The Upshot of the SARS-CoV-2 Pandemic on Nursing Assistants: Evaluating Mental Health Indicators in Huelva
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Instruments
- Emotional exhaustion: high (≥27), medium (19–26), and low (≤18).
- Depersonalization: high (≥10), medium (6–9), and low (≤5).
- Personal realization: high (≥40), medium (34–39), and low (≤33).
2.4. Data Analysis
- -
- Cross-tabulation analyses for depersonalization, emotional exhaustion, and personal realization as a function of gender, work center, contact with SARS-CoV-2, marital status, and parent status. Chi-squared tests were also performed between these variables.
- -
- Since the normality tests for depersonalization, age, personal realization, and emotional exhaustion showed normal distribution, the Mann–Whitney U-test was chosen for the independence tests with categorical variables of two categories, and the Kruskal–Wallis H-test for three or more groups. We also examined the correlations between the different defined variables, through Spearman’s Rho.
- -
- Cross-tabulation analyzes based on the results obtained in the GHQ-12 due to depersonalization, emotional exhaustion, contact with SARS-CoV-2 and personal realization. Chi-square tests were also performed between these variables.
- -
- Cross-tabulation analyses based on the results obtained in the GHQ-12 as a function of sex, marital status, parent status and age. Chi-square tests were also performed between these variables.
3. Results
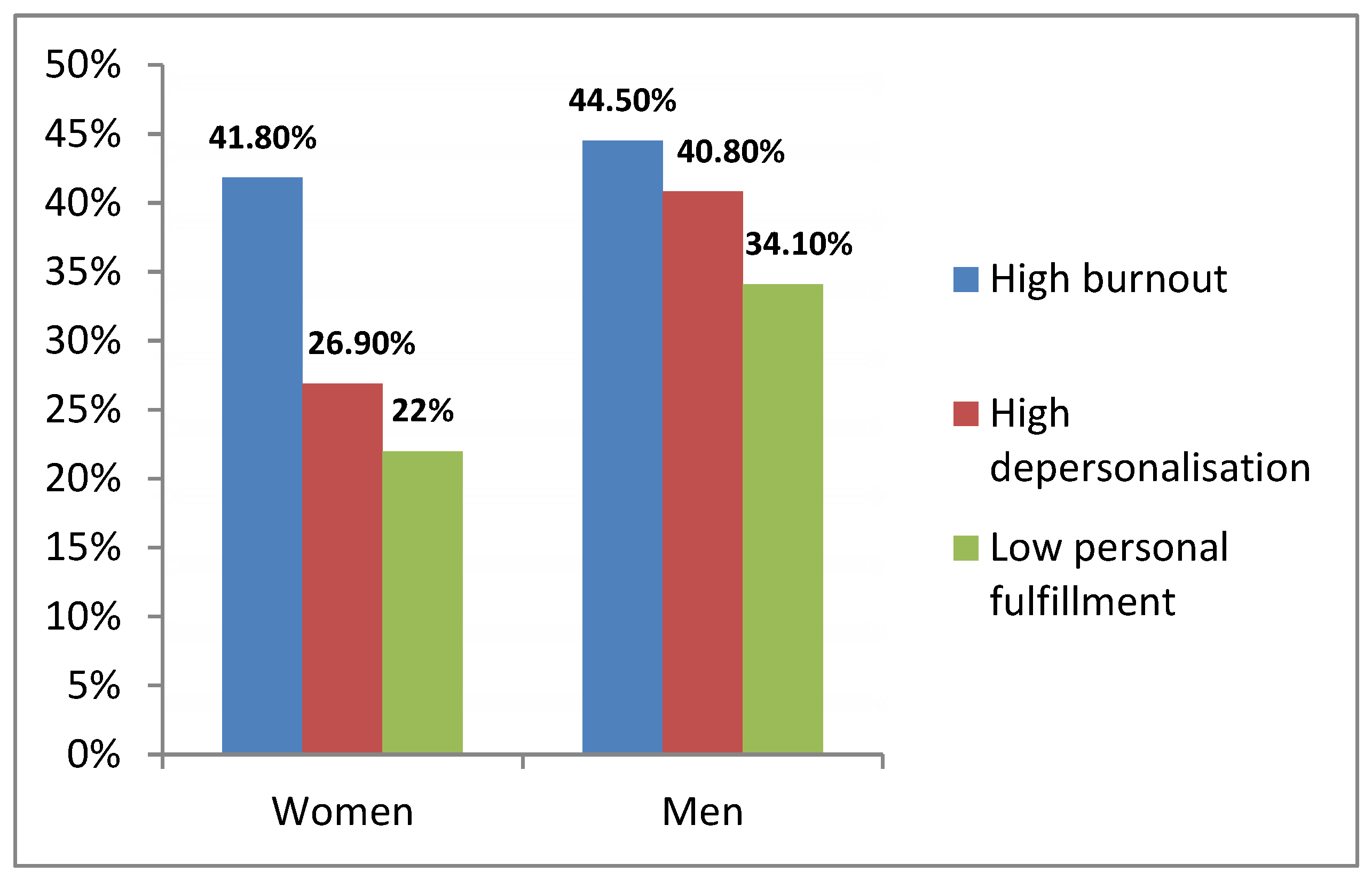
3.1. Relationship of Emotional Exhaustion, Depersonalization, and Personal Realization with Gender
3.2. Prevalence of Depersonalization, Emotional Exhaustion, and Personal Realization as a Function of Work Center
3.3. Correlation of Emotional Exhaustion, Depersonalization and Personal Realization with Age, Marital Status, and Parent Status
3.4. Correlation of Emotional Exhaustion, Depersonalization and Personal Realization with GHQ-12 Results and Situations of Contact with SARS-CoV-2 in the Workplace
