Association between the Right Ventricular Longitudinal Shortening Fraction and Mortality in Acute Respiratory Distress Syndrome Related to COVID-19 Infection: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
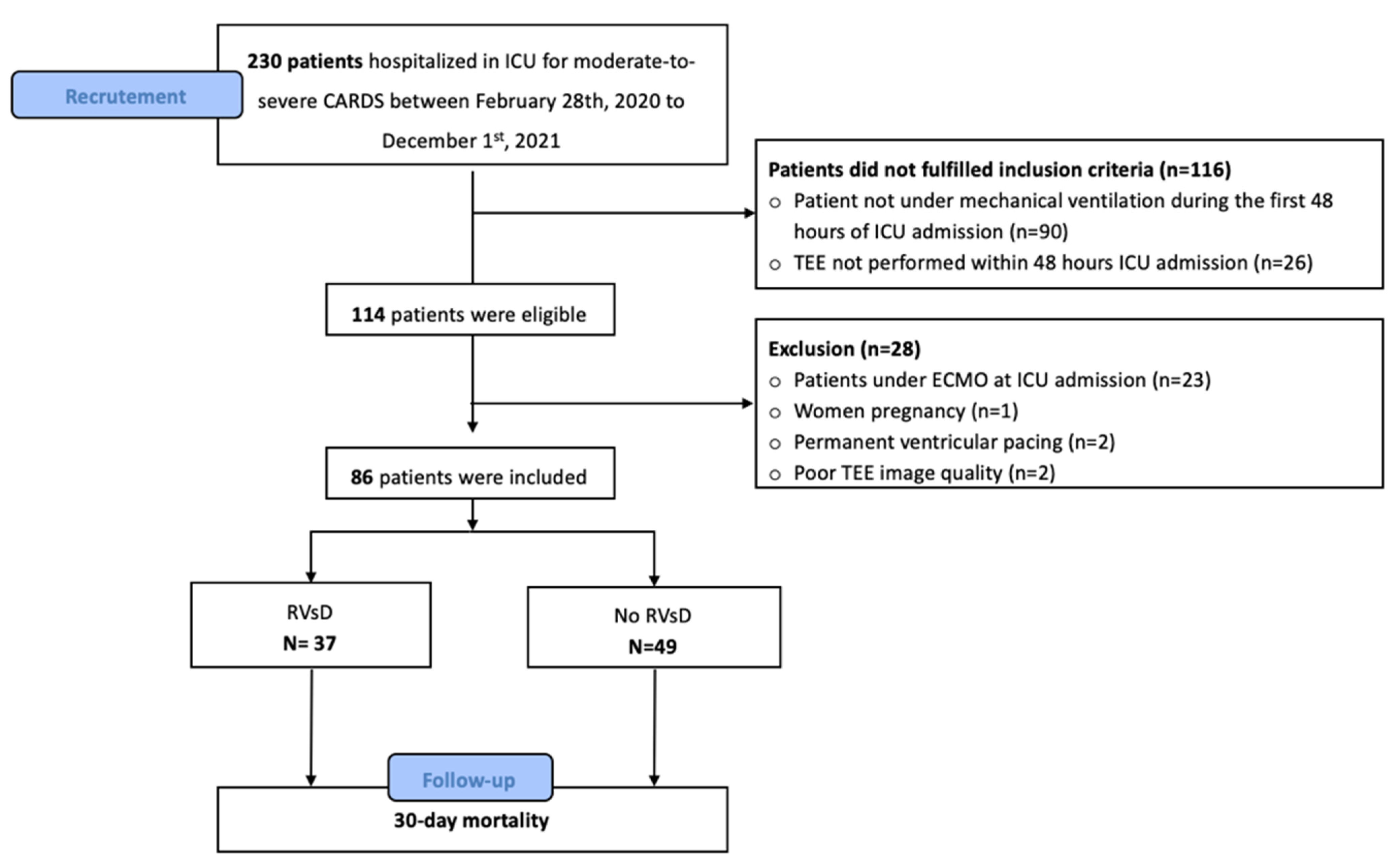
2.1. Population
2.2. Ethics
2.3. Data
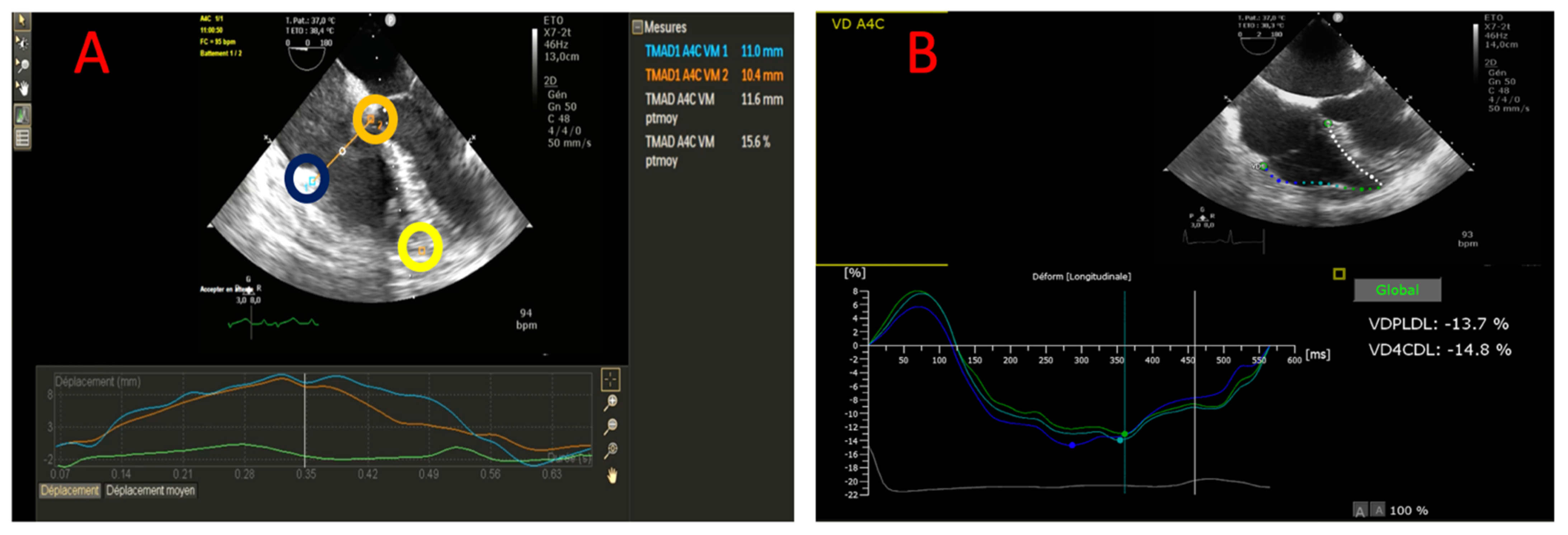
2.4. TEE Measurement
2.5. Statistical Analysis
3. Results
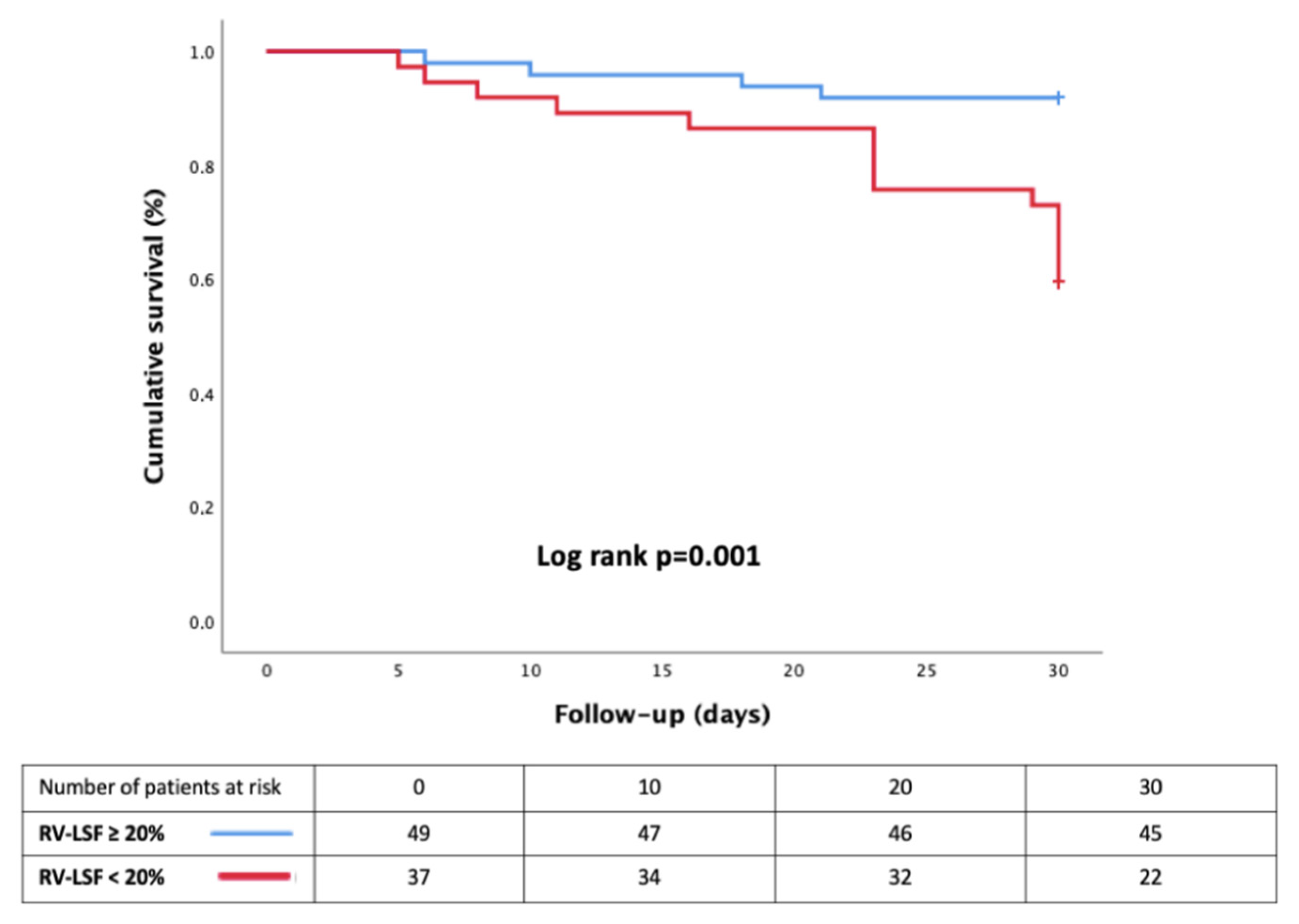
Mortality Risk Factors
4. Discussion
4.1. RVsD in CARDS
4.2. RVD Dysfunction and COVID-19 Infection
4.3. RV-LSF and Mortality
4.4. Bi-Ventricular Dysfunction
5. Limits
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Corica, B.; Marra, A.M.; Basili, S.; Cangemi, R.; Cittadini, A.; Proietti, M.; Romiti, G.F. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 17774. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieillard-Baron, A.; Matthay, M.; Teboul, J.L.; Bein, T.; Schultz, M.; Magder, S.; Marini, J.J. Experts’ opinion on management of hemodynamics in ARDS patients: Focus on the effects of mechanical ventilation. Intensive Care Med. 2016, 42, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Lhéritier, G.; Legras, A.; Caille, A.; Lherm, T.; Mathonnet, A.; Frat, J.P.; Courte, A.; Martin-Lefèvre, L.; Gouëllo, J.-P.; Amiel, J.-B.; et al. Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: A multicenter study. Intensive Care Med. 2013, 39, 1734–1742. [Google Scholar] [CrossRef] [PubMed]
- Nicoara, A.; Skubas, N.; Ad, N.; Finley, A.; Hahn, R.T.; Mahmood, F.; Mankad, S.; Nyman, C.B.; Pagani, F.; Porter, T.R.; et al. Guidelines for the Use of Transesophageal Echocardiography to Assist with Surgical Decision-Making in the Operating Room: A Surgery-Based Approach. J. Am. Soc. Echocardiogr. 2020, 33, 692–734. [Google Scholar] [CrossRef] [PubMed]
