Case Series on the Long-Term Effect of Three Different Types of Maxillary Implant-Supported Overdentures on Clinical Outcomes and Complications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Treatment Allocation
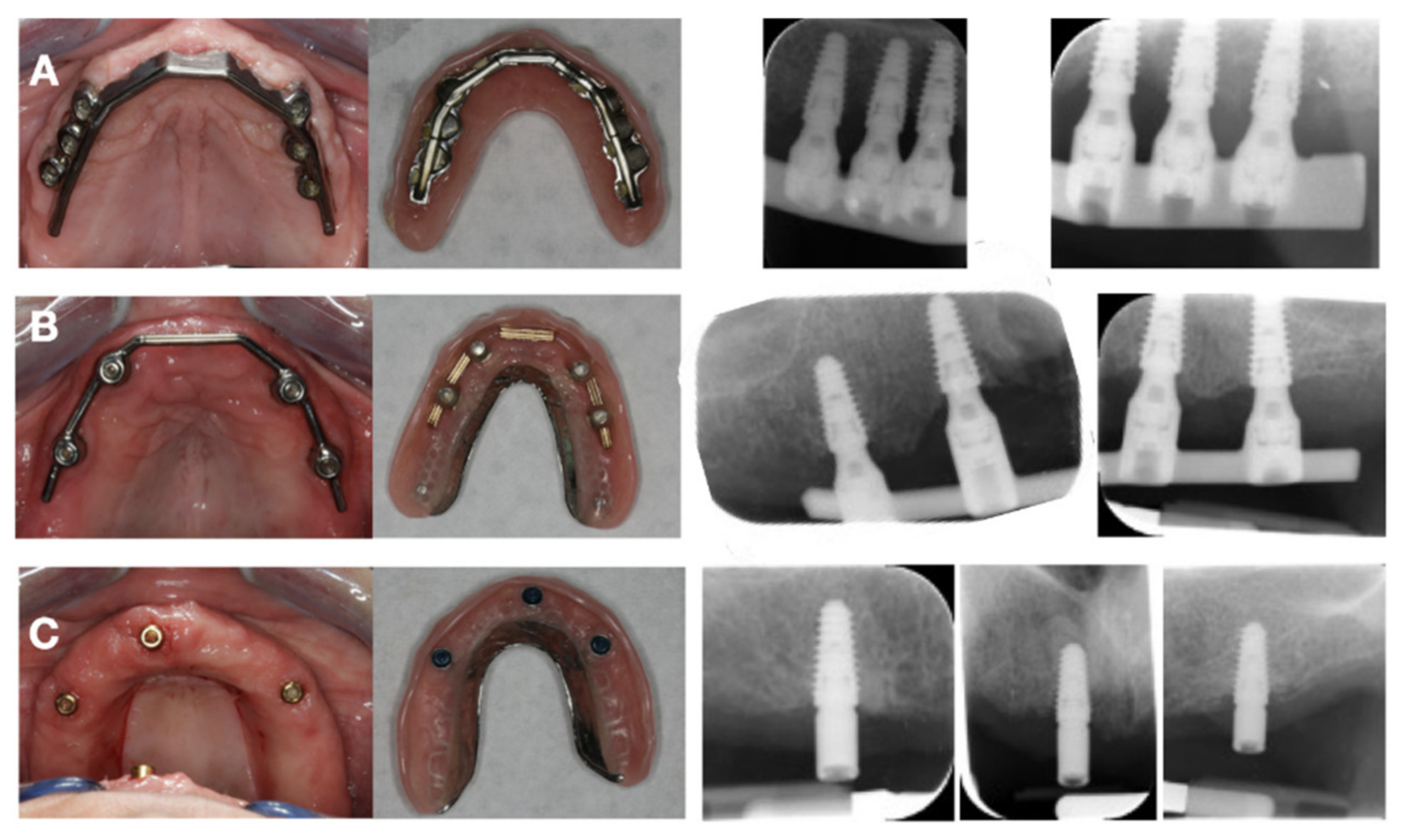
2.2. Surgical and Prosthetic Procedure
2.3. Clinical Assessment
2.4. Statistical Analysis
3. Results
3.1. Clinical Outcome
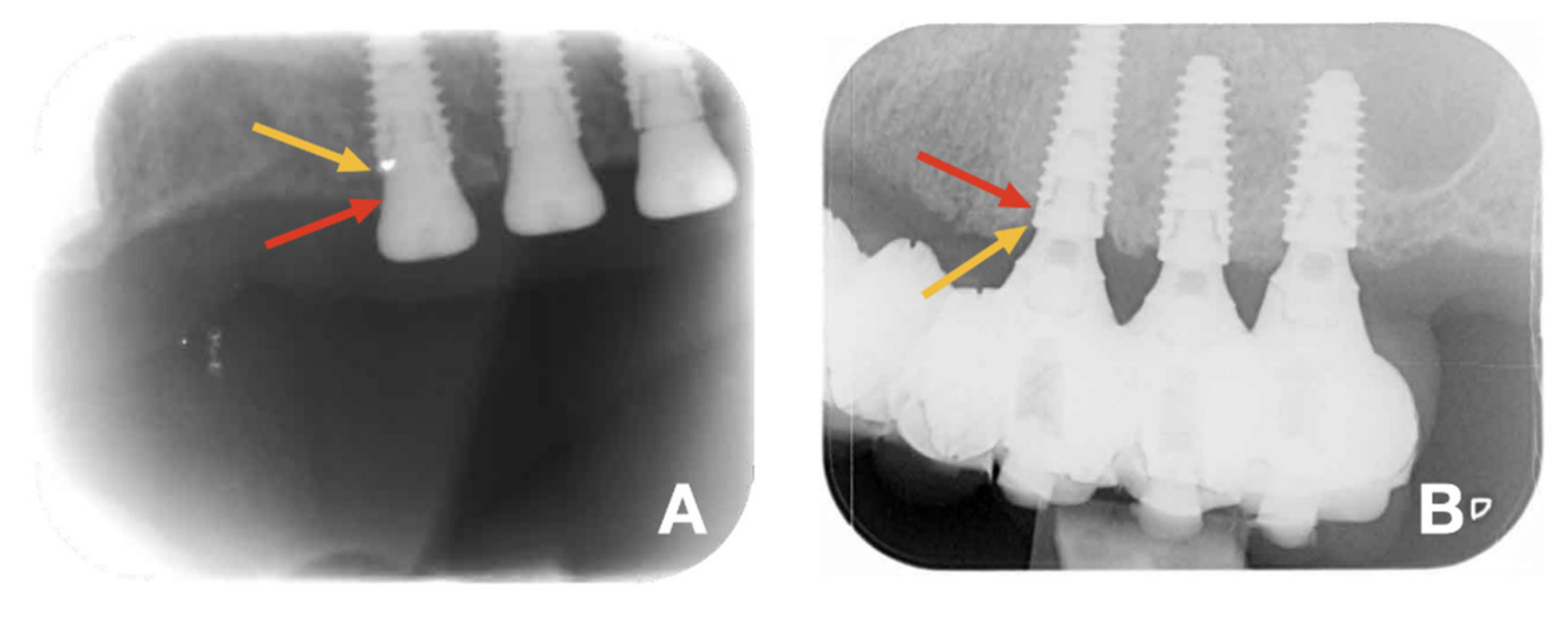
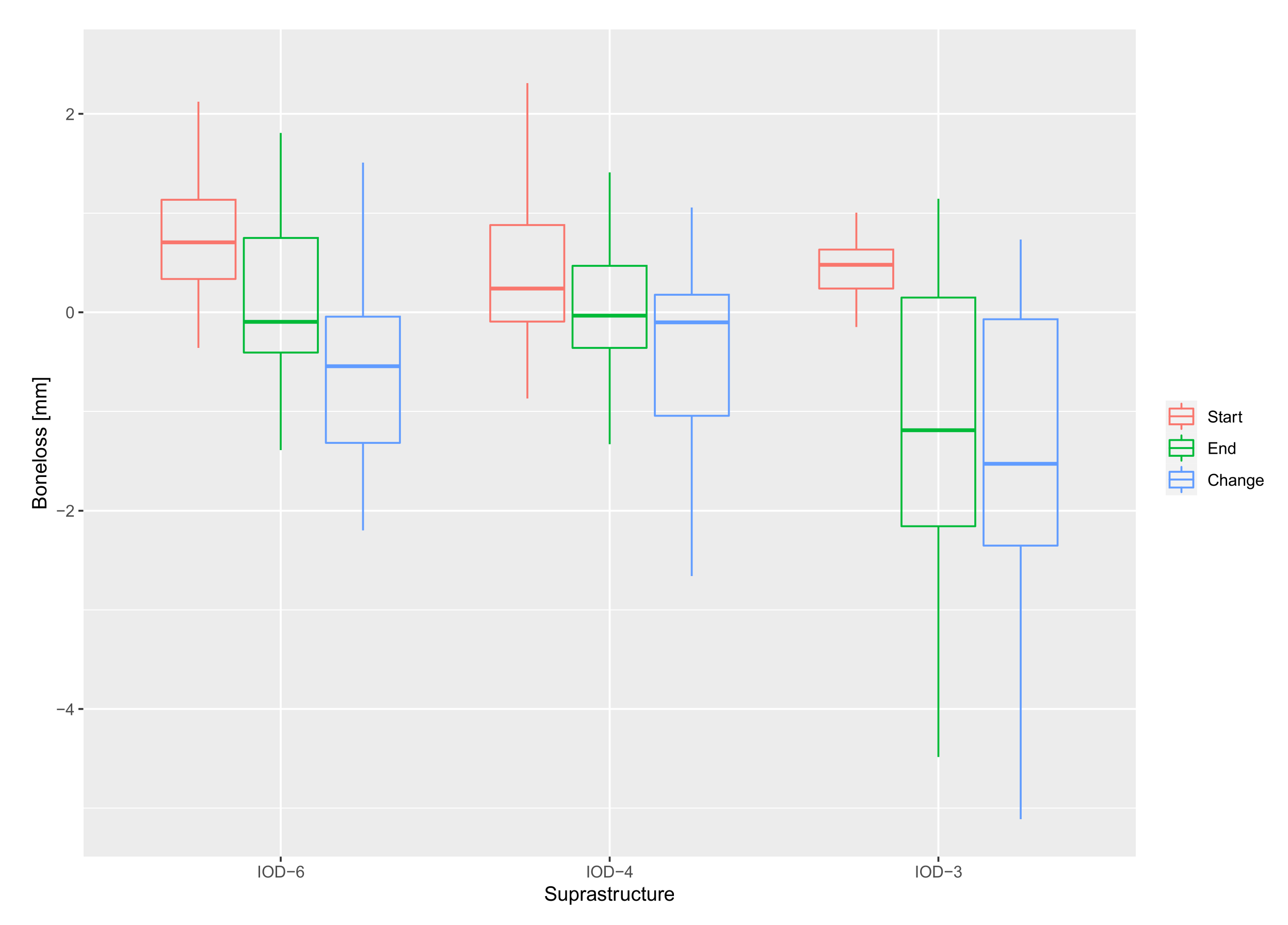
3.2. Bone Level and Probing Pocket Depth
3.3. Peri-Implant Health
3.4. Complications
4. Discussion
4.1. Survival
4.2. Bone Loss
4.3. Peri-Implant Health
4.4. Complications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holm-Pedersen, P.; Lang, N.P.; Muller, F. What are the longevities of teeth and oral implants? Clin. Oral Implant. Res. 2007, 18 (Suppl. 3), 15–19. [Google Scholar] [CrossRef] [PubMed]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Lund, J.P.; MacEntee, M.; Mericske-Stern, R.; et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24–25, 2002. Int. J. Oral Maxillofac. Implant. 2002, 17, 601–602. [Google Scholar]
- Pjetursson, B.E.; Tan, K.; Lang, N.P.; Brägger, U.; Egger, M.; Zwahlen, M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin. Oral Implant. Res. 2004, 15, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Simonis, P.; Dufour, T.; Tenenbaum, H. Long-term implant survival and success: A 10–16-year follow-up of non-submerged dental implants. Clin. Oral Implant. Res. 2010, 21, 772–777. [Google Scholar] [CrossRef]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur. J. Oral Sci. 1998, 106, 721–764. [Google Scholar] [CrossRef]
- Jemt, T.; Johansson, J. Implant treatment in the edentulous maxillae: A 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin. Implant Dent. Relat. Res. 2006, 8, 61–69. [Google Scholar] [CrossRef]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Francischone, C.; Rigolizzo, M. “All-on-4” immediate-function concept for completely edentulous maxillae: A clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl 1), e139–e150. [Google Scholar] [CrossRef]
