Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Computed Tomography Technique
2.3. Radiological Assessment
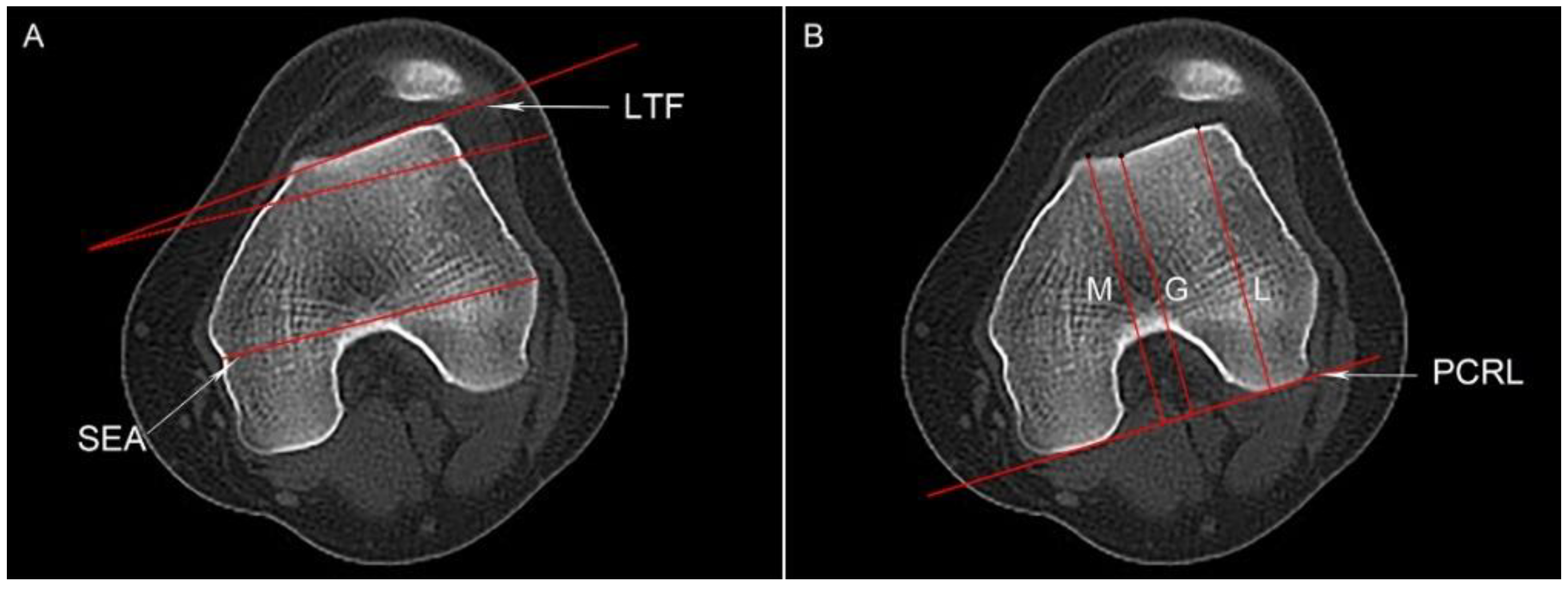
2.3.1. Trochlear Dysplasia
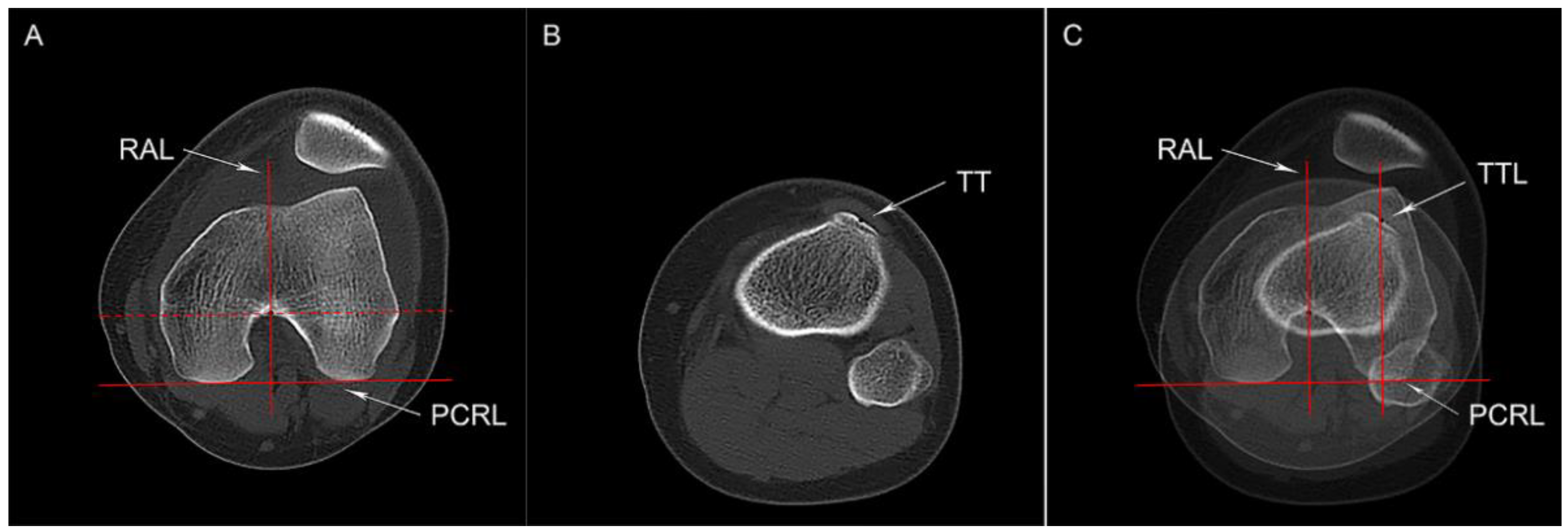
2.3.2. Tibial Tubercle Lateralization
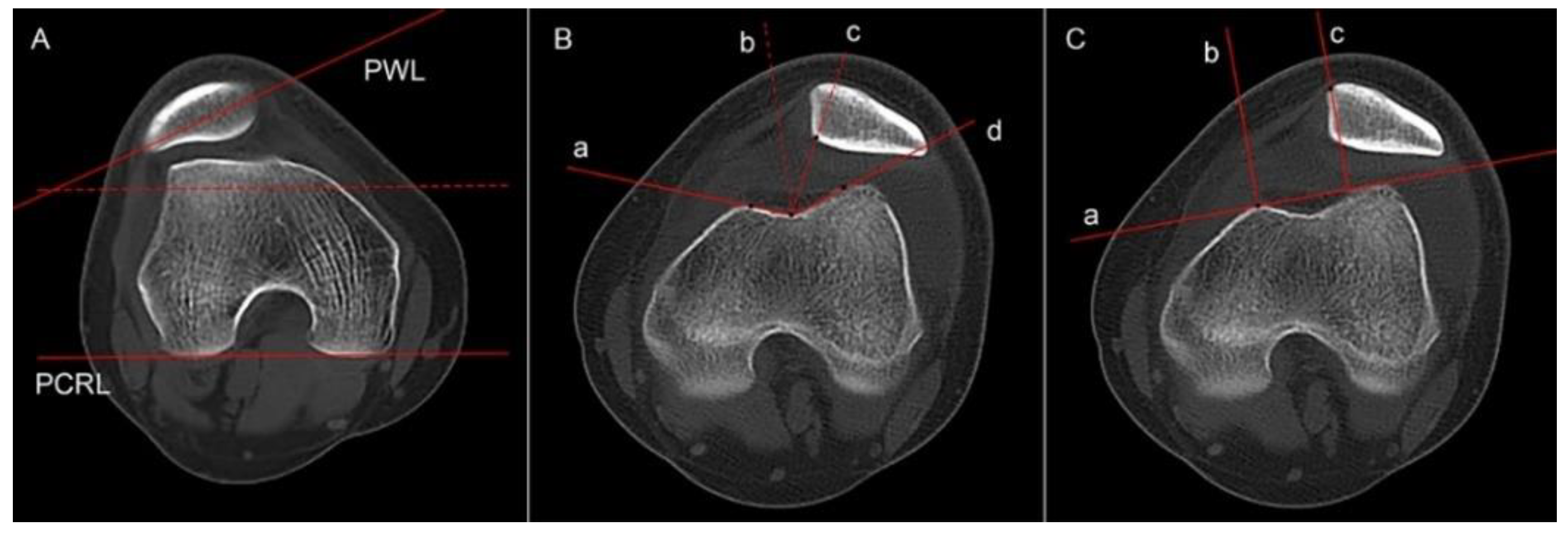
2.3.3. Femoral Anteversion
2.3.4. Knee Joint Rotation and Tibial Torsion
2.3.5. Patellar Height and HKA Angle
2.3.6. Patella Position Relative to the Trochlea
2.4. Statistical Analysis
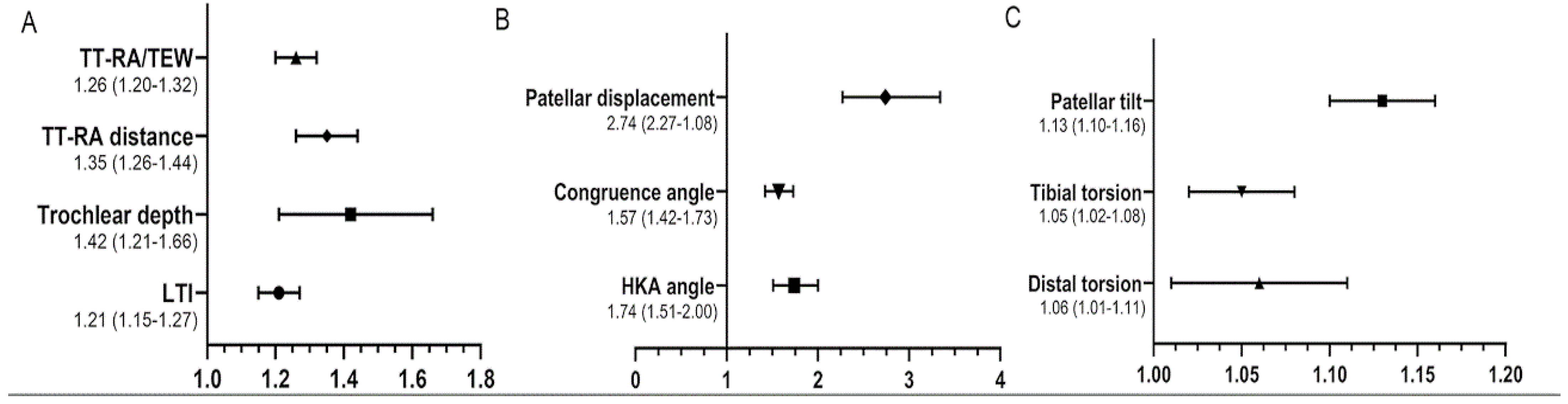
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and natural history of acute patellar dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Uimonen, M.M.; Repo, J.P.; Huttunen, T.T.; Nurmi, H.; Mattila, V.M.; Paloneva, J. Surgery for patellar dislocation has evolved towards anatomical reconstructions with assessment and treatment of anatomical risk factors. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1944–1951. [Google Scholar] [CrossRef]
- Gravesen, K.S.; Kallemose, T.; Blønd, L.; Troelsen, A.; Barfod, K.W. High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1204–1209. [Google Scholar] [CrossRef] [PubMed]
- Christensen, T.C.; Sanders, T.L.; Pareek, A.; Mohan, R.; Dahm, D.L.; Krych, A.J. Risk Factors and Time to Recurrent Ipsilateral and Contralateral Patellar Dislocations. Am. J. Sports Med. 2017, 45, 2105–2110. [Google Scholar] [CrossRef] [PubMed]
- Xiong, R.; Chen, C.; Yin, L.; Gong, X.; Luo, J.; Wang, F.; Yang, L.; Guo, L. How Do Axial Scan Orientation Deviations Affect the Measurements of Knee Anatomical Parameters Associated with Patellofemoral Instability? A Simulated Computed Tomography Study. J. Knee