- Gibson, L.E.; Fenza, R.D.; Lang, M.; Capriles, M.I.; Li, M.D.; Kalpathy-Cramer, J.; Little, B.P.; Arora, P.; Mueller, A.L.; Ichinose, P.; et al. Right Ventricular Strain Is Common in Intubated COVID-19 Patients and Does Not Reflect Severity of Respiratory Illness. J. Intensive Care Med. 2021, 36, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, H.; Zhu, S.; Xie, Y.; Wang, B.; He, L.; Zhang, D.; Zhang, Y.; Yuan, H.; Wu, C.; et al. Prognostic Value of Right Ventricular Longitudinal Strain in Patients with COVID-19. JACC: Cardiovasc. Imaging 2020, 13, S1936878X20303429. [Google Scholar] [CrossRef] [PubMed]
- Maniwa, N.; Hozumi, T.; Takemoto, K.; Wada, T.; Kashiwagi, M.; Shimamura, K.; Shiono, Y.; Kuroi, A.; Matsuo, Y.; Ino, Y.; et al. Value of tissue-tracking tricuspid annular plane by speckle-tracking echocardiography for the assessment of right ventricular systolic dysfunction. Echocardiography 2019, 36, 110–118. [Google Scholar] [CrossRef] [Green Version]
- Beyls, C.; Bohbot, Y.; Caboche, M.; Huette, P.; Haye, G.; Dupont, H.; Mahjoub, Y.; Osama, A.-A. Preload Dependency of 2D Right Ventricle Speckle Tracking Echocardiography Parameters in Healthy Volunteers: A Prospective Pilot Study. J. Clin. Med. 2021, 11, 19. [Google Scholar] [CrossRef]
- Beyls, C.; Bohbot, Y.; Huette, P.; Booz, T.; Daumin, C.; Abou-Arab, O.; Mahjoub, Y. Usefulness of right ventricular longitudinal shortening fraction to detect right ventricular dysfunction in acute cor pulmonale related to COVID-19. J. Cardiothorac. Vasc. Anesth. 2021, 35, S1053077021000604. [Google Scholar] [CrossRef]
- Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Aubron, C.; Brochard, L.; Chiche, J.D.; Combes, A.; Dreyfuss, D.; Forel, J.-M.; Guérin, C.; Jaber, S.; Mekontso-Dessap, A.; et al. Formal guidelines: Management of acute respiratory distress syndrome. Ann. Intensive Care 2019, 9, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popescu, B.A.; Andrade, M.J.; Badano, L.P.; Fox, K.F.; Flachskampf, F.A.; Lancellotti, P.; Varga, A.; Sicari, R.; Evangelista, A.; Nihoyannopoulos, P.; et al. European Association of Echocardiography recommendations for training, competence, and quality improvement in echocardiography. Eur. J. Echocardiogr. 2009, 10, 893–905. [Google Scholar] [CrossRef] [Green Version]
