Myocardial Function during Ventilation with Lower versus Higher Positive End-Expiratory Pressure in Patients without ARDS
Abstract
:1. Introduction
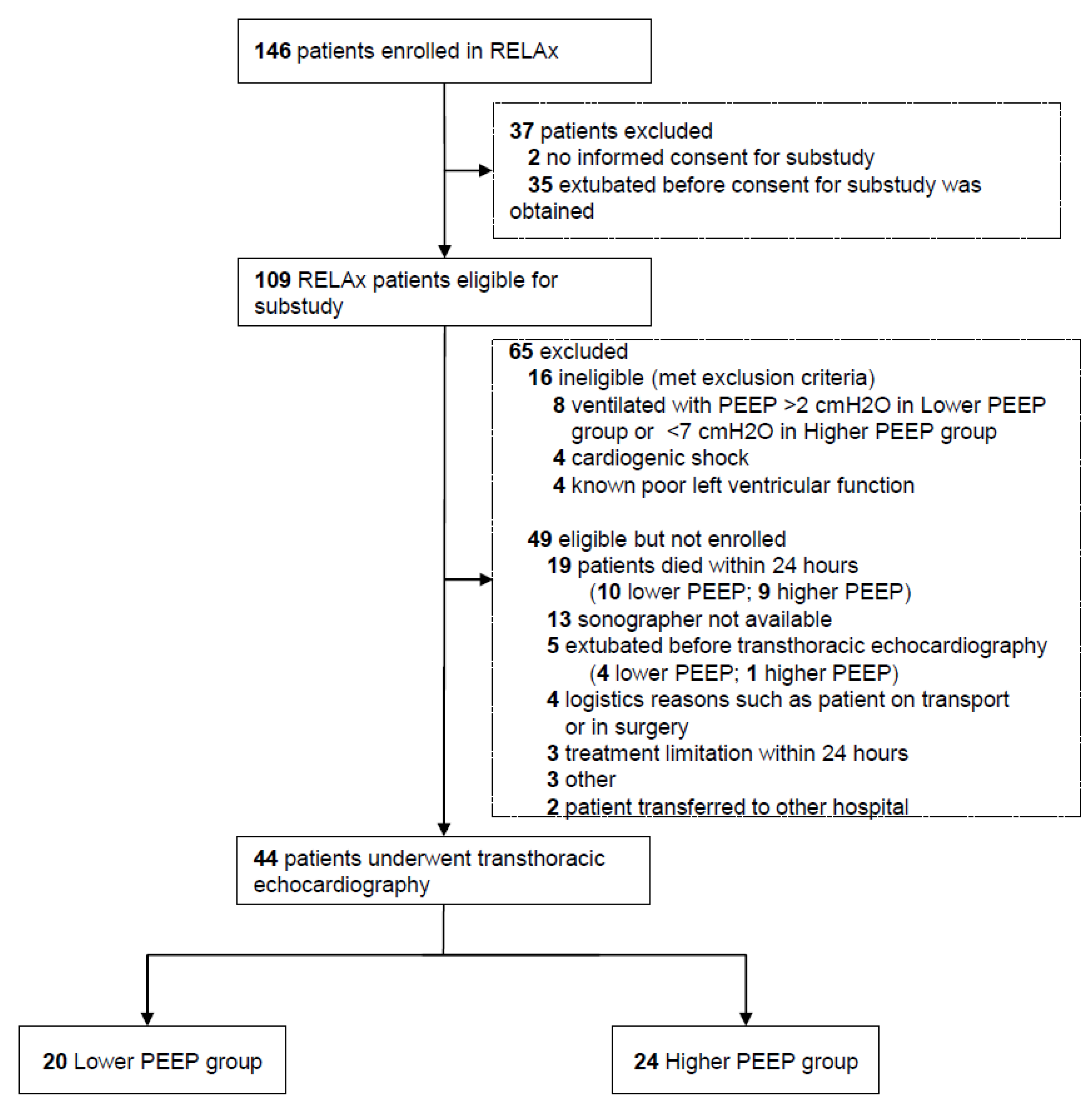
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Protocol
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Respiratory and Hemodynamic Parameters
3.3. Echocardiographic Evaluation
3.4. Right and Left Ventricular Systolic and Diastolic Function
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fraser, J.F.; Vm, R. Ventilator-Induced Lung Injury. N. Engl. J. Med. 2014, 370, 979–980. [Google Scholar] [CrossRef] [Green Version]
- Neto, A.S.; Simonis, F.D.; Barbas, C.S.V.; Biehl, M.; Determann, R.M.; Elmer, J.; Friedman, G.; Gajic, O.; Goldstein, J.N.; Linko, R.; et al. Lung-Protective Ventilation with Low Tidal Volumes and the Occurrence of Pulmonary Complications in Patients Without Acute Respiratory Distress Syndrome: A Systematic Review and Individual Patient Data Analysis. Crit. Care Med. 2015, 43, 2155–2163. [Google Scholar] [CrossRef] [PubMed]
- Neto, A.S.; Filho, R.R.; Cherpanath, T.; Determann, R.; Dongelmans, D.A.; Paulus, F.; Tuinman, P.R.; Pelosi, P.; De Abreu, M.G.; For the PROVE Network Investigators; et al. Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: A systematic review and meta-analysis of randomized controlled trials. Ann. Intensiv. Care 2016, 6, 109. [Google Scholar] [CrossRef] [Green Version]
- Peñuelas, O.; Muriel, A.; Abraira, V.; Frutos-Vivar, F.; Mancebo, J.; Raymondos, K.; Du, B.; Thille, A.W.; Ríos, F.; González, M.; et al. Inter-country variability over time in the mortality of mechanically ventilated patients. Intensiv. Care Med. 2020, 46, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Writing Committee and Steering Committee for the RELAx Collaborative Group; Algera, A.G.; Pisani, L.; Neto, A.S.; Boer, S.S.D.; Bosch, F.F.H.; Bruin, K.; Klooster, P.M.; Van Der Meer, N.J.M.; Nowitzky, R.O.; et al. Effect of a Lower vs Higher Positive End-Expiratory Pressure Strategy on Ventilator-Free Days in ICU Patients Without ARDS: A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2020, 324, 2509. [Google Scholar] [CrossRef]
- Luecke, T.; Pelosi, P. Clinical review: Positive end-expiratory pressure and cardiac output. Crit. Care 2005, 9, 607–621. [Google Scholar] [CrossRef] [Green Version]
- Pinsky, M.R. The hemodynamic consequences of mechanical ventilation: An evolving story. Intensiv. Care Med. 1997, 23, 493–503. [Google Scholar] [CrossRef]
