Questionnaire-Based Study Evaluating the Hand Hygiene Practices and the Impact of Disinfection in the COVID-19 Pandemic on Hand Skin Conditions in Poland
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Informed Consent
2.2. Study Design and Population
2.3. Study Protocol
2.4. Statistical Analysis
3. Results
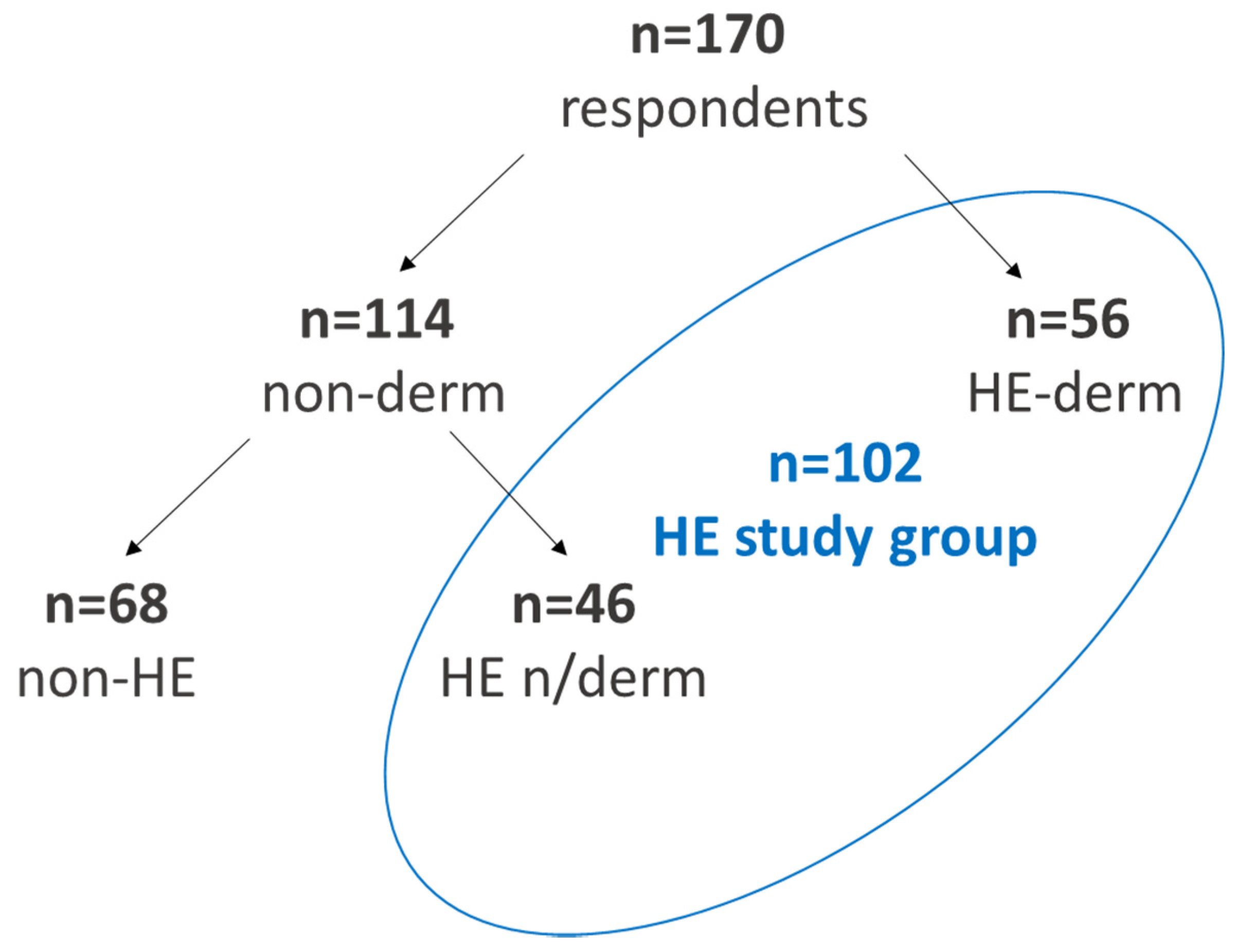
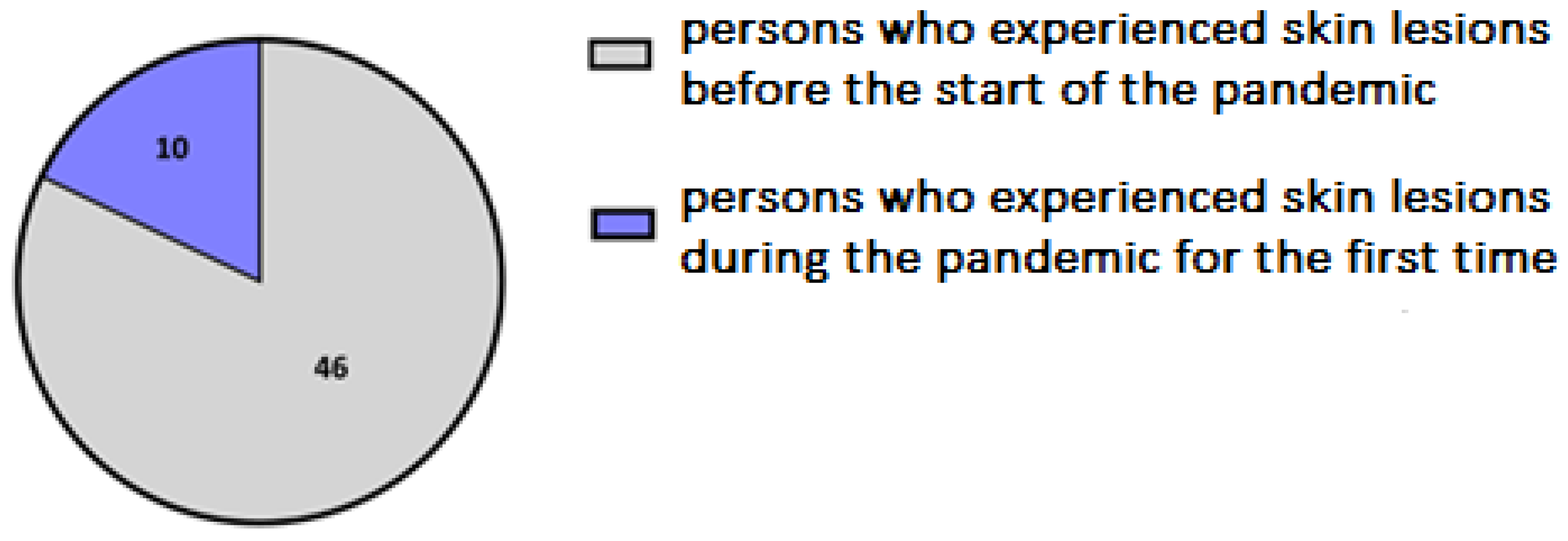
3.1. Study Group
3.2. Study Outcomes
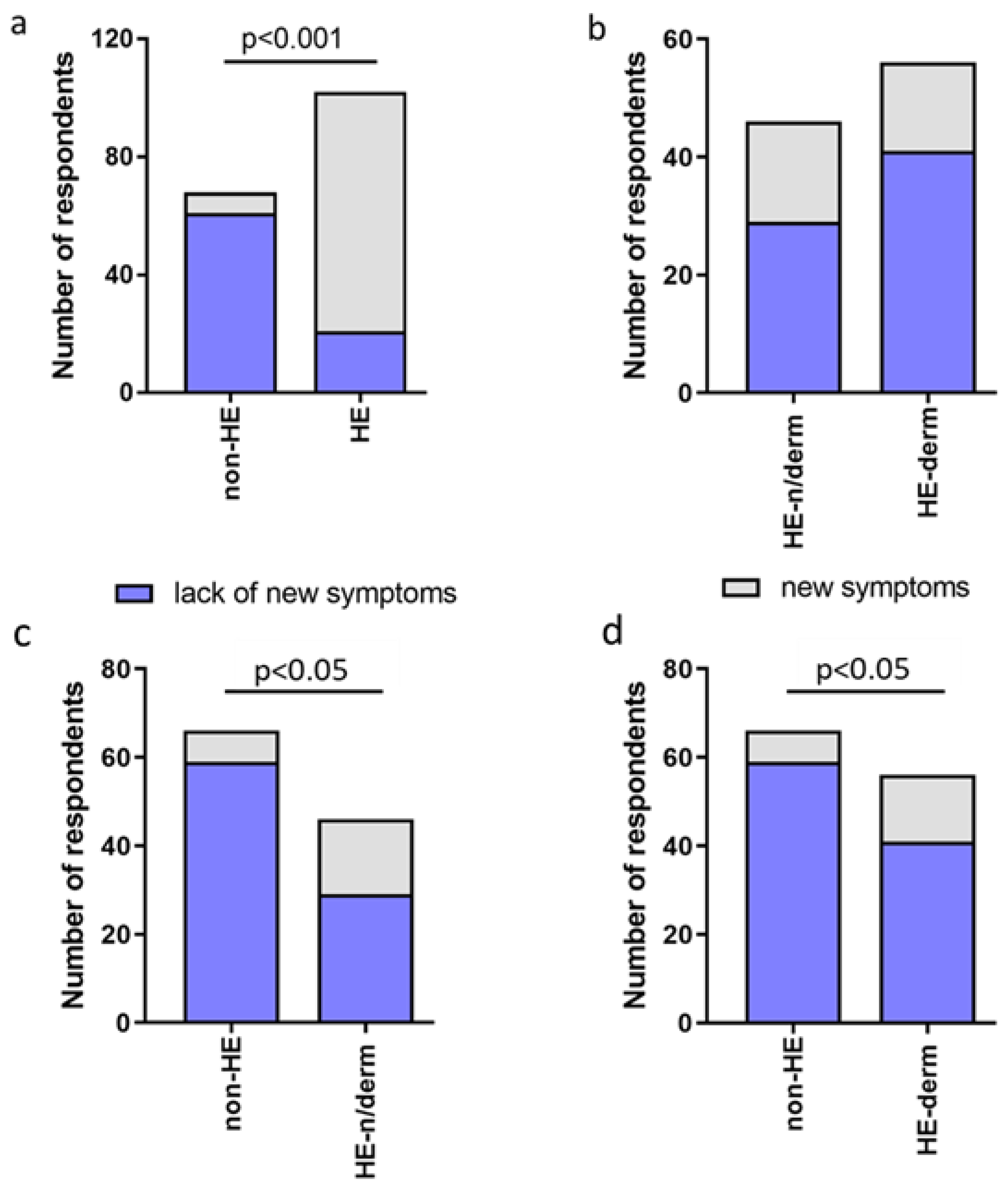
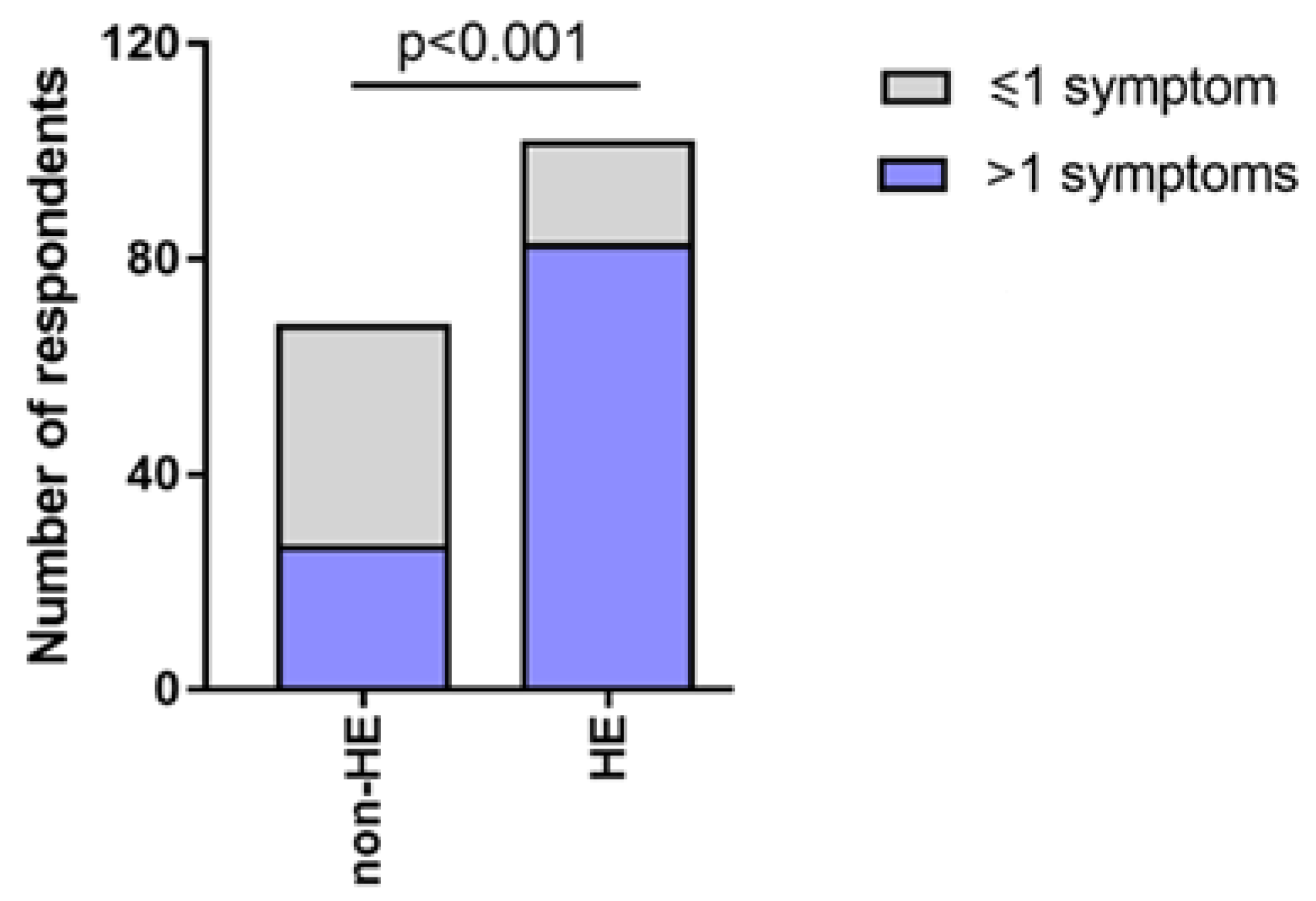