- Mekontso Dessap, A.; Boissier, F.; Charron, C.; Bégot, E.; Repessé, X.; Legras, A.; Brun-Buisson, C.; Vignon, P.; Vieillard-Baron, A. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: Prevalence, predictors, and clinical impact. Intensive Care Med. 2016, 42, 862–870. [Google Scholar] [CrossRef]
- Alonso, P.; Andrés, A.; Miró, V.; Igual, B.; Sánchez, I.; Salvador, A. Diagnostic power of echocardiographic speckle tracking of the tricuspid annular motion to assess right ventricular dysfunction. Int. J. Cardiol. 2014, 172, e218–e219. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef]
- Voigt, J.-U.; Cvijic, M. 2- and 3-Dimensional Myocardial Strain in Cardiac Health and Disease. JACC Cardiovasc. Imaging 2019, 12, 1849–1863. [Google Scholar] [CrossRef]
- Chotalia, M.; Ali, M.; Alderman, J.E.; Kalla, M.; Parekh, D.; Bangash, M.N.; Patel, J.M. Right Ventricular Dysfunction and Its Association with Mortality in Coronavirus Disease 2019 Acute Respiratory Distress Syndrome. Crit. Care Med. 2021, 49, 1757–1768. [Google Scholar] [CrossRef]
- Mahjoub, Y.; Rodenstein, D.O.; Jounieaux, V. Severe COVID-19 disease: Rather AVDS than ARDS? Crit. Care 2020, 24, 327. [Google Scholar] [CrossRef]
- Lang, M.; Som, A.; Mendoza, D.P.; Flores, E.J.; Reid, N.; Carey, D.; Li, M.D.; Witkin, A.; Rodriguez-Lopez, J.M.; Shepard, J.-A.O.; et al. Hypoxaemia related to COVID-19: Vascular and perfusion abnormalities on dual-energy CT. Lancet Infect. Dis. 2020, 20, S1473309920303674. [Google Scholar] [CrossRef]
- Mahjoub, Y.; Rodenstein, D.; Jounieaux, V. AVDS should not dethrone ARDS. Crit. Care 2021, 25, 400. [Google Scholar] [CrossRef] [PubMed]
- Caravita, S.; Baratto, C.; Di Marco, F.; Calabrese, A.; Balestrieri, G.; Russo, F.; Faini, A.; Soranna, D.; Perego, G.B.; Badano, L.P.; et al. Haemodynamic characteristics of COVID-19 patients with acute respiratory distress syndrome requiring mechanical ventilation. An invasive assessment using right heart catheterization. Eur. J. Heart Fail. 2020, 22, 2228–2237. [Google Scholar] [CrossRef] [PubMed]