Surg. 2018, 31, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Balcarek, P.; Zimmermann, F. Deepening trochleoplasty and medial patellofemoral ligament reconstruction normalize patellotrochlear congruence in severe trochlear dysplasia. Bone Jt. J. 2019, 101-B, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Ahrend, M.D.; Eisenmann, T.; Herbst, M.; Gueorguiev, B.; Keller, G.; Schmidutz, F.; Döbele, S.; Schröter, S.; Ihle, C. Increased tibial tubercle-trochlear groove and patellar height indicate a higher risk of recurrent patellar dislocation following medial reefing. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1404–1413. [Google Scholar] [CrossRef]
- Pruneski, J.; O’Mara, L.; Perrone, G.S.; Kiapour, A.M. Changes in Anatomic Risk Factors for Patellar Instability During Skeletal Growth and Maturation. Am. J. Sports Med. 2022, 50, 2424–2432. [Google Scholar] [CrossRef]
- Geraghty, L.; Zordan, R.; Walker, P.; Chao, T.W.; Talbot, S. Patellar dislocation is associated with increased tibial but not femoral rotational asymmetry. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2342–2351. [Google Scholar] [CrossRef]
- Simonaitytė, R.; Rutkauskas, S.; Čekanauskas, E.; Labanauskas, L.; Barauskas, V. First-Time Acute Lateral Patellar Dislocation in Children and Adolescents: What About Unaffected Knee Patellofemoral Joint Anatomic Abnormalities? Medicina 2021, 57, 206. [Google Scholar] [CrossRef]
- Chen, J.; Huang, X.; Xu, Z.; Zhang, H.; Zhou, A.; Zhao, P.; Yin, L. Ipsilateral patellofemoral morphological abnormalities are more severe than those of contralateral joints in patients with unilateral patellar dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2709–2716. [Google Scholar] [CrossRef]
