Association of Ramadan Participation with Psychological Parameters: A Cross-Sectional Study during the COVID-19 Pandemic in Iran
Abstract
:1. Introduction
2. Population and Methods
2.1. Participants
2.2. Measures
2.2.1. Demographic Information
2.2.2. Primary Outcomes and Measures: PA Behavior
2.2.3. Secondary Outcomes and Measures: Anxiety, Well-Being, and Sleep-Quality
2.3. Statistical Analysis
3. Results
3.1. Primary Outcomes: PA Behavior
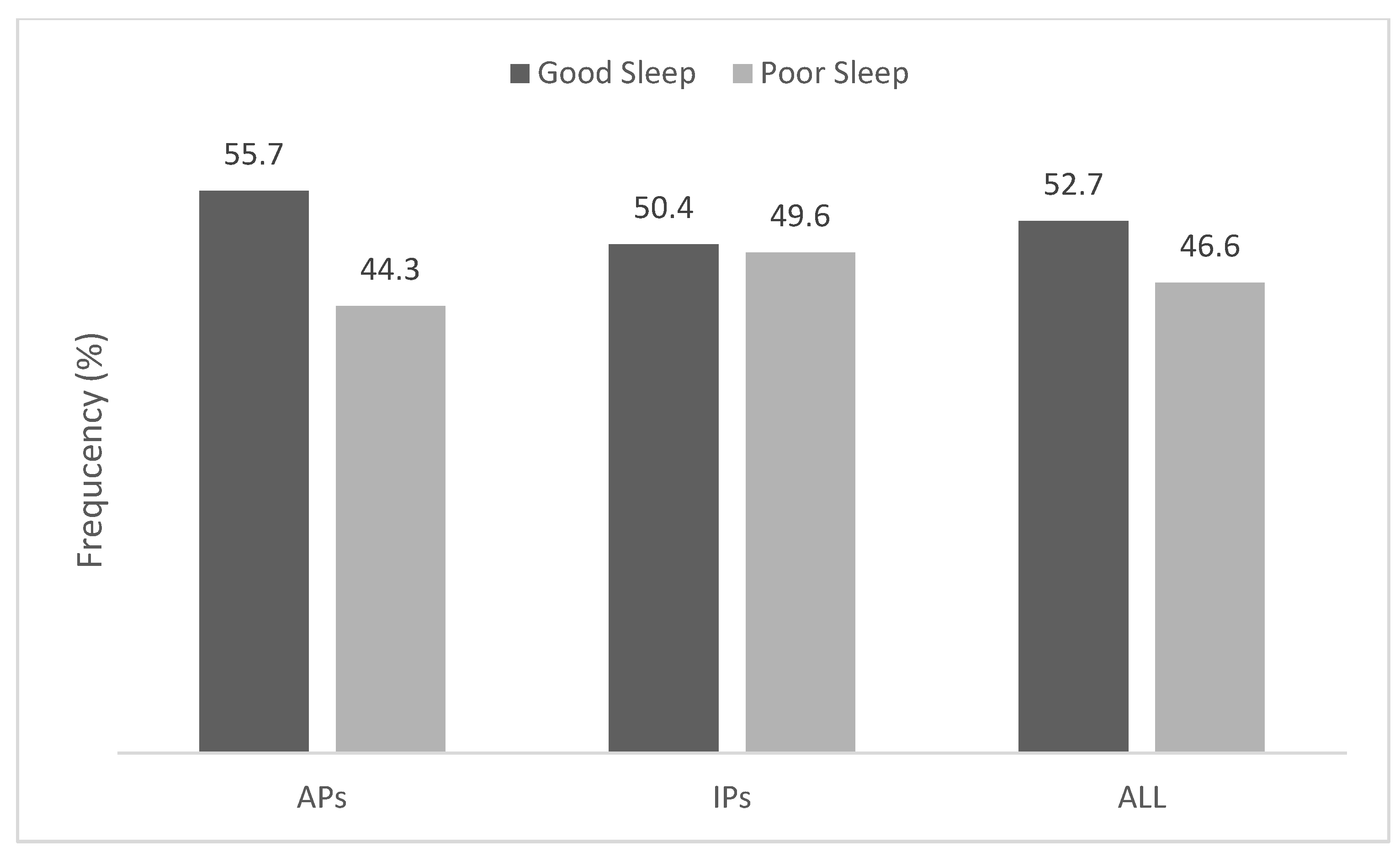
3.2. Secondary Outcomes:Anxiety, Well-Being, and Sleep-Quality
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Akbari, M.; Seydavi, M.; Zamani, E. The mediating role of personalized psychological flexibility in the association between distress intolerance and psychological distress: A national survey during the fourth waves of COVID-19 pandemic in Iran. Clin. Psychol. Psychother. 2021, 28, 1416–1426. [Google Scholar] [CrossRef]
- Heidari, M.; Jafari, H. Challenges of COVID-19 Vaccination in Iran: In the Fourth Wave of Pandemic Spread. Prehospital Disaster Med. 2021, 36, 659–660. [Google Scholar] [CrossRef]
- Akbari, H.; Pourabbas, M.; Yoosefi, M.; Briki, W.; Attaran, S.; Mansoor, H.; Teixeira, A. How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 7847–7857. [Google Scholar]
- Ghram, A.; Ben Saad, H.; Briki, W.; Jiménez-Pavón, D.; Mansoor, H.; Moalla, W.; Akbari, H.A.; Ghram, A.; Al-Mohannadi, A.S.; Arena, R.; et al. Ramadan Intermittent Fasting, Physical Activity, and COVID-19 Pandemic in Patients with Chronic Diseases. Am. J. Med. 2021, 134, 1189–1191. [Google Scholar] [CrossRef]
- Ghram, A.; Bragazzi, N.L.; Briki, W.; Jenab, Y.; Khaled, M.; Haddad, M.; Chamari, K. COVID-19 Pandemic and Physical Exercise: Lessons Learnt for Confined Communities. Front. Psychol. 2021, 12, 618585. [Google Scholar] [CrossRef]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad. Med. 2021, 133, 469–480. [Google Scholar] [CrossRef]
- Ghram, A.; Moalla, W.; Lavie, C.J. Vaccine and physical activity in the era of COVID-19 pandemic. Prog. Cardiovasc. Dis. 2021, 67, 33–34. [Google Scholar] [CrossRef]
- Haddad, M.; Abbes, Z.; Ghram, A.; Cosma, G.; Chamari, K. Chapter 13—Physical activity as a counteracting measure to mitigate the harmful effects of COVID-19 lockdowns: Special focus on healthy children, adolescents, adults, elderly, athletes, and people with Down syndrome. In Mental Health Effects of COVID-19; Moustafa, A.A., Ed.; Academic Press: Cambridge, MA, USA, 2021; pp. 215–234. [Google Scholar]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021, 64, 108–110. [Google Scholar] [CrossRef]
- Jiménez-Pavón, D.; Carbonell-Baeza, A.; Lavie, C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog. Cardiovasc. Dis. 2020, 63, 386–388. [Google Scholar] [CrossRef]