- Helms, J.; Combes, A.; Aissaoui, N. Cardiac injury in COVID-19. Intensive Care Med. 2021, 48, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Van den Heuvel, F.M.A.; Vos, J.L.; Koop, Y.; Van Dijk, A.P.J.; Duijnhouwer, A.L.; De Mast, Q.; van de Veerdonk, F.L.; Bosch, F.; Kok, B.; Netea, M.G.; et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth. Heart J. 2020, 28, 410–417. [Google Scholar] [CrossRef]
- Park, J.; Kim, Y.; Pereira, J.; Hennessey, K.C.; Faridi, K.F.; McNamara, R.L.; Velazquez, E.J.; Hur, D.J.; Sugeng, L.; Agarwal, V. Understanding the role of left and right ventricular strain assessment in patients hospitalized with COVID-19. Am. Heart J. Plus Cardiol. Res. Pract. 2021, 6, 100018. [Google Scholar] [CrossRef]
- Bieber, S.; Kraechan, A.; Hellmuth, J.C.; Muenchhoff, M.; Scherer, C.; Schroeder, I.; Irlbeck, M.; Kaeaeb, S.; Massberg, S.; Hausleiter, J.; et al. Left and right ventricular dysfunction in patients with COVID-19-associated myocardial injury. Infection 2021, 49, 491–500. [Google Scholar] [CrossRef]
- DiLorenzo, M.P.; Bhatt, S.M.; Mercer-Rosa, L. How best to assess right ventricular function by echocardiography. Cardiol. Young 2015, 25, 1473–1481. [Google Scholar] [CrossRef]
- Loo, J.; Spittle, D.A.; Newnham, M. COVID-19, immunothrombosis and venous thromboembolism: Biological mechanisms. Thorax 2021, 76, 412–420. [Google Scholar] [CrossRef]
- Shantsila, E.; Lip, G.Y.H. Thrombotic Complications in Heart Failure: An Underappreciated Challenge. Circulation 2014, 130, 387–389. [Google Scholar] [CrossRef] [Green Version]
- Bleakley, C.; Singh, S.; Garfield, B.; Morosin, M.; Surkova, E.; Mandalia, M.S.; Dias, B.; Androulakis, E.; Price, L.C.; McCabe, C.; et al. Right ventricular dysfunction in critically ill COVID-19 ARDS. Int. J. Cardiol. 2020, 327, 251–258. [Google Scholar] [CrossRef]
