Which Surgery for Stage II–III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients †
Abstract
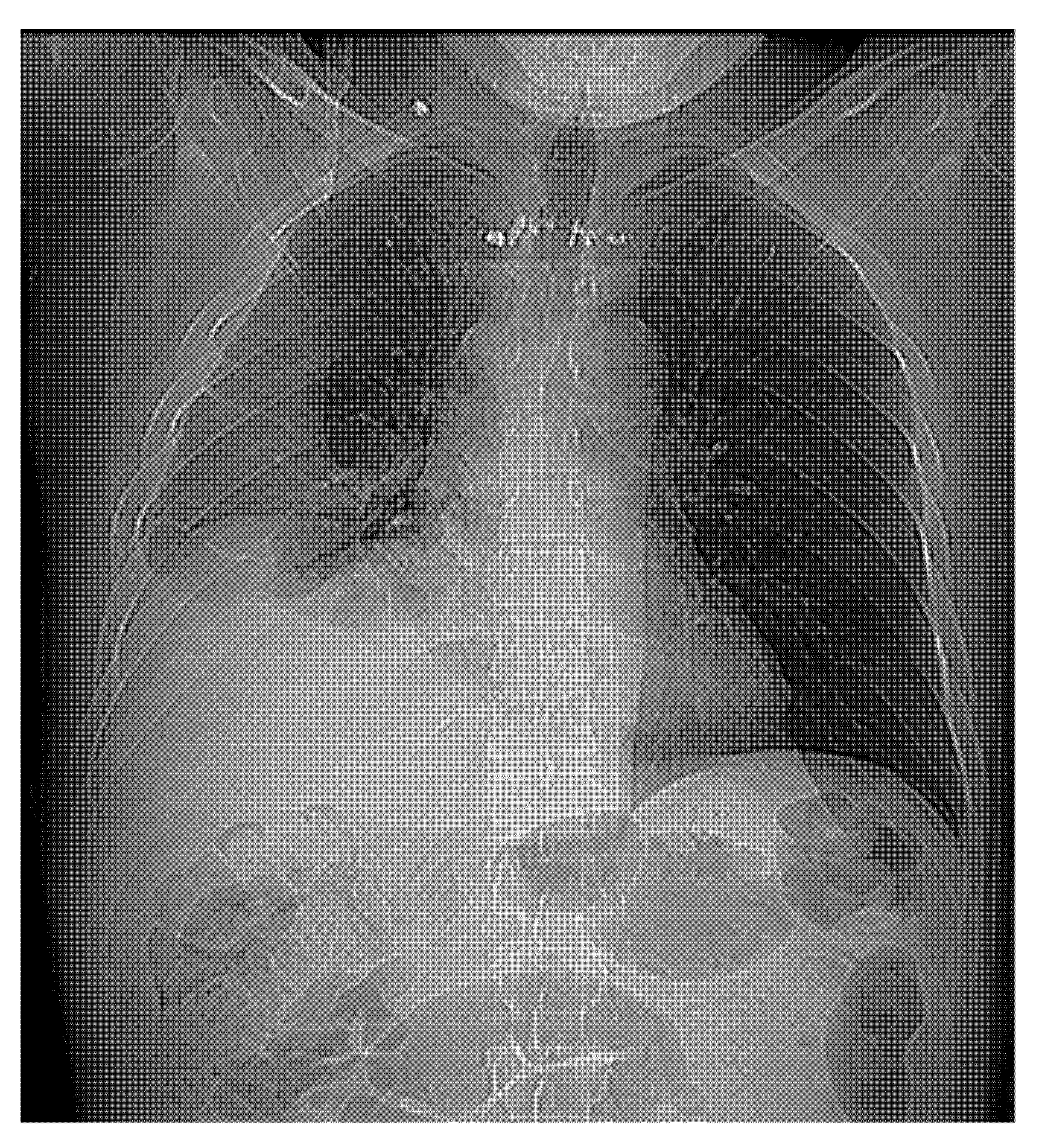
1. Introduction
2. Materials and Methods