3.5. Correlation of Probable Non-Psychotic Psychiatric Pathology (Positive GHQ-12) with Gender, Marital Status, Age, and Parent Status
3.6. Correlation of Probable Non-Psychotic Psychiatric Pathology (Positive GHQ-12) with Situations of Contact with SARS-CoV-2 in the Work
4. Discussion
4.1. Implications for Practice
4.2. Limitations
5. Conclusions
6. Relevance Statement
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Shanafelt, T.D.; Sinsky, C.A.; Cipriano, P.F.; Bhatt, J.; Ommaya, A.; West, C.P.; Meyers, D. Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care; NAM Perspectives. Discussion Paper; National Academy of Medicine: Washington, DC, USA, 2017; Available online: https://nam.edu/burnout-among-health-careprofessionals-a-call-to-explore-and-address-this-underrecognized-threat-to-safe-high-quality-care (accessed on 20 October 2021).
- Ruotsalainen, J.H.; Verbeek, J.H.; Mariné, A.; Serra, C. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2014, 11, CD002892. [Google Scholar] [CrossRef]
- Vivas-Manrique, S.D.; Muñoz, M.F. Síndrome de Burnout, de un fenómeno laboral a un diagnóstico médico. Rev. Colomb. de Salud Ocupacional 2019, 9, e-5662. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Bradley, K.A.; Wipf, J.E.; Back, A.L. Burnout and Self-Reported Patient Care in an Internal Medicine Residency Program. Ann. Intern. Med. 2002, 136, 358–367. [Google Scholar] [CrossRef]
- Ng, Q.X.; Lim, D.Y.; Chee, K.T. Reimagining the spectrum of affective disorders. Bipolar Disord. 2020, 22, 638–639. [Google Scholar] [CrossRef]
- Consejería de Salud y Familias de la Junta de Andalucía. Informe COVID-19 en Andalucía. Dirección General de Salud Pública y Ordenación Farmacéutica. Sistema de Vigilancia Epidemiológica de Andalucía. 2021. Available online: http://www.juntadeandalucia.es/institutodeestadisticaycartografia/salud/COVID19.html (accessed on 20 September 2020).