- Lemarié, J.; Maigrat, C.-H.; Kimmoun, A.; Dumont, N.; Bollaert, P.E.; Selton-Suty, C.; Gibot, S.; Huttin, O. Feasibility, reproducibility and diagnostic usefulness of right ventricular strain by 2-dimensional speckle-tracking echocardiography in ARDS patients: The ARD strain study. Ann. Intensive Care 2020, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Badano, L.P.; Kolias, T.J.; Muraru, D.; Abraham, T.P.; Aurigemma, G.; Edvardsen, T.; D’Hooge, J.; Donal, E.; Fraser, A.G.; Marwick, T.; et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: A consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur. Heart J.-Cardiovasc. Imaging 2018, 19, 591–600. [Google Scholar] [CrossRef]
- Toulouse, E.; Masseguin, C.; Lafont, B.; McGurk, G.; Harbonn, A.; Roberts, J.A.; Granier, S.; Dupeyron, A.; Bazinijk, J.E. French legal approach to clinical research. Anaesth. Crit. Care Pain Med. 2018, 37, 607–614. [Google Scholar] [CrossRef] [Green Version]
| Variables | No RVsD (n = 49) | RVsD (n = 37) | p |
|---|---|---|---|
| Age (years) | 63 (59–69) | 59 (55–68) | 0.13 |
| BMI (kg·m−2) | 29.3 (25.8–34.4) | 30.1 (24.8–35.8) | 0.87 |
| Male gender (n; %) | 35 (71) | 27 (73) | 0.47 |
| SAPS II score | 45 (29–66) | 51 (30–63) | 0.94 |
| Medical history, n (%) | |||
| No history | 7 (14) | 5 (13) | 1 |
| Hypertension | 30 (61) | 16 (43) | 0.12 |
| Diabetes | 15 (30) | 8 (21) | 0.46 |
| Dyslipidemia | 12 (24) | 15 (41) | 0.16 |
| Smoking (former or active) | 6 (12) | 6 (16) | 0.75 |
| Chronic kidney disease | 4 (8) | 4 (11) | 0.72 |
| COPD/asthma | 4 (8) | 7 (19) | 0.19 |
| Coronary or peripheral artery disease | 5 (10) | 4 (11) | 1 |
| CT scan (n = 86/86), n (%) | |||
| Ground-glass opacification | 42 (85) | 36 (97) | 1 |
| Consolidation | 25 (51) | 22 (59) | 0.81 |
| Crazy paving | 15 (31) | 7 (19) | 0.21 |
| Lung involvement > 50% | 22 (44) | 19 (51) | 0.66 |
| Pulmonary embolism | 1(3) | 4 (10) | 0.16 |
| Biological data before TEE | |||
| Lactate (mmol−1) | 2.0 (1.7–2.4) | 2.1 (1.5–2.5) | 0.56 |
| Serum-creatinine (µmol·L−1) | 69 (58–88) | 86 (69–107) | 0.07 |
