Coracoid Impingement and Morphology Is Associated with Fatty Infiltration and Rotator Cuff Tears
Abstract
1. Introduction
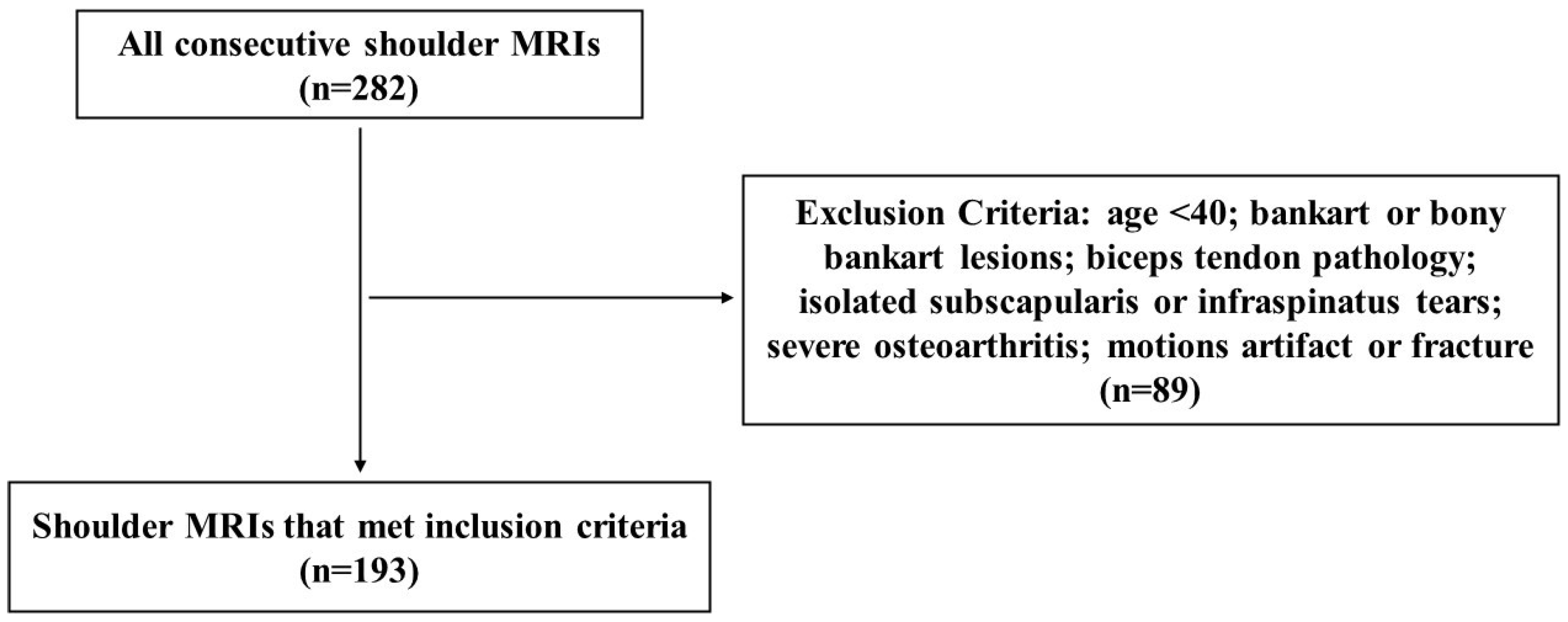
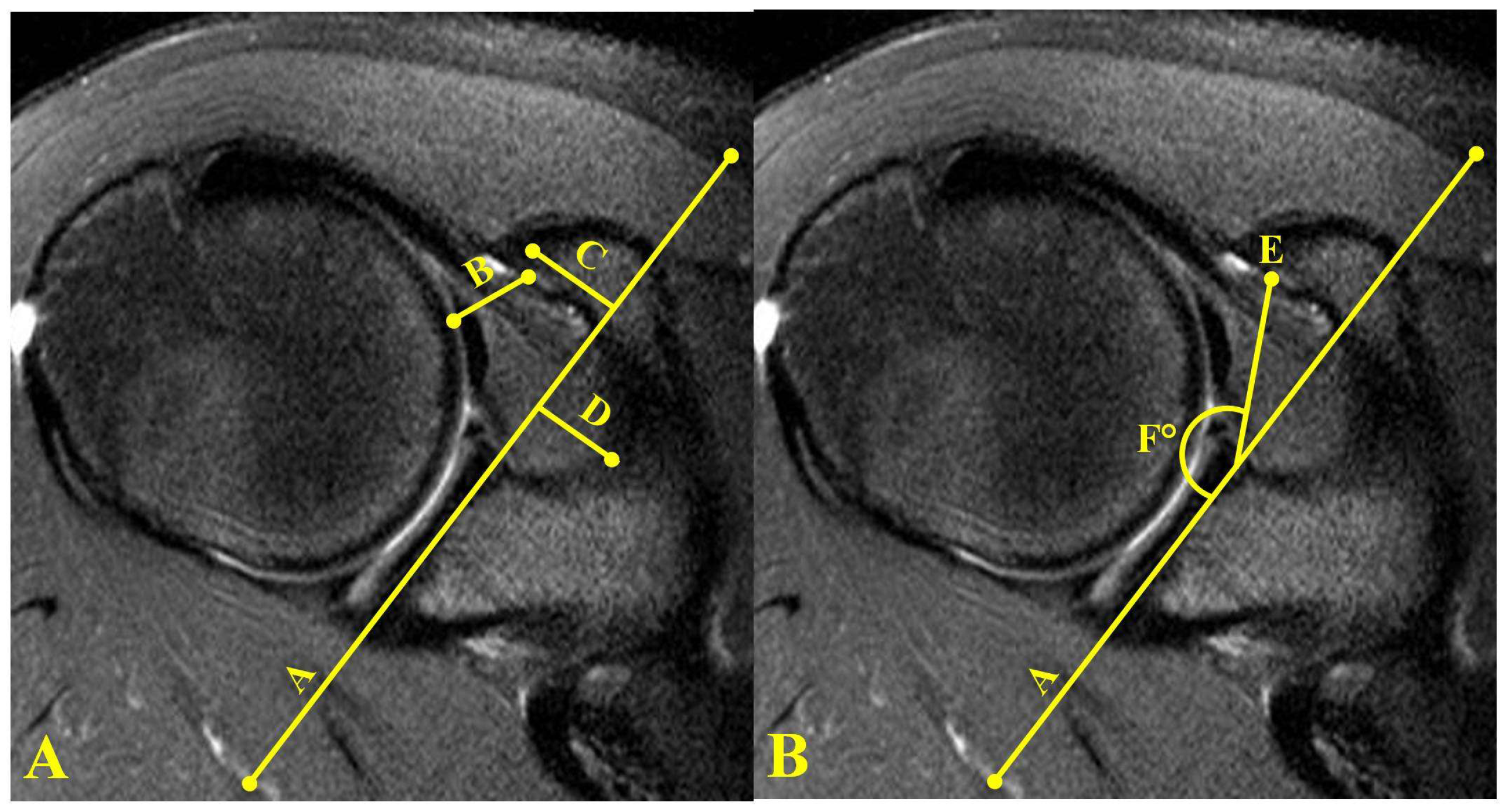
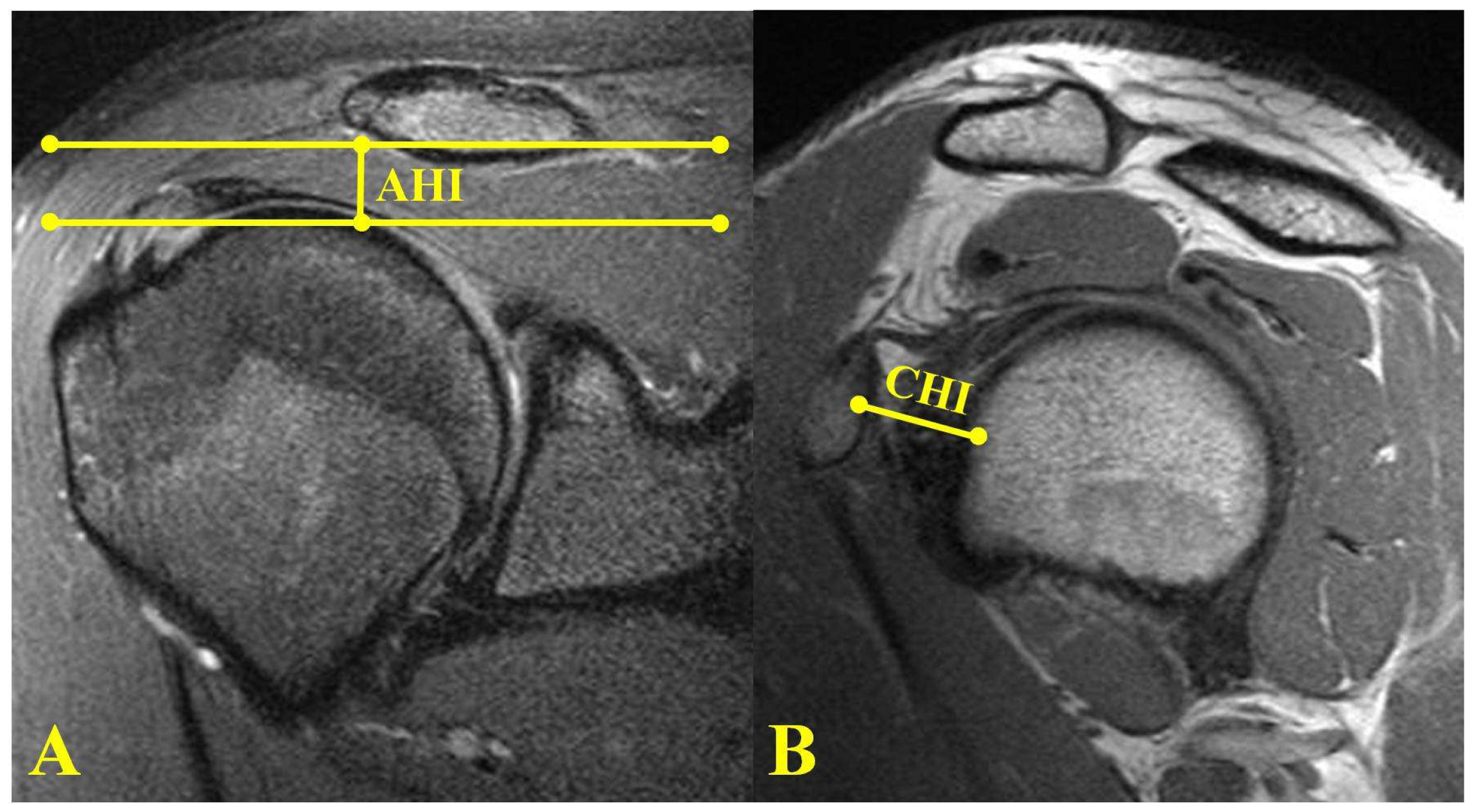
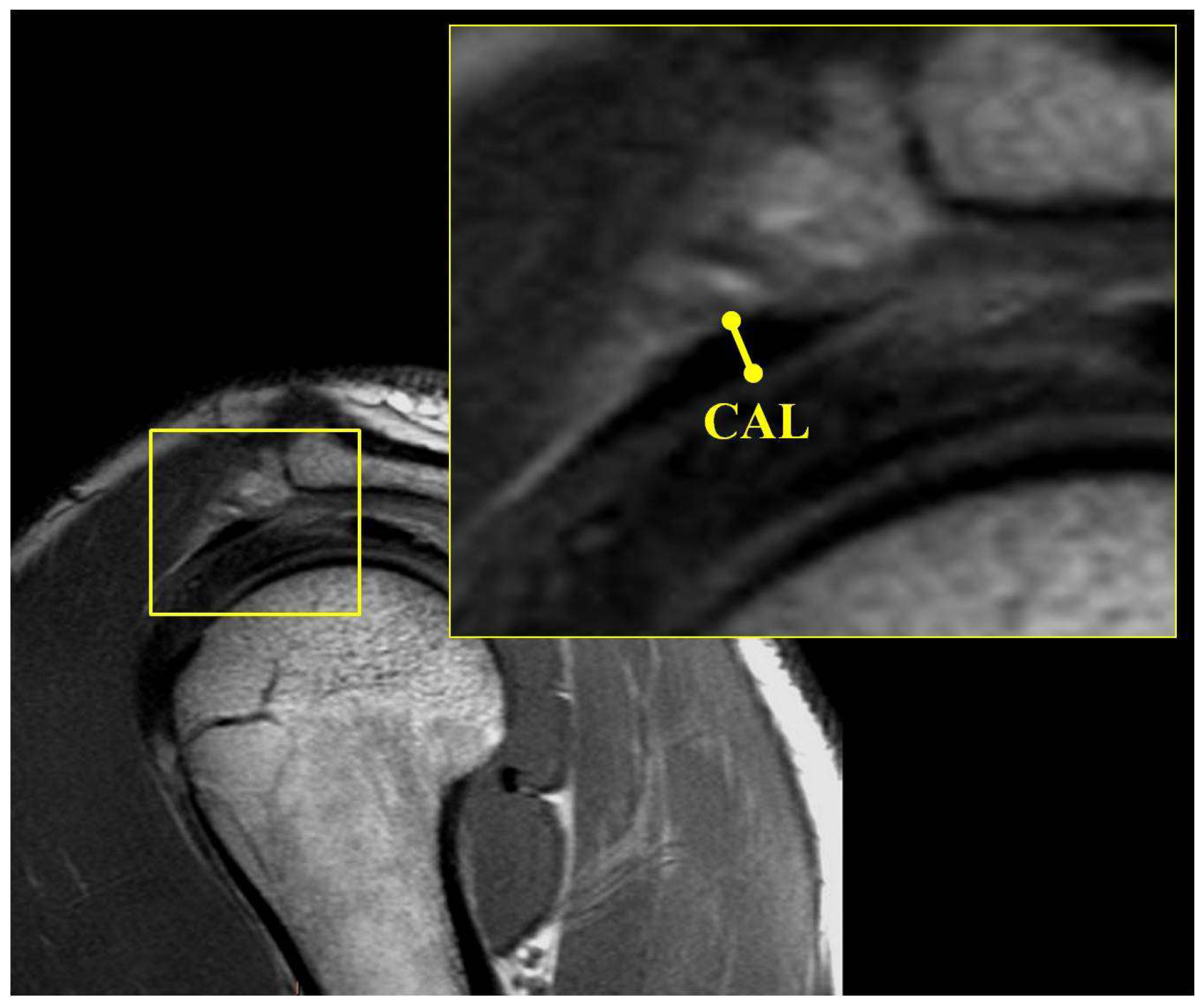
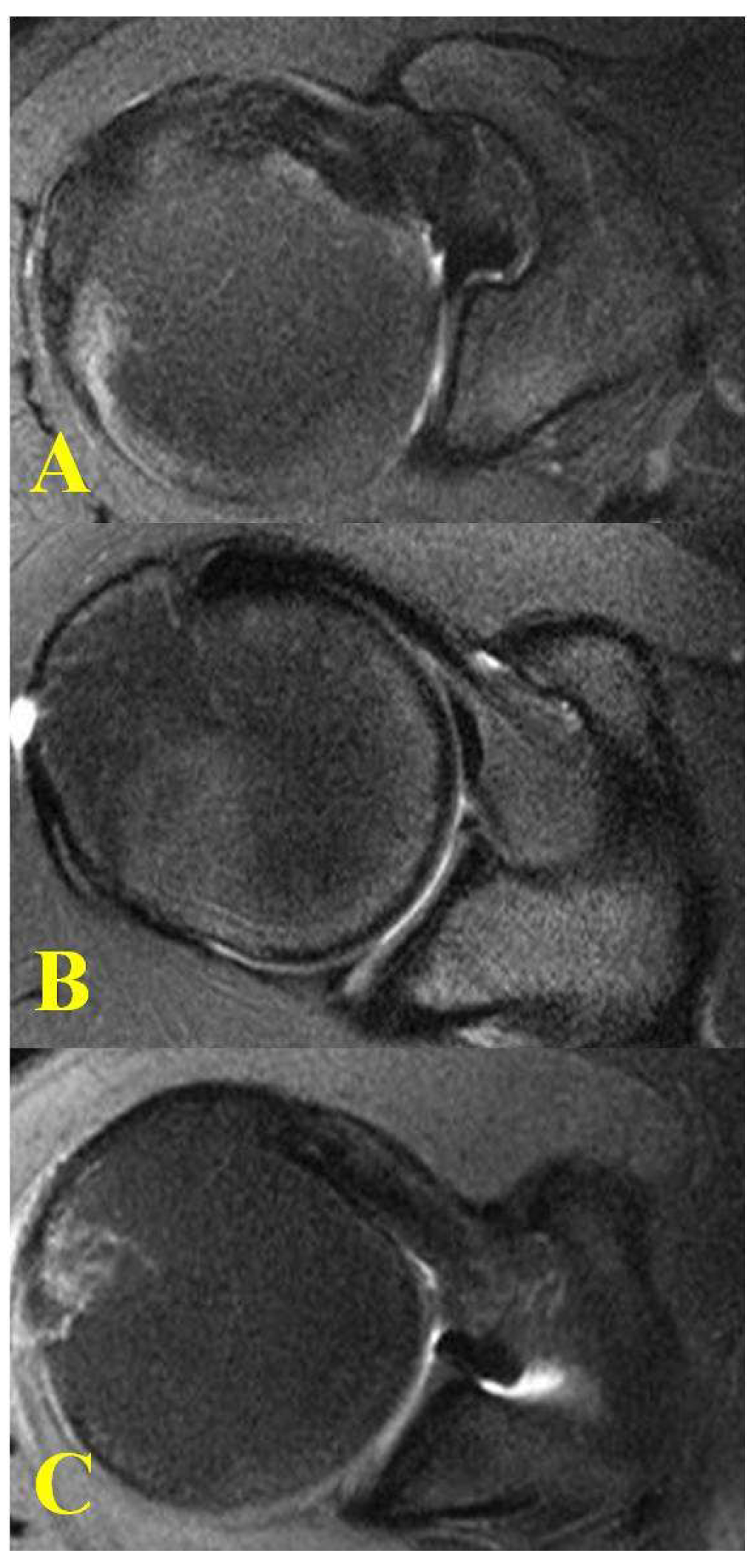
2. Materials and Methods
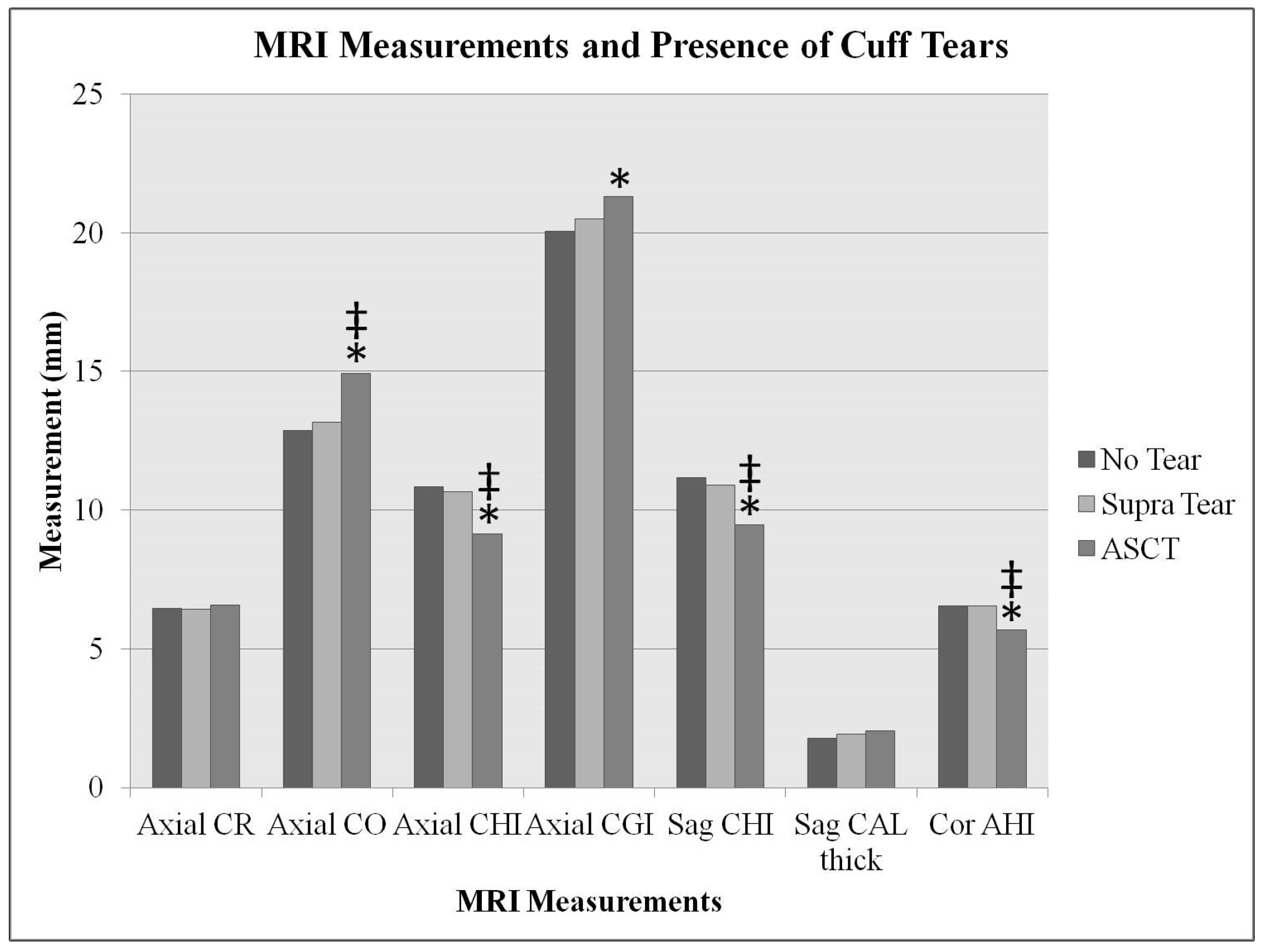
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gerber, C.; Terrier, F.; Ganz, R. The role of the coracoid process in the chronic impingement syndrome. J. Bone Jt. Surg. 1985, 67, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Goldthwait, J. An anatomic and mechanical study of the shoulder joint, explaining many of the cases of painful shoulder, many of the recurrent dislocations and many of the cases of brachial neuralgias or neuritis. J. Bone Jt. Surg. 1909, 6, 579–606. [Google Scholar]
- Burns, W.; Whipple, T. Anatomic relationships in the shoulder impingement syndrome. Clin. Orthop. Relat. Res. 1993, 294, 96–102. [Google Scholar] [CrossRef]
- Dines, D.; Warren, R.; Inglis, A. Surgical treatment of lesions of the long head of the biceps. Clin. Orthop. Relat. Res. 1982, 164, 165–171. [Google Scholar] [CrossRef]
- Dumontier, C.; Sautet, A.; Gagey, O.; Apoil, A. Rotator interval lesions and their relation to coracoid impingement syndrome. J. Shoulder Elbow Surg. 1999, 8, 130–135. [Google Scholar] [CrossRef]
