Preoperative Anxiety in the Surgical Transfer and Waiting Area: A Cross-Sectional Mixed Method Study
Abstract
1. Introduction
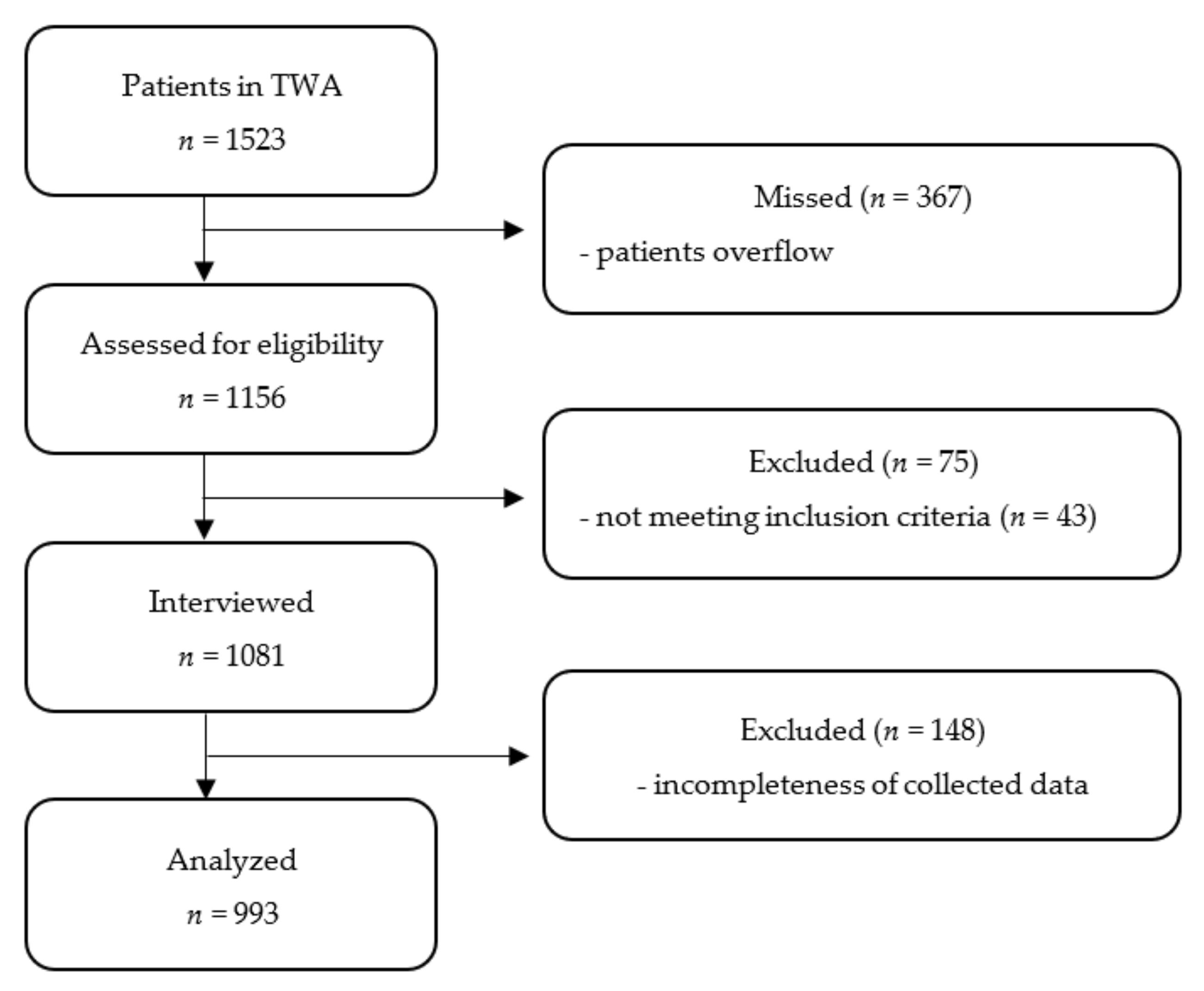
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Aust, H.; Eberhart, L.; Sturm, T.; Schuster, M.; Nestoriuc, Y.; Brehm, F.; Rusch, D. A cross-sectional study on preoperative anxiety in adults. J. Psychosom. Res. 2018, 111, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Kain, Z.N.; Sevarino, F.; Alexander, G.M.; Pincus, S.; Mayes, L.C. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. J. Psychosom. Res. 2000, 49, 417–422. [Google Scholar] [CrossRef]
- Kil, H.K.; Kim, W.O.; Chung, W.Y.; Kim, G.H.; Seo, H.; Hong, J.Y. Preoperative anxiety and pain sensitivity are independent predictors of propofol and sevoflurane requirements in general anaesthesia. Br. J. Anaesth. 2012, 108, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Eberhart, L.; Aust, H.; Schuster, M.; Sturm, T.; Gehling, M.; Euteneuer, F.; Rusch, D. Preoperative anxiety in adults—A cross-sectional study on specific fears and risk factors. BMC Psychiatry 2020, 20, 140. [Google Scholar] [CrossRef]
- Maurice-Szamburski, A.; Auquier, P.; Viarre-Oreal, V.; Cuvillon, P.; Carles, M.; Ripart, J.; Honore, S.; Triglia, T.; Loundou, A.; Leone, M.; et al. Effect of sedative premedication on patient experience after general anesthesia: A randomized clinical trial. JAMA 2015, 313, 916–925. [Google Scholar] [CrossRef]
- Kindler, C.H.; Harms, C.; Amsler, F.; Ihde-Scholl, T.; Scheidegger, D. The visual analog scale allows effective measurement of preoperative anxiety and detection of patients’ anesthetic concerns. Anesth. Analg. 2000, 90, 706–712. [Google Scholar] [CrossRef]
- Miller, K.M.; Wysocki, T.; Cassady, J.F., Jr.; Cancel, D.; Izenberg, N. Validation of measures of parents’ preoperative anxiety and anesthesia knowledge. Anesth. Analg. 1999, 88, 251–257. [Google Scholar] [CrossRef]
- Kumar, A.; Dubey, P.K.; Ranjan, A. Assessment of Anxiety in Surgical Patients: An Observational Study. Anesth. Essays Res. 2019, 13, 503–508. [Google Scholar] [CrossRef]
- Moerman, N.; van Dam, F.S.; Muller, M.J.; Oosting, H. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth. Analg. 1996, 82, 445–451. [Google Scholar]
- Lipman, R.S. Differentiating anxiety and depression in anxiety disorders: Use of rating scales. Psychopharmacol. Bull. 1982, 18, 69–77. [Google Scholar]
- Maurice-Szamburski, A.; Loundou, A.; Capdevila, X.; Bruder, N.; Auquier, P. Validation of the French version of the Amsterdam preoperative anxiety and information scale (APAIS). Health Qual. Life Outcomes 2013, 11, 166. [Google Scholar] [CrossRef] [PubMed]