- Astrand, P.; Engquist, B.; Dahlgren, S.; Grondahl, K.; Engquist, E.; Feldmann, H. Astra Tech and Branemark system implants: A 5-year prospective study of marginal bone reactions. Clin. Oral Implant. Res. 2004, 15, 413–420. [Google Scholar] [CrossRef]
- Linkevicius, T.; Apse, P.; Grybauskas, S.; Puisys, A. The influence of soft tissue thickness on crestal bone changes around implants: A 1-year prospective controlled clinical trial. Int. J. Oral Maxillofac. Implant. 2009, 24, 712–719. [Google Scholar]
- Albrektsson, T.; Canullo, L.; Cochran, D.; De Bruyn, H. “Peri-Implantitis”: A Complication of a Foreign Body or a Man-Made “Disease”. Facts and Fiction. Clin. Implant Dent. Relat. Res. 2016, 18, 840–849. [Google Scholar] [CrossRef]
- Sinjari, B.; D’Addazio, G.; De Tullio, I.; Traini, T.; Caputi, S. Peri-Implant Bone Resorption during Healing Abutment Placement: The Effect of a 0.20% Chlorhexidine Gel vs. Placebo-A Randomized Double Blind Controlled Human Study. BioMed Res. Int. 2018, 2018, 5326340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinjari, B.; D’Addazio, G.; Traini, T.; Varvara, G.; Scarano, A.; Murmura, G.; Caputi, S. A 10-year retrospective comparative human study on screw-retained versus cemented dental implant abutments. J. Biol. Regul. Homeost. Agents 2019, 33, 787–797. [Google Scholar] [PubMed]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef] [PubMed]
- Doornewaard, R.; Jacquet, W.; Cosyn, J.; De Bruyn, H. How do peri-implant biologic parameters correspond with implant survival and peri-implantitis? A critical review. Clin. Oral. Implants Res. 2018, 29 (Suppl. 18), 100–123. [Google Scholar] [CrossRef]
- Heydecke, G.; Zwahlen, M.; Nicol, A.; Nisand, D.; Payer, M.; Renouard, F.; Grohmann, P.; Muhlemann, S.; Joda, T. What is the optimal number of implants for fixed reconstructions: A systematic review. Clin. Oral Implants Res. 2012, 23 (Suppl 6), 217–228. [Google Scholar] [CrossRef]
- Mertens, C.; Steveling, H.G. Implant-supported fixed prostheses in the edentulous maxilla: 8-year prospective results. Clin. Oral Implant. Res. 2011, 22, 464–472. [Google Scholar] [CrossRef]