- Cunningham, G.; Lädermann, A. Redefining anterior shoulder impingement: A literature review. Int. Orthop. 2018, 42, 359–366. [Google Scholar] [CrossRef]
- Lo, I.; Parten, P.; Burkhart, S. Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: An arthroscopic approach. Arthroscopy 2003, 19, 1068–1078. [Google Scholar] [CrossRef]
- Suenaga, N.; Minami, A.; Kaneda, K. Postoperative subcoracoid impingement syndrome in patients with rotator cuff tear. J. Shoulder Elbow Surg. 2000, 9, 275–278. [Google Scholar] [CrossRef]
- Mallac, C. Uncommon Injuries Subcoracoid Impingement. Sports Injury Bulletin. Available online: https://www.sportsinjurybulletin.com/uncommon-injuries-subcoracoid-impingement/ (accessed on 25 February 2022).
- Colas, F.; Nevoux, J.; Gagey, O. The subscapular and subcoracoid bursae: Descriptive and functional anatomy. J. Shoulder Elbow Surg. 2004, 13, 454–458. [Google Scholar] [CrossRef]
- Harrison, A.; Flatow, E. Subacromial impingement syndrome. J. Am. Acad. Orthop. Surg. 2011, 19, 701–708. [Google Scholar] [CrossRef]
- McKernan, M.; Schickendantz MFrangiamore, S.J. Diagnosis and Management of Subcoracoid Impingement. J. Am. Acad. Orthop. Surg. 2021, 29, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Lo, I.; Burkhart, S. Arthroscopic coracoplasty through the rotator interval. Arthroscopy 2003, 19, 667–671. [Google Scholar] [CrossRef]