- Boker, A.; Brownell, L.; Donen, N. The Amsterdam preoperative anxiety and information scale provides a simple and reliable measure of preoperative anxiety. Can. J. Anaesth. 2002, 49, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Farrar, J.T.; Portenoy, R.K.; Berlin, J.A.; Kinman, J.L.; Strom, B.L. Defining the clinically important difference in pain outcome measures. Pain 2000, 88, 287–294. [Google Scholar] [CrossRef]
- Mouelhi, Y.; Jouve, E.; Castelli, C.; Gentile, S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual. Life Outcomes 2020, 18, 136. [Google Scholar] [CrossRef]
- Gerbershagen, H.J.; Aduckathil, S.; van Wijck, A.J.; Peelen, L.M.; Kalkman, C.J.; Meissner, W. Pain intensity on the first day after surgery: A prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013, 118, 934–944. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Mavridou, P.; Dimitriou, V.; Manataki, A.; Arnaoutoglou, E.; Papadopoulos, G. Patient’s anxiety and fear of anesthesia: Effect of gender, age, education, and previous experience of anesthesia. A survey of 400 patients. J. Anesth. 2013, 27, 104–108. [Google Scholar] [CrossRef]
- Attias, S.; Keinan Boker, L.; Arnon, Z.; Ben-Arye, E.; Bar’am, A.; Sroka, G.; Matter, I.; Somri, M.; Schiff, E. Effectiveness of integrating individualized and generic complementary medicine treatments with standard care versus standard care alone for reducing preoperative anxiety. J. Clin. Anesth. 2016, 29, 54–64. [Google Scholar] [CrossRef]
- Matthias, A.T.; Samarasekera, D.N. Preoperative anxiety in surgical patients—Experience of a single unit. Acta Anaesthesiol. Taiwanica 2012, 50, 3–6. [Google Scholar] [CrossRef]
- Pokharel, K.; Bhattarai, B.; Tripathi, M.; Khatiwada, S.; Subedi, A. Nepalese patients’ anxiety and concerns before surgery. J. Clin. Anesth. 2011, 23, 372–378. [Google Scholar] [CrossRef]
- Buonanno, P.; Laiola, A.; Palumbo, C.; Spinelli, G.; Terminiello, V.; Servillo, G. Italian validation of the Amsterdam Preoperative Anxiety and Information Scale. Minerva Anestesiol. 2017, 83, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Michaelides, A.; Zis, P. Depression, anxiety and acute pain: Links and management challenges. Postgrad. Med. 2019, 131, 438–444. [Google Scholar] [CrossRef] [PubMed]
- James, J.E.; Hardardottir, D. Influence of attention focus and trait anxiety on tolerance of acute pain. Br. J. Health Psychol. 2002, 7, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Wetsch, W.A.; Pircher, I.; Lederer, W.; Kinzl, J.F.; Traweger, C.; Heinz-Erian, P.; Benzer, A. Preoperative stress and anxiety in day-care patients and inpatients undergoing fast-track surgery. Br. J. Anaesth. 2009, 103, 199–205. [Google Scholar] [CrossRef]
