Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ohrbach, R.; Michelotti, A. The role of stress in the etiology of oral parafunction and myofascial pain. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.C.; Cioffi, I. Effects of trait anxiety, somatosensory amplification, and facial pain on self-reported oral behaviors. Clin. Oral Investig. 2019, 23, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J.; Garofalo, J.P.; Ellis, E.; Holt, C. Major psychological disorders in acute and chronic TMD: An initial examination. J. Am. Dent. Assoc. 1996, 127, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Bandettini di Poggio, A.; Cantini, E.; Dell’Osso, L.; Bosco, M. Mood and anxiety psychopathology and temporomandibular disorder: A spectrum approach. J. Oral Rehabil. 2004, 31, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Wieckiewicz, M.; Grychowska, N.; Wojciechowski, K.; Pelc, A.; Augustyniak, K.; Sleboda, A.; Zietek, M. Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed Res. Int. 2014, 2014, 472346. [Google Scholar] [CrossRef] [PubMed]
- Kostrzewa-Janicka, J.; Pietrzak, B.; Jurkowski, P.; Wielgos, M.; Binkowska, M.; Mierzwińska-Nastalska, E. Effects of oral contraceptives on the treatment for internal derangements in temporomandibular joints in women. Neuro Endocrinol. Lett. 2013, 34, 566–572. [Google Scholar]
- LeResche, L.; Saunders, K.; Von Korff, M.R.; Barlow, W.; Dworkin, S.F. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain 1997, 69, 153–160. [Google Scholar] [CrossRef]
- Kotrzewa-Janicka, J.; Anulewicz, A.; Magciak, M.; Meredyk, K.; Jurkowski, P. Effects of general factors on temporomandibular joint dysfunction treatment effectiveness. Protet. Stomatol. 2015, 3, 193–201. [Google Scholar] [CrossRef]
- Bucci, R.; Koutris, M.; Palla, S.; Rebaudo, G.F.; Lobbezoo, F.; Michelotti, A. Occlusal tactile acuity in temporomandibular disorder patients: A case control study. J Oral Rehabil. 2020, 47, 923–929. [Google Scholar] [CrossRef]
- Bucci, R.; Koutris, M.; Lobbezoo, F.; Michelotti, A. Occlusal sensitivity in individuals with different frequencies of oral parafunction. J. Prosthet. Dent. 2019, 122, 119–122. [Google Scholar] [CrossRef]
- Surowiecki, D.; Szerszeń, M.; Wróbel-Bednarz, K.; Walczyk, A. Compatibility of the digital design of prosthetic crowns with restorations made in the technology of selective laser sintering of metal powders. Protet. Stomatol. 2020, 70, 132–143. [Google Scholar] [CrossRef]
- Gawlak, D.; Łuniewska, J.; Stojak, W.; Hovhannisyan, A.; Stróżyńska, A.; Mańka-Malara, K.; Adamiec, M.; Rysz, A. The prevalence of orodental trauma during epileptic seizures in terms of dental treatment—Survey study. Neurol. Neurochir. Pol. 2017, 51, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Gawlak, D.; Mańka-Malara, K.; Mierzwińska-Nastalska, E.; Waśniewski, B.; Ryszkowska, J. Comparison of hardness, energy absorption and water absorbability of polymeric materials used in the manufacture of mouthguards. Dent. Med. Probl. 2015, 52, 78–85. [Google Scholar]
- Kondrat, W.; Sierpińska, T.; Gołębiewska, M. Electronic diagnostics in the study of functional mandibular movements. Protet. Stomatol. 2009, 1, 10–15. [Google Scholar]
- Dejak, A.; Gliszczyńska, A.; Kapiczke, A.; Dejak, B. Comparison of TMJ angles based on the ARCUSdigma II examination and occlusion records in the Protar 7 articulator. Protet. Stomatol. 2018, 68, 73–84. [Google Scholar] [CrossRef][Green Version]
- Torabi, K.; Pour, S.R.; Ahangari, A.H.; Ghodsi, S. A clinical comparative study of Cadiax Compact II and intraoral records using wax and addition silicone. Int. J. Prosthdont. 2014, 27, 541–543. [Google Scholar] [CrossRef]
- R Core Team. A Language and Environment for Statistical Computing. 2021. Available online: https://www.R-project.org/ (accessed on 20 March 2022).