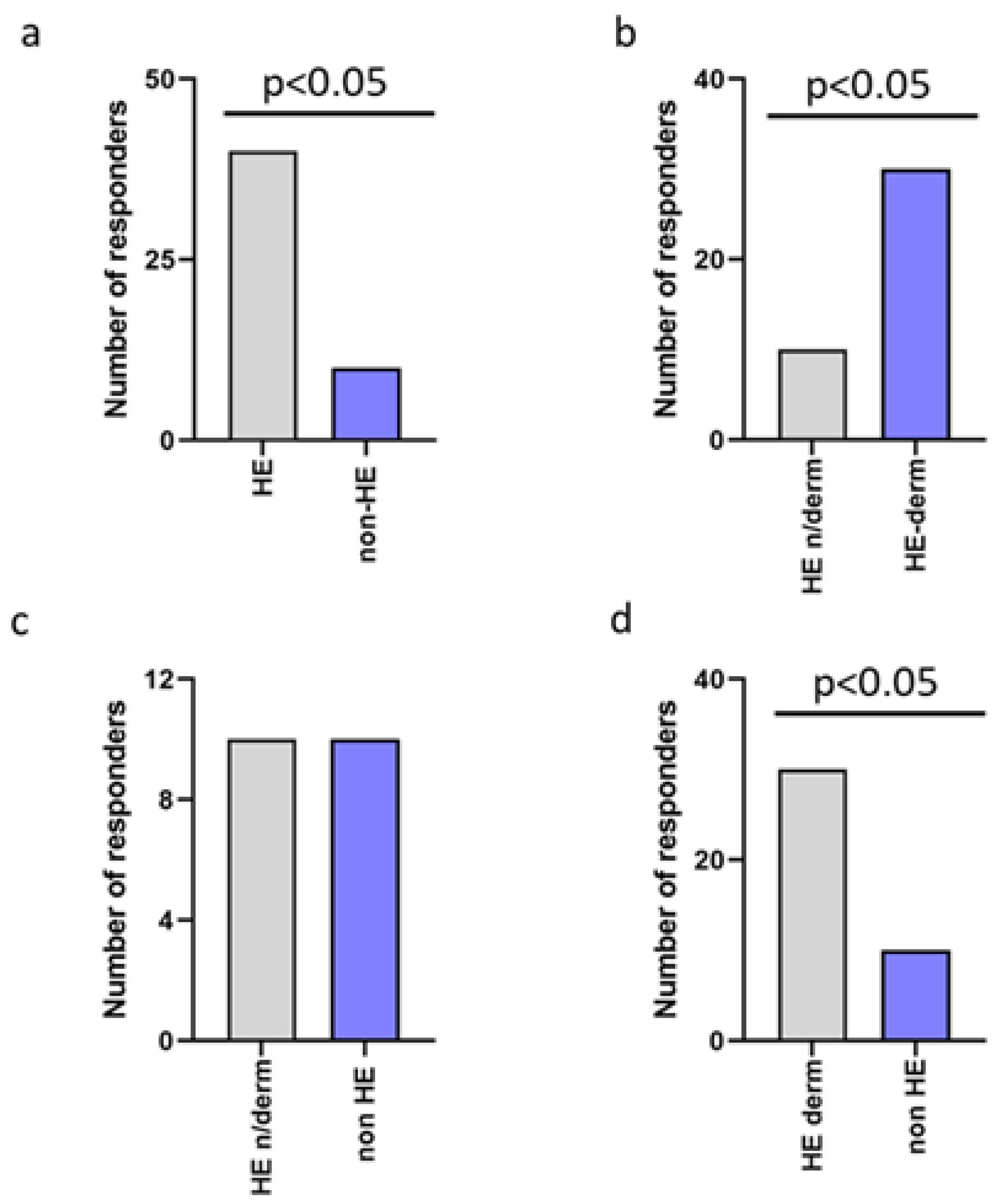
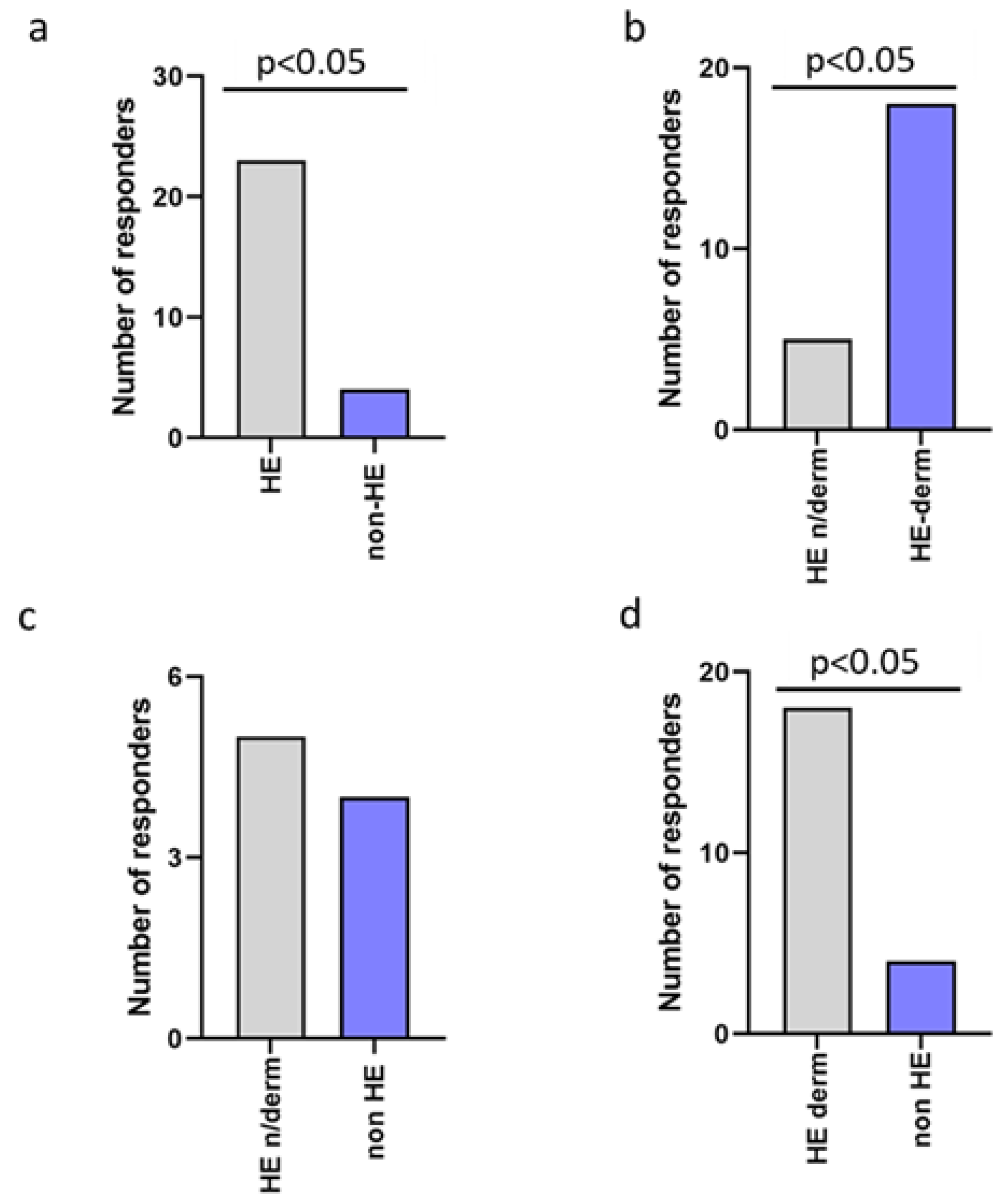
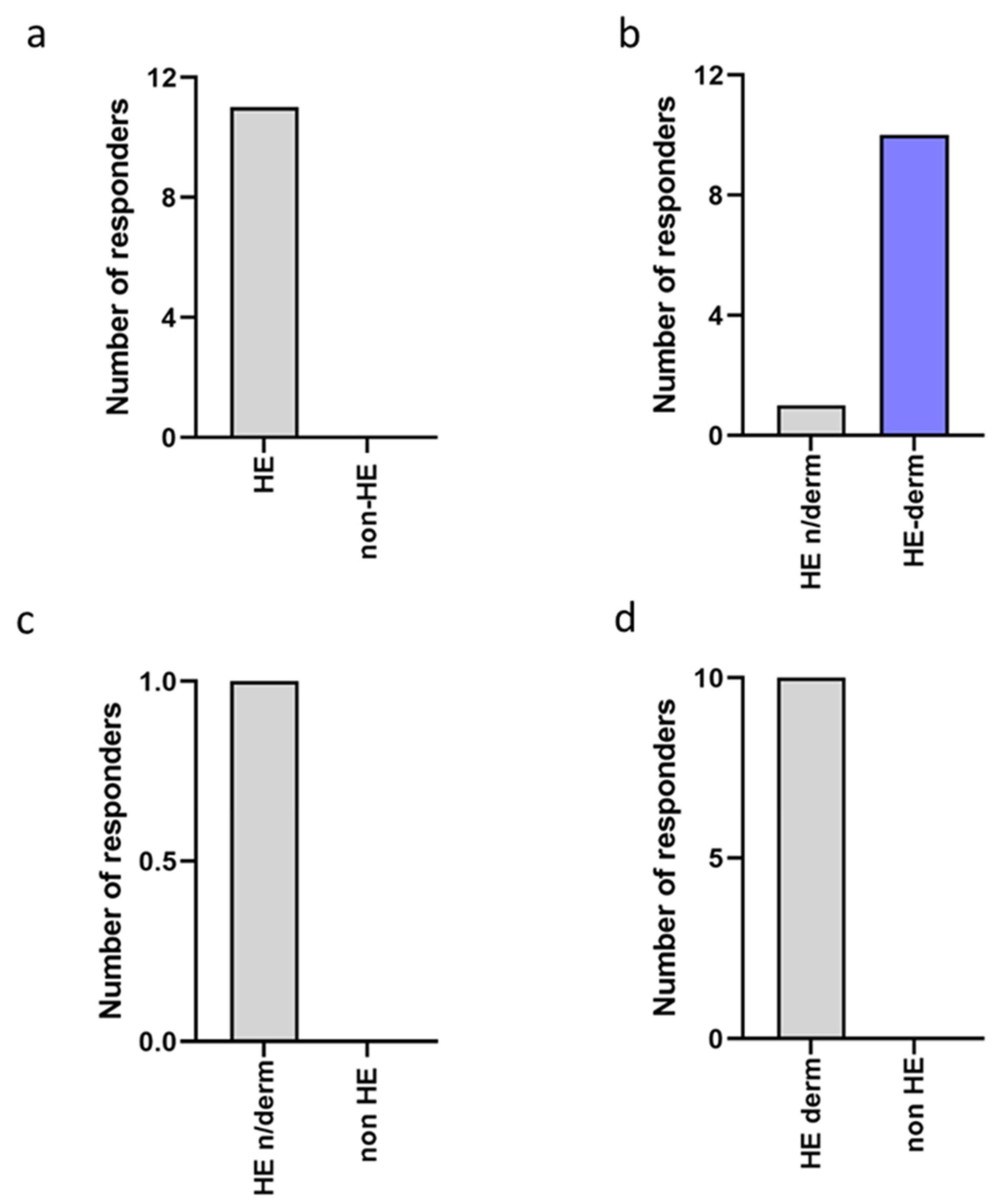
3.2.1. The Occurrence of New Symptoms
3.2.2. Negative Effects and Lack of Negative Effects
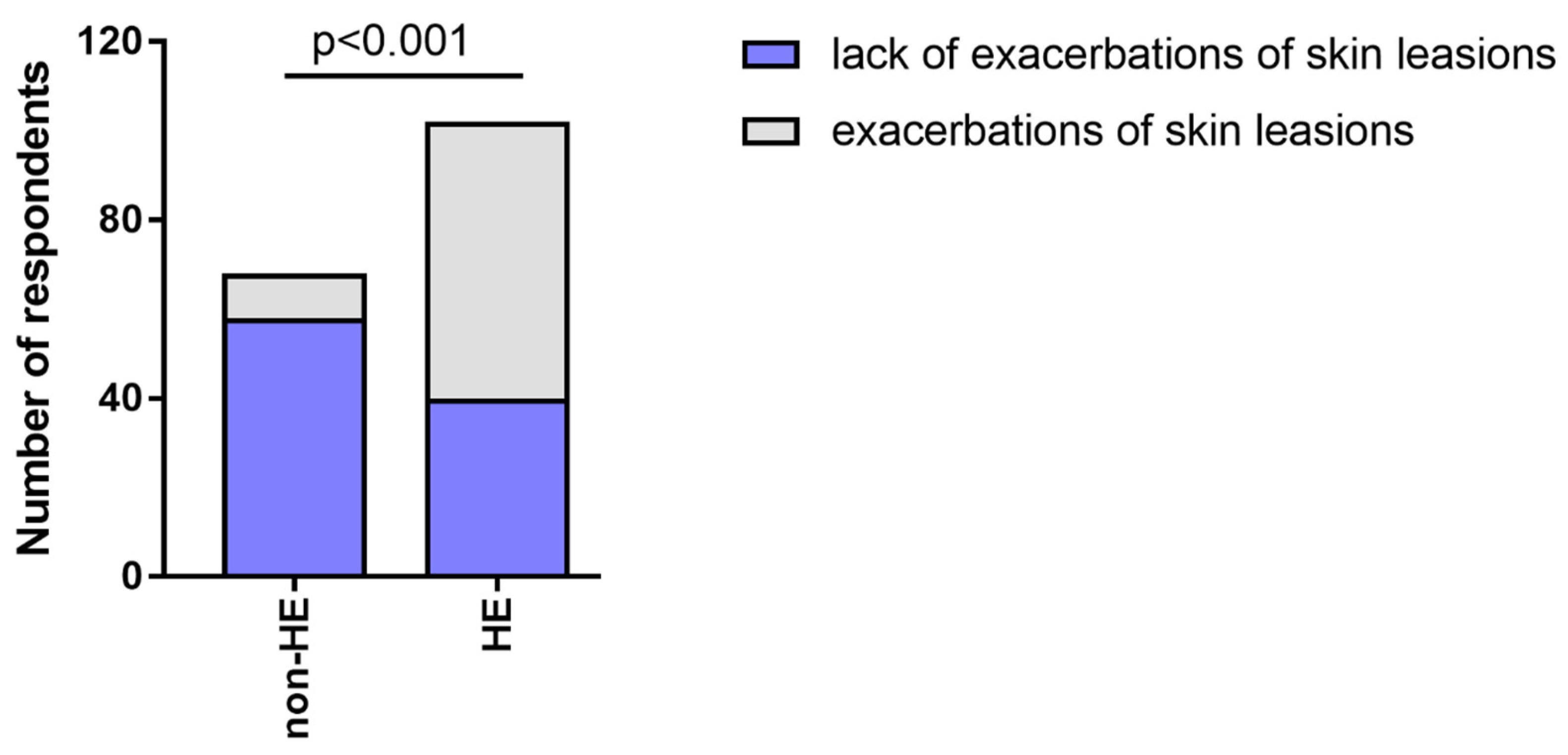