- Jaquith, B.P.; Parikh, S.N. Predictors of Recurrent Patellar Instability in Children and Adolescents After First-time Dislocation. J. Pediatr. Orthop. 2017, 37, 484–490. [Google Scholar] [CrossRef]
- Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Demehri, S.; Thawait, G.K.; Williams, A.A.; Kompel, A.; Elias, J.J.; Carrino, J.A.; Cosgarea, A.J. Imaging characteristics of contralateral asymptomatic patellofemoral joints in patients with unilateral instability. Radiology 2014, 273, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Lippacher, S.; Dejour, D.; Elsharkawi, M.; Dornacher, D.; Ring, C.; Dreyhaupt, J.; Reichel, H.; Nelitz, M. Observer agreement on the Dejour trochlear dysplasia classification: A comparison of true lateral radiographs and axial magnetic resonance images. Am. J. Sports Med. 2012, 40, 837–843. [Google Scholar] [CrossRef]
- Paiva, M.; Blønd, L.; Hölmich, P.; Steensen, R.N.; Diederichs, G.; Feller, J.A.; Barfod, K.W. Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 746–755. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Zhang, H.; Fu, B.; Mohamed, S.I.; Zhang, J.; Zhou, A. Tibial Tubercle-Roman Arch Distance: A New Measurement of Patellar Dislocation and Indication of Tibial Tubercle Osteotomy. Orthop. J. Sports Med. 2020, 8, 2325967120914872. [Google Scholar] [CrossRef]
- Chen, J.; Yin, B.; Yao, J.; Zhou, Y.; Zhang, H.; Zhang, J.; Zhou, A. Femoral anteversion measured by the surgical transepicondylar axis is a reliable parameter for evaluating femoral rotational deformities in patients with patellar dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2022, 1–9. [Google Scholar] [CrossRef]