- Cohen, J. 1988 Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar] [CrossRef]
- Caro, A.J.; Peraire, M.; Martinez-Gomis, J.; Anglada, J.M.; Samsó, J. Reproductibility of lateral excursive tooth contact in a semi-adjustable articulator depending on the type of lateral guidance. J. Oral Rehabil. 2005, 32, 174–179. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Yar, R.; Barclay, C.; Satterthwaite, S.D. Sagittal condylar angle and gender differences. J. Prosthodont. 2013, 22, 561–565. [Google Scholar] [CrossRef]
- Canning, T.; O’Connell, B.C.; Houston, F.; O’Sullivan, M. The effect of skeletal pattern on determining articulator settings for prosthodontic rehabilitation: An in vivo study. Int. J. Prosthodont. 2011, 24, 16–25. [Google Scholar]
- Zimmer, B.; Jäger, A.; Kubein-Meesenburg, D. Comparison of ‘normal’ TMJ-function in Class I, II, and III individuals. Eur. J. Orthod. 1991, 13, 27–34. [Google Scholar] [CrossRef]
- Cimić, S.; Simunković, S.K.; Catić, A. The relationship between Angle type of occlusion and recorded Bennett angle values. J. Prosthet. Dent. 2016, 115, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.M. Changes in the relationship of nasion point A and point B and the effect upon ANB. Am. J. Orthod. 1969, 56, 143–163. [Google Scholar] [CrossRef]
- Jacobson, A. The ‘Wits’ appraisal of jaw disharmony. Am. J. Orthod. 1975, 67, 125–138. [Google Scholar] [CrossRef]
- Freeman, R.S. Adjusting A-N-B angles to reflect the effects of maxillary position. Angle Orthod. 1981, 51, 162–171. [Google Scholar] [PubMed]
- Rushton, R.; Cohen, A.M.; Linney, A.D. The relationship and reproducibility of angle ANB and the Wits appraisal. Br. J. Orthod. 1991, 18, 225–231. [Google Scholar] [CrossRef]
- Rotberg, S.; Fried, N.; Kane, J.; Shapiro, E. Predicting the ‘Wits’ appraisal from the ANB angle. Am. J. Orthod. 1980, 77, 636–642. [Google Scholar] [CrossRef]
- Roth, R. The ‘Wits’ appraisal—Its skeletal and dentoalveolar background. Eur. J. Orthod. 1982, 4, 21–28. [Google Scholar] [CrossRef]
- Sherman, S.L.; Woods, M.; Nanda, R.S. The longitudinal effects of growth on the Wits appraisal. Am. J. Orthod. Dent. Orthop. 1988, 93, 429–436. [Google Scholar] [CrossRef]