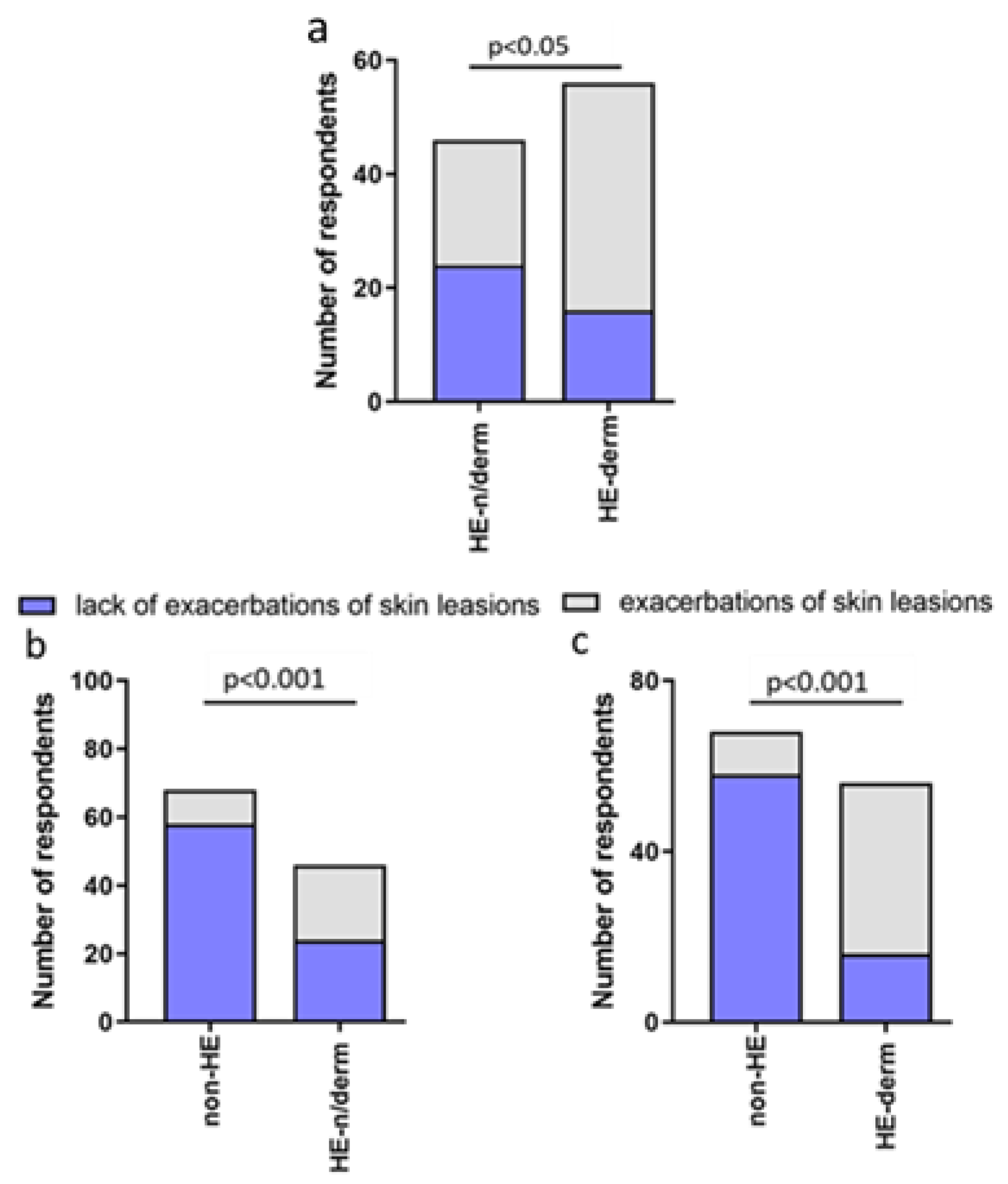
3.2.3. The Exacerbations of Skin Lesions
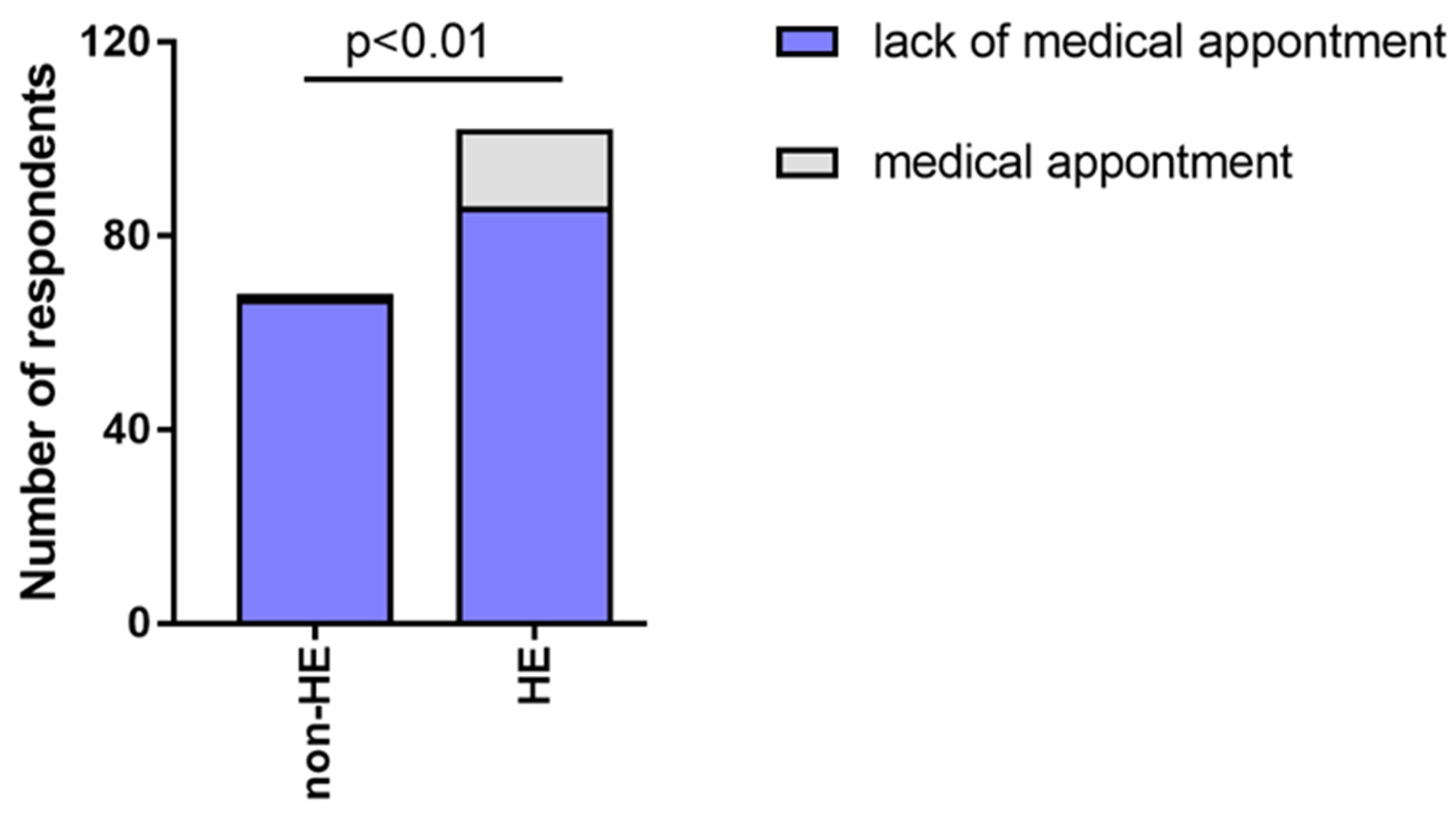
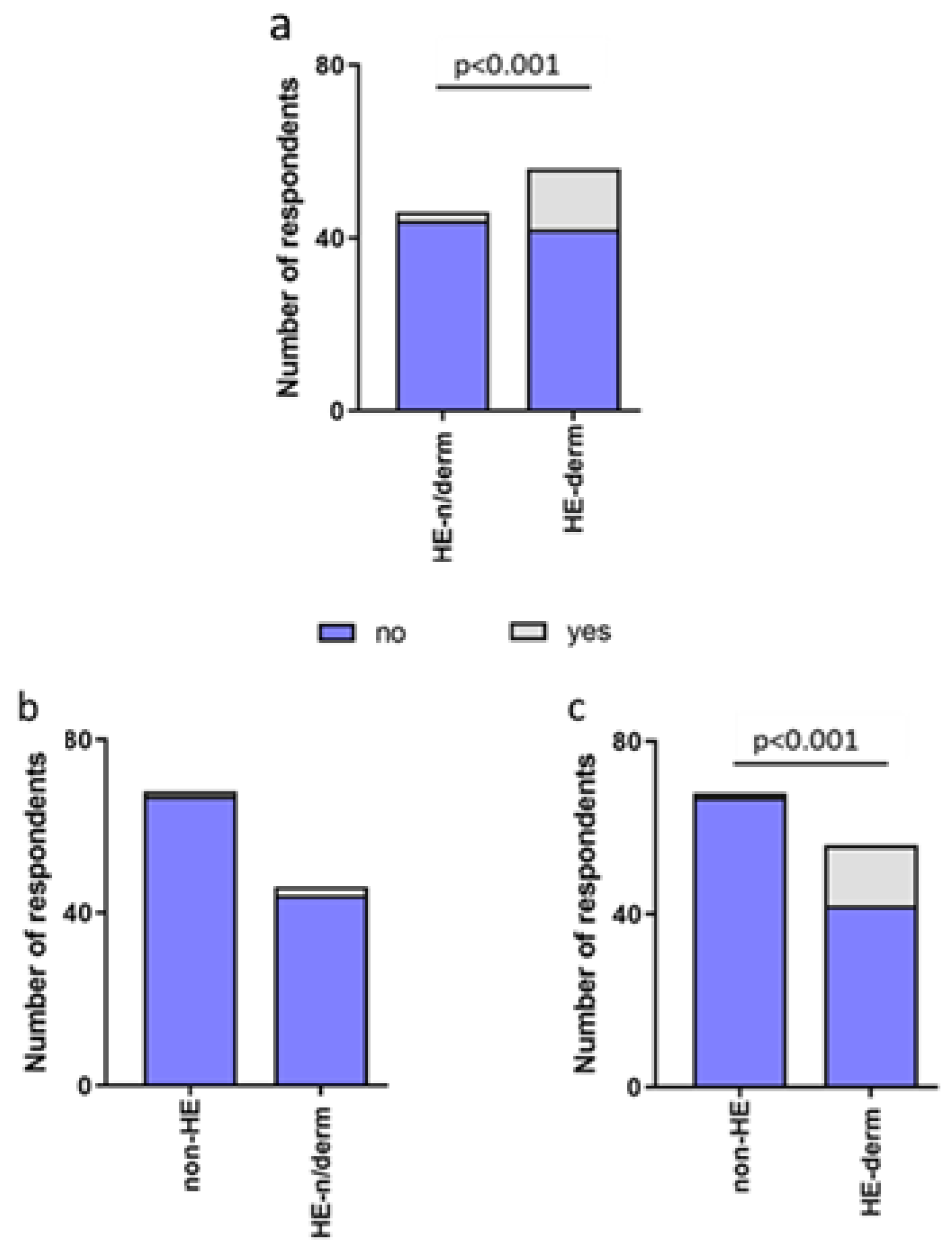
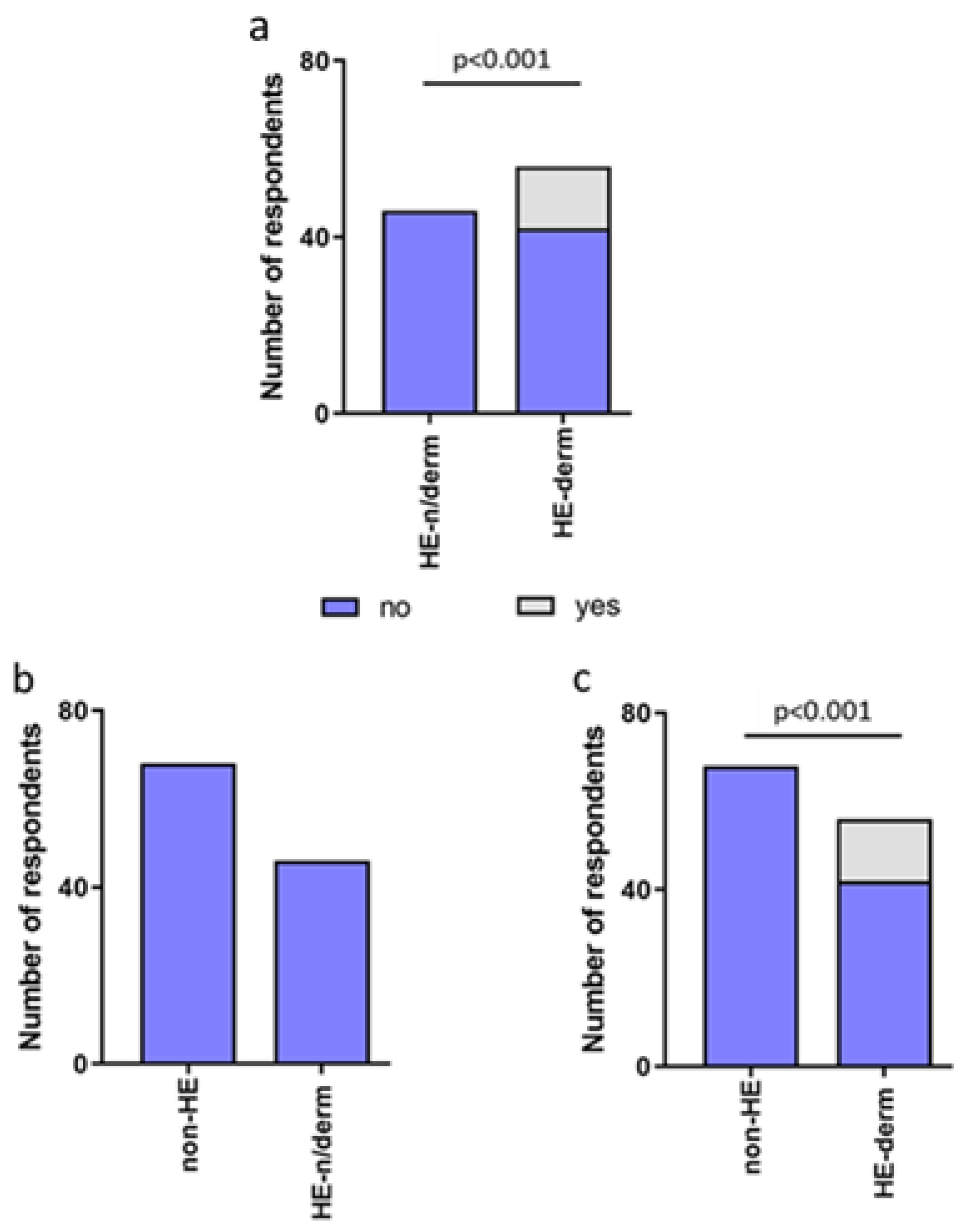
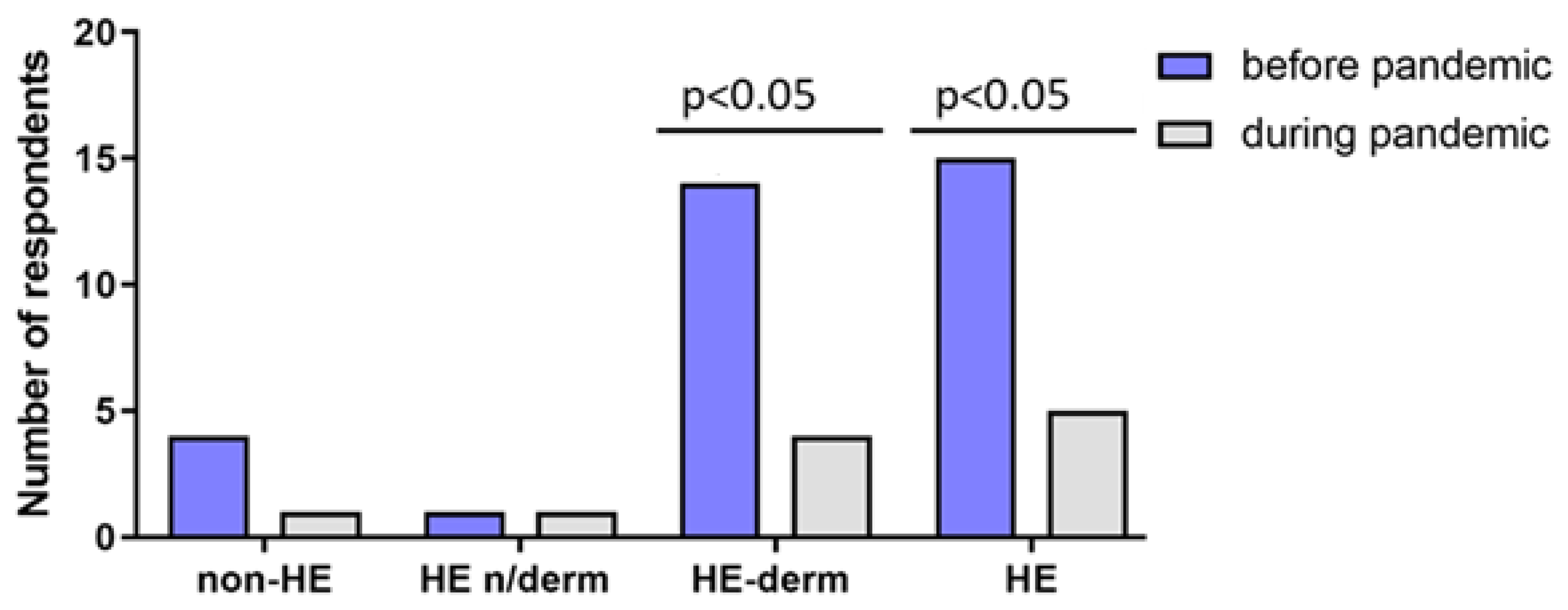