- Chen, J.; Wu, C.; Ye, Z.; Zhao, J.; Xie, G. Tibial Tuberosity-Trochlear Groove Distance and Its Components in Patients with and without Episodic Patellar Dislocation: A Study of 781 Knees. J. Bone Joint Surg. Am. 2022, 104, 504–511. [Google Scholar] [CrossRef]
- Xu, C.; Cui, Z.; Yan, L.; Chen, Z.; Wang, F. Anatomical Components Associated with Increased Tibial Tuberosity-Trochlear Groove Distance. Orthop. J. Sports Med. 2022, 10, 23259671221113841. [Google Scholar] [CrossRef]
- Parikh, S.N.; Redman, C.; Gopinathan, N.R. Simultaneous treatment for patellar instability and genu valgum in skeletally immature patients: A preliminary study. J. Pediatr. Orthop. B 2019, 28, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Ling, D.I.; Brady, J.M.; Arendt, E.; Tompkins, M.; Agel, J.; Askenberger, M.; Balcarek, P.; Parikh, S.; Shubin Stein, B.E. Development of a Multivariable Model Based on Individual Risk Factors for Recurrent Lateral Patellar Dislocation. J. Bone Joint Surg. Am. 2021, 103, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Yin, H.; Xu, C.; Zhang, H.; Guo, A.; Diao, N. Association of patellofemoral morphology and alignment with the radiographic severity of patellofemoral osteoarthritis. J. Orthop. Surg. Res. 2021, 16, 548. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.K.; Wang, X.M.; Niu, Y.Z.; Liu, H.X.; Wang, F. Relationship between Patellar Tracking and the “Screw-home” Mechanism of Tibiofemoral Joint. Orthop. Surg. 2016, 8, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Nelitz, M.; Lippacher, S.; Reichel, H.; Dornacher, D. Evaluation of trochlear dysplasia using MRI: Correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 120–127. [Google Scholar] [CrossRef]