- Hernandez, A.I.; Jasinevicius, T.R.; Kaleinikova, Z.; Sadan, A. Symmetry of horizontal and sagittal condylar path angles: An in vivo study. Cranio 2010, 28, 60–66. [Google Scholar] [CrossRef]
- Hüe, O. Condylar paths during protrusion in edentulous patients: Analysis with electronic axiography. J. Prosthodont. 2011, 20, 294–298. [Google Scholar] [CrossRef]
- Schierz, O.; Klinger, N.; Schön, G.; Reissmann, D.R. The reliability of computerized condylar path angle assessment. Int. J. Comput. Dent. 2014, 17, 35–51. [Google Scholar] [PubMed]
- Abrahamsson, C.; Henrikson, T.; Bondemark, L.; Ekhberg, E. Masticatiory function in patients with dentofacial deformities before and after orthognatic treatment—A prospective, longitudinal, and controlled study. Eur. J. Orthod. 2015, 37, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Cimić, S.; Simunković, S.K.; Badel, T.; Dulcić, N.; Alajbeg, I.; Catić, A. Measurements of the sagittal condylar inclination: Intraindividual variations. Cranio 2014, 32, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Maglione, H.O.; Roldan, O.V.; Carreira, R.; Mainieri, S. Analysis of condylar path inclination and incisal guidance. Cranio 1989, 7, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Kucukkeles, N.; Ozkan, H.; Ari-Demirkaya, A.; Cilingirturk, A.M. Compatibiity of mechanical and computerized axiographs: A pilot study. J. Prosthet. Dent. 2005, 94, 190–194. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, J.; Nelson, S.; Nowlin, T. Comparison of condylar guidance setting obtained from a wax record versus an extraoral tracing: A pilot study. J. Prosthet. Dent. 2003, 89, 54–59. [Google Scholar] [CrossRef]
- Curtis, D.A. A comparison of protrusive interocclusal records to pantographic tracings. J. Prosthet. Dent. 1989, 62, 154–156. [Google Scholar] [CrossRef]
- Cimić, S.; Simunković, S.K.; Simonić Kocijan, S.; Matijević, J.; Dulcić, N.; Catić, A. Articulator-related registration and analysis of sagittal condylar inclination. Acta Clin. Croat. 2015, 54, 432–437. [Google Scholar]