3.2.4. Medical Appointments
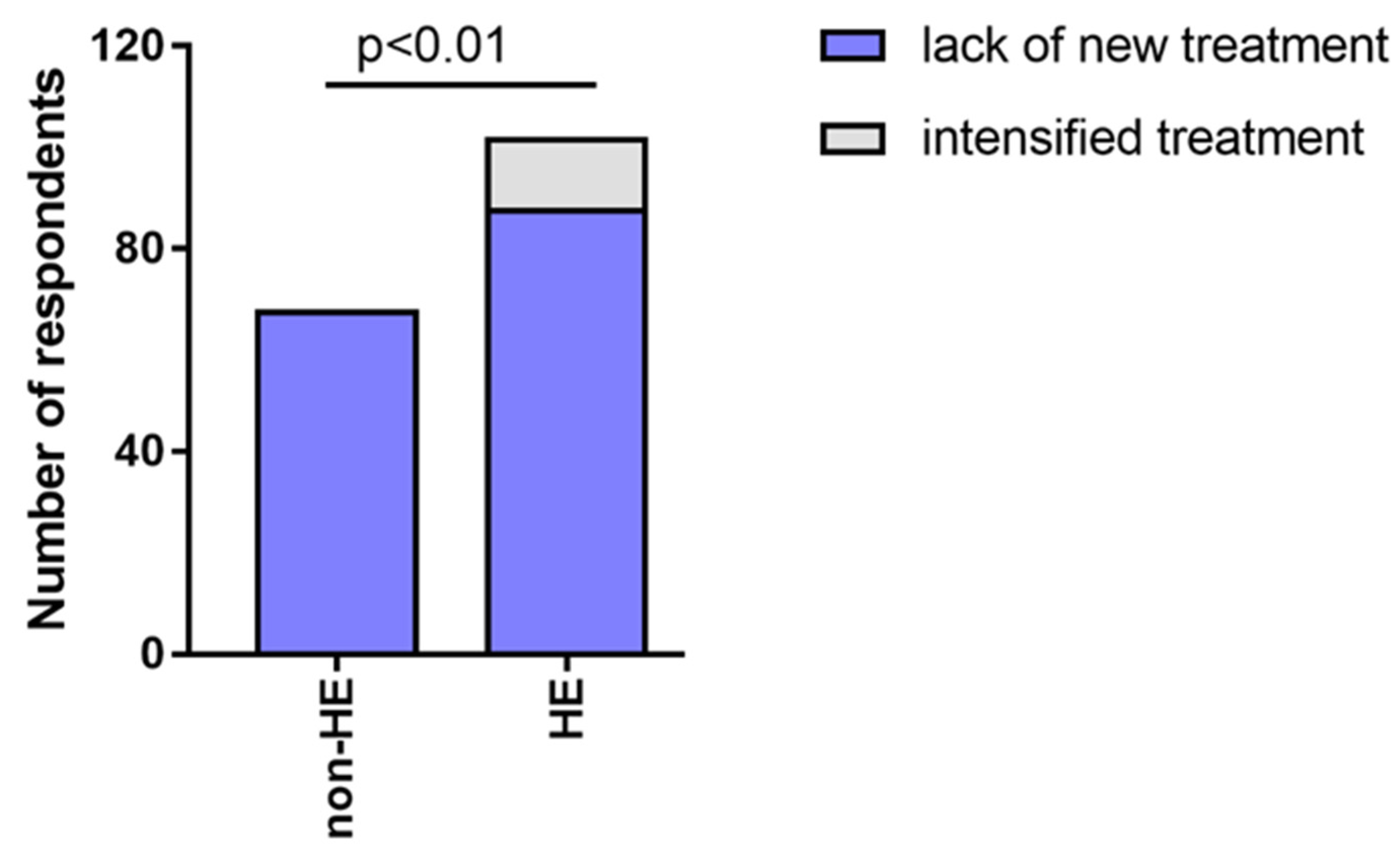
3.2.5. New Treatment
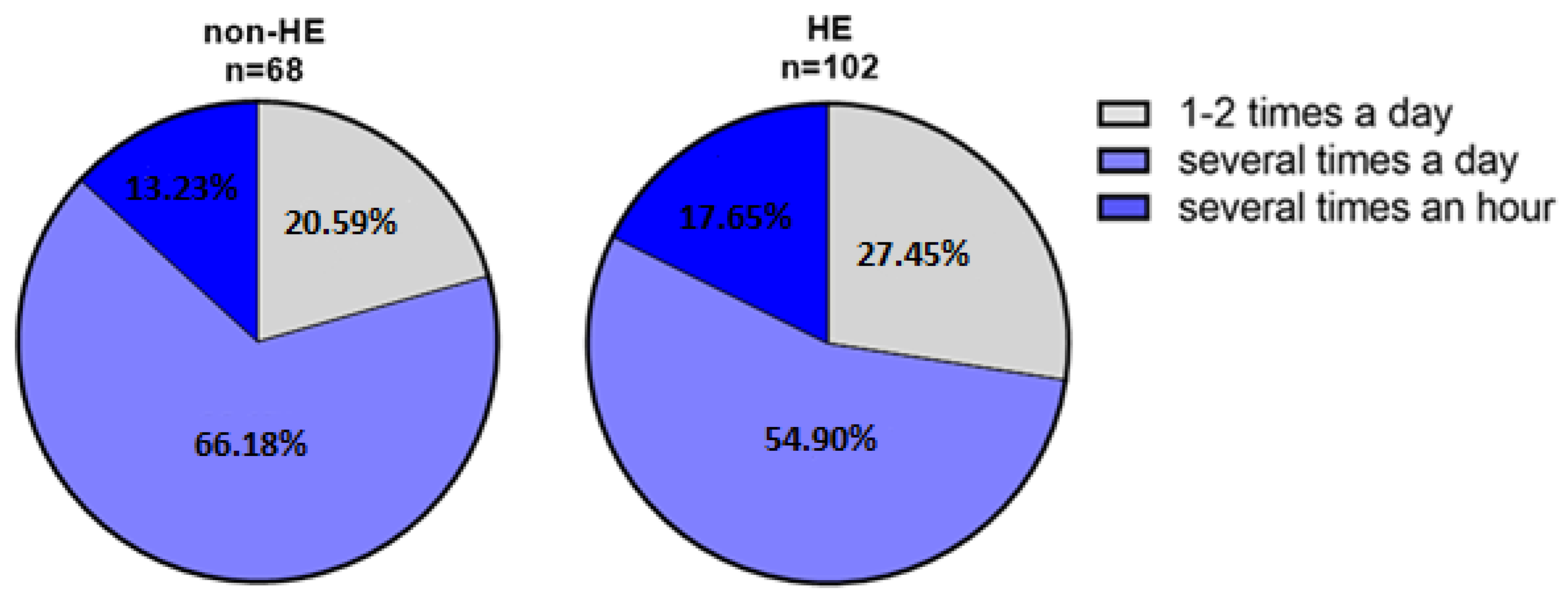
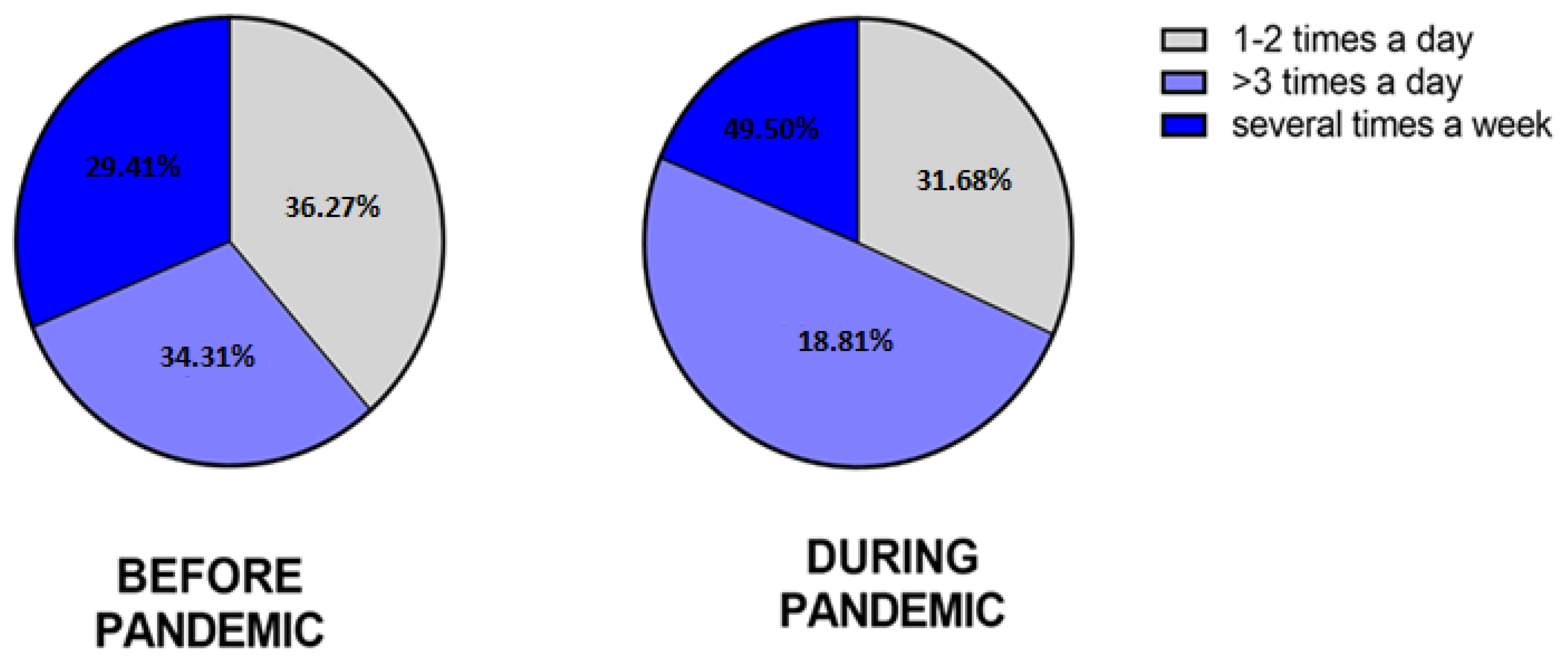
3.2.6. The Frequency of Hand Skin Disinfection
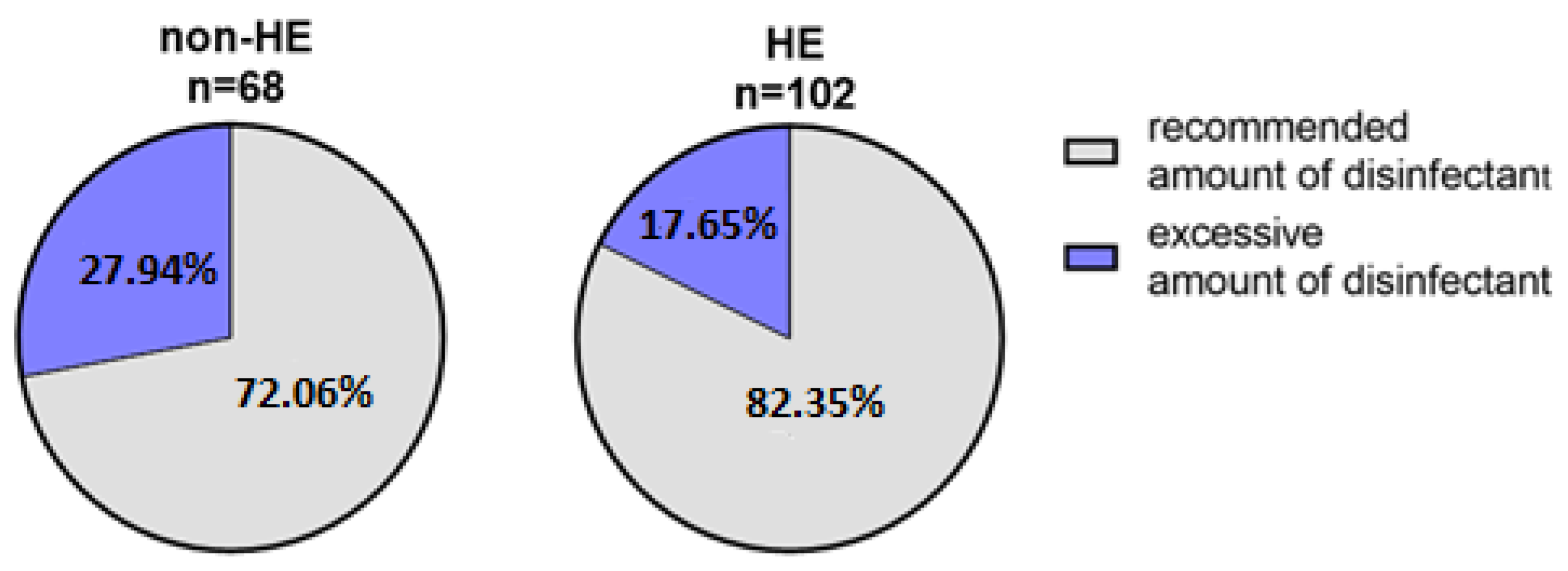