- Huntington, L.S.; Webster, K.E.; Devitt, B.M.; Scanlon, J.P.; Feller, J.A. Factors Associated with an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2020, 48, 2552–2562. [Google Scholar] [CrossRef]
- Parikh, S.N.; Lykissas, M.G.; Gkiatas, I. Predicting Risk of Recurrent Patellar Dislocation. Curr. Rev. Musculoskelet. Med. 2018, 11, 253–260. [Google Scholar] [CrossRef]
- Stephen, J.M.; Lumpaopong, P.; Dodds, A.L.; Williams, A.; Amis, A.A. The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am. J. Sports Med. 2015, 43, 186–194. [Google Scholar] [CrossRef]
- Hinz, M.; Cotic, M.; Diermeier, T.; Imhoff, F.B.; Feuerriegel, G.C.; Woertler, K.; Themessl, A.; Imhoff, A.B.; Achtnich, A. Derotational distal femoral osteotomy for patients with recurrent patellar instability and increased femoral antetorsion improves knee function and adequately treats both torsional and valgus malalignment. Knee Surg. Sports Traumatol. Arthrosc. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.; Schmoelz, W.; Schoettle, P.; Zwierzina, M.; Heinrichs, C.; Attal, R. Increased internal femoral torsion can be regarded as a risk factor for patellar instability—A biomechanical study. Clin. Biomech. 2017, 47, 103–109. [Google Scholar] [CrossRef]
- Takagi, S.; Sato, T.; Watanabe, S.; Tanifuji, O.; Mochizuki, T.; Omori, G.; Endo, N. Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2891–2898. [Google Scholar] [CrossRef] [PubMed]

| Study Group (n = 17) | Control Group (n = 34) | p Value | |
|---|---|---|---|
| Sex, n | n.s | ||
| Female | 12 | 24 | |
| Male | 5 | 10 | |