| BNP (pg·mL−1) | 53 (32–110) | 59 (18–209) | 0.79 |
| Troponine Tc HS (ng·mL−1) | 24 (11–51) | 34 (10–66) | 0.27 |
| Procalcitonin (µg·L−1) | 0.54 (0.19–1.72) | 0.55 (0.22–2.26) | 0.93 |
| C reactive protein, mg L−1 | 181 (96–263) | 156 (90–220) | 0.72 |
| Time from first symptoms to ICU admission (days) | 8 (6–11) | 7 (4–9) | 0.60 |
| No RV Dysfunction (n = 49) | RV Dysfunction (n = 37) | p | |
|---|---|---|---|
| Hemodynamic parameters during TEE | |||
| Heart rate (bpm) | 82 [72–92] | 82 [71–97] | 0.89 |
| Systolic blood pressure (mmHg) | 131 [112–151] | 124 [109–141] | 0.21 |
| Mean blood pressure (mmHg) | 85 [71–96] | 84 [70–98] | 0.78 |
| Diastolic blood ressure (mmHg) | 66 [55–78] | 78 [60–80] | 0.28 |
| Ventilator settings during TEE | |||
| Tidal volume (mL·kg−1) | 5.9 (5.5–6.8) | 6.0 (5.3–6.6) | 0.75 |
| PaO2/FiO2 (mmHg) | 103 (80–167) | 110 (90–168) | 0.59 |
| Positive end expiratory pressure, (cmH2O) | 12 (10–14) | 12 (10–14) | 0.62 |
| Respiratory rate | 27 (24–31) | 28 (24–30) | 0.81 |
| Plateau pressure (cmH2O) | 26 (23–28) | 27 (24–30) | 0.23 |
| Driving pressure | 14 (11–16) | 14 (12–17) | 0.37 |
| Respiratory system Compliance (mL·cmH2O−1) | 30.3 (28.1–36.2) | 33.8 (29.3–38.3) | 0.26 |
| Rescue therapy | |||
| Neuromuscular blocker, n (%) | 49 (100) | 37 (100) | 1 |
| Inhaled nitric oxide, n (%) | 31 (63) | 22 (59) | 0.53 |
| Vasopressor use, n (%) | 24 (49) | 23 (63) | 0.28 |
| - Norepinephrine, (µ/kg/min) | 0 (0–0.16) | 0.15 (0–0.61) | 0.01 |
| Vasoactive-inotropic score (VIS) | 0 (0–16) | 15 (0–61) | 0.01 |
| SOFA cv | 0 (0–4) | 4 (0–4) | 0.02 |
| TEE parameters | |||
| RV EDA | 18.5 (14.9–22.0) | 22.4 (18.7–26.7) | 0.006 |
| RV ESA | 9.7 (7.5–12.0) | 13.0 (11.2–18.4) | 0.001 |
| RV EDA/LV EDA | 0.68 (0.56–0.88) | 1.06 (0.71–1.15) | 0.003 |
| RV-FAC (%) | 48.7 (41.1–54.7) | 41.2 (32.0–46.9) | 0.003 |
| Acute cor pulmonale | 10 (20) | 18 (49) | 0.005 |
| - BNP (pg·mL−1) | 19 (11–52) | 39 (16–105) | 0.21 |
| - Troponine Tc HS (ng·mL−1) | 41 (21–83) | 59 (25–115) | 0.57 |
