiike, S.; et al. Changes in endolymphatic hydrops after sac surgery examined by Gd-enhanced MRI. Acta Otolaryngol. 2013, 133, 924–929. [Google Scholar] [CrossRef]
- Miyagawa, M.; Fukuoka, H.; Tsukada, K.; Oguchi, T.; Takumi, Y.; Sugiura, M.; Ueda, H.; Kadoya, M.; Usami, S. Endolymphatic hydrops and therapeutic effects are visualized in ‘atypical’ Meniere’s disease. Acta Otolaryngol. 2009, 129, 1326–1329. [Google Scholar] [CrossRef]
- Connor, S.E.J.; Pai, I. Endolymphatic hydrops magnetic resonance imaging in Meniere’s disease. Clin. Radiol. 2021, 76, 76.e1–76.e19. [Google Scholar] [CrossRef] [PubMed]
- Eliezer, M.; Gillibert, A.; Tropres, I.; Krainik, A.; Attye, A. Influence of inversion time on endolymphatic hydrops evaluation in 3D-FLAIR imaging. J. Neuroradiol. 2017, 44, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Naganawa, S.; Satake, H.; Kawamura, M.; Fukatsu, H.; Sone, M.; Nakashima, T. Separate visualization of endolymphatic space, perilymphatic space and bone by a single pulse sequence; 3D-inversion recovery imaging utilizing real reconstruction after intratympanic Gd-DTPA administration at 3 Tesla. Eur. Radiol. 2008, 18, 920–924. [Google Scholar] [CrossRef] [PubMed]
| CoEH Number of Ears (Percentage) | VEH Barath Number of Ears (Percentage) | VEH Bernaerts Number of Ears (Percentage) | PE Number of Ears (Percentage) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical diagnosis | Number of ears (total 220) | Rad1 | Rad2 | Oto | Rad1 | Rad2 | Oto | Rad1 | Rad2 | Oto | Rad1 | Rad2 | Oto |
| Definite MD | 75 | 58 (77%) | 60 (80%) | 57 (76%) | 56 (74.7%) | 61 (81.3%) | 62 (82.7%) | 47 (62.7%) | 46 (61.3%) | 44 (58.7%) | |||
| Probable MD | 5 | 0 (0%) | 1 (20%) | ||||||||||
| Other diseases | 67 | 4 (6%) | 4 (6%) | 3 (4.5%) | 3 (4.5%) | 5 (7.5%) | 9 (13.4%) | ||||||
| Asymptomatic | 73 | 4 (5.5%) | 6 (8.2%) | 2 (2.7%) | 2 (2.7%) | 8 (11%) | 4 (5.5%) | 2 (2.7%) | |||||
| Radiological Feature | Friedman ANOVA p-Value | Kendall’s Concordance Coefficient | Pairs of Observers Compared | Number of Different Observations | Wilcoxon Test Results p-Value | ANOVA Test Results p-Value |
|---|---|---|---|---|---|---|
| CoEH | 0.0000 * | 0.0456 | Rad1 vs. Rad2 | 11 | 0.0164 | 0.0067 * |
| Rad1 vs. Oto | 19 | 0.0269 | 0.0116 * | |||
| Rad2 vs. Oto | 30 | 0.0014 | 0.0003 * | |||
| VEH Barath | 0.0111 * | 0.0205 | Rad1 vs. Rad2 | 0 | -- | -- |
| Rad1 vs. Oto | 8 | 0.0587 | 0.0339 * | |||
| Rad2 vs. Oto | 8 | 0.0587 | 0.0339 * | |||
| VEH Bernaerts | 0.1030 | 0.0103 | Rad1 vs. Rad2 | 0 | -- | |
| Rad1 vs. Oto | 11 | 0.1823 | 0.1317 | |||
| Rad2 vs. Oto | 11 | 0.1823 | 0.1317 | |||
| PE | 0.2053 | 0.0072 | Rad1 vs. Rad2 | 7 | 0.3105 | 0.2568 |
| Rad1 vs. Oto | 11 | 0.1823 | 0.1317 | |||
| Rad2 vs. Oto | 6 | 0.4631 | 0.4142 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wnuk, E.; Lachowska, M.; Jasińska-Nowacka, A.; Maj, E.; Niemczyk, K. Reliability of Endolymphatic Hydrops Qualitative Assessment in Magnetic Resonance Imaging. J. Clin. Med. 2023, 12, 202. https://doi.org/10.3390/jcm12010202
Wnuk E, Lachowska M, Jasińska-Nowacka A, Maj E, Niemczyk K. Reliability of Endolymphatic Hydrops Qualitative Assessment in Magnetic Resonance Imaging. Journal of Clinical Medicine. 2023; 12(1):202. https://doi.org/10.3390/jcm12010202
Chicago/Turabian StyleWnuk, Emilia, Magdalena Lachowska, Agnieszka Jasińska-Nowacka, Edyta Maj, and Kazimierz Niemczyk. 2023. "Reliability of Endolymphatic Hydrops Qualitative Assessment in Magnetic Resonance Imaging" Journal of Clinical Medicine 12, no. 1: 202. https://doi.org/10.3390/jcm12010202
APA StyleWnuk, E., Lachowska, M., Jasińska-Nowacka, A., Maj, E., & Niemczyk, K. (2023). Reliability of Endolymphatic Hydrops Qualitative Assessment in Magnetic Resonance Imaging. Journal of Clinical Medicine, 12(1), 202. https://doi.org/10.3390/jcm12010202