- Warner, J.; Higgins, L.; Parsons, I.; Dowdy, P. Diagnosis and treatment of anterosuperior rotator cuff tears. J. Shoulder Elbow Surg. 2001, 10, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Dines, D.; Warren, R.; Inglis, A.; Pavlov, H. The coracoid impingement syndrome. J. Bone Jt. Surg. 1990, 72, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Freehill, M. Coracoid impingement: Diagnosis and treatment. J. Am. Acad. Orthop. Surg. 2011, 19, 191–197. [Google Scholar] [CrossRef]
- Kragh, J.; Doukas, W.; Basamania, C. Primary coracoid impingement syndrome. Am. J. Orthop. (Belle Mead NJ) 2004, 33, 229–232. [Google Scholar]
- Paulson, M.; Watnik, N.; Dines, D. Coracoid impingement syndrome, rotator interval reconstruction, and biceps tenodesis in the overhead athlete. Orthop. Clin. 2001, 32, 485–493. [Google Scholar] [CrossRef]
- Karnaugh, R.; Sperling, J.; Warren, R. Arthroscopic treatment of coracoid impingement. Arthroscopy 2001, 17, 784–787. [Google Scholar] [CrossRef]
- Goutallier, D.; Postel, J.; Bernageau, J.; Lavau, L.; Voisin, M. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994, 304, 78–83. [Google Scholar] [CrossRef]
- Gladstone, J.; Bishop, J.; Lo, I.; Flatow, E. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am. J. Sports Med. 2007, 35, 719–728. [Google Scholar] [CrossRef]