| - Lactate (mmol−1) | 1.8 (1.0–2.1) | 1.9 (1.1–2.4) | 0.46 |
| Left ventricular ejection fraction (%) | 65.6 (57.3–72.0) | 56.1 (42.9–67.9) | 0.03 |
| Cardiac output (L·min−1) | 5.0 (4.5–6.5) | 4.4 (2.9–6.7) | 0.06 |
| Valvular heart disease | |||
| - Severe mitral regurgitation | 1 | 1 | - |
| - Severe aortic regurgitation | 1 | 0 | - |
| 2D-STE parameters (n = 81/86) | |||
| RV-GLS (%) | 20.7 (16.9–27.5) | 17.9 (13.2–20.7) | 0.005 |
| RV-FWLS (%) | 25 (20.5–29.8) | 20.2 (16.4–25.6) | 0.002 |
| TAD parameters | |||
| ❖ TADlat (mm) | 23.0 (20.5–26.7) | 15.7 (12.0–18.1) | 0.0001 |
| ❖ TADsep (mm) | 14.0 (10.0–15.6) | 8.1 (7.2–10.3) | 0.0001 |
| ❖ RV-LSF (%) | 26.0 (23.0–29.4) | 16.5 (13.7–19.4) | 0.0001 |
| No RV Dysfunction (n = 49) | RV Dysfunction (n = 37) | p | |
|---|---|---|---|
| Outcomes † | |||
| Ventilator acquired pneumonia | 38 (76) | 32 (65) | 0.56 |
| Renal replacement therapy | 13 (26) | 12 (31) | 0.63 |
| Pulmonary embolism | 3 (6) | 8 (22) | 0.04 |
| Cardiogenic shock | 2 (4) | 7 (19) | 0.03 |
| Veno-venous ECMO * | 7 (14) | 8 (22) | 0.41 |
| Veno-arterial ECMO * | 0 | 2 (5) | 0.18 |
| Time under mechanical ventilation | 17 (11–28) | 20 (11–31) | 0.70 |
| 30-day mortality (n, %) | 4 (8) | 15 (40) | 0.0001 |
| Length of stay in ICU (days) | 21 (15–44) | 23 (11–35) | 0.42 |
| In-hospital mortality (n, %) | 12 (24) | 17 (46) | 0.04 |
| Hospital length of stay (days) | 32 19–49 | 39 24–55 | 0.35 |
| In-hospital mortality causes (n, %) | |||
| Cardiogenic shock | 2 | 5 | 0.13 |
| Respiratory failure | 3 | 5 | 0.28 |
| Multiple organ failure | 5 | 6 | 0.51 |
| End of life decision | 2 | 1 | 1 |
| Variables | 30 Days Mortality | |||
|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | |||
| HR (95% CI) | p | HR (95% CI) | p | |
| SAPS II (for each point) | 2.9 (1.1–7.8) | 0.03 | 1.03 (1.01–1.04) | 0.04 |
| Acute cor pulmonale | 3.44 (1.33–8.98) | 0.01 | 3.01 (1.13–7.94) | 0.03 |
| PaO2/FiO2 < 150 mmHg | 1.9 (0.55–6.59) | 0.29 | - | - |
| Driving pressure > 18 | 2.14 (0.68–6.68) | 0.19 | - | - |