- Laddu, D.R.; Lavie, C.J.; Phillips, S.A.; Arena, R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Prog. Cardiovasc. Dis. 2020, 64, 102–104. [Google Scholar] [CrossRef]
- Morin, C.M.; Carrier, J.; Bastien, C.; Godbout, R. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can. J. Public Health 2020, 111, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.K.; Ramadan, H.K.-A.; Refay, S.M.; Khashbah, M.A. Comparison of knowledge, attitude, socioeconomic burden, and mental health disorders of COVID-19 pandemic between general population and health care workers in Egypt. Egypt. J. Neurol. Psychiatry Neurosurg. 2021, 57, 25. [Google Scholar] [CrossRef]
- Guo, Y.; Cheng, C.; Zeng, Y.; Li, Y.; Zhu, M.; Yang, W.; Xu, H.; Li, X.; Leng, J.; Monroe-Wise, A.; et al. Mental Health Disorders and Associated Risk Factors in Quarantined Adults During the COVID-19 Outbreak in China: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e20328. [Google Scholar] [CrossRef] [PubMed]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 109, 110207. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Lessan, N.; Ali, T. Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients 2019, 11, 1192. [Google Scholar] [CrossRef] [Green Version]
- Zijoud, S.R.H.; Farahani, A.J. Ramadan Coincides with the COVID-19 Pandemic: What Should Be Done? Disaster Med. Public Health Prep. 2020, 14, e7–e8. [Google Scholar] [CrossRef] [Green Version]
- Leiper, J.B.; Molla, A.M.; Molla, A.M. Effects on health of fluid restriction during fasting in Ramadan. Eur. J. Clin. Nutr. 2003, 57, S30–S38. [Google Scholar] [CrossRef] [Green Version]
- Akbari, H.A.; Ghram, A.; Yoosef, M.; Arena, R.; Lavie, C.J.; Chtourou, H.; Ben Saad, H.; Chamari, K. The COVID-19 pandemic and physical activity during intermittent fasting, is it safe? A call for action. Biol. Sport 2021, 38, 729–732. [Google Scholar] [CrossRef]
- Salim, I.; Al Suwaidi, J.; Ghadban, W.; Alkilani, H.; Salam, A.M. Impact of religious Ramadan fasting on cardiovascular disease: A systematic review of the literature. Curr. Med. Res. Opin. 2013, 29, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Almeneessier, A.S.; BaHammam, A.S. How does diurnal intermittent fasting impact sleep, daytime sleepiness, and markers of the biological clock? Current insights. Nat. Sci. Sleep 2018, 10, 439–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charan, J.; Biswas, T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farmanbar, R.; Niknami, S.; Lubans, D.; Hidarnia, A. Predicting exercise behaviour in Iranian college students: Utility of an integrated model of health behaviour based on the transtheoretical model and self-determination theory. Health Educ. J. 2013, 72, 56–69. [Google Scholar] [CrossRef]