2.1. Surgical Technique
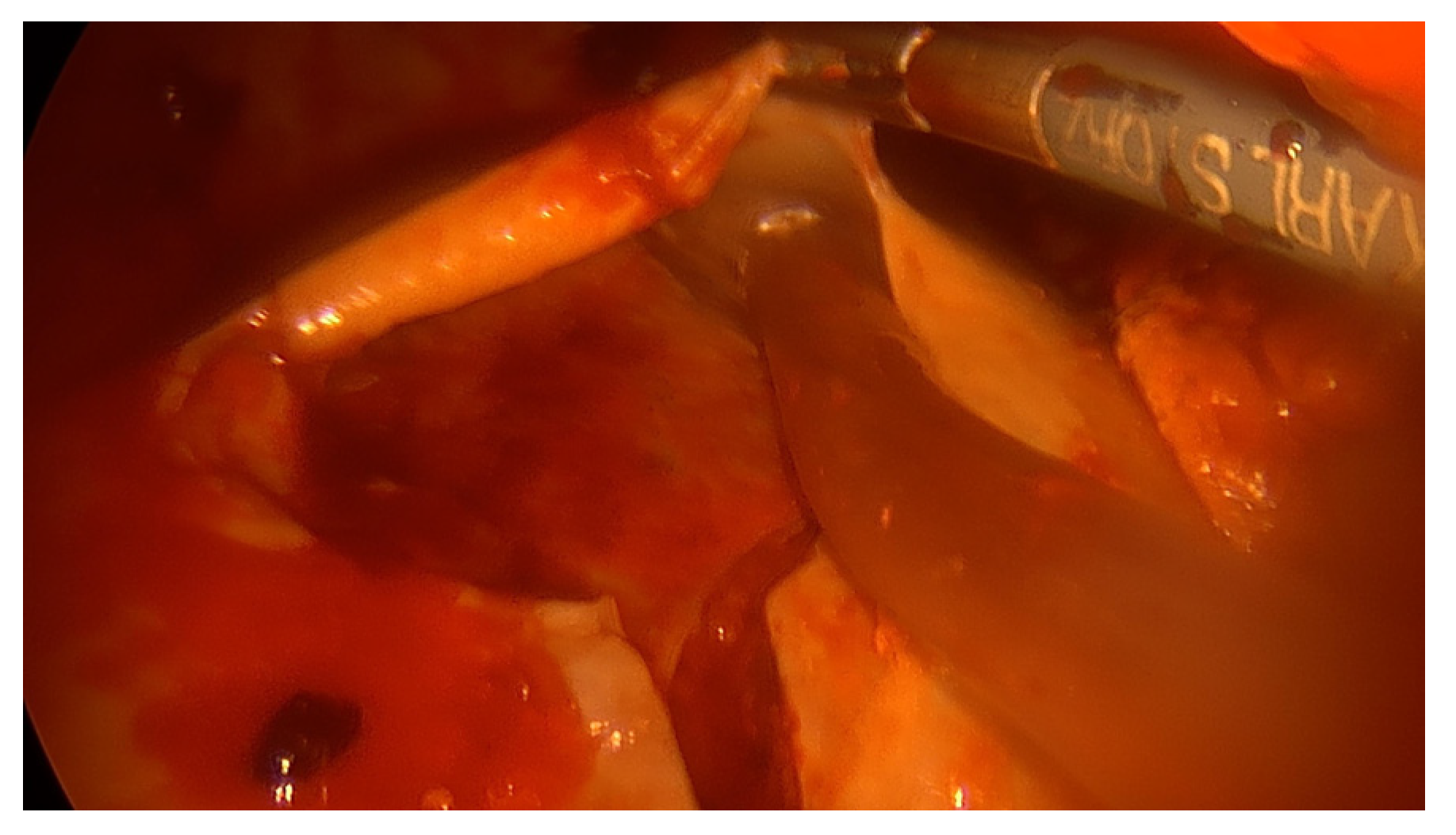
- OT group
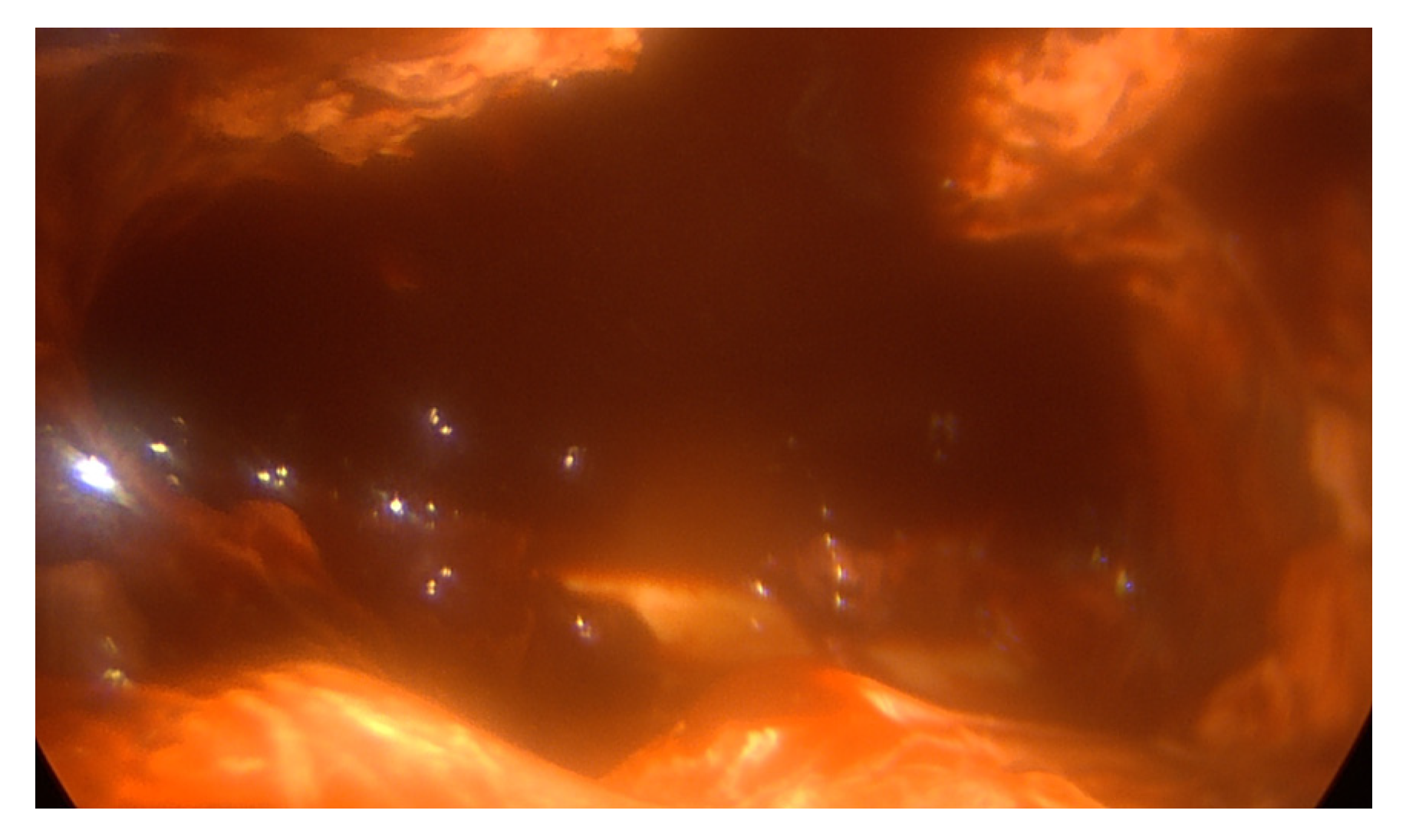
- VT group
2.2. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dadonaite, B.; Roser, M. Pneumonia. Our World in Data 2018. Available online: https://ourworldindata.org/pneumonia (accessed on 13 August 2022).