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory Manual, 3rd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1982. [Google Scholar]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job Burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Goldberg, D.; Williams, P. User’s Guide to the General Health Questionnaire; NFER-Nelson: Berkshire, UK, 1988. [Google Scholar]
- E Muñóz, P.; Vázquez, J.L.; Insausti, F.R.; Pastrana, E.; Varo, J. [Spanish adaptation of the General Health Questionnaire (G.H.Q.) of D. P. Goldberg (a method for identifying psychiatric cases in the community)]. Arch. de Neurobiol. 1979, 42, 139–158. [Google Scholar]
- Sánchez-López, M.D.P.; Dresch, V. The 12-Item General Health Questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema 2008, 20, 839–843. [Google Scholar]
- Gispert, R.; Rajmil, L.; Schiaffino, A.; Herdman, M. Sociodemographic and health-related correlates of psychiatric distress in a general population. Soc. Psychiatry 2003, 38, 677–683. [Google Scholar] [CrossRef]
- Ruiz, F.J.; García-Beltrán, D.M.; Suárez-Falcón, J.C. General Health Questionnaire-12 validity in Colombia and factorial equivalence between clinical and nonclinical participants. Psychiatry Res. 2017, 256, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Burrone, M.S.; Abeldaño, A.; Lucchese, M.; Susser, L.; Enders, J.; Alvarado, R.; Valencia, E.; Fernandez, R. Evaluación psicométrica y estudio de fiabilidad del cuestionario general de salud (GHQ-12) en consultantes adultos del primer nivel de atención en Córdoba—Argentina. Rev. Fac. Cien. Med. Univ. Nac. Cordoba 2015, 72, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015, 52, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Ogińska-Bulik, N. Occupational Stress and Its Consequences in Healthcare Professionals: The Role of Type D Personality. Int. J. Occup. Med. Environ. Health 2006, 19, 113–122. [Google Scholar] [CrossRef]
- Piñeiro, I.; Rodríguez, S.; Albite, A.; Freire, C.; Ferradás, M.D.M. Sobrecarga y salud percibida en cuidadores informales de pacientes con enfermedad mental. Eur. J. Health Res. 2017, 3, 185–196. [Google Scholar] [CrossRef]
- Tifner, S.; Martín, P.; de Nasetta, S.A.; de Bortoli, M.A. Burnout en el colectivo docente. Stud. Rev. De Humanid. 2006, 12, 279–291. [Google Scholar]
- Mamani-Encalada, A.; Obando-Zegarra, R.; Uribe-Malca, A.M.; Vivanco-Tello, M. Factores que desencadenan el estrés y sus consecuencias en el desempeño laboral en emergencia. Rev. Per. Obst. Enf. 2007, 3. Available online: http://www.aulavirtualusmp.pe/ojs/index.php/rpoe/article/viewFile/543/415 (accessed on 15 July 2021).
- Castro-Vázquez, Á.; Espinosa-Gutiérrez, I.; Rodríguez-Contreras, P.; Santos-Iglesias, P. Relación entre el estado de salud percibido e indicadores de salud en la población española. Int. J. Clin. Health Psychol. 2007, 7, 883–898. [Google Scholar]
- Schaufeli, W.B.; Leiter, M.P.; Maslach, C. Burnout: 35 years of research and practice. Career Dev. Int. 2009, 14, 204–220. [Google Scholar] [CrossRef]
- De Simone, S.; Planta, A.; Cicotto, G. The role of job satisfaction, work engagement, self-efficacy and agentic capacities on nurses’ turnover intention and patient satisfaction. Appl. Nurs. Res. 2018, 39, 130–140. [Google Scholar] [CrossRef]
- Elvira, J.A.M.; Cabrera, J.H. Estrés y burnout en profesores. Int. J. Clin. Health Psychol. 2004, 4, 597–621. [Google Scholar]
- Carlotto, M.S.; Câmara, S.G. Análise da produção científica sobre a Síndrome de Burnout no Brasil. Psico 2008, 39. Available online: https://revistaseletronicas.pucrs.br/ojs/index.php/revistapsico/article/view/1461 (accessed on 20 October 2021).