- Amireault, S.; Godin, G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire: Validity Evidence Supporting its Use for Classifying Healthy Adults into Active and Insufficiently Active Categories. Percept. Mot. Ski. 2015, 120, 604–622. [Google Scholar] [CrossRef] [PubMed]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Warburton, D.E.; Charlesworth, S.; Ivey, A.; Nettlefold, L.; Bredin, S.S. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 39. [Google Scholar] [CrossRef] [Green Version]
- Omani-Samani, R.; Maroufizadeh, S.; Ghaheri, A.; Navid, B. Generalized Anxiety Disorder-7 (GAD-7) in people with infertility: A reliability and validity study. Middle East Fertil. Soc. J. 2018, 23, 446–449. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Rafiey, H.; Alipour, F.; Lebeau, R.; Rarani, M.A.; Salimi, Y.; Ahmadi, S. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF) in Iranian earthquake survivors. Int. J. Ment. Health 2017, 46, 243–251. [Google Scholar] [CrossRef]
- Keyes, C.L.M. Mental Illness and/or Mental Health? Investigating Axioms of the Complete State Model of Health. J. Consult. Clin. Psychol. 2005, 73, 539–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chehri, A.; Nourozi, M.; Eskandari, S.; Khazaie, H.; Hemati, N.; Jalali, A. Validation of the Persian version of the Pittsburgh Sleep Quality Index in elderly population. Sleep Sci. 2020, 13, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br. J. Sports Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef]
- Schoofs, M.C.A.; Bakker, E.A.; de Vries, F.; Hartman, Y.A.W.; Spoelder, M.; Thijssen, D.H.J.; Eijsvogels, T.M.H.; Buffart, L.M.; Hopman, M.T.E. Impact of Dutch COVID-19 restrictive policy measures on physical activity behavior and identification of correlates of physical activity changes: A cohort study. BMC Public Health 2022, 22, 147. [Google Scholar] [CrossRef]
- Cheval, B.; Sivaramakrishnan, H.; Maltagliati, S.; Fessler, L.; Forestier, C.; Sarrazin, P.; Orsholits, D.; Chalabaev, A.; Sander, D.; Ntoumanis, N.; et al. Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland. J. Sports Sci. 2021, 39, 699–704. [Google Scholar] [CrossRef]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [Green Version]
- Alghamdi, A.S.; Alghamdi, K.A.; Jenkins, R.O.; Alghamdi, M.N.; Haris, P.I. Impact of Ramadan on Physical Activity and Sleeping Patterns in Individuals with Type 2 Diabetes: The First Study Using Fitbit Device. Diabetes Ther. 2020, 11, 1331–1346. [Google Scholar] [CrossRef]