- Pinsky, M.R.; Desmet, J.-M.; Vincent, J.-L. Effect of Positive End-expiratory Pressure on Right Ventricular Function in Humans. Am. Rev. Respir. Dis. 1992, 146, 681–687. [Google Scholar] [CrossRef]
- Franchi, F.; Faltoni, A.; Cameli, M.; Muzzi, L.; Lisi, M.; Cubattoli, L.; Cecchini, S.; Mondillo, S.; Biagioli, B.; Taccone, F.S.; et al. Influence of Positive End-Expiratory Pressure on Myocardial Strain Assessed by Speckle Tracking Echocardiography in Mechanically Ventilated Patients. BioMed Res. Int. 2013, 2013, 918548. [Google Scholar] [CrossRef]
- Van den Berg, P.C.; Jansen, J.R.C.; Pinsky, M.R. Effect of positive pressure on venous return in volume-loaded cardiac surgical patients. J. Appl. Physiol. 2002, 92, 1223–1231. [Google Scholar] [CrossRef] [Green Version]
- Schulman, D.S.; Biondi, J.W.; Matthay, R.A.; Zaret, B.L.; Soufer, R. Differing responses in right and left ventricular filling, loading and volumes during positive end-expiratory pressure. Am. J. Cardiol. 1989, 64, 772–777. [Google Scholar] [CrossRef]
- McCaul, C.; Kornecki, A.; Engelberts, D.; McNamara, P.; Kavanagh, B.P. Positive End-Expiratory Pressure Improves Survival in a Rodent Model of Cardiopulmonary Resuscitation Using High-Dose Epinephrine. Anesth. Analg. 2009, 109, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- Herff, H.; Paal, P.; von Goedecke, A.; Lindner, K.H.; Severing, A.C.; Wenzel, V. Influence of ventilation strategies on survival in severe controlled hemorrhagic shock. Crit. Care Med. 2008, 36, 2613–2620. [Google Scholar] [CrossRef] [PubMed]
- Krismer, A.C.; Wenzel, V.; Lindner, K.H.; Haslinger, C.W.; Oroszy, S.; Stadlbauer, K.H.; Königsrainer, A.; Boville, B.; Hörmann, C. Influence of Positive End-Expiratory Pressure Ventilation on Survival During Severe Hemorrhagic Shock. Ann. Emerg. Med. 2005, 46, 337–342. [Google Scholar] [CrossRef]
- Algera, A.G.; Pisani, L.; Chaves, R.C.D.F.; Amorim, T.C.; Cherpanath, T.; Determann, R.; Dongelmans, D.A.; Paulus, F.; Tuinman, P.R.; For the PROVE Network Investigators; et al. Effects of peep on lung injury, pulmonary function, systemic circulation and mortality in animals with uninjured lungs—A systematic review. Ann. Transl. Med. 2018, 6, 25. [Google Scholar] [CrossRef]