- Liem, D.; Lichtenberg, S.; Magosch, P.; Habermeyer, P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J. Bone Jt. Surg. 2007, 89, 1770–1776. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, D.; de Beer, J.; du Toit, F. Coracoid process anatomy: Implications in radiographic imaging and surgery. Clin. Anat. 2007, 20, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Neto, A.; Almeida, A.; Maiorino, R.; Zoppi Filho, A.; Benegas, E. An anatomical study of the subcoracoid space. Clinics 2006, 61, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Kleist, K.; Freehill, M.; Hamilton, L.; Buss, D.; Fritts, H. Computed tomography analysis of the coracoid process and anatomic structures of the shoulder after arthroscopic coracoid decompression: A cadaveric study. J. Shoulder Elbow Surg. 2007, 16, 245–250. [Google Scholar] [CrossRef]
- Tham, A.; Purchase, R.; Kelly, J. The relation of the coracoid process to the glenoid: An anatomic study. Arthroscopy 2009, 25, 846–848. [Google Scholar] [CrossRef]
- Armitage, M.; Elkinson, I.; Giles, J.; Athwal, G. An anatomic, computed tomographic assessment of the coracoid process with special reference to the congruent-arc latarjet procedure. Arthroscopy 2011, 27, 1485–1489. [Google Scholar] [CrossRef]