- Wolf, S.; Seiffer, B.; Zeibig, J.-M.; Welkerling, J.; Brokmeier, L.; Atrott, B.; Ehring, T.; Schuch, F.B. Is Physical Activity Associated with Less Depression and Anxiety During the COVID-19 Pandemic? A Rapid Systematic Review. Sports Med. 2021, 51, 1771–1783. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Farooq, A.; Chamari, K.; Sayegh, S.; El Akoum, M.; Al-Mohannadi, A.S. Ramadan daily intermittent fasting reduces objectively assessed habitual physical activity among adults. BMC Public Health 2021, 21, 1912. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Valabhji, J. Obesity as a Risk Factor for Severe COVID-19: Summary of the Best Evidence and Implications for Health Care. Curr. Obes. Rep. 2021, 10, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Sanchis-Gomar, F.; Arena, R. Fit Is It in COVID-19, Future Pandemics, and Overall Healthy Living. Mayo Clin. Proc. 2021, 96, 7–9. [Google Scholar] [CrossRef]
- Bayani, A.A.; Esmaeili, R.; Ganji, G. The Impact of Fasting on the Psychological Well-Being of Muslim Graduate Students. J. Relig. Health 2020, 59, 3270–3275. [Google Scholar] [CrossRef]
- Albrecht, J.N.; Werner, H.; Rieger, N.; Widmer, N.; Janisch, D.; Huber, R.; Jenni, O.G. Association Between Homeschooling and Adolescent Sleep Duration and Health During COVID-19 Pandemic High School Closures. JAMA Netw. Open 2022, 5, e2142100. [Google Scholar] [CrossRef]
- Trabelsi, K.; Ammar, A.; Zlitni, S.; Boukhris, O.; Khacharem, A.; El-Abed, K.; Khanfir, S.; Shephard, R.J.; Stannard, S.R.; Bragazzi, N.L.; et al. Practical recommendations to improve sleep during Ramadan observance in healthy practitioners of physical activity. Tunis. Med. 2019, 97, 1077–1086. [Google Scholar]
- Bahammam, A. Does Ramadan fasting affect sleep? Int. J. Clin. Pract. 2006, 60, 1631–1637. [Google Scholar] [CrossRef]
- Bahammam, A. Effect of fasting during Ramadan on sleep architecture, daytime sleepiness and sleep pattern. Sleep Biol. Rhythm. 2004, 2, 135–143. [Google Scholar] [CrossRef]
- Lipert, A.; Kozłowski, R.; Rasmus, P.; Marczak, M.; Timler, M.; Timler, D.; Kaniecka, E.; Nasser, A.; Ghaddar, M.; Ghaddar, A. Sleep Quality and Performance in Professional Athletes Fasting during the Month of Ramadan. Int. J. Environ. Res. Public Health 2021, 18, 6890. [Google Scholar] [CrossRef] [PubMed]
- Faris, M.A.-I.E.; Jahrami, H.A.; AlHayki, F.A.; Alkhawaja, N.A.; Ali, A.M.; Aljeeb, S.H.; Abdulghani, I.H.; Bahammam, A.S. Effect of diurnal fasting on sleep during Ramadan: A systematic review and meta-analysis. Sleep Breath. 2020, 24, 771–782. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, K.; Ammar, A.; Glenn, J.M.; Boukhris, O.; Khacharem, A.; Bouaziz, B.; Zmijewski, P.; Lanteri, P.; Garbarino, S.; Clark, C.C.T.; et al. Does observance of Ramadan affect sleep in athletes and physically active individuals? A systematic review and meta-analysis. J. Sleep Res. 2021, e13503. [Google Scholar] [CrossRef] [PubMed]