| Age, median (IQR), y | 19.2 (7.0) | 19.0 (7.0) | n.s |
| Skeletal maturity, n% | 35.3% | 35.3% | n.s |
| Side of knee, n | 0.569 a | ||
| Left | 9 | 15 | |
| Right | 8 | 19 | |
| Interval time, month | 46 (IQR, 18) | - | - |
| Inter-Observer 1 | Inter-Observer 2 | Intra-Observer 1 | Intra-Observer 2 | |
|---|---|---|---|---|
| Dejour classification a | 0.91 (0.85, 0.95) | 0.94 (0.88, 0.97) | 0.93 (0.85, 0.96) | 0.87 (0.74, 0.94) |
| LTI | 0.88 (0.83, 0.93) | 0.85 (0.77, 0.92) | 0.86 (0.79, 0.91) | 0.90 (0.85, 0.94) |
| Trochlear depth | 0.78 (0.66, 0.85) | 0.80 (0.68, 0.89) | 0.82 (0.77, 0.90) | 0.80 (0.69, 0.88) |
| TT-RA distance | 0.91 (0.83, 0.93) | 0.88 (0.84, 0.92) | 0.83 (0.75, 0.91) | 0.95 (0.92, 0.98) |
| Total femoral torsion | 0.93 (0.88, 0.96) | 0.94 (0.89, 0.97) | 0.85 (0.74, 0.92) | 0.93 (0.89, 0.97) |
| Neck torsion | 0.95 (0.92, 0.98) | 0.94 (0.91, 0.96) | 0.96 (0.94, 0.98) | 0.97 (0.95, 0.98) |
| Mid torsion | 0.93 (0.88, 0.97) | 0.91 (0.85, 0.94) | 0.90 (0.82, 0.94) | 0.92 (0.87, 0.98) |
| Distal torsion | 0.95 (0.91, 0.98) | 0.94 (0.90, 0.97) | 0.90 (0.83, 0.94) | 0.96 (0.94, 0.98) |
| Knee joint rotation | 0.93 (0.88, 0.97) | 0.89 (0.79, 0.94) | 0.93 (0.85, 0.97) | 0.96 (0.92, 0.99) |
| Tibial torsion | 0.96 (0.94, 0.99) | 0.93 (0.90, 0.96) | 0.97 (0.95, 0.99) | 0.92 (0.86, 0.95) |
| PCA | 0.94 (0.89, 0.96) | 0.93 (0.85, 0.97) | 0.87 (0.78, 0.92) | 0.96 (0.93, 0.99) |
| TEW | 0.96 (0.93, 0.99) | 0.92 (0.83, 0.96) | 0.91 (0.80, 0.95) | 0.94 (0.87, 0.99) |
| Patellar height | 0.90 (0.83, 0.96) | 0.89 (0.81, 0.94) | 0.82 (0.74, 0.91) | 0.91 (0.82, 0.98) |
| HKA angle | 0.95 (0.87, 0.98) | 0.92 (0.83, 0.97) | 0.87 (0.75, 0.94) | 0.92 (0.88, 0.97) |