- Gerber, C.; Terrier, F.; Zehnder, R.; Ganz, R. The subcoracoid space. An anatomic study. Clin. Orthop. Relat. Res. 1987, 215, 132–138. [Google Scholar] [CrossRef]
- Bonutti, P.; Norfray, J.; Friedman, R.; Genez, B. Kinematic MRI of the shoulder. J. Comput. Assist. Tomogr. 1993, 17, 666–669. [Google Scholar] [CrossRef]
- Friedman, R.; Bonutti, P.; Genez, B. Cine magnetic resonance imaging of the subcoracoid region. Orthopedics 1998, 21, 545–548. [Google Scholar]
- Giaroli, E.; Major, N.; Lemley, D.; Lee, J. Coracohumeral interval imaging in subcoracoid impingement syndrome on MRI. AJR Am. J. Roentgenol. 2006, 186, 242–246. [Google Scholar] [CrossRef]
- Tan, V.; Moore, R.; Omarini, L.; Kneeland, J.; Williams, G.; Iannotti, J. Magnetic resonance imaging analysis of coracoid morphology and its relation to rotator cuff tears. Am. J. Orthop. (Belle Mead NJ) 2002, 31, 329–333. [Google Scholar]
- Richards, D.; Burkhart, S.; Campbell, S. Relation between narrowed coracohumeral distance and subscapularis tears. Arthroscopy 2005, 21, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Park, S.; Keum, J.; Oh, J.; Park, J. The diagnosis and prognosis of impingement syndrome in the shoulder with using quantitative SPECT assessment: A prospective study of 73 patients and 24 volunteers. Clin. Orthop. Surg. 2009, 1, 194–200. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tracy, M.; Trella, T.; Nazarian, L.; Tuohy, C.; Williams, G. Sonography of the coracohumeral interval: A potential technique for diagnosing coracoid impingement. J. Ultrasound Med. 2010, 29, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Asal, N.; Şahan, M.H. Radiological Variabilities in Subcoracoid Impingement: Coracoid Morphology, Coracohumeral Distance, Coracoglenoid Angle, and Coracohumeral Angle. Med. Sci. Monit. 2018, 24, 8678–8684. [Google Scholar] [CrossRef]
- Osti, L.; Buda, M.; Del Buono, A. Fatty infiltration of the shoulder: Diagnosis and reversibility. Muscles Ligaments Tendons J. 2013, 3, 351–354. [Google Scholar] [CrossRef]
- Lädermann, A. The law of use and disuse: Critical Shoulder angle and rotator cuff tears—Association does not imply causation. Arthroscopy 2020, 36, 2342–2343. [Google Scholar] [CrossRef]

| No Tear (n = 63) | Supraspinatus Tear (n = 72) | Anterosuperior Rotator Cuff Tears (ASCT) (n = 58) | |
|---|---|---|---|
| Age | 52.2 ± 9.56 (40.3–87.2) | 54.9 ± 8.76 (40.5–80) | 60.3 ± 10.01 (42–87.6) * |
| Sex | |||
| Male | 28 | 37 | 37 |
| Female | 35 | 35 | 21 |
| Coracoid Morphology | |||
| Flat | 5 | 9 | 1 |
| Curved | 34 | 42 | 46 * |
| Hooked | 24 | 21 | 11 |
| No Tear (mm) (n = 63) | Supraspinatus Tear (mm) (n = 72) | Anterosuperior Rotator Cuff Tears (ASCT) (mm) (n = 58) | No Tear vs. Supraspinatus Tear | No Tear vs. ASCT | Supraspinatus Tear vs. ASCT | |