- Roky, R.; Chapotot, F.; Hakkou, F.; Benchekroun, M.T.; Buguet, A. Sleep during Ramadan intermittent fasting. J. Sleep Res. 2001, 10, 319–327. [Google Scholar] [CrossRef]
- Faris, M.A.-I.E.; Jahrami, H.A.; Alsibai, J.; Obaideen, A.A. Impact of Ramadan diurnal intermittent fasting on the metabolic syndrome components in healthy, non-athletic Muslim people aged over 15 years: A systematic review and meta-analysis. Br. J. Nutr. 2020, 123, 1–22. [Google Scholar] [CrossRef]
- Tinsley, G.; Forsse, J.S.; Butler, N.K.; Paoli, A.; Bane, A.A.; La Bounty, P.M.; Morgan, G.B.; Grandjean, P.W. Time-restricted feeding in young men performing resistance training: A randomized controlled trial. Eur. J. Sport Sci. 2017, 17, 200–207. [Google Scholar] [CrossRef]
- Kalam, F.; Gabel, K.; Cienfuegos, S.; Wiseman, E.; Ezpeleta, M.; Steward, M.; Pavlou, V.; Varady, K.A. Alternate day fasting combined with a low-carbohydrate diet for weight loss, weight maintenance, and metabolic disease risk reduction. Obes. Sci. Pract. 2019, 5, 531–539. [Google Scholar] [CrossRef]
- Davis, C.S.; Clarke, R.E.; Coulter, S.N.; Rounsefell, K.N.; Walker, R.E.; Rauch, C.E.; Ryan, L. Intermittent energy restriction and weight loss: A systematic review. Eur. J. Clin. Nutr. 2015, 70, 292–299. [Google Scholar] [CrossRef]
- Berthelot, E.; Etchecopar-Etchart, D.; Thellier, D.; Lancon, C.; Boyer, L.; Fond, G. Fasting Interventions for Stress, Anxiety and Depressive Symptoms: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3947. [Google Scholar] [CrossRef]
- Raveendran, A.V.; Jayadevan, R.; Sashidharan, S. Long COVID: An overview. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 869–875. [Google Scholar] [CrossRef]
- Lauwers, M.; Au, M.; Yuan, S.; Wen, C. COVID-19 in Joint Ageing and Osteoarthritis: Current Status and Perspectives. Int. J. Mol. Sci. 2022, 23, 720. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Ghram, A.; Ayadi, H.; Knechtle, B.; Ben Saad, H. What should a family physician know about nutrition and physical exercise rehabilitation’ advices to communicate to “long-term COVID-19” patients? Postgrad. Med. 2022, 134, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Blumberg, S.J.; Brick, J.M.; Couper, M.P.; Courtright, M.; Garland, P. Prepared for the AAPOR Executive Council by a Task Force operating under the auspices of the AAPOR Standards Committee, with members including. Research synthesis: AAPOR report on online panels. Public Opin. Q. 2010, 74, 711–781. [Google Scholar]