- Algera, A.G.; Pisani, L.; Bergmans, D.C.J.; Boer, S.D.; De Borgie, C.A.J.; Bosch, F.H.; Bruin, K.; Cherpanath, T.G.; Determann, R.M.; For the RELAx Investigators and the PROVE Network Investigators; et al. RELAx—REstricted versus Liberal positive end-expiratory pressure in patients without ARDS: Protocol for a randomized controlled trial. Trials 2018, 19, 272. [Google Scholar] [CrossRef] [Green Version]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Cherpanath, T.G.V.; Simonis, F.D.; Bouma, B.; de Bruin-Bon, R.H.; Determann, R.M.; Juffermans, N.P.; de Abreu, M.G.; Pelosi, P.; Neto, A.S.; Groeneveld, J.A.B.; et al. Myocardial Function during Low versus Intermediate Tidal Volume Ventilation in Patients without Acute Respiratory Distress Syndrome. Anesthesiology 2020, 132, 1102–1113. [Google Scholar] [CrossRef]
- Schmitt, J.-M.; Vieillard-Baron, A.; Augarde, R.; Prin, S.; Page, B.; Jardin, F. Positive end-expiratory pressure titration in acute respiratory distress syndrome patients: Impact on right ventricular outflow impedance evaluated by pulmonary artery Doppler flow velocity measurements. Crit. Care Med. 2001, 29, 1154–1158. [Google Scholar] [CrossRef]
- Dessap, A.M.; Charron, C.; Devaquet, J.; Aboab, J.; Jardin, F.; Brochard, L.; Vieillard-Baron, A. Impact of acute hypercapnia and augmented positive end-expiratory pressure on right ventricle function in severe acute respiratory distress syndrome. Intensiv. Care Med. 2009, 35, 1850–1858. [Google Scholar] [CrossRef]
- Fougères, E.; Teboul, J.-L.; Richard, C.; Osman, D.; Chemla, D.; Monnet, X. Hemodynamic impact of a positive end-expiratory pressure setting in acute respiratory distress syndrome: Importance of the volume status*. Crit. Care Med. 2010, 38, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Dessap, A.M.; Boissier, F.; Charron, C.; Bégot, E.; Repessé, X.; Legras, A.; Brun-Buisson, C.; Vignon, P.; Vieillard-Baron, A. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: Prevalence, predictors, and clinical impact. Intensiv. Care Med. 2015, 42, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Tei, C.; Dujardin, K.S.; Hodge, D.O.; Bailey, K.R.; McGoon, M.D.; Tajik, A.; Seward, J.B. Doppler echocardiographic index for assessment of global right ventricular function. J. Am. Soc. Echocardiogr. 1996, 9, 838–847. [Google Scholar] [CrossRef]
- Esteban, A.; Frutos-Vivar, F.; Muriel, A.; Ferguson, N.; Peñuelas, O.; Abraira, V.; Raymondos, K.; Rios, F.; Nin, N.; Apezteguía, C.; et al. Evolution of Mortality over Time in Patients Receiving Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2013, 188, 220–230. [Google Scholar] [CrossRef]