|---|---|---|---|---|---|---|
| p-Value | p-Value | p-Value | ||||
| Axial CR | 6.45 ± 1.72 (3.5–10.5) | 6.42 ± 1.61 (1.8–10.2) | 6.59 ± 1.7 (2.6–11) | 0.920 | 0.668 | 0.577 |
| Axial CO | 12.87 ± 4.91 (2.1–22.1) | 13.15 ± 4.78 (2.7–25.6) | 14.92 ± 4.64 (5.1–24.8) | 0.739 | 0.020 * | 0.035 * |
| Axial CHI | 10.83 ± 3.1 (6.1–20.6) | 10.65 ± 3.33 (4.9–19.4) | 9.14 ± 2.92 (2.8–16.1) | 0.746 | 0.003 * | 0.007 * |
| Axial CGI | 20.04 ± 3.51 (13.2–27.4) | 20.49 ± 3.06 (13.5–28.4) | 21.3 ± 3.18 (15.1–28.7) | 0.425 | 0.042 * | 0.146 |
| CG angle | 146.79 ± 10.3 (127–176) | 146.97 ± 11.52 (121–174) | 143.14 ± 9.74 (126–167) | 0.925 | 0.048 * | 0.046 * |
| Sag CHI | 11.173 ± 3.25 (5.9–24.4) | 10.9 ± 3.31 (4.1–19.6) | 9.47 ± 2.63 (2.6–16.1) | 0.625 | 0.002 * | 0.009 * |
| Sag CAL thickness | 1.78 ± 0.66 (0.8–4.1) | 1.92 ± 0.69 (0.9–3.7) | 2.03 ± 0.75 (0.9–4.6) | 0.224 | 0.053 | 0.389 |
| Cor AHI | 6.54 ± 1.29 (2–9.7) | 6.53 ± 1.37 (3.9–11.4) | 5.69 ± 1.84 (1.4–8.9) | 0.978 | 0.004 * | 0.003 * |
| No Tear (mm) (n = 63) | Supraspinatus Tear (mm) (n = 72) | Anterosuperior Rotator Cuff Tears (ASCT) (mm) (n = 58) | No Tear vs. Supraspinatus Tear | No Tear vs. ASCT | Supraspinatus Tear vs. ASCT | |
|---|---|---|---|---|---|---|
| p-Value | p-Value | p-Value | ||||