| Characteristics | Men N (%) | Women N (%) | Total N (%) | p-Value | |
|---|---|---|---|---|---|
| 179 (35.1) | 331 (64.9) | 510 (100) | |||
| Age | (years) | 31 ± 13 | 30 ± 12 | 31 ± 12 | 0.25 |
| Height | (cm) | 176 ± 7 | 163 ± 6 | 168 ± 9 | <0.001 |
| Weight | (kg) | 79 ± 14 | 63 ± 13 | 69 ± 15 | <0.001 |
| Marital status | Single | 111 (62.0) | 205 (61.9) | 316 (62.0) | 0.99 |
| Married | 68 (38.0) | 126 (38.1) | 194 (38.0) | ||
| Schooling-level | High school | 5 (2.8) | 18 (5.4) | 23 (4.5) | 0.42 |
| Diploma | 48 (26.8) | 70 (21.1) | 118 (23.1) | ||
| Associate | 16 (8.9) | 26 (7.9) | 42 (8.2) | ||
| Bachelor | 63 (35.2) | 126 (38.1) | 189 (37.1) | ||
| Master | 37 (20.7) | 64 (19.3) | 101 (19.8) | ||
| Doctoral | 10 (5.6) | 27 (8.2) | 37 (7.3) | ||
| Employment status (pre-Ramadan) | Full-time | 79 (44.1) | 63 (19.0) | 142 (27.8) | <0.001 |
| Part-time | 34 (19.0) | 64 (19.3) | 98 (19.2) | ||
| Unemployed | 55 (30.7) | 124 (37.5) | 179 (35.1) | ||
| Homemaker | 0 (0.0) | 64 (19.3) | 64 (12.5) | ||
| Retired | 11 (6.1) | 15 (4.5) | 26 (5.1) | ||
| Unable to work | 0 (0.0) | 1 (0.3) | 1 (0.2) | ||
| Employment status (in Ramadan) | No change | 141 (78.8) | 267 (80.7) | 408 (80.0) | 0.067 |
| Decreased hours | 19 (10.6) | 30 (9.1) | 49 (9.6) | ||
| Remote work | 3 (1.7) | 19 (5.7) | 22 (4.3) | ||
| Laid off | 4 (2.2) | 6 (1.8) | 10 (2.0) | ||
| Employed | 3 (1.7) | 4 (1.2) | 7 (1.4) | ||
| Increased hours | 9 (5.0) | 5 (1.5) | 14 (2.7) | ||
| Environment | Urban | 157 (87.7) | 309 (93.4) | 466 (91.4) | 0.091 |
| Suburban | 8 (4.5) | 9 (2.7) | 17 (3.3) | ||
| Rural | 14 (7.8) | 13 (3.9) | 27 (5.3) | ||
| Location | Central | 73 (40.8) | 116 (35.0) | 189 (37.1) | 0.35 |
| Northern | 29 (16.2) | 55 (16.6) | 84 (16.5) | ||
| Southern | 19 (10.6) | 29 (8.8) | 48 (9.4) | ||
| Eastern | 28 (15.6) | 51 (15.4) | 79 (15.5) | ||
| Western | 30 (16.8) | 80 (24.2) | 110 (21.6) | ||
| Fasting status | Full | 91 (50.8) | 115 (34.7) | 206 (40.4) | <0.001 |
| Not at all | 58 (32.4) | 114 (34.4) | 172 (33.7) | ||
| Partial | 30 (16.8) | 102 (30.8) | 132 (25.9) | ||
| Reason for not fasting | Fear of COVID-19 | 5 (2.8) | 14 (4.2) | 19 (3.7) | <0.001 |
| Diabetes | 4 (2.2) | 5 (1.5) | 9 (1.8) | ||
| CVD | 1 (0.6) | 4 (1.2) | 5 (1.0) | ||
| Kidney disease | 5 (2.8) | 7 (2.1) | 12 (2.4) | ||
| Mental disease | 0 (0.0) | 10 (3.0) | 10 (2.0) | ||
| Other diseases | 10 (5.6) | 59 (17.8) | 69 (13.5) | ||
| Personal reasons | 61 (34.1) | 119 (36.0) | 180 (35.3) | ||
| Religion | Shia | 153 (85.5) | 304 (91.8) | 457 (89.6) | 0.011 |
| Sunni | 14 (7.8) | 21 (6.3) | 35 (6.9) | ||
| Zoroastrianism | 0 (0.0) | 1 (0.3) | 1 (0.2) | ||
| Other | 1 (0.6) | 2 (0.6) | 3 (0.6) | ||