- Konaté, N.Y.; Djérédou, K.B.; Kamagaté, F.S.; Thiam, A.; Pesson, D.M.; Assi, K.D.; Touré, S. Determination of the average value of the condylar slope of black Africans. Odontostomatol. Trop. 2008, 31, 33–37. [Google Scholar]
- Han, B.; Kang, H.; Liu, L.; Yi, X.; Li, X. Comparisons of condylar movements with the functional occlusal clutch and tray clutch recordings methods in CADIAX system. Int. J. Oral Sci. 2010, 2, 208–214. [Google Scholar] [CrossRef]
- Matsumura, H.; Tsukiyama, Y.; Koyano, K. Analysis of sagittal condylar path inclination in consideration of Fischer’s angle. J. Oral Rehabil. 2006, 33, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Theusner, J.; Plesh, O.; Curtis, D.A.; Hutton, J.E. Axiographic tracings of temporomandibular joint movements. J. Prosthet. Dent. 1993, 69, 209–215. [Google Scholar] [CrossRef]
- Boulos, P.J.; Adib, S.M.; Naltchayan, L.J. The horizontal condylar inclination: Clinical comparison of different recording methods. Gen. Dent. 2007, 55, 112–116. [Google Scholar]
- English, J.D.; Buschang, P.H.; Throckmorton, G.S. Does malloclusion affect masticatory performance? Angle Orthod. 2002, 72, 21–27. [Google Scholar] [PubMed]
- Ugolini, A.; Mapelli, A.; Segù, M.; Zago, M.; Codari, M.; Sforza, A. Three-dimensional mandibular motion in skeletal Class-III patients. Cranio 2018, 36, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, Z.Z.; Alhaija, E.S.A.; AlWahadni, A.M.; Al-Ajlouni, Y. Bite force changes after surgical correction of mandibular prognatism in subjects with increased vertical dimention: A prospective clinical trial. J. Orofac. Orthop. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ringqvist, M. Isometric bite force and its relation to dimensions of the facial skeleton. Acta Odontol. Scand. 1973, 31, 35–42. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W. Occlusal forces in normal- and long-face children. J. Dent. Res. 1983, 62, 571–574. [Google Scholar] [CrossRef]
- Bakke, M.; Tuxen, A.; Vilmann, P.; Jensen, B.R.; Vilmann, A.; Toft, M. Ultrasound image of human masseter muscle related to bite force, electromyography, facial morphology, and occlusal factors. Scand. J. Dent. Res. 1992, 100, 164–171. [Google Scholar] [CrossRef]