- Briel, M.; Meade, M.; Mercat, A.; Brower, R.G.; Talmor, D.; Walter, S.D.; Slutsky, A.S.; Pullenayegum, E.; Urbach, R.; Anvari, M.; et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: Systematic review and meta-analysis. JAMA 2010, 303, 865–873. [Google Scholar] [CrossRef]
- Yoshifuku, S.; Otsuji, Y.; Takasaki, K.; Yuge, K.; Kisanuki, A.; Toyonaga, K.; Lee, S.; Murayama, T.; Nakashima, H.; Kumanohoso, T.; et al. Tei C: Pseudonormalized Doppler total ejection isovolume (Tei) index in patients with right ventricular acute myocardial infarction. Am. J. Cardiol. 2003, 91, 527–531. [Google Scholar] [CrossRef]
|
Lower PEEP (n = 20) |
Higher PEEP (n = 24) | p Value | |
|---|---|---|---|
| Age, y | 64 (56 to 72) | 65 (59 to 70) | 0.93 |
| Female gender, No. (%) | 10 (50) | 8 (33) | 0.34 |
| Height, cm | 172 ± 10 | 175 ± 7 | 0.25 |
| Weight, cm | 76 ± 16 | 83 ± 16 | 0.15 |
| SOFA score a | 10.1 ± 2.9 | 9.6 ± 3.7 | 0.69 |
| Reason for ICU admission, No. (%) | 0.07 | ||
| Elective surgery | 4 (20) | 0 (0) | |
| Urgent surgery | 3 (15) | 4 (16) | |
| Medical | 13 (65) | 20 (84) | |
| Reason for intubation, No. (%) | 0.28 | ||
| Respiratory failure | 6 (30) | 7 (29) | 0.42 |
| Pneumonia | 2 (33) | 3 (43) | |
| Cardiogenic pulmonary edema | 2 (33) | 1 (14) | |
| Sepsis | 2 (33) | 2 (29) | |
| COPD, gold I-II | 0 (0) | 1 (14) | |
| Cardiac arrest | 1 (5) | 5 (21) | |
| Planned postoperative ventilation | 7 (35) | 3 (12) | |
| Depressed level of consciousness | 5 (25) | 6 (25) | |
| Airway protection | 1 (5) | 3 (12) | |
| Ventilatory mode, No. (%) | 0.33 | ||
| Pressure-controlled | 5 (25) | 6 (25) | |
| Pressure support | 15 (75) | 15 (63) | |
| Adaptive support ventilation | 0 | 3 (12) | |
| Sedation | 5 (25) | 13 (54) | 0.09 |
| Propofol | 5 (25) | 12 (50) | 0.17 |
| Midazolam | 2 (10) | 2 (8) | 1.00 |
| RASS b | −3 (−3 to −1) | −4 (−5 to −3) | 0.06 |
| Vasopressors and inotropes | |||
| Norepinephrine, No. (%) | 5 (25) | 7 (29) | 0.98 |
| Norepinephrine dose, μg kg−1 min−1 | 0.12 ± 0.11 | 0.13 ± 0.08 | 0.78 |
| Milrinon, No. (%) | 1 (5) | 0 (0) | 0.93 |
| Milrinon dose, μg kg−1 min−1 | 0.17 (0.18 to 0.17) | 0 (0) | 1 |
| Sinus rhythm, No. (%) | 17 (85) | 22 (85) | 0.83 |
| Fluid balance, mL | 304 (−604 to 928) | 1215 (−89 to 1944) | 0.04 |
|
Lower PEEP (n = 20) |
Higher PEEP (n = 24) | Point Estimate of the Difference (95% CI) | p Value | |
|---|---|---|---|---|
| Time, h a | 36 (27 to 46) | 36 (27 to 46) | 0 (−7 to 9) | 0.76 |
| Respiration | ||||
| PEEP, cmH2O | 0 ± 1 | 8 ± 1 | −8 (−8.1 to −7.9) | <0.01 |