| Patellar tilt | 0.88 (0.81, 0.93) | 0.86 (0.77, 0.94) | 0.91 (0.84, 0.95) | 0.93 (0.84, 0.97) |
| Congruence angle | 0.87 (0.81, 0.95) | 0.91 (0.85, 0.96) | 0.92 (0.83, 0.96) | 0.89 (0.82, 0.94) |
| Patellar displacement | 0.93 (0.85, 0.97) | 0.91 (0.85, 0.94) | 0.88 (0.78, 0.93) | 0.92 (0.86, 0.97) |
| Study Group | Control Group | p Value | |
|---|---|---|---|
| LTI, ° | 11.9 (9.4–13.6) | 13.9 (11.1–16.2) | <0.001 |
| Trochlear depth, mm | 3.8 (2.6–4.2) | 4.1 (3.3–4.5) | <0.001 |
| TT-RA distance, mm | 24.1 (20.9–25.7) | 19.5 (17.9–22.2) | <0.001 |
| Total femoral torsion, ° | 19.2 (14.7–22.7) | 18.5(16.6–21.3) | 0.551 |
| Neck torsion, ° | 23.3 (20.2–25.3) | 22.3 (19.1–25.4) | 0.375 |
| Mid torsion, ° | 27.1 (26.3–29.5) | 27.2 (24.6–29.8) | 0.302 |
| Distal torsion, ° | 14.4 (11.1–16.6) | 14.6 (10.9–18.3) | 0.057 |
| Knee joint rotation, ° | 9.5 (7.3–12.1) | 9.4 (7.4–12.6) | 0.295 |
| Tibial torsion, ° | 32.1 (28.7–35.5) | 30.8 (23.1–32.7) | 0.001 |
| PCA, ° | 4.4 (2.2–5.4) | 4.4 (2.8–4.7) | 0.867 |
| TEW, mm | 72.7 (70.2–74.6) | 73.1 (70.3–74.9) | 0.122 |
| Patellar height | 1.32 (1.22–1.39) | 1.34 (1.12–1.50) | 0.863 |
| HKA angle, ° | 1.9 (1.3–2.8) | 0.8 (−0.5–1.8) | <0.001 |
| Patellar tilt, ° | 23.9 (20.9–33.1) | 17.8 (13.5–22.4) | <0.001 |
| Congruence angle, ° | 10.2 (9.0–13.0) | 9.2 (6.5–10.5) | <0.001 |
| Patellar displacement, mm | 9.9 (9.3–11.0) | 7.6 (6.4–9.9) | <0.001 |
| TT-RA/TEW, % | 32.7 (29.8–34.9) | 27.6 (24.6–31.3) | <0.001 |
| Dejour classification (A/B/C/D) | 1/2/7/7 | 4/12/12/6 | <0.001 a |
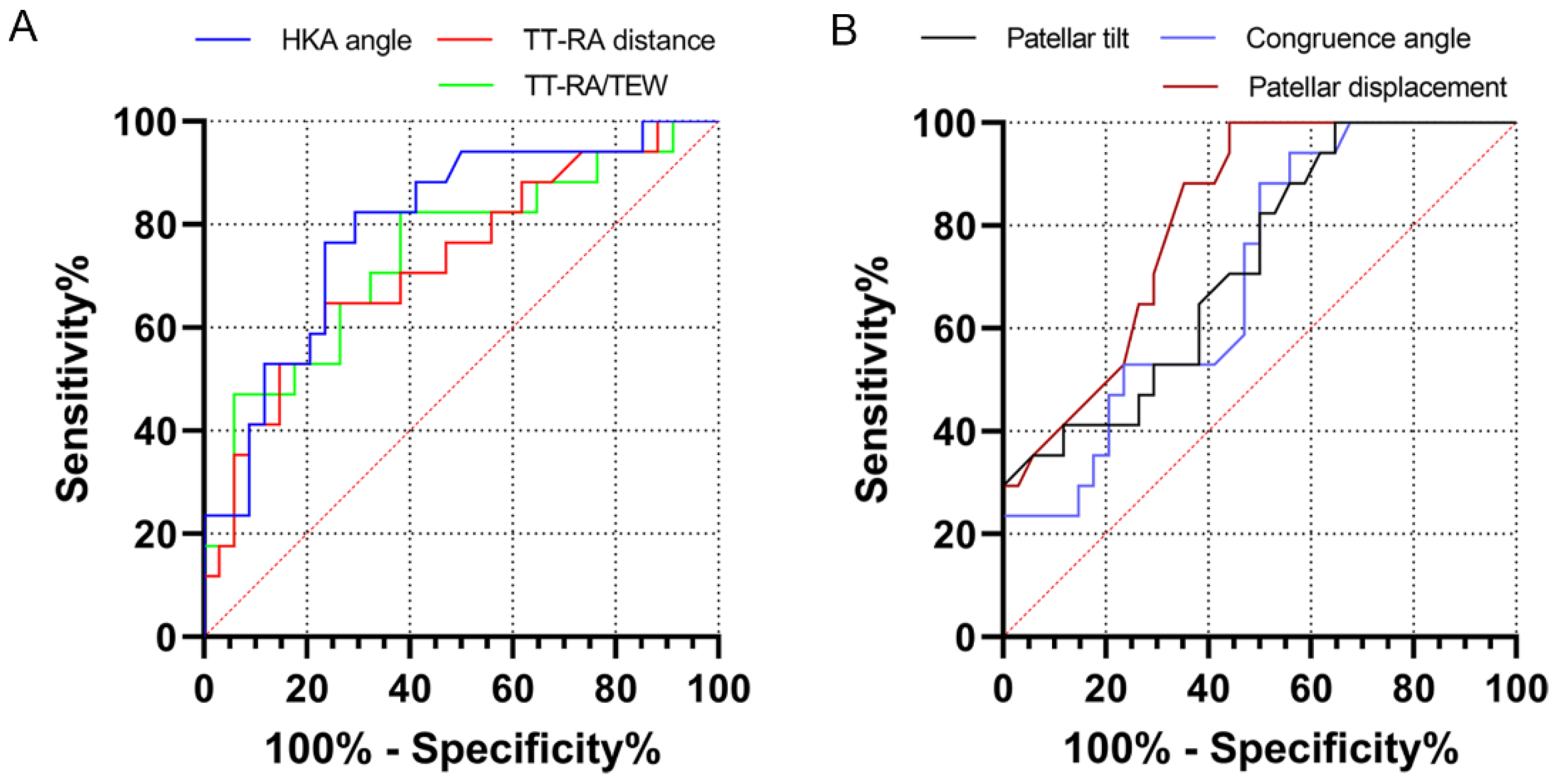
| Variables | AUC | p Value | Cutoff Value | Sensitivity, % | Specificity, % |