- Kostrzewa-Janicka, J. The bite force and its relation to facial morphology in patients with temporomandibular disorders. Protet. Stomatol. 2007, 57, 316–324. [Google Scholar]
- Santander, P.; Quast, A.; Olbrish, C.; Rose, M.; Moser, N.; Schliephake, H.; Meyer-Marcotty, P. Comprehensive 3D analysis of condylar morphology in adults with different skeletal patterns—A cross-sectional study. Head Face Med. 2020, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Hasebe, A.; Yamaguchi, T.; Nakawaki, T.; Hikita, Y.; Katayama, K.; Maki, K. Comparison of condylar size among different anterioposterior and vertical skeletal patterns using cone-beam computed tomography. Angle Orthod. 2019, 89, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Chae, J.M.; Park, J.H.; Tai, K.; Mizutani, K.; Uzuka, S.; Miyashita, W.; Seo, H.Y. Evaluation of condyle-fossa relationships in adolescents with various skeletal patterns using cone-beam computed tomography. Angle Orthod. 2020, 90, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Arieta-Miranda, J.M.; Silva-Valencia, M.; Flores-Mir, C.; Paredes-Sampen, N.A.; Arriola-Guillen, L.E. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. Prog Orthod. 2013, 18, 36. [Google Scholar] [CrossRef] [PubMed]
- Katsavrias, E.G.; Halazonetis, D.J. Condyle and fossa shape in Class II and Class III skeletal patterns: A morphometric tomographic study. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 337–346. [Google Scholar] [CrossRef]
- Katsavrias, E.G. Morphology of the temporomandibular joint in subjects with Class II division 2 malocclusions. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 470–478. [Google Scholar] [CrossRef]



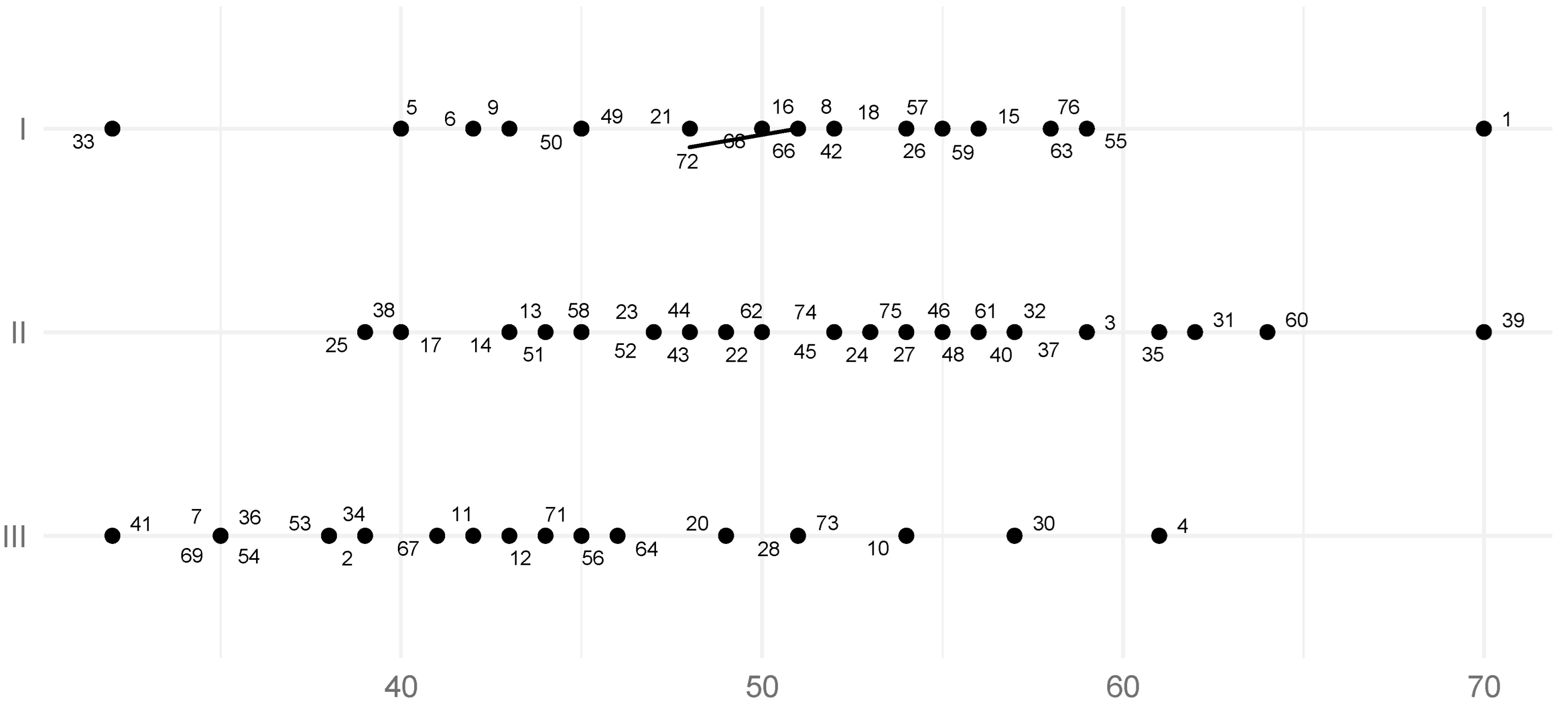


| Class | N | Min | Q1 | Median | Average | Q3 | Max | SD | SE |
|---|---|---|---|---|---|---|---|---|---|
| All | 75 | 32 | 43.0 | 50.0 | 49.2 | 55.5 | 70 | 8.5 | 0.98 |
| I | 23 | 32 | 45.8 | 51.5 | 51.0 | 55.8 | 70 | 7.9 | 1.65 |
| II | 29 | 39 | 47.0 | 52.0 | 51.8 | 56.0 | 70 | 7.6 | 1.41 |
| III | 23 | 32 | 37.2 | 42.5 | 43.6 | 49.5 | 61 | 8.1 | 1.69 |