| RVsD | ||||
| ∘ RV-LSF < 20% | 5.51 (1.82–16.7) | 0.002 | 4.45 (1.43–13.8) | 0.01 |
| ∘ RV-FAC < 35% | 0.72 (0.21–2.5) | 0.61 | - | - |
| ∘ RV-FWLS < 21% | 1.38 (0.56–3.4) | 0.48 | - | - |
| Pulmonary embolism before TEE | 0.81 (0.11–6.11) | 0.84 | - | - |
| SOFA cv | 1.29 (0.99–1.68) | 0.06 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beyls, C.; Daumin, C.; Hermida, A.; Booz, T.; Ghesquieres, T.; Crombet, M.; Martin, N.; Huette, P.; Jounieaux, V.; Dupont, H.; et al. Association between the Right Ventricular Longitudinal Shortening Fraction and Mortality in Acute Respiratory Distress Syndrome Related to COVID-19 Infection: A Prospective Study. J. Clin. Med. 2022, 11, 2625. https://doi.org/10.3390/jcm11092625
Beyls C, Daumin C, Hermida A, Booz T, Ghesquieres T, Crombet M, Martin N, Huette P, Jounieaux V, Dupont H, et al. Association between the Right Ventricular Longitudinal Shortening Fraction and Mortality in Acute Respiratory Distress Syndrome Related to COVID-19 Infection: A Prospective Study. Journal of Clinical Medicine. 2022; 11(9):2625. https://doi.org/10.3390/jcm11092625
Chicago/Turabian StyleBeyls, Christophe, Camille Daumin, Alexis Hermida, Thomas Booz, Tristan Ghesquieres, Maxime Crombet, Nicolas Martin, Pierre Huette, Vincent Jounieaux, Hervé Dupont, and et al. 2022. "Association between the Right Ventricular Longitudinal Shortening Fraction and Mortality in Acute Respiratory Distress Syndrome Related to COVID-19 Infection: A Prospective Study" Journal of Clinical Medicine 11, no. 9: 2625. https://doi.org/10.3390/jcm11092625
APA StyleBeyls, C., Daumin, C., Hermida, A., Booz, T., Ghesquieres, T., Crombet, M., Martin, N., Huette, P., Jounieaux, V., Dupont, H., Abou-Arab, O., & Mahjoub, Y. (2022). Association between the Right Ventricular Longitudinal Shortening Fraction and Mortality in Acute Respiratory Distress Syndrome Related to COVID-19 Infection: A Prospective Study. Journal of Clinical Medicine, 11(9), 2625. https://doi.org/10.3390/jcm11092625