- Bergendal, T.; Engquist, B. Implant-supported overdentures: A longitudinal prospective study. Int. J. Oral Maxillofac. Implants 1998, 13, 253–262. [Google Scholar]
- Visser, A.; Raghoebar, G.M.; Meijer, H.J.; Vissink, A. Implant-retained maxillary overdentures on milled bar suprastructures: A 10-year follow-up of surgical and prosthetic care and aftercare. Int. J. Prosthodont. 2009, 22, 181–192. [Google Scholar]
- Jemt, T.; Chai, J.; Harnett, J.; Heath, M.R.; Hutton, J.E.; Johns, R.B.; McKenna, S.; McNamara, D.C.; van Steenberghe, D.; Taylor, R.; et al. A 5-year prospective multicenter follow-up report on overdentures supported by osseointegrated implants. Int. J. Oral Maxillofac. Implants 1996, 11, 291–298. [Google Scholar]
- Sadowsky, S.J. Mandibular implant-retained overdentures: A literature review. J. Prosthet. Dent. 2001, 86, 468–473. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Treatment considerations for maxillary implant overdentures: A systematic review. J. Prosthet. Dent. 2007, 97, 340–348. [Google Scholar] [CrossRef]
- Slot, W.; Raghoebar, G.M.; Vissink, A.; Huddleston Slater, J.J.; Meijer, H.J. A systematic review of implant-supported maxillary overdentures after a mean observation period of at least 1 year. J. Clin. Periodontol. 2010, 37, 98–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roccuzzo, M.; Bonino, F.; Gaudioso, L.; Zwahlen, M.; Meijer, H.J. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures. Clin. Oral Implants Res. 2012, 23 (Suppl 6), 229–237. [Google Scholar] [CrossRef] [PubMed]
- Klemetti, E. Is there a certain number of implants needed to retain an overdenture? J. Oral Rehabil. 2008, 35 (Suppl 1), 80–84. [Google Scholar] [CrossRef]
- Naert, I.; Gizani, S.; van Steenberghe, D. Rigidly splinted implants in the resorbed maxilla to retain a hinging overdenture: A series of clinical reports for up to 4 years. J. Prosthet. Dent. 1998, 79, 156–164. [Google Scholar] [CrossRef]
- Kiener, P.; Oetterli, M.; Mericske, E.; Mericske-Stern, R. Effectiveness of maxillary overdentures supported by implants: Maintenance and prosthetic complications. Int. J. Prosthodont. 2001, 14, 133–140. [Google Scholar]