- Dean, N.C.; Griffith, P.P.; Sorensen, J.S.; McCauley, L.; Jones, B.E.; Lee, Y.C.G. Pleural Effusions at First ED Encounter Predict Worse Clinical Outcomes in Patients with Pneumonia. Chest 2016, 149, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Bobbio, A.; Bouam, S.; Frenkiel, J.; Zarca, K.; Fournel, L.; Canny, E.; Icard, P.; Porcher, R.; Alifano, M. Epidemiology and prognostic factors of pleural empyema. Thorax 2021, 76, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.C.; Parker, E.F.; Shaw, R.R.; Wilson, N.J.; Webb, W.R. Management of nontuberculous empyema. Am. Rev. Respir. Dis. 1962, 85, 935–936. [Google Scholar]
- Farjah, F.; Symons, R.G.; Krishnadasan, B.; Wood, D.E.; Flum, D.R. Management of pleural space infections: A population-based analysis. J. Thorac. Cardiovasc. Surg. 2007, 133, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Davies, H.E.; Davies, R.J.O.; Davies, C.W.H.; on behalf of the BTS Pleural Disease Guideline Group. Management of pleural infection in adults: British Thoracic Society pleural disease guideline 2010. Thorax 2010, 65 (Suppl. 2), ii41–ii53. [Google Scholar] [CrossRef]
- Bilgin, M.; Akcali, Y.; Oguzkaya, F. Benefits of early aggressive management of empyema thoracis. ANZ J. Surg. 2006, 76, 120–122. [Google Scholar] [CrossRef]
- Muhammad, M.I.A. Management of complicated parapneumonic effusion and empyema using different treatment modalities. Asian Cardiovasc. Thorac. Ann. 2012, 20, 177–181. [Google Scholar] [CrossRef]
- Höfken, H.; Herrmann, D.; Ewig, S.; Volmerig, J.; Hecker, E. Video-Assisted Thoracoscopic Surgery of Parapneumonic Empyema—A 10-year Single-Centre Experience. Pneumologie 2018, 72, 843–850. [Google Scholar] [CrossRef]
- Chambers, A.; Routledge, T.; Dunning, J.; Scarci, M. Is video-assisted thoracoscopic surgical decortication superior to open surgery in the management of adults with primary empyema? Interact. Cardiovasc. Thorac. Surg. 2010, 11, 171–177. [Google Scholar] [CrossRef]
- Scarci, M.; Abah, U.; Solli, P.; Page, A.; Waller, D.A.; Van Schil, P.; Melfi, F.; Schmid, R.A.; Athanassiadi, K.; Uva, M.S.; et al. EACTS expert consensus statement for surgical management of pleural empyema. Eur. J. Cardio-Thorac. Surg. 2015, 48, 642–653. [Google Scholar] [CrossRef]
- Wait, M.A.; Sharma, S.; Hohn, J.; Nogare, A.D. A randomized trial of empyema therapy. Chest 1997, 111, 1548–1551. [Google Scholar] [CrossRef]
- Towe, C.W.; Carr, S.R.; Donahue, J.M.; Burrows, W.M.; Perry, Y.; Kim, S.; Kosinski, A.; Linden, P.A. Morbidity and 30-day mortality after decortication for parapneumonic empyema and pleural effusion among patients in the Society of Thoracic Surgeons’ General Thoracic Surgery Database. J. Thorac. Cardiovasc. Surg. 2019, 157, 1288–1297.e4. [Google Scholar] [CrossRef] [PubMed]
- Arnold, D.T.; Hamilton, F.W.; Morris, T.T.; Suri, T.; Morley, A.; Frost, V.; Vipond, I.B.; Medford, A.R.; Payne, R.A.; Muir, P.; et al. Epidemiology of pleural empyema in English hospitals and the impact of influenza. Eur. Respir. J. 2020, 57, 2003546. [Google Scholar] [CrossRef] [PubMed]