| Pmax, cmH2O | 11.7 ± 4.1 | 20.1 ± 4.7 | −8.4 (−11.1 to −5.6) | <0.01 |
| FiO2, % | 27 (24 to 35) | 30 (24 to 34) | −3 (−4 to 4) | 0.91 |
| SpO2 | 97 (96 to 99) | 98 (95 to 99) | −1 (−0.9 to 1.9) | 0.45 |
| VT/predicted body weight, mL/kg b | 7.22 (6.3 to 8.1) | 7.02 (5.3 to 9.1) | 0.20 (−1.4 to1.2) | 0.97 |
| RR, breaths/min = | 19 ± 6 | 22 ± 6 | −3 (−6 to 1) | 0.12 |
| Minute volume, L/min = | 9. 5(8.1 to 10.8) | 10.2 (8.7 to 13.1) | −0.5 (−3.5 to 0.3) | 0.14 |
| Laboratory | ||||
| pH | 7.46 ± 0.05 | 7.42 ± 0.04 | 0.04 (0.01 to 0.07) | 0.01 |
| PaCO2, kPa | 4.6 (4.1 to 5.2) | 5.1 (4.7 to 5.5) | −0.5 (−0.9 to 0.1) | 0.07 |
| PaO2, kPa | 10.8 (10.4 to 12.6) | 11.0 (10.1 to 12.0) | -0.2 (−1.1 to 1.1) | 0.82 |
| Hemoglobin, mmol/L | 6.3 ± 0.05 | 7.3 ± 0.04 | −1 (−1.9 to −0.2) | 0.01 |
| Hemodynamics | ||||
| HR, mmHg | 81 (67 to 100) | 82 (66 to 105) | −1 (−18 to 10.9) | 0.65 |
| SBP, mmHg | 138 ± 26 | 125 ± 29 | 13 (−4 to 29) | 0.15 |
| DBP, mmHg | 63 ± 11 | 61 ± 12 | 2 (−4 to 9) | 0.51 |
| MAP, mmHg | 88 ± 15 | 82 ± 15 | 6 (−2 to 15) | 0.17 |
| Right Ventricular Variables |
Lower PEEP (n = 20) |
Higher PEEP (n = 24) |
Point Estimate of the Difference (95% CI) | p Value | Left Ventricular Variables |
Lower PEEP (n = 20) |
Higher PEEP (n = 24) |
Point Estimate of the Difference (95% CI) | p Value |
|---|---|---|---|---|---|---|---|---|---|
| Primary parameter | |||||||||
| Myocardial performance index | 0.32 (0.26 to 0.39) | 0.38 (0.32 to 0.41) | −0.03 (−0.11 to 0.03) | 0.33 | Myocardial performance index | 0.41 (0.37 to 0.49) | 0.45 (0.39 to 0.54) | −0.02 (−0.09 to 0.04) | 0.35 |
| Systolic parameters | Systolic parameters | ||||||||
| Tricuspid annular plane systolic excursion (mm) | 22 (17 to 25) | 20 (18 to 22) | 0.0 (−3 to 4) | 0.75 | Ejection fraction, %, | 55 (49 to 58) | 59 (51 to 65) | −5.1 (−10.9 to 2.9) | 0.23 |
| Global longitudinal strain, %, median (IQR) | −18 (−20 to −11) | −22 (−24 to −16) | 4 (−2.1 to 9.9) | 0.17 | Global longitudinal strain, % | −12 (−19 to −8) | −12 (−15 to 10) | 0.2 (−2.7 to 3.2) | 0.92 |
| Isovolumetric acceleration, m/s | 3.3 (3.1 to 4.1) | 3.1 (2.5 to 4.9) | 0.0 (−1.4 to 0.7) | 0.41 | Isovolumetric acceleration, m/s | 3.2 (2.1 to 4.7) | 3.4 (2.1 to 5.9) | −0.3 (−1.5 to 0.6) | 0.49 |
| Systolic maximal velocity, cm/s | 12.4 ± 3 | 12.5 ± 4 | −0.1 (−2.4 to 2.2) | 0.91 | Systolic maximal velocity, cm/s | 8.3 ± 2.2 | 8.3 ± 2.3 | 0 (−1.4 to 1.4) | 0.92 |
| Diastolic parameters | Diastolic parameters | ||||||||