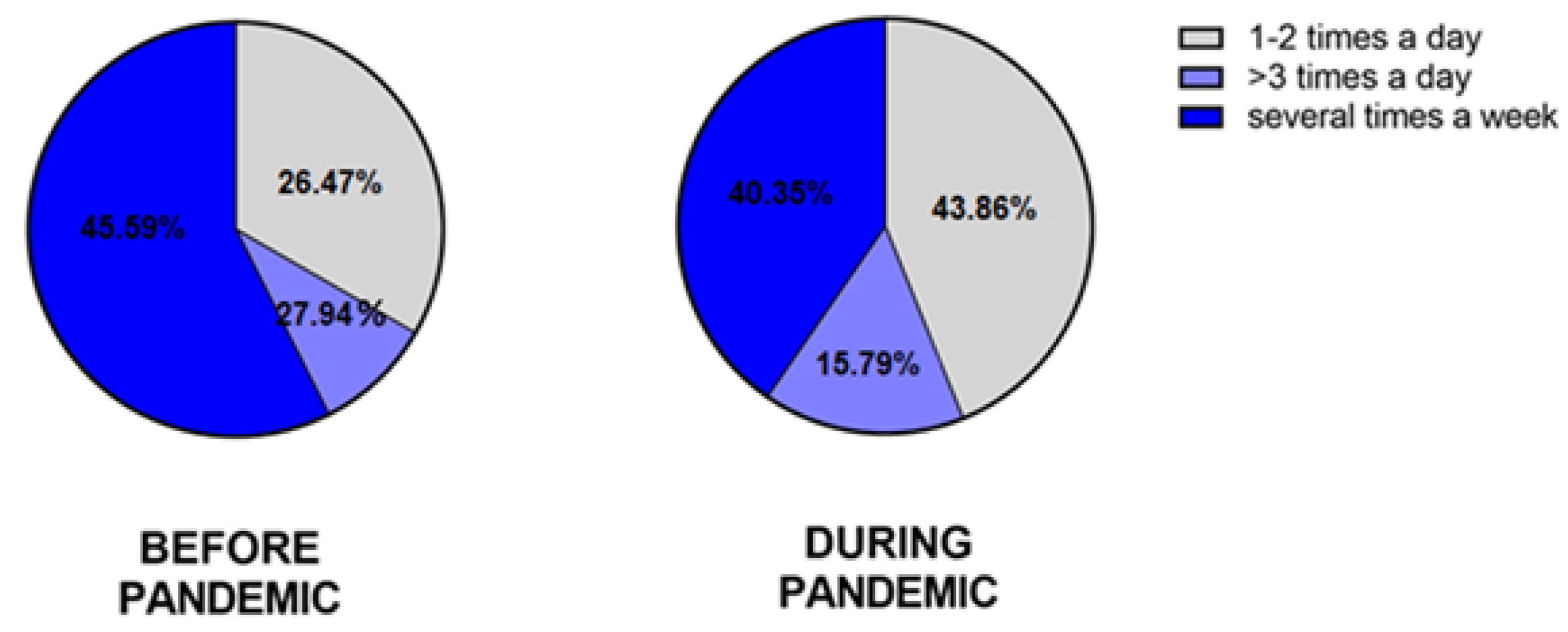
3.2.7. The Moisturizing
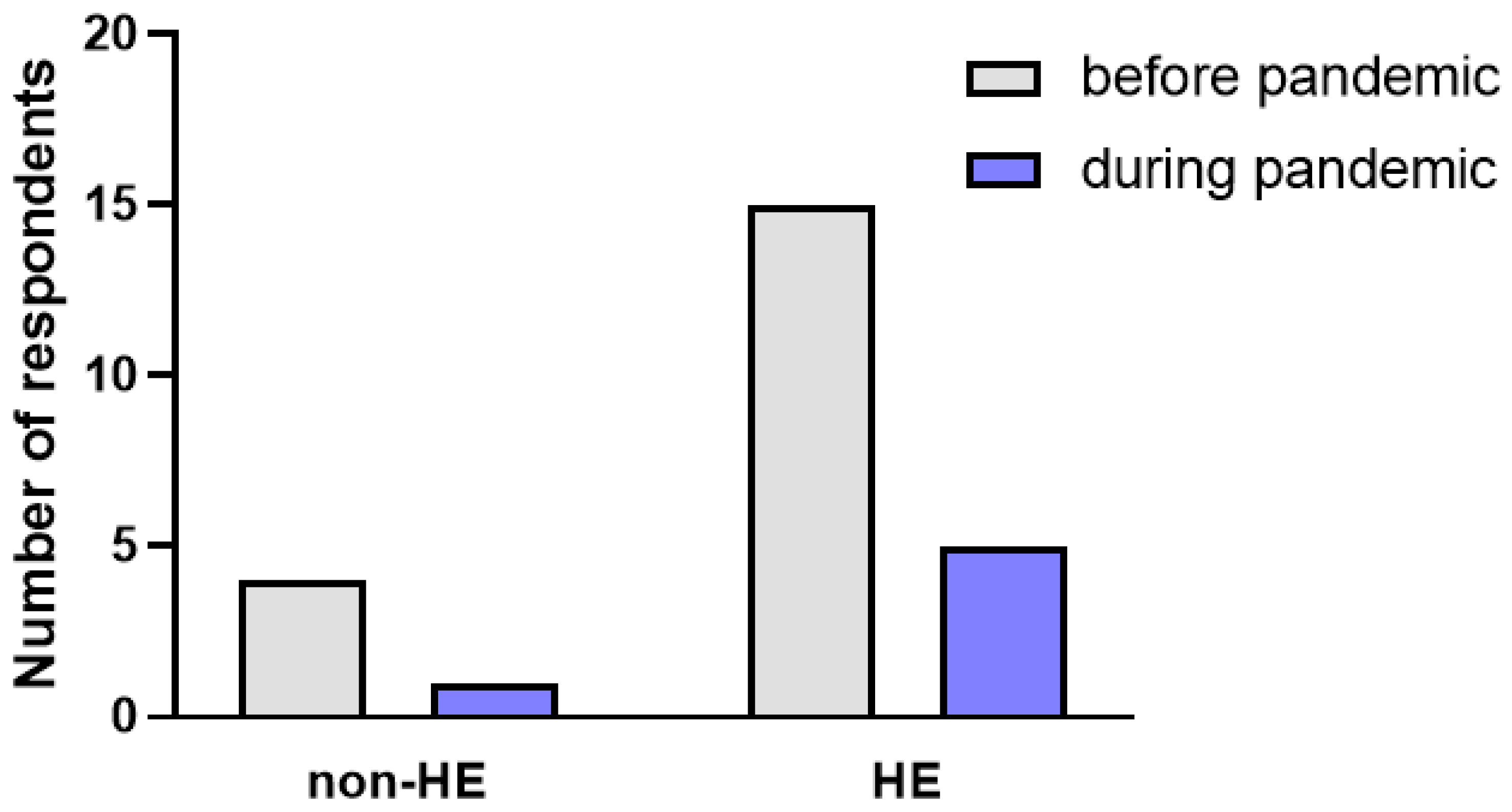
3.2.8. Skin Infection
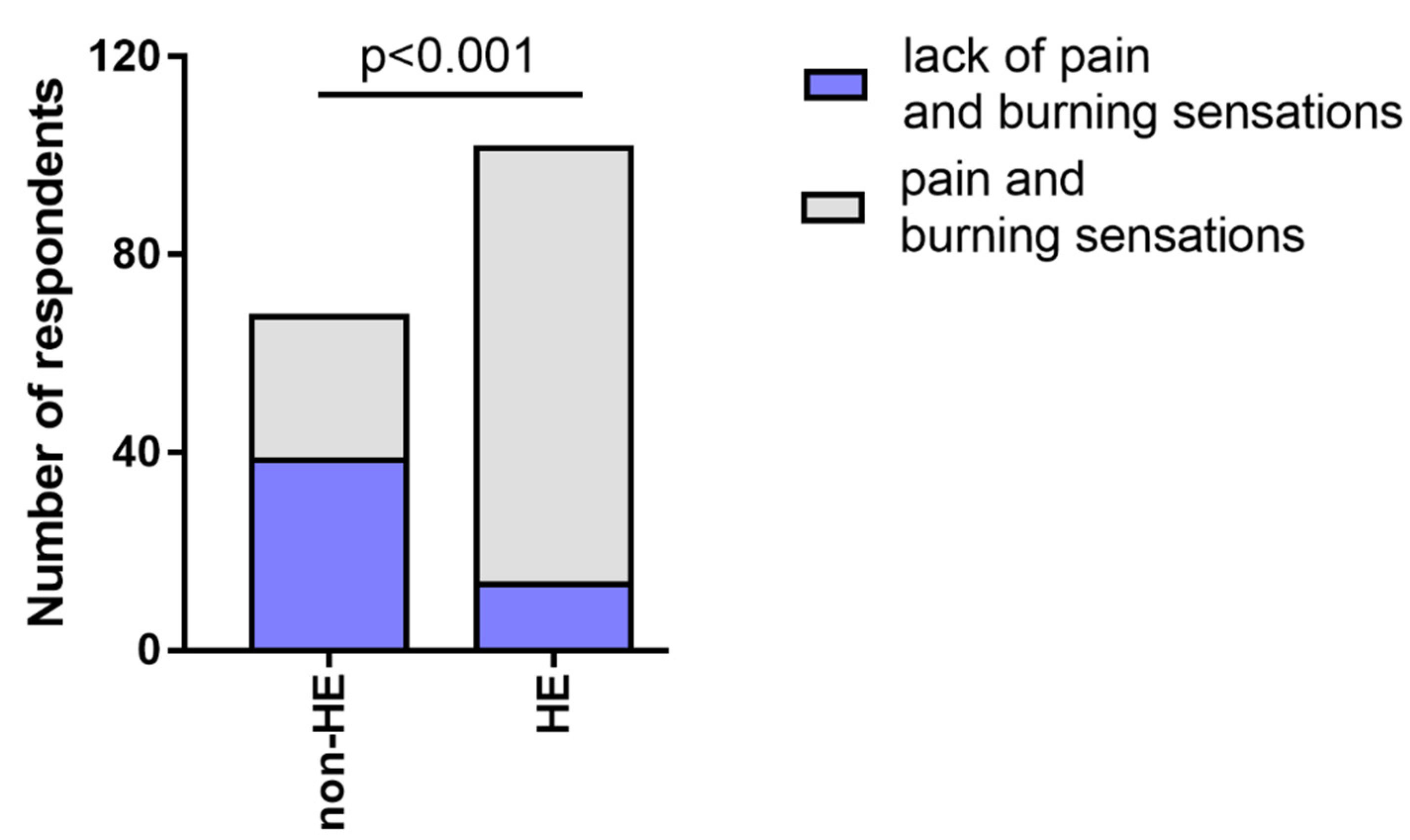
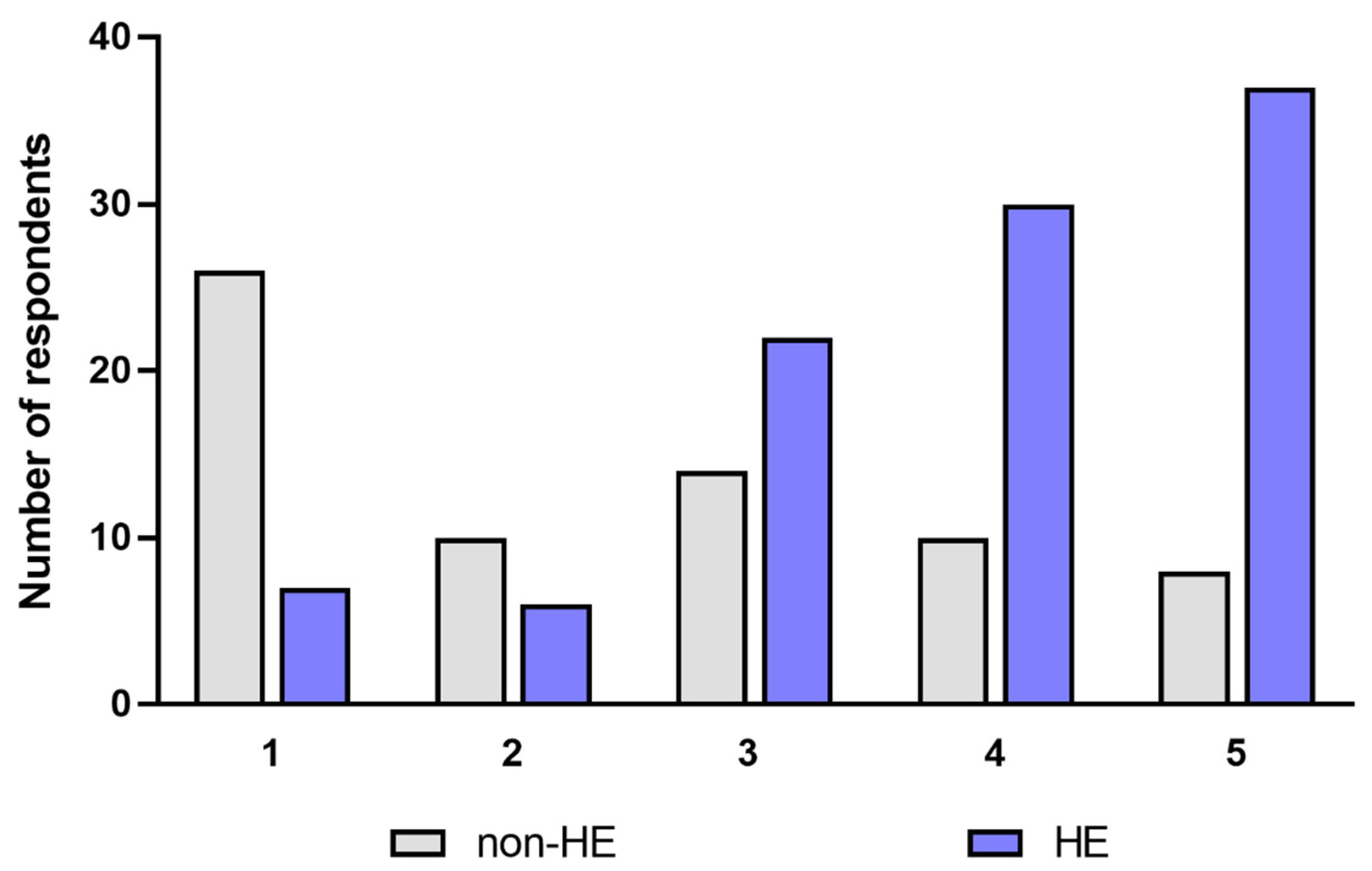
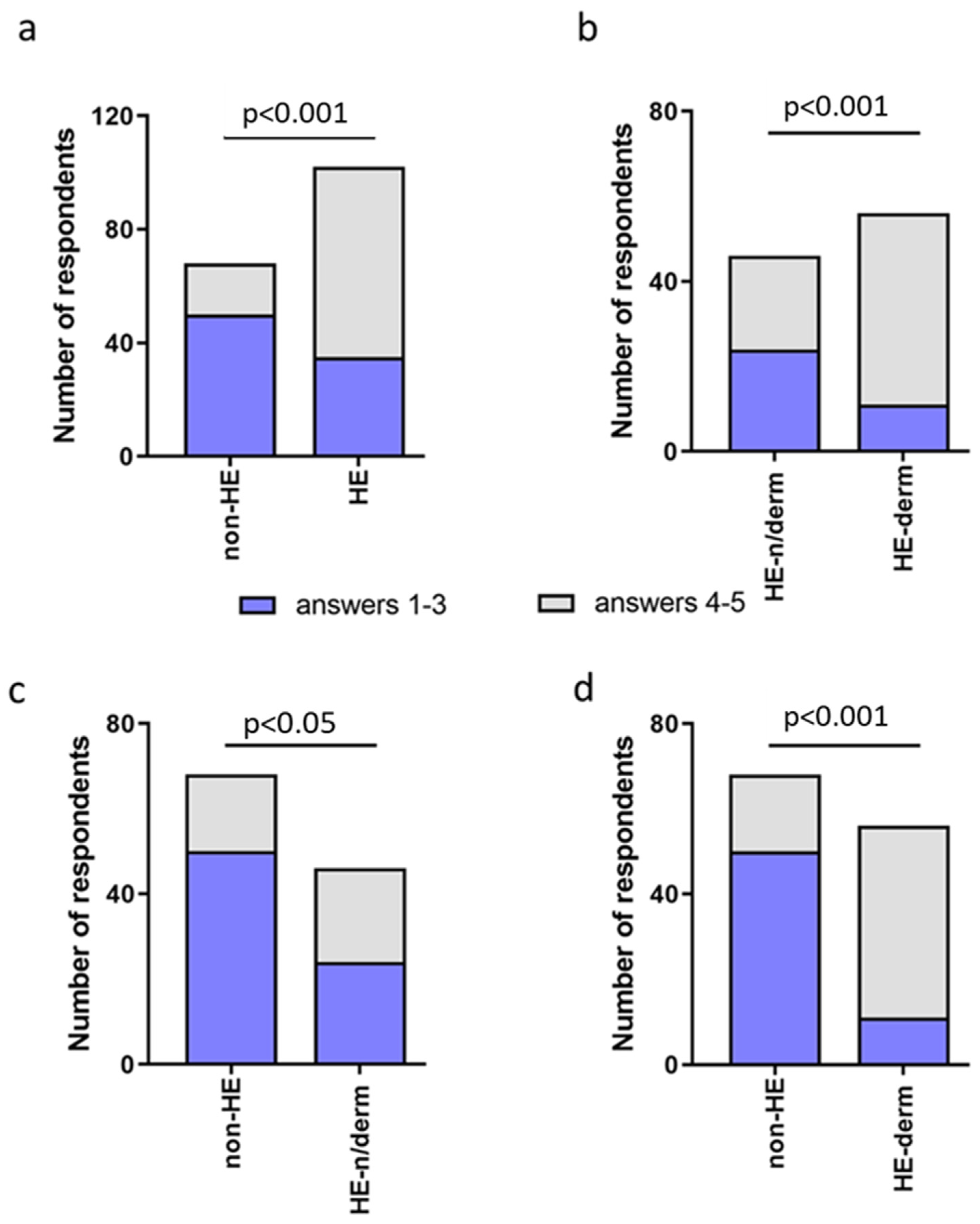
3.2.9. Quality of Life
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Water, Sanitation, Hygiene, and Waste Management for SARS-CoV-2, the Virus that Causes COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-WASH-2020.4 (accessed on 26 January 2021).