| Irreligion | 11 (6.1) | 3 (0.9) | 14 (2.7) | ||
| Ethnicity | Azari | 31 (17.3) | 53 (16.0) | 84 (16.5) | 0.2 |
| Kurdish | 18 (10.1) | 37 (11.2) | 55 (10.8) | ||
| Turkmen | 0 (0.0) | 2 (0.6) | 2 (0.4) | ||
| Lor | 11 (6.1) | 24 (7.3) | 35 (6.9) | ||
| Arab | 4 (2.2) | 0 (0.0) | 4 (0.8) | ||
| Baloch | 2 (1.1) | 3 (0.9) | 5 (1.0) | ||
| Fars | 100 (55.9) | 194 (58.6) | 294 (57.6) | ||
| Others | 13 (7.3) | 18 (5.4) | 31 (6.1) | ||
| Vaccination status | Yes | 3 (1.7) | 15 (4.5) | 18 (3.5) | 0.095 |
| No | 176 (98.3) | 316 (95.5) | 492 (96.5) | ||
| COVID-19 experience | Pre-Ramadan | 57 (31.8) | 100 (30.2) | 157 (30.8) | 0.53 |
| In Ramadan | 5 (2.8) | 16 (4.8) | 21 (4.1) | ||
| Never | 117 (65.4) | 215 (65.0) | 332 (65.1) | ||
| Characteristics | IPs N (%) | APs N (%) | Total N (%) | p-Value | |
|---|---|---|---|---|---|
| 282 (55.3) | 228 (44.7) | 510 (100) | |||
| Godin Leisure Score | (absolute value) | 7 ± 8 | 127 ± 369 | 61 ± 254 | <0.001 |
| Strenuous PA | (min/wk) | 3 ± 14 | 65 ± 223 | 31 ± 152 | <0.001 |
| Moderate PA | (min/wk) | 8 ± 24 | 71 ± 142 | 36 ± 101 | <0.001 |
| Mild/light PA | (min/wk) | 25 ± 170 | 59 ± 109 | 40 ± 147 | 0.007 |
| Changes in PA duration | Less | 76 (27.0) | 96 (42.1) | 172 (33.7) | <0.001 |
| About the same | 66 (23.4) | 96 (42.1) | 162 (31.8) | ||
| More | 7 (2.5) | 18 (7.9) | 25 (4.9) | ||
| Common PA type | Weight training | 4 (1.4) | 13 (5.7) | 17 (3.3) | <0.001 |
| Biking/cycling | 5 (1.8) | 21 (9.2) | 26 (5.1) | ||
| Walking | 88 (31.2) | 114 (50.0) | 202 (39.6) | ||
| Running | 2 (0.7) | 14 (6.1) | 16 (3.1) | ||
| Martial arts | 1 (0.4) | 3 (1.3) | 4 (0.8) | ||
| Online training | 8 (2.8) | 9 (3.9) | 17 (3.3) | ||
| Others | 25 (8.9) | 34 (14.9) | 59 (11.6) | ||
| Changes in PA type | Very similar | 74 (26.2) | 118 (51.8) | 192 (37.6) | <0.001 |
| Somewhat similar | 33 (11.7) | 66 (28.9) | 99 (19.4) | ||
| Not so similar | 29 (10.3) | 24 (10.5) | 53 (10.4) | ||
| Common PA location | Outdoors | 79 (28.0) | 127 (55.7) | 206 (40.4) | <0.001 |
| Indoors | 3 (1.1) | 15 (6.6) | 18 (3.5) | ||
| In the house | 52 (18.4) | 65 (28.5) | 117 (22.9) | ||
| Changes in PA location | Yes | 37 (13.1) | 55 (24.1) | 92 (18.0) | <0.001 |
| No | 100 (35.5) | 154 (67.5) | 254 (49.8) | ||
| Factors | IPs N (%) 282 (55.3) | APs N (%) 228 (44.7) | Total N (%) 510 (100) | p-Value |
|---|---|---|---|---|
| Emotional well-being | 11.24 ± 3.91 | 12.11 ± 3.90 | 11.63 ± 3.93 | 0.014 |
| Psychological well-being | 18.11 ± 7.13 | 20.25 ± 6.50 | 19.07 ± 6.93 | <0.001 |
| Social well-being | 18.05 ± 6.78 | 20.48 ± 6.43 | 19.14 ± 6.73 | <0.001 |
| Overall well-being | 47.40 ± 16.22 | 52.84 ± 15.04 | 49.84 ± 15.92 | <0.001 |