- Humphrey, J.A.; Johnson, S.L.; Patel, S.; Malik, M.; Willis-Owen, C.A.; Bendall, S. Patients’ preferred mode of travel to the orthopaedic theatre. World J. Orthop. 2015, 6, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Kojima, Y.; Ina, H.; Fujita, T.; Mitono, H. Relieving anxiety by entering the operating room on foot. Can. J. Anaesth. 2002, 49, 885–886. [Google Scholar] [CrossRef][Green Version]
- Biddiss, E.; Knibbe, T.J.; McPherson, A. The effectiveness of interventions aimed at reducing anxiety in health care waiting spaces: A systematic review of randomized and nonrandomized trials. Anesth. Analg. 2014, 119, 433–448. [Google Scholar] [CrossRef]
- Kaës, R. Du Moi-peau aux enveloppes psychiques. Genèse et développement d’un concept. Le Carnet Psy 2007, 117, 33–39. [Google Scholar] [CrossRef]
- Ciccone, A. Enveloppe psychique et fonction contenante: Modèles et pratiques. Cah. Psychol. Clin. 2001, 17, 81–102. [Google Scholar] [CrossRef]
- Soltner, C.; Giquello, J.A.; Monrigal-Martin, C.; Beydon, L. Continuous care and empathic anaesthesiologist attitude in the preoperative period: Impact on patient anxiety and satisfaction. Br. J. Anaesth. 2011, 106, 680–686. [Google Scholar] [CrossRef]
| APAIS 7 [5 to 10] | VAS-A 3 [1 to 5] | COVI 3 [2 to 5] | |
|---|---|---|---|
| APAIS | 1 | ρ 0.65, p < 0.0001 | ρ 0.58, p < 0.0001 |
| VAS-A | 1 | ρ 0.54, p < 0.0001 | |
| COVI | 1 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| All Patients n (% of Total) | APAIS ≥ 11 n = 230 (24.7%) | APAIS < 11 n = 703 (75.3%) | p-Value | Odds Ratio (95%CI) | p-Value | |
| Age, years | 61 [45 to 72] | 58 [41 to 70] | 62 [47 to 73] | 0.0107 | 0.99 (0.98 to 1.01) | 0.4263 |
| Sex [F] | 435 (46.6%) | 141 (32.4%) | 294 (67.6%) | <.0001 | 2.29 (1.63 to 3.21) | <0.001 |
| BMI, kg/m2 | 24.6 [21.6 to 27.7] | 24.22 [21.5 to 27.4] | 24.8 [21.6 to 27.9] | 0.3425 | 0.99 (0.96 to 1.02) | 0.5819 |
| ASA class I vs. ≥ II | 280 (30%) | 87 (31.1%) | 193 (68.9%) | 0.0037 | 1.44 (0.93 to 2.23) | 0.0978 |
| Inpatient setting (Y) | 588 (63.0%) | 157 (26.7%) | 431 (73.3%) | 0.0594 | 2.13 (1.34 to 3.39) | 0.0014 |
| Hospitalisation > 24 h(Y) | 123 (13.2%) | 23 (18.7%) | 100 (81.3%) | 0.1158 | 0.71 (0.40 to 1.25) | 0.2357 |
| Previous OR experience (Y) | 868 (93.1%) | 206 (23.7%) | 662 (76.7%) | 0.0348 | 0.56 (0.29 to 1.05) | 0.0698 |
| Anxiolytic premedication (Y) | 114 (12.2%) | 34 (29.8%) | 80 (70.2%) | 0.2015 | 1.19 (0.73 to 1.96) | 0.4772 |