- Doornewaard, R.; Sakani, S.; Matthys, C.; Glibert, M.; Bronkhorst, E.; Vandeweghe, S.; Vervaeke, S.; De Bruyn, H. Four-implant-supported overdenture treatment in the maxilla. Part I: A randomized controlled split mouth trial assessing the effect of microthreads and abutment connection type on 4 years peri-implant health. Clin. Implant Dent. Relat. Res. 2021, 23, 671–679. [Google Scholar] [CrossRef]
- Mombelli, A.; van Oosten, M.A.; Schurch, E., Jr.; Land, N.P. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef]
- Zarb, G.A.; Albrektsson, T. Consensus report: Towards optimized treatment outcomes for dental implants. J. Prosthet. Dent. 1998, 80, 641. [Google Scholar] [CrossRef]
- Meijer, H.J.; Kuiper, J.H.; Starmans, F.J.; Bosman, F. Stress distribution around dental implants: Influence of superstructure, length of implants, and height of mandible. J. Prosthet. Dent. 1992, 68, 96–102. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Meijer, H.J.; Slot, W.; Slater, J.J.; Vissink, A. A systematic review of implant-supported overdentures in the edentulous maxilla, compared to the mandible: How many implants? Eur. J. Oral Implant. 2014, 7 (Suppl 2), S191–S201. [Google Scholar]
- Slot, W.; Raghoebar, G.M.; Cune, M.S.; Vissink, A.; Meijer, H.J. Maxillary overdentures supported by four or six implants in the anterior region: 5-year results from a randomized controlled trial. J. Clin. Periodontol. 2016, 43, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Van Doorne, L.; Gholami, P.; D’Haese, J.; Hommez, G.; Meijer, G.; De Bruyn, H. Three-Dimensional Radiographic Outcome of Free-Handed Flaplessly Placed Mini Dental Implants in Edentulous Maxillae after 2-Years Function. J. Clin. Med. 2020, 9, 2120. [Google Scholar] [CrossRef]
- Kamei, K.; Gonda, T.; Takahashi, T.; Maeda, Y. Mechanical Study of Optimal Implant Position for Maxillary Implant-Supported Overdentures Using Three-Dimensional Simulation Software. Int. J. Prosthodont. 2018, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Dimililer, G.; Kücükkurt, S.; Cetiner, S. Biomechanical effects of implant number and diameter on stress distributions in maxillary implant-supported overdentures. J. Prosthet. Dent. 2018, 119, 244–249.e6. [Google Scholar] [CrossRef]