- Leiter, M.P.; Maslach, C. The impact of interpersonal environment on burnout and organizational commitment. J. Organ. Behav. 1988, 9, 297–308. [Google Scholar] [CrossRef]
- Toya, A.M.-D.; Gallegos, W.L.A.; Caycho-Rodríguez, T. Síndrome de burnout en médicos de la ciudad de Arequipa (Perú). Rev. Chil. De Neuro-Psiquiatr. 2019, 57, 139–148. [Google Scholar] [CrossRef]
- Marenco-Escuderos, A.D.; Ávila-Toscano, J.H. Dimensiones de apoyo social asociadas con síndrome de burnout en docentes de media académica. Pensam. Psicológico 2016, 14, 7–18. [Google Scholar] [CrossRef][Green Version]
- Ballester-Arnal, R.; Gómez-Martínez, S.; Gil Juliá, B.; Ferrándiz-Sellés, M.D.; Collado-Boira, E. Burnout y factores estresantes en profesionales sanitarios de las unidades de cuidados intensivos. Rev. De Psicopatol. Y Psicol. Clín. 2016, 21, 129–136. [Google Scholar] [CrossRef][Green Version]
- Sierra, M.; David, A.S.; Hunter, E.C.M. The epidemiology of depersonalisation and derealisation. Soc. Psychiatry 2004, 39, 9–18. [Google Scholar] [CrossRef]
- Erquicia, J.; Valls, L.; Barja, A.; Gil, S.; Miquel, J.; Leal-Blanquet, J.; Schmidt, C.; Checa, J.; Vega, D. Impacto emocional de la pandemia de COVID-19 en los trabajadores sanitarios de uno de los focos de contagio más importantes de Europa. Med. Clin. 2020, 155, 434–440. [Google Scholar] [CrossRef]
- Pérez-Ortega, S.; Mesa, R.; Fernández, C.; Valverde, J. Situación de la enfermera de cardiología durante la pandemia COVID-19. Enferm. Cardiol. 2020, 27, 82–89. [Google Scholar]
- Santamaria, M.D.; Ozamiz-Etxebarria, N.; Rodríguez, I.R.; Albondiga-Mayor, J.J.; Gorrochategui, M.P. Impacto psicológico de la COVID-19 en una muestra de profesionales sanitarios españoles. Rev. Psiquiatr. Salud. Ment. 2021, 14, 106–112. [Google Scholar] [CrossRef]
- Molina-Praena, J.; Ramirez-Baena, L.; Gómez-Urquiza, J.L.; Cañadas, G.R.; De La Fuente, E.I.; La Fuente, G.A.C.-D. Levels of Burnout and Risk Factors in Medical Area Nurses: A Meta-Analytic Study. Int. J. Environ. Res. Public Health 2018, 15, 2800. [Google Scholar] [CrossRef] [PubMed]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA J. Am. Med. Assoc. 2020, 323, 2466–2467. [Google Scholar] [CrossRef] [PubMed]
- Peterson, U.; Demerouti, E.; Bergström, G.; Samuelsson, M.; Åsberg, M.; Nygren, Å. Burnout and physical and mental health among Swedish healthcare workers. J. Adv. Nurs. 2008, 62, 84–95. [Google Scholar] [CrossRef] [PubMed]
- González-Jiménez, A.J.; López-Martínez, M.J.; Zapata-Boluda, R.M.; Cala, V.; Dalouh, R. Investigación Educativa Y Salud Transcultural en Contextos Multiculturales; Editorial Universidad de Almería: Almería, España, 2016. [Google Scholar]
- Cañadas-De-La Fuente, G.A.; Ortega, E.; Ramirez-Baena, L.; De La Fuente-Solana, E.I.; Vargas, C.; Gómez-Urquiza, J.L. Gender, Marital Status, and Children as Risk Factors for Burnout in Nurses: A Meta-Analytic Study. Int. J. Environ. Res. Public Health 2018, 15, 2102. [Google Scholar] [CrossRef] [PubMed]

| Sociodemographic Variables | |||||
|---|---|---|---|---|---|
| Sex | Men (%) | Women (%) | |||
| 9.27% | 90.73% | ||||
| Age range | Between 27 and 63 years | Between 22 and 64 years | |||
| 51.1959 | 44.4835 | ||||
| Work center | Complejo Hospitalario Juan Ramón Jiménez (%) | Hospital Infanta Elena (%) | |||
| 62.94% | 37.06% | ||||
| Marital status | Married (%) | Single (%) | Divorced (%) | Widowed (%) | Companion (%) |
| 46.7% | 30.9% | 4.8% | 3% | 14.6% | |