| Pain (NS > 3) in the TWA (Y) | 160 (17.2%) | 50 (31.3%) | 110 (68.7%) | 0.0434 | 1.57 (1.04 to 2.37) | 0.0336 |
| Procedures with preserved consciousness (Y) | 473 (50.7%) | 110 (23.3%) | 363 (76.7%) | 0.3242 | 0.80 (0.56 to 1.13) | 0.2056 |
| Anticipated pain level associated with procedure | ||||||
| No pain to light pain vs. moderate to severe pain | 413 (44.3%) | 81 (19.6%) | 332 (80.4%) | 0.0017 | 1.33 (0.87 to 2.03) | 0.1839 |
| Arrival mode | ||||||
| Walking | 71 (7.6%) | 17 (23.9%) | 54 (76.1%) | 1 | 1 (1 to 1) | 1 |
| Wheelchair | 63 (6.8%) | 18 (28.6%) | 45 (71.4%) | 0.4512 | 0.97 (0.36 to 2.63) | 0.9453 |
| Stretcher | 120 (12.8%) | 18 (15%) | 102 (85%) | 0.0088 | 0.29 (0.11 to 0.75) | 0.0110 |
| Bed | 679 (72.8%) | 177 (26.1%) | 502 (73.9%) | 0.1055 | 0.42 (0.18 to 1.02) | 0.0543 |
| Supine Position | 799 (85.6%) | 195 (24.4%) | 604 (75.6%) | 0.6658 | 0.36 (0.18 to 0.72) | 0.0035 |
| Satisfaction with the arrival mode (Y) | 775 (83.1%) | 200 (25.8%) | 575 (74.2%) | 0.0847 | 1.14 (0.60 to 1.87) | 0.5977 |
| VAS-A Changes | All Patients n = 933 | APAIS ≥ 11 n = 230 | APAIS ≤ 11 n = 703 | |
|---|---|---|---|---|
| Increase | 96 (10.29%) | 27 (11.7%) χ2 = 0.47 | 69 (9.8%) χ2 = 0.15 | p = 0.0003 * |
| Decrease | 127 (13.61%) | 49 (21.3%) χ2 = 1 | 78 (11.1%) χ2 = 3.27 | |
| No changes | 710 (76.1%) | 154 (67%) χ2 = 2.52 | 556 (79.1%) χ2 = 0.83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dziadzko, M.; Mazard, T.; Bonhomme, M.; Raffin, M.; Pradat, P.; Forcione, J.-M.; Minjard, R.; Aubrun, F. Preoperative Anxiety in the Surgical Transfer and Waiting Area: A Cross-Sectional Mixed Method Study. J. Clin. Med. 2022, 11, 2668. https://doi.org/10.3390/jcm11092668
Dziadzko M, Mazard T, Bonhomme M, Raffin M, Pradat P, Forcione J-M, Minjard R, Aubrun F. Preoperative Anxiety in the Surgical Transfer and Waiting Area: A Cross-Sectional Mixed Method Study. Journal of Clinical Medicine. 2022; 11(9):2668. https://doi.org/10.3390/jcm11092668
Chicago/Turabian StyleDziadzko, Mikhail, Tessa Mazard, Myriam Bonhomme, Mahé Raffin, Pierre Pradat, Jean-Marc Forcione, Raphael Minjard, and Frederic Aubrun. 2022. "Preoperative Anxiety in the Surgical Transfer and Waiting Area: A Cross-Sectional Mixed Method Study" Journal of Clinical Medicine 11, no. 9: 2668. https://doi.org/10.3390/jcm11092668
APA StyleDziadzko, M., Mazard, T., Bonhomme, M., Raffin, M., Pradat, P., Forcione, J.-M., Minjard, R., & Aubrun, F. (2022). Preoperative Anxiety in the Surgical Transfer and Waiting Area: A Cross-Sectional Mixed Method Study. Journal of Clinical Medicine, 11(9), 2668. https://doi.org/10.3390/jcm11092668