| General Anxiety Disorder-7 | 5.77 ± 4.58 | 5.72 ± 4.63 | 5.75 ± 4.60 | 0.90 |
| Pittsburgh Sleep-quality Index | 6.00 ± 3.26 | 5.45 ± 2.87 | 5.75 ± 3.10 | 0.046 |
| IPs (N = 282) | APs (N = 228) | |||||||
|---|---|---|---|---|---|---|---|---|
| Factors | Full-Fast (N = 116) | Partial-Fast (N = 78) | No-Fast (N = 88) | p-Value | Full-Fast (N = 90) | Partial-Fast (N = 54) | No-Fast (N = 84) | p-Value |
| Emotional well-being | 11.98 ± 3.61 # | 11.24 ± 4.03 | 10.27 ± 4.02 | 0.008 | 12.90 ± 3.69 # | 12.09 ± 3.31 | 11.26 ± 4.32 | 0.021 |
| Psychological well-being | 19.84 ± 7.10 # | 17.58 ± 7.14 | 16.31 ± 6.71 | 0.001 | 21.67 ± 6.43 # | 19.54 ± 5.26 | 19.20 ± 7.07 | 0.028 |
| Social well-being | 18.94 ± 6.33 | 17.50 ± 6.95 | 17.36 ± 7.14 | 0.18 | 21.86 ± 6.18 | 19.22 ± 5.69 | 19.82 ± 6.91 | 0.028 |
| Overall well-being | 50.76 ± 15.50 # | 46.32 ± 16.95 | 43.94 ± 15.79 | 0.009 | 56.42 ± 14.32 # | 50.85 ± 12.83 | 50.29 ± 16.46 | 0.014 |
| General Anxiety Disorder-7 | 4.76 ± 4.34 # | 5.94 ± 4.26 | 6.97 ± 4.90 | 0.003 | 4.41 ± 4.08 # | 5.70 ± 3.76 | 7.13 ± 5.27 | <0.001 |
| Pittsburgh Sleep-quality Index | 5.94 ± 3.35 | 6.32 ± 3.34 | 5.80 ± 3.08 | 0.57 | 4.81 ± 2.64 * | 6.33 ± 2.79 | 5.55 ± 3.02 | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akbari, H.A.; Yoosefi, M.; Pourabbas, M.; Weiss, K.; Knechtle, B.; Vancini, R.L.; Trakada, G.; Ben Saad, H.; Lavie, C.J.; Ghram, A. Association of Ramadan Participation with Psychological Parameters: A Cross-Sectional Study during the COVID-19 Pandemic in Iran. J. Clin. Med. 2022, 11, 2346. https://doi.org/10.3390/jcm11092346
Akbari HA, Yoosefi M, Pourabbas M, Weiss K, Knechtle B, Vancini RL, Trakada G, Ben Saad H, Lavie CJ, Ghram A. Association of Ramadan Participation with Psychological Parameters: A Cross-Sectional Study during the COVID-19 Pandemic in Iran. Journal of Clinical Medicine. 2022; 11(9):2346. https://doi.org/10.3390/jcm11092346
Chicago/Turabian StyleAkbari, Hesam Addin, Mohammad Yoosefi, Maryam Pourabbas, Katja Weiss, Beat Knechtle, Rodrigo Luiz Vancini, Georgia Trakada, Helmi Ben Saad, Carl J. Lavie, and Amine Ghram. 2022. "Association of Ramadan Participation with Psychological Parameters: A Cross-Sectional Study during the COVID-19 Pandemic in Iran" Journal of Clinical Medicine 11, no. 9: 2346. https://doi.org/10.3390/jcm11092346
APA StyleAkbari, H. A., Yoosefi, M., Pourabbas, M., Weiss, K., Knechtle, B., Vancini, R. L., Trakada, G., Ben Saad, H., Lavie, C. J., & Ghram, A. (2022). Association of Ramadan Participation with Psychological Parameters: A Cross-Sectional Study during the COVID-19 Pandemic in Iran. Journal of Clinical Medicine, 11(9), 2346. https://doi.org/10.3390/jcm11092346