- Shen, K.R.; Bribriesco, A.; Crabtree, T.; Denlinger, C.; Eby, J.; Eiken, P.; Jones, D.R.; Keshavjee, S.; Maldonado, F.; Paul, S.; et al. The American Association for Thoracic Surgery consensus guidelines for the management of empyema. J. Thorac. Cardiovasc. Surg. 2017, 153, e129–e146. [Google Scholar] [CrossRef] [PubMed]
- Mondoni, M.; Saderi, L.; Trogu, F.; Terraneo, S.; Carlucci, P.; Ghelma, F.; Centanni, S.; Sotgiu, G. Medical thoracoscopy treatment for pleural infections: A systematic review and meta-analysis. BMC Pulm. Med. 2021, 21, 127. [Google Scholar] [CrossRef] [PubMed]
- Sokouti, M.; Sadeghi, R.; Pashazadeh, S.; Abadi, S.E.H.; Sokouti, M.; Ghojazadeh, M.; Sokouti, B. Treating empyema thoracis using video-assisted thoracoscopic surgery and open decortication procedures: A systematic review and meta-analysis by meta-mums tool. Arch. Med. Sci. 2019, 15, 912–935. [Google Scholar] [CrossRef]
- Tong, B.C.; Hanna, J.; Toloza, E.M.; Onaitis, M.W.; D’Amico, T.A.; Harpole, D.H.; Burfeind, W.R. Outcomes of video-assisted thoracoscopic decortication. Ann. Thorac. Surg. 2010, 89, 220–225. [Google Scholar] [CrossRef]
- Chan, D.T.L.; Sihoe, A.D.L.; Chan, S.; Tsang, D.S.F.; Fang, B.; Lee, T.-W.; Cheng, L.-C. Surgical treatment for empyema thoracis: Is video-assisted thoracic surgery “better” than thoracotomy? Ann. Thorac. Surg. 2007, 84, 225–231. [Google Scholar] [CrossRef]
- Cardillo, G.; Carleo, F.; Carbone, L.; Di Martino, M.; Salvadori, L.; Petrella, L.; Martelli, M. Chronic postpneumonic pleural empyema: Comparative merits of thoracoscopic versus open decortication. Eur. J. Cardio-Thorac. Surg. 2009, 36, 914–918. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Bjelanović, D.; Gudelj, R.; Jukić, M.; Petrić, J.; Furlan, D. Video-assisted thoracic surgery in early stage of pediatric pleural empyema improves outcome. Thorac. Cardiovasc. Surg. 2021, 69, 475–480. [Google Scholar] [CrossRef]
- Mummadi, S.R.; Stoller, J.K.; Lopez, R.; Kailasam, K.; Gillespie, C.T.; Hahn, P.Y. Epidemiology of Adult Pleural Disease in the United States. Chest 2021, 160, 1534–1551. [Google Scholar] [CrossRef] [PubMed]
- Stefani, A.; Aramini, B.; della Casa, G.; Ligabue, G.; Kaleci, S.; Casali, C.; Morandi, U. Preoperative predictors of successful surgical treatment in the management of parapneumonic empyema. Ann. Thorac. Surg. 2013, 96, 1812–1819. [Google Scholar] [CrossRef] [PubMed]
- Lardinois, D.; Gock, M.; Pezzetta, E.; Buchli, C.; Rousson, V.; Furrer, M.; Ris, H.-B. Delayed referral and gram-negative organisms increase the conversion thoracotomy rate in patients undergoing video-assisted thoracoscopic surgery for empyema. Ann. Thorac. Surg. 2005, 79, 1851–1856. [Google Scholar] [CrossRef]
- Chung, J.H.; Lee, S.H.; Kim, K.T.; Jung, J.S.; Son, H.S.; Sun, K. Optimal timing of thoracoscopic drainage and decortication for empyema. Ann. Thorac. Surg. 2014, 97, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Shahin, Y.; Beggs, D.; Black, E.; Majewski, A.; Duffy, J. Surgical management of primary empyema of the pleural cavity: Outcome of 81 patients? Interact. Cardiovasc. Thorac. Surg. 2010, 10, 565–567. [Google Scholar] [CrossRef]