- Di Francesco, F.; De Marco, G.; Sommella, A.; Lanza, A. Splinting vs Not Splinting Four Implants Supporting a Maxillary Overdenture: A Systematic Review. Int. J. Prosthodont. 2019, 32, 509–518. [Google Scholar] [CrossRef]
- Dierens, M.; Vandeweghe, S.; Kisch, J.; Nilner, K.; De Bruyn, H. Long-term follow-up of turned single implants placed in periodontally healthy patients after 16–22 years: Radiographic and peri-implant outcome. Clin. Oral Implants Res. 2012, 23, 197–204. [Google Scholar] [CrossRef]
- Verhoeven, J.W.; Cune, M.S.; de Putter, C. Reliability of some clinical parameters of evaluation in implant dentistry. J. Oral Rehabil. 2000, 27, 211–216. [Google Scholar] [CrossRef]
- Onclin, P.; Slot, W.; Vissink, A.; Raghoebar, G.M.; Meijer, H.J.A. Incidence of peri-implant mucositis and peri-implantitis in patients with a maxillary overdenture: A sub-analysis of two prospective studies with a 10-year follow-up period. Clin. Implant Dent. Relat. Res. 2022, 1–8. [Google Scholar] [CrossRef]
- Meyle, J.; Gersok, G.; Boedeker, R.H.; Gonzales, J.R. Long-term analysis of osseointegrated implants in non-smoker patients with a previous history of periodontitis. J. Clin. Periodontol. 2014, 41, 504–512. [Google Scholar] [CrossRef]
- Mangano, C.; Mangano, F.; Shibli, J.A.; Ricci, M.; Sammons, R.L.; Figliuzzi, M. Morse taper connection implants supporting “planned” maxillary and mandibular bar-retained overdentures: A 5-year prospective multicenter study. Clin. Oral Implant. Res. 2011, 22, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Slot, W.; Raghoebar, G.M.; van Dijk, G.; Meijer, H.J. Attachment of clips in a bar-retained maxillary implant overdenture: A clinical report. J. Prosthet. Dent. 2012, 107, 353–357. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Periodontol. 2018, 89 (Suppl. 1), S267–S290. [Google Scholar] [CrossRef] [PubMed]