| Class | N | Min | Q1 | Median | Average | Q3 | Max | SD | SE |
|---|---|---|---|---|---|---|---|---|---|
| All | 75 | 24 | 44.0 | 50 | 49.7 | 55.0 | 70 | 9.3 | 1.07 |
| I | 23 | 40 | 49.2 | 52 | 52.2 | 55.8 | 70 | 6.7 | 1.40 |
| II | 29 | 28 | 46.8 | 52 | 51.8 | 55.2 | 70 | 9.2 | 1.71 |
| III | 23 | 24 | 38.0 | 41 | 44.2 | 50.0 | 64 | 9.7 | 2.02 |
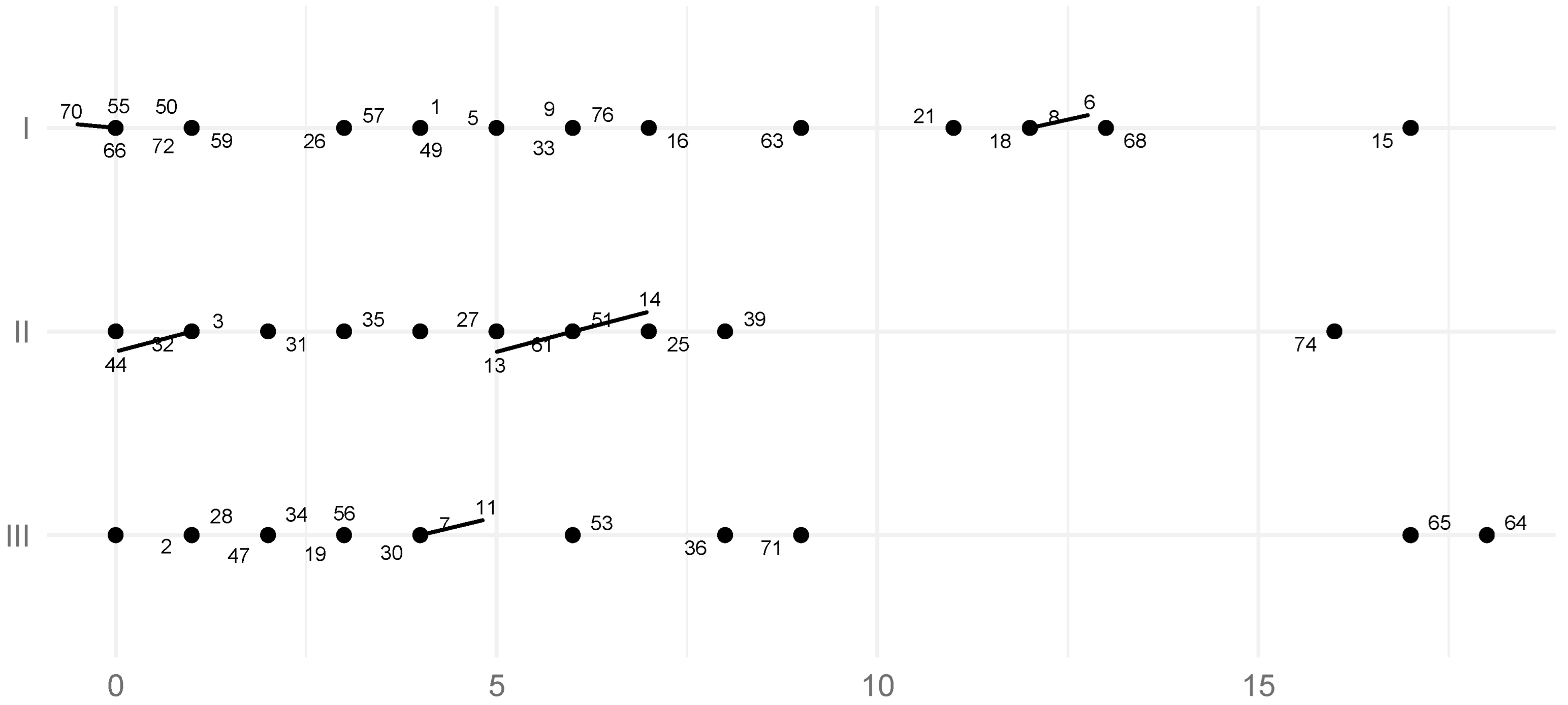
| Class | N | Min | Q1 | Median | Average | Q3 | Max | SD | SE |
|---|---|---|---|---|---|---|---|---|---|
| All | 75 | 0 | 0.0 | 3.0 | 4.1 | 6.0 | 18 | 4.6 | 0.53 |
| I | 23 | 0 | 1.5 | 5.5 | 6.0 | 10.5 | 17 | 5.0 | 1.04 |
| II | 29 | 0 | 0.0 | 3.0 | 3.2 | 5.0 | 16 | 3.6 | 0.67 |
| III | 23 | 0 | 0.0 | 2.0 | 3.6 | 4.0 | 18 | 5.1 | 1.06 |
| Class | N | Min | Q1 | Median | Average | Q3 | Max | SD | SE |
|---|---|---|---|---|---|---|---|---|---|
| All | 75 | 0 | 0 | 2 | 4.3 | 7 | 22 | 5.2 | 0.60 |
| I | 23 | 0 | 0 | 3 | 5.2 | 7 | 22 | 6.0 | 1.25 |
| II | 29 | 0 | 0 | 2 | 4.1 | 7 | 15 | 5.1 | 0.95 |
| III | 23 | 0 | 0 | 2 | 3.6 | 5 | 16 | 4.5 | 0.94 |
| The Coefficient for the ANB Angle | The Average from the Model | The p-Value of Test F | R2 | |
|---|---|---|---|---|
| SCI Left | 0.77 | 47.5 | 0.012 | 0.098 |
| SCI Right | 0.72 | 48.5 | 0.039 | 0.069 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandowska, A.; Mańka-Malara, K.; Kostrzewa-Janicka, J. Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes. J. Clin. Med. 2022, 11, 2664. https://doi.org/10.3390/jcm11092664
Lewandowska A, Mańka-Malara K, Kostrzewa-Janicka J. Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes. Journal of Clinical Medicine. 2022; 11(9):2664. https://doi.org/10.3390/jcm11092664
Chicago/Turabian StyleLewandowska, Anahit, Katarzyna Mańka-Malara, and Jolanta Kostrzewa-Janicka. 2022. "Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes" Journal of Clinical Medicine 11, no. 9: 2664. https://doi.org/10.3390/jcm11092664
APA StyleLewandowska, A., Mańka-Malara, K., & Kostrzewa-Janicka, J. (2022). Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes. Journal of Clinical Medicine, 11(9), 2664. https://doi.org/10.3390/jcm11092664