| Goutallier Subscap | 0.4 ± 0.75 (0–3) | 0.37 ± 0.54 (0–2) | 1.34 ± 0.91 (0–3) | 0.846 | 0.001 * | 0.001 * |
| Goutallier Supra | 0.78 ± 0.94 (0–4) | 1.15 ± 0.99 (0–4) | 1.9 ± 1.24 (0–4) | 0.026 * | 0.001 * | 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Amin, S.F., III; Maffulli, N.; Mai, M.C.; Rodriguez, H.C.; Jaso, V.; Cannon, D.; Gupta, A. Coracoid Impingement and Morphology Is Associated with Fatty Infiltration and Rotator Cuff Tears. J. Clin. Med. 2022, 11, 2661. https://doi.org/10.3390/jcm11092661
El-Amin SF III, Maffulli N, Mai MC, Rodriguez HC, Jaso V, Cannon D, Gupta A. Coracoid Impingement and Morphology Is Associated with Fatty Infiltration and Rotator Cuff Tears. Journal of Clinical Medicine. 2022; 11(9):2661. https://doi.org/10.3390/jcm11092661
Chicago/Turabian StyleEl-Amin, Saadiq F., III, Nicola Maffulli, Matthew C. Mai, Hugo C. Rodriguez, Victoria Jaso, Dylan Cannon, and Ashim Gupta. 2022. "Coracoid Impingement and Morphology Is Associated with Fatty Infiltration and Rotator Cuff Tears" Journal of Clinical Medicine 11, no. 9: 2661. https://doi.org/10.3390/jcm11092661
APA StyleEl-Amin, S. F., III, Maffulli, N., Mai, M. C., Rodriguez, H. C., Jaso, V., Cannon, D., & Gupta, A. (2022). Coracoid Impingement and Morphology Is Associated with Fatty Infiltration and Rotator Cuff Tears. Journal of Clinical Medicine, 11(9), 2661. https://doi.org/10.3390/jcm11092661