| Total Patient Group | IOD-6 | IOD-4 | IOD-3 | ||
|---|---|---|---|---|---|
| Number of patients | Baseline | 31 | 9 | 12 | 10 |
| Follow-up | 23 | 7 (−1 §) | 11 (10 + 1 §) | 5 | |
| Number of implants | Baseline | 132 | 54 | 48 | 30 |
| Follow-up | 102 | 42 | 46 (44 + 2 §) | 15 | |
| Bone level at baseline (mm) | Mean (SD; range) | 0.55 (0.74; −1.06–2.48) | 0.70 (0.77; −1.06–2.13) | 0.45 (0.77; −0.87–2.48) | 0.39 (0.39; −0.50–1.01) |
| Bone level at follow-up (mm) | Mean (SD; range) | −0.10 (1.01; −4.49–2.14) | 0.02 (0.91; −2.8–1.81) | 0.06 (0.70; −1.33–2.14) | −1.03 (1.61; −4.49–1.15) |
| Bone loss (mm) | Mean (SD; range) | 0.65 (1.20; −2.44–5.11) | 0.68 (1.06; −1.51–4.57) | 0.39 (1.06; −2.43–3.6) | 1.43 (1.68; −0.74–5.11) |
| PPD (mm) | Mean (SD; range) | 3.6 (0.66; 2.0–5.3) | 3.8 (0.69; 2.5–5.3) | 3.5 (0.59; 2.33–5) | 3.2 (0.56; 2–4) |
| BOP (relative %) | Mean (SD; range) | 61.6% (31.1%; 0–100%) | 78.6% (24.9%; 33.0–100%) | 54.5% (33.2%; 0–100%) | 53.3% (29.8%; 33.0–100%) |
| Variable | Effect | 95% CI | p-Value | |
|---|---|---|---|---|
| Bone Loss (mm) | Intercept | −0.030 | [−0.642 … 0.583] | 0.925 |
| Bone level at baseline | 0.074 | [−0.142 … 0.290] | 0.503 | |
| IOD-6 vs. IOD-4 | 0.085 | [−0.685 … 0.855] | 0.828 | |
| IOD-6 vs. IOD-3 | −0.985 | [−1.940 … −0.028] | 0.044 | |
| IOD-4 vs. IOD-3 * | −1.070 | [−1.959 … −0.180] | 0.018 | |
| PPD (mm) | Intercept | 3.754 | [3.427 … 4.080] | <0.001 |
| IOD-6 vs. IOD-4 | 0.188 | [−0.612 … 0.237] | 0.387 | |
| IOD-6 vs. IOD-3 | −0.599 | [−1.136 … −0.062] | 0.029 | |
| IOD-4 vs. IOD-3 * | −0.411 | [−0.917 … −0.094] | 0.111 |
| Pocket Depth | |||||
|---|---|---|---|---|---|
| Bone Loss | ≤3 mm | >3 mm and ≤4 mm | >4 mm and ≤5 mm | >5 mm | Total |
| <0 mm | 5 (2,1.9%) | 23 (12, 11.8%) | 4 (3, 2.9%) | 1 (1, 0.9%) | 33 |
| ≤1 mm | 8 (4, 3.9%) | 23 (17, 16.7%) | 5 (4, 3.9%) | 0 | 36 |
| >1 ≤2 mm | 7 (4, 3.9%) | 9 (7, 6.9%) | 3 (3, 2.9%) | 0 | 19 |
| >2 ≤3 mm | 2 (0) | 9 (5, 4.9%) | 2 (2, 1.9%) | 1 (1, 0.9%) | 14 |
| Total |
22 (10, 10.2%) |
64 (41, 41.8%) |
14 (12, 12.2%) |
2 (2, 1.9%) | 102 |
| Complications | |||||||
|---|---|---|---|---|---|---|---|