- Hirose, R.; Bandou, R.; Ikegaya, H.; Watanabe, N.; Yoshida, T.; Daidoji, T.; Naito, Y.; Itoh, Y.; Nakaya, T. Disinfectant effectiveness against SARS-CoV-2 and influenza viruses present on human skin: Model-based evaluation. Clin. Microbiol. Infect. 2021, 27, 1042. [Google Scholar] [CrossRef]
- Guertler, A.; Moellhoff, N.; Schenck, T.L.; Hagen, C.S.; Kendziora, B.; Giunta, R.E.; French, L.E.; Reinholz, M. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: Comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermat. 2020, 83, 108–114. [Google Scholar] [CrossRef]
- Rundle, C.W.; Presley, C.L.; Militello, M.; Barber, C.; Powell, D.L.; Jacob, S.E.; Atwater, A.R.; Watsky, K.L.; Yu, J.; Dunnick, C.A. Hand hygiene during COVID-19: Recommendations from the American Contact Dermatitis Society. J. Am. Acad. Dermatol. 2020, 83, 1730–1737. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Schuttelaar, M.L.A.; Alfonso, J.H.; Andersen, K.E.; Angelova-Fischer, I.; Arents, B.W.M.; Bauer, A.; Brans, R.; Cannavo, A.; Chiristoffers, W.A.; et al. Guidelines for diagnosis, prevention, and treatment of hand eczema. Contact Dermat. 2021, 86, 333–441. [Google Scholar] [CrossRef]
- Loh, E.W.; Yew, Y.W. Hand hygiene and hand eczema: A systematic review and meta-analysis. Contact Dermat. 2022, 87, 303–314. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Thyssen, J.P.; Paller, A.S.; Drucker, A.M.; Wollenberg, A.; Lee, K.H.; Kabashima, K.; Todd, G.; Schmid-Grendelmeier, P.; Bieber, T. What’s in a name? Atopic dermatitis or atopic eczema, but not eczema alone. Allergy 2017, 72, 2026–2030. [Google Scholar] [CrossRef]
- Quaade, A.S.; Simonsen, A.B.; Halling, A.S.; Thyssen, J.P.; Johansen, J.D. Prevalence, incidence, and severity of hand eczema in the general population—A systematic review and meta-analysis. Contact Dermat. 2021, 84, 361–374. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Johansen, J.D.; Linneberg, A.; Menné, T. The epidemiology of hand eczema in the general population-prevalence and main findings. Contact Dermat. 2010, 62, 75–87. [Google Scholar] [CrossRef]
- Ruff, S.M.D.; Engebretsen, K.A.; Zachariae, C.; Silverberg, J.I.; Egeberg, A.; Thyssen, J.P. The association between atopic dermatitis and hand eczema: A systematic review and meta-analysis. Br. J. Dermatol. 2018, 178, 879–888. [Google Scholar] [CrossRef]
- Mora-Fernández, V.; Mercader, G.P.; Borrego, H.L.; González, P.R.; Córdoba, G.S.; Giménez, A.A.; Ruiz, G.I.; Miquel, M.F.J.; Silvestre, S.J.F.; Ortiz de Frutos, F.J.; et al. Epidemiological, Clinical, and Allergy Profile of Patients with Atopic Dermatitis and Hand Eczema: Evaluation of the Spanish Contact Dermatitis Registry (REIDAC). Actas Dermosifiliogr. 2022, 113, 236–243. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, J.; Sun, S.; Gao, M.; Tong, A. Prevalence and risk factors of hand eczema in hospital-based nurses in northern China. Australas. J. Dermatol. 2018, 59, e194–e197. [Google Scholar] [CrossRef]
- Gasparini, G.; Carmisciano, L.; Giberti, I.; Murgioni, F.; Parodi, A.; Gallo, R. Healthy Hands: A pilot study for the prevention of chronic hand eczema in healthcare workers of an Italian University Hospital. G. Ital. Dermatol. Venereol. 2020, 155, 760–763. [Google Scholar] [CrossRef]
- Hamnerius, N.; Svedman, C.; Bergendorff, O.; Björk, J.; Bruze, M.; Engfeldt, M.; Pontén, A. Hand eczema and occupational contact allergies in healthcare workers with a focus on rubber additives. Contact Dermat. 2018, 79, 149–156. [Google Scholar] [CrossRef]
- Symanzik, C.; Stasielowicz, L.; Brans, R.; Skudlik, C.; John, S.M. Prevention of occupational hand eczema in healthcare workers during the COVID-19 pandemic: A controlled intervention study. Contact Dermat. 2022, 87, 500–510. [Google Scholar] [CrossRef]
- Deleuran, M.; Vestergaard, C. Clinical heterogeneity and differential diagnosis of atopic dermatitis. Br. J. Dermatol. 2014, 170, 2–6. [Google Scholar] [CrossRef]
- Leung, D.Y.; Bieber, T. Atopic dermatitis. Lancet 2003, 361, 151–160. [Google Scholar] [CrossRef]
- Pourani, M.R.; Ganji, R.; Dashti, T.; Dadkhahfar, S.; Gheisari, M.; Abdollahimajd, F.; Dadras, M.S. Impact of COVID-19 Pandemic on Patients with Atopic Dermatitis. Actas Dermosifiliogr. 2021, 20, 286–293. [Google Scholar] [CrossRef]
- Sacotte, R.; Silverberg, J.I. Epidemiology of adult atopic dermatitis. Clin. Dermatol. 2018, 36, 595–605. [Google Scholar] [CrossRef]
- Rendon, A.; Schäkel, K. Psoriasis Pathogenesis and Treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef]
- Machado, Á.; Torres, T. Spotlight on risankizumab and its potential in the treatment of plaque psoriasis: Evidence to date. Psoriasis 2018, 8, 83–92. [Google Scholar] [CrossRef]
- Kendziora, B.; Guertler, A.; Ständer, L.; Frey, S.; French, L.E.; Wollenberg, A.; Reinholz, M. Evaluation of hand hygiene and onset of hand eczema after the outbreak of SARS-CoV-2 in Munich. Eur. J. Dermatol. 2020, 30, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Doğan, E.I.; Birgül, Ö.K. New-Onset or Exacerbated Occupational Hand Eczema among Healthcare Workers during the COVID-19 Pandemic: A Growing Health Problem. Acta Dermatovenerol. Croat. 2021, 291, 21–29. [Google Scholar] [PubMed]
- Babino, G.; Argenziano, G.; Balato, A. Impact in Contact Dermatitis during and after SARS-CoV2 Pandemic. Curr. Treat. Options Allergy 2022, 9, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Pawar, M.; Bothra, A.; Choudhary, N. Overzealous hand hygiene during the COVID 19 pandemic causing an increased incidence of hand eczema among general population. J. Am. Acad. Dermatol. 2020, 83, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Erdem, Y.; Altunay, I.K.; Çerman, A.A.; Inal, S.; Ugurer, E.; Sivaz, O.; Kaya, H.E.; Gulsunay, I.E.; Sekerlisoy, G.; Vural, O.; et al. The risk of hand eczema in healthcare workers during theCOVID-19 pandemic: Do we need specific attention or prevention strategies? Contact Dermat. 2020, 83, 422–423. [Google Scholar] [CrossRef]
- Jindal, R.; Pandhi, D. Hand Hygiene Practices and Risk and Prevention of Hand Eczema during the COVID-19 Pandemic. Indian Dermatol. Online J. 2020, 11, 540–543. [Google Scholar] [CrossRef]
- Techasatian, L.; Thaowandee, W.; Chaiyarit, J.; Uppala, R.; Sitthikarnkha, P.; Paibool, W.; Charoenwat, B.; Wongmast, P.; Laoaroon, N.; Suphakunpinyo, C.; et al. Hand Hygiene Habits and Prevalence of Hand Eczema During the COVID-19 Pandemic. J. Prim. Care Community Health 2021, 12, 21501327211018013. [Google Scholar] [CrossRef]
- Agner, T.; Elsner, P. Hand eczema: Epidemiology, prognosis and prevention. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 4–12. [Google Scholar] [CrossRef]
- Diepgen, T.L.; Andersen, K.E.; Chosidow, O.; Coenraads, P.J.; Elsner, P.; English, J.; Fartasch, M.; Gimenez-Arnau, A.; Nixon, R.; Sasseville, D.; et al. Guidelines for diagnosis, prevention and treatment of hand eczema—Short version. J. Dtsch. Dermatol. Ges. 2015, 13, e1–e22. [Google Scholar] [CrossRef]
- Molin, S. Pathogenesis of hand eczema. Hautarzt 2019, 70, 755–759. [Google Scholar] [CrossRef]
- Ong, P.Y.; Leung, D.Y.M. Bacterial and Viral Infections in Atopic Dermatitis: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2016, 51, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Haslund, P.; Bangsgaard, N.; Jarløv, J.O.; Skov, L.; Skov, R.; Agner, T. Staphylococcus aureus and hand eczema severity. Br. J. Dermatol. 2009, 161, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Sachdeva, M.; Alavi, A.; Shi, V.Y.; Hsiao, J.L. Optimizing care for atopic dermatitis patients during the COVID-19 pandemic. J. Am. Acad. Dermatol. 2020, 83, e165–e167. [Google Scholar] [CrossRef] [PubMed]
- Blicharz, L.; Czuwara, J.; Samochocki, Z.; Goldust, M.; Chrostowska, S.; Olszewska, M.; Rudnicka, L. Hand eczema—A growing dermatological concern during the COVID-19 pandemic and possible treatments. Dermatol. Ther. 2020, 33, e13545. [Google Scholar] [CrossRef]
- Reich, A.; Wójcik-Maciejewicz, A.; Slominski, A.T. Stress and the skin. G. Ital. Dermatol. Venereol. 2010, 145, 213–219. [Google Scholar]
- Lewicka, M.; Hamilton, J.G.; Waters, E.A.; Orom, H.; Schofield, E.; Kiviniemi, M.T.; Kanetsky, P.A.; Hay, J.L. Associations between social COVID-19 exposure and psychological functioning. J. Behav. Med. 2022, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Arndt, J.; Smith, N.; Tausk, F. Stress and Atopic Dermatitis. Curr. Allergy Asthma Rep. 2008, 8, 312–317. [Google Scholar] [CrossRef]
- Kodama, A.; Horikawa, T.; Suzuki, T.; Ajiki, W.; Takashima, T.; Harada, S.; Ichihashi, M. Effect of stress on atopic dermatitis: Investigation in patients after the great hanshin earthquake. J. Allergy Clin. Immunol. 1999, 104, 173–176. [Google Scholar] [CrossRef]
- Koo, J.Y.M.; Lee, C.S. General approach to evaluating psychodermatological disorders. In Psychocutaneous Medicine; Koo, J.Y.M., Lee, C.S., Eds.; Marcel Dekker: New York, NY, USA, 2003; pp. 1–29. [Google Scholar]
- Elias, P.M.; Sun, R.; Eder, A.R.; Wakefieldet, J.S.; Man, M.-Q. Treating atopic dermatitis at the source: Corrective barrier repair therapy based upon new pathogenic insights. Expert Rev. Dermatol. 2013, 8, 27–36. [Google Scholar] [CrossRef]
- Jafferany, M.; Ferreira, B.R.; Abdelmaksoud, A.; Mkhoyan, R. Management of psychocutaneous disorders: A practical approach for dermatologists. Dermatol. Ther. 2020, 33, e13969. [Google Scholar] [CrossRef]
- Senra, M.S.; Wollenberg, A. Psychodermatological aspects of atopic dermatitis. Br. J. Dermatol. 2014, 170, 38–43. [Google Scholar] [CrossRef]



| Characteristics | N (%) |
|---|---|
| Gender | |
| Female | 142 (83.53%) |
| Male | 28 (16.47%) |
| Age (years) | |
| 18–24 | 89 (52.35%) |
| 25–36 | 70 (41.18%) |
| 36–45 | 5 (2.94%) |
| >45 | 6 (3.53%) |
| Education | |
| Primary | 2 (1.18%) |
| Secondary | 84 (49.41%) |
| Higher | 84 (49.41%) |
| Residence | |
| Rural | 21 (12.35%) |
| City to 250.000 inhabitants | 54 (31.77%) |
| City with more than 250.000 inhabitants | 95 (55.88%) |
| Hand Skin Dermatoses | N (%) |
|---|---|
| Hand eczema | 56 (100.00%) |
| Atopic dermatitis | 33 (58.93%) |
| Hand and nail psoriasis | 8 (14.29%) |
| HE-Study Group, N (%) | Non-HE, N (%) | |
|---|---|---|
| Number of respondents | 81 (79.41%) | 7 (10.29%) |
| New symptom | ||
| Dryness | 62 (60.78%) | 3 (4.41%) |
| Roughness | 53 (51.96%) | 2 (2.94%) |
| Redness | 40 (39.22%) | 0 |
| Vesicles filled with serum fluid | 7 (6.86%) | 0 |
| Pus-filled pustules | 5 (4.90%) | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polecka, A.; Owsianko, N.; Awchimkow, A.; Baran, A.; Hermanowicz, J.M.; Flisiak, I. Questionnaire-Based Study Evaluating the Hand Hygiene Practices and the Impact of Disinfection in the COVID-19 Pandemic on Hand Skin Conditions in Poland. J. Clin. Med. 2023, 12, 195. https://doi.org/10.3390/jcm12010195
Polecka A, Owsianko N, Awchimkow A, Baran A, Hermanowicz JM, Flisiak I. Questionnaire-Based Study Evaluating the Hand Hygiene Practices and the Impact of Disinfection in the COVID-19 Pandemic on Hand Skin Conditions in Poland. Journal of Clinical Medicine. 2023; 12(1):195. https://doi.org/10.3390/jcm12010195
Chicago/Turabian StylePolecka, Agnieszka, Natalia Owsianko, Andrzej Awchimkow, Anna Baran, Justyna Magdalena Hermanowicz, and Iwona Flisiak. 2023. "Questionnaire-Based Study Evaluating the Hand Hygiene Practices and the Impact of Disinfection in the COVID-19 Pandemic on Hand Skin Conditions in Poland" Journal of Clinical Medicine 12, no. 1: 195. https://doi.org/10.3390/jcm12010195
APA StylePolecka, A., Owsianko, N., Awchimkow, A., Baran, A., Hermanowicz, J. M., & Flisiak, I. (2023). Questionnaire-Based Study Evaluating the Hand Hygiene Practices and the Impact of Disinfection in the COVID-19 Pandemic on Hand Skin Conditions in Poland. Journal of Clinical Medicine, 12(1), 195. https://doi.org/10.3390/jcm12010195