| Parenthood | Yes (%) | No (%) | |||
| 64.1% | 35.9% | ||||
| Spearman’s Rho | Age | Emotional Exhaustion | Depersonalization | |
|---|---|---|---|---|
| Age | Correlation coefficient | 1.000 | 0.157 | 0.035 |
| Sig. (bilateral) | 0.000 ** | 0.266 | ||
| n | 313 | 313 | 313 | |
| Emotional exhaustion | Correlation coefficient | 0.157 | 1.000 | 0.363 |
| Sig. (bilateral) | 0.000 ** | 0.000 ** | ||
| n | 313 | 313 | 313 | |
| Depersonalization | Correlation coefficient | 0.035 | 0.363 | 1.000 |
| Sig. (bilateral) | 0.266 | 0.000 ** | ||
| n | 313 | 313 | 313 | |
| Possible Non-Psychotic Psychiatric Case | |||||
|---|---|---|---|---|---|
| Yes | No | Pearson’s Chi-Squared | Asymptotic Significance (Bilateral) | ||
| % | % | ||||
| Emotional exhaustion | High | 58.7% | 28.5% | 167.362 | 0.000 * |
| Medium | 33.0% | 28.7% | |||
| Low | 8.4% | 42.8% | |||
| Depersonalization | High | 37.2% | 25.0% | 30.645 | 0.000 * |
| Medium | 18.8% | 32.7% | |||
| Low | 44.1% | 42.3% | |||
| Personal realization | High | 31.5% | 19.5% | 21.725 | 0.000 * |
| Medium | 27.3% | 36.9% | |||
| Low | 41.1% | 43.6% | |||
| Possible Non-Psychotic Psychiatric Case (GHQ-12) | |||||
| Independent Variables | Yes (%) | No (%) | Pearson’s Chi-Squared | Asymptotic Significance (Bilateral) | |
| Sex | Men | 48.6% | 51.4% | 0.076 | 0.782 * |
| Women | 47.6% | 52.4% | |||
| Marital status | Married | 52.6% | 47.4% | 23.588 | 0.000 * |
| Single | 48.1% | 51.9% | |||
| Divorced | 39.2% | 60.8% | |||
| Widowed | 64.3% | 35.7% | |||
| With a partner | 32.0% | 68.0% | |||
| Parent status | Yes | 46.2% | 53.8% | 1.909 | 0.167 * |
| No | 50.7% | 49.3% | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gago-Valiente, F.-J.; Moreno-Sánchez, E.; Vélez-Moreno, E.; Merino-Godoy, M.-d.-l.-Á.; Sáez-Padilla, J.; de Paula Rodríguez-Miranda, F.; da Costa, E.I.M.T.; Saenz-de-la-Torre, L.-C.; Segura-Camacho, A.; Mendoza-Sierra, M.-I. The Upshot of the SARS-CoV-2 Pandemic on Nursing Assistants: Evaluating Mental Health Indicators in Huelva. J. Clin. Med. 2022, 11, 2586. https://doi.org/10.3390/jcm11092586
Gago-Valiente F-J, Moreno-Sánchez E, Vélez-Moreno E, Merino-Godoy M-d-l-Á, Sáez-Padilla J, de Paula Rodríguez-Miranda F, da Costa EIMT, Saenz-de-la-Torre L-C, Segura-Camacho A, Mendoza-Sierra M-I. The Upshot of the SARS-CoV-2 Pandemic on Nursing Assistants: Evaluating Mental Health Indicators in Huelva. Journal of Clinical Medicine. 2022; 11(9):2586. https://doi.org/10.3390/jcm11092586
Chicago/Turabian StyleGago-Valiente, Francisco-Javier, Emilia Moreno-Sánchez, Emilia Vélez-Moreno, María-de-los-Ángeles Merino-Godoy, Jesús Sáez-Padilla, Francisco de Paula Rodríguez-Miranda, Emília Isabel Martins Teixeira da Costa, Luis-Carlos Saenz-de-la-Torre, Adrián Segura-Camacho, and María-Isabel Mendoza-Sierra. 2022. "The Upshot of the SARS-CoV-2 Pandemic on Nursing Assistants: Evaluating Mental Health Indicators in Huelva" Journal of Clinical Medicine 11, no. 9: 2586. https://doi.org/10.3390/jcm11092586
APA StyleGago-Valiente, F.-J., Moreno-Sánchez, E., Vélez-Moreno, E., Merino-Godoy, M.-d.-l.-Á., Sáez-Padilla, J., de Paula Rodríguez-Miranda, F., da Costa, E. I. M. T., Saenz-de-la-Torre, L.-C., Segura-Camacho, A., & Mendoza-Sierra, M.-I. (2022). The Upshot of the SARS-CoV-2 Pandemic on Nursing Assistants: Evaluating Mental Health Indicators in Huelva. Journal of Clinical Medicine, 11(9), 2586. https://doi.org/10.3390/jcm11092586