| Early/atrial velocity ratio | 1.1 (0.8 to 1.2) | 0.9 (0.8 to 1.1) | 0.1 (−0.1 to 0.3) | 0.53 | Early/atrial velocity ratio | 0.9 (0.72 to 1.1) | 1.0 (0.66 to 1.3) | −0.0 (−0.3 to 0.2) | 0.81 |
| Early maximal diastolic velocity, cm/s | 11.1 ± 3 | 12.7 ± 4 | −1.6 (−4.1 to 0.8) | 0.21 | Early maximal diastolic velocity, cm/s | 8.7 ± 3.4 | 8.7 ± 3.1 | 0 (−1.9 to 2.1) | 0.95 |
| E/E′ | 4.1 (3.3 to 5.6) | 4.1 (3.3 to 5.6) | 0.6 (−0.5 to 1.6) | 0.28 | E/E′ | 8.3 (6.1 to 11.6) | 8.6 (6.4 to 10.8) | 0.2 (−2.4 to 2.7) | 0.82 |
| General parameters | General parameters | ||||||||
| Pulmonary acceleration time, m/s2 | 9.1 ± 4 | 8.9 ± 3 | 0.2 (−3.1 to 3.2) | 0.93 | Cardiac index, l min−1 m2 −1 | 2.8 ± 0.9 | 2.5 ± 0.7 | 0.3 −0.2 to 0.9) | 0.24 |
| Right ventricle/left ventricle diameter a | 0.72 (0.61 to 0.81) | 0.74 (0.61 to 0.93) | −0.02 (−0.2 to 0.1) | 0.75 | Eccentricity index | 1 (0.8 to 1.1) | 0.9 (0.8 to 1.0) | 0.05 (−0.07 to 0.21) | 0.39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Algera, A.G.; Pierrakos, C.; Botta, M.; Zimatore, C.; Pisani, L.; Tuinman, P.-R.; Bos, L.D.J.; Lagrand, W.K.; Gama de Abreu, M.; Pelosi, P.; et al. Myocardial Function during Ventilation with Lower versus Higher Positive End-Expiratory Pressure in Patients without ARDS. J. Clin. Med. 2022, 11, 2309. https://doi.org/10.3390/jcm11092309
Algera AG, Pierrakos C, Botta M, Zimatore C, Pisani L, Tuinman P-R, Bos LDJ, Lagrand WK, Gama de Abreu M, Pelosi P, et al. Myocardial Function during Ventilation with Lower versus Higher Positive End-Expiratory Pressure in Patients without ARDS. Journal of Clinical Medicine. 2022; 11(9):2309. https://doi.org/10.3390/jcm11092309
Chicago/Turabian StyleAlgera, Anna Geke, Charalampos Pierrakos, Michela Botta, Claudio Zimatore, Luigi Pisani, Pieter-Roel Tuinman, Lieuwe D. J. Bos, Wim K. Lagrand, Marcello Gama de Abreu, Paolo Pelosi, and et al. 2022. "Myocardial Function during Ventilation with Lower versus Higher Positive End-Expiratory Pressure in Patients without ARDS" Journal of Clinical Medicine 11, no. 9: 2309. https://doi.org/10.3390/jcm11092309
APA StyleAlgera, A. G., Pierrakos, C., Botta, M., Zimatore, C., Pisani, L., Tuinman, P.-R., Bos, L. D. J., Lagrand, W. K., Gama de Abreu, M., Pelosi, P., Serpa Neto, A., Schultz, M. J., Cherpanath, T. G. V., & Paulus, F. (2022). Myocardial Function during Ventilation with Lower versus Higher Positive End-Expiratory Pressure in Patients without ARDS. Journal of Clinical Medicine, 11(9), 2309. https://doi.org/10.3390/jcm11092309