| Suprastructure | Patient ID | Total No. | Technical | Biological | Aesthetic | Mean Bone Loss (mm) | Mean PPD (mm) |
| IOD-6 | 1 | 1 | 1 | 1.84 | 4.42 | ||
| 2 | 2 | 2 | 0.60 | 3.69 | |||
| 3 | 2 | 2 | −0.06 | 3.86 | |||
| 4 | 4 | 4 | 0.72 | 3.03 | |||
| 5 | 1 | 1 | 0.77 | 3.53 | |||
| 6 | 2 | 1 | 0.25 | 3.14 | |||
| 7 | 1 | 1 | 0.61 | 4.61 | |||
| IOD-4 | 8 | 0.98 | 2.92 | ||||
| 9 | 2 | 2 | −0.01 | 3.58 | |||
| 10 | 1 | 1 | 0.16 | 4.08 | |||
| 11 | 1.15 | 3.38 | |||||
| 12 | 2 | 1 * | 1 | −1.05 | 3.88 | ||
| 13 | 0.14 | 4.29 | |||||
| 14 | 1 | 1 | 0.64 | 3.75 | |||
| 15 | −0.20 | 3.42 | |||||
| 16 | 1 | 1 | 0.18 | 3.38 | |||
| 17 | 2.10 | 3.21 | |||||
| 18 | −0.12 | 3.42 | |||||
| IOD-3 | 19 | 1 | 1 | 3.49 | 3.44 | ||
| 20 | 1 | 1 | 1.83 | 3.33 | |||
| 21 | 4 | 4 | −0.67 | 3.11 | |||
| 22 | 1.91 | 2.72 | |||||
| 23 | 3 | 2 | 1 ** | 0.20 | 3.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naeini, E.N.; De Bruyn, H.; Bronkhorst, E.M.; D’haese, J. Case Series on the Long-Term Effect of Three Different Types of Maxillary Implant-Supported Overdentures on Clinical Outcomes and Complications. J. Clin. Med. 2022, 11, 2251. https://doi.org/10.3390/jcm11082251
Naeini EN, De Bruyn H, Bronkhorst EM, D’haese J. Case Series on the Long-Term Effect of Three Different Types of Maxillary Implant-Supported Overdentures on Clinical Outcomes and Complications. Journal of Clinical Medicine. 2022; 11(8):2251. https://doi.org/10.3390/jcm11082251
Chicago/Turabian StyleNaeini, Emitis Natali, Hugo De Bruyn, Ewald M. Bronkhorst, and Jan D’haese. 2022. "Case Series on the Long-Term Effect of Three Different Types of Maxillary Implant-Supported Overdentures on Clinical Outcomes and Complications" Journal of Clinical Medicine 11, no. 8: 2251. https://doi.org/10.3390/jcm11082251
APA StyleNaeini, E. N., De Bruyn, H., Bronkhorst, E. M., & D’haese, J. (2022). Case Series on the Long-Term Effect of Three Different Types of Maxillary Implant-Supported Overdentures on Clinical Outcomes and Complications. Journal of Clinical Medicine, 11(8), 2251. https://doi.org/10.3390/jcm11082251