- Casali, C.; Storelli, E.S.; Di Prima, E.; Morandi, U. Long-term functional results after surgical treatment of parapneumonic thoracic empyema. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Bedawi, E.O.; Ricciardi, S.; Hassan, M.; Gooseman, M.R.; Asciak, R.; Castro-Anon, O.; Armbruster, K.; Bonifazi, M.; Poole, S.; Harris, E.K.; et al. ERS/ESTS statement on the management of pleural infection in adults. Eur. Respir. J. 2022, 60, 2201062. [Google Scholar] [CrossRef]

| Characteristics | OPEN (n = 75) | VATS (n = 644) | p Value |
|---|---|---|---|
| Male/female | 43/32 | 471/173 | |
| Age (range) | 58 (23–83) | 56 (17–82) | |
| Symptoms duration (days) | 7 ± 2 | 5 ± 2 | |
| Preoperative treatment: | |||
| chest drainage | 63 (84%) | 543 (84.3%) | 0.473 |
| thoracentesis | 12 (16%) | 101 (15.7%) | 0.475 |
| Smoking history | 25 (33.3%) | 141 (21.9%) | 0.013 |
| Intravenous drug abuse | 11 (14.6%) | 23 (3.5%) | 0.000 |
| Comorbidities | |||
| Diabetes | 51 (68%) | 432 (67%) | 0.430 |
| Alcoholism | 24 (32%) | 81 (12.6%) | 0.000 |
| Cardiovascular | 45 (60%) | 376 (58.4) | 0.395 |
| Liver cirrhosis | 18 (24%) | 26 (4%) | 0.036 |
| Empyema stage II | 8 (10.6%) | 545 (84.6%) | |
| Empyema stage III | 67 (89.3%) | 99 (15.4%) |
| Paramether | OPEN (n = 75) | VATS (n = 644) | p Value |
|---|---|---|---|
| Operative time (min, SD) | 92.7 ± 6.8 | 112.2 ± 7.4 | <0.0001 |
| Re-expansion of the lung (n, percentage) | 75 (100%) | 643 (99.8%) | n.s. |
| Redo surgery (bleeding) | 5.3% (4/75) | 1.86% (12/644) | 0.05 |
| Postoperative mortality | 5.3% (4/75) | 0.77% (5/644) | 0.008 |
| Morbidity | 21.3% (16/75) | 13.9% (90/644) | 0.08 |
| Postoperative air leak (days) | 4.3 ± 3,8 | 3.1 ± 2.6 | <0.0001 |
| Postoperative lenght of stay (days) | 10 ± 6.5 | 8 ± 2.4 | <0.0001 |
| Postoperative pain (median, range) | |||
| 1 and 6 days after surgery | 6 (4–9) | 4 (3–6) | <0.0001 |
| 6 months | 2 (0–4) | 2 (0–3) | 0.08 |
| Time to return to work (days, SD) | 33.2 ± 8.6 | 23.4 ± 4.8 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricciardi, S.; Giovanniello, D.; Carleo, F.; Di Martino, M.; Jaus, M.O.; Mantovani, S.; Treggiari, S.; Tritapepe, L.; Cardillo, G. Which Surgery for Stage II–III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients. J. Clin. Med. 2023, 12, 136. https://doi.org/10.3390/jcm12010136
Ricciardi S, Giovanniello D, Carleo F, Di Martino M, Jaus MO, Mantovani S, Treggiari S, Tritapepe L, Cardillo G. Which Surgery for Stage II–III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients. Journal of Clinical Medicine. 2023; 12(1):136. https://doi.org/10.3390/jcm12010136
Chicago/Turabian StyleRicciardi, Sara, Delia Giovanniello, Francesco Carleo, Marco Di Martino, Massimo O. Jaus, Sara Mantovani, Stefano Treggiari, Luigi Tritapepe, and Giuseppe Cardillo. 2023. "Which Surgery for Stage II–III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients" Journal of Clinical Medicine 12, no. 1: 136. https://doi.org/10.3390/jcm12010136
APA StyleRicciardi, S., Giovanniello, D., Carleo, F., Di Martino, M., Jaus, M. O., Mantovani, S., Treggiari, S., Tritapepe, L., & Cardillo, G. (2023). Which Surgery for Stage II–III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients. Journal of Clinical Medicine, 12(1), 136. https://doi.org/10.3390/jcm12010136