|---|---|---|---|---|---|
| LTI | 0.669 | 0.051 | - | - | - |
| Trochlear depth | 0.593 | 0.285 | - | - | - |
| TT-RA distance | 0.727 | 0.009 | 20.0 | 82.3 | 44.1 |
| Distal torsion | 0.548 | 0.583 | - | - | - |
| Tibial rotation | 0.545 | 0.603 | - | - | - |
| HKA angle | 0.797 | <0.001 | 1.3 | 82.4 | 70.6 |
| Patellar tilt | 0.703 | 0.019 | 19.0 | 88.2 | 50.0 |
| Congruence angle | 0.725 | 0.009 | 8.7 | 82.4 | 51.1 |
| Patellar displacement | 0.817 | <0.001 | 9.2 | 88.2 | 64.7 |
| TT-RA/TEW | 0.741 | 0.006 | 29.5 | 83.3 | 61.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Li, Q.; Liu, S.; Fan, L.; Yin, B.; Yang, X.; Wang, L.; Xu, Z.; Zhang, J.; Quan, Z.; et al. Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies. J. Clin. Med. 2023, 12, 180. https://doi.org/10.3390/jcm12010180
Chen J, Li Q, Liu S, Fan L, Yin B, Yang X, Wang L, Xu Z, Zhang J, Quan Z, et al. Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies. Journal of Clinical Medicine. 2023; 12(1):180. https://doi.org/10.3390/jcm12010180
Chicago/Turabian StyleChen, Jiaxing, Qiaochu Li, Sizhu Liu, Lin Fan, Baoshan Yin, Xinyu Yang, Linbang Wang, Zijie Xu, Jian Zhang, Zhengxue Quan, and et al. 2023. "Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies" Journal of Clinical Medicine 12, no. 1: 180. https://doi.org/10.3390/jcm12010180
APA StyleChen, J., Li, Q., Liu, S., Fan, L., Yin, B., Yang, X., Wang, L., Xu, Z., Zhang, J., Quan, Z., & Zhou, A. (2023). Prediction of Subsequent Contralateral Patellar Dislocation after First-Time Dislocation Based on Patellofemoral Morphologies. Journal of Clinical Medicine, 12(1), 180. https://doi.org/10.3390/jcm12010180





