Real-World Data of Trastuzumab Deruxtecan for Advanced Gastric Cancer: A Multi-Institutional Retrospective Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment
2.3. Evaluation and Statistical Analysis
3. Results
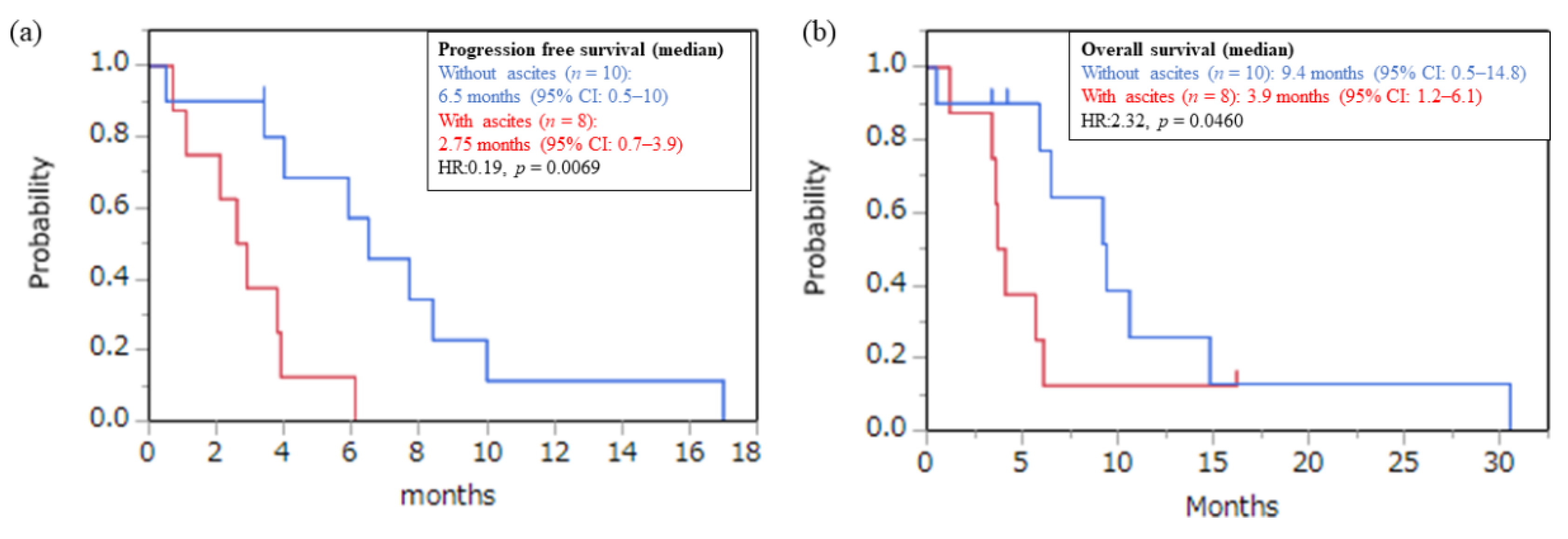
3.1. Efficacy
3.2. Safety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gravalos, C.; Jimeno, A. HER2 in Gastric Cancer: A New Prognostic Factor and a Novel Therapeutic Target. Ann. Oncol. 2008, 19, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in Combination with Chemotherapy Versus Chemotherapy Alone for Treatment of HER2-Positive Advanced Gastric or Gastro-oesophageal Junction Cancer (ToGA): A phase 3, Open-Label, Randomised Controlled Trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Ogitani, Y.; Aida, T.; Hagihara, K.; Yamaguchi, J.; Ishii, C.; Harada, N.; Soma, M.; Okamoto, H.; Oitate, M.; Arakawa, S.; et al. DS-8201a, a Novel HER2-Targeting ADC with a Novel DNA Topoisomerase I Inhibitor, Demonstrates a Promising Antitumor Efficacy with Differentiation from T-DM1. Clin. Cancer Res. 2016, 22, 5097–5108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shitara, K.; Iwata, H.; Takahashi, S.; Tamura, K.; Park, H.; Modi, S.; Tsurutani, J.; Kadowaki, S.; Yamaguchi, K.; Iwasa, S.; et al. Trastuzumab deruxtecan (DS-8201a) in patientswith advanced HER2-positive gastric cancer:a dose-expansion, phase 1 study. Lancet Oncol. 2019, 20, 827–836. [Google Scholar] [CrossRef]
- Shitara, K.; Bang, Y.J.; Iwasa, S.; Sugimoto, N.; Ryu, M.H.; Sakai, D.; Chung, H.C.; Kawakami, H.; Yabusaki, H.; Lee, J.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Gastric Cancer. N. Engl. J. Med. 2020, 382, 2419–2430. [Google Scholar] [CrossRef] [PubMed]
- Osa, A.; Uenami, T.; Koyama, S.; Fujimoto, K.; Okuzaki, D.; Takimoto, T.; Hirata, H.; Yano, Y.; Yokota, S.; Kinehara, Y.; et al. Clinical Implications of Monitoring Nivolumab Immunokinetics in Non-Small Cell Lung Cancer patients. JCI Insight. 2018, 3, e59125. [Google Scholar] [CrossRef] [PubMed]
- Iwata, T.N.; Ishii, C.; Ishida, S.; Ogitani, Y.; Wada, T.; Agatsuma, T. A HER2-Targeting Antibody-Drug Conjugate, Trastuzumab Deruxtecan (DS-8201a), Enhances Antitumor Immunity in a Mouse Model. Mol. Cancer Ther. 2018, 17, 1494–1503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makiyama, A.; Sukawa, Y.; Kashiwada, T.; Kawada, J.; Hosokawa, A.; Horie, Y.; Tsuji, A.; Moriwaki, T.; Tanioka, H.; Shinozaki, K.; et al. Randomized, phase II Study of Trastuzumab Beyond Progression in Patients with HER2-Positive Advanced Gastric or Gastroesophageal Junction Cancer: WJOG7112G (T-ACT Study). J. Clin. Oncol. 2020, 38, 1919–1927. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.S.; Liu, Z.X.; Lu, Y.X.; Bao, H.; Wu, X.; Zeng, Z.L.; Liu, Z.; Zhao, Q.; He, C.Y.; Lu, J.H.; et al. Liquid biopsies to track trastuzumab resistance in metastatic HER2-positive gastric cancer. Gut 2019, 68, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Pietrantonio, F.; Caporale, M.; Morano, F.; Scartozzi, M.; Gloghini, A.; De Vita, F.; Giommoni, E.; Fornaro, L.; Aprile, G.; Melisi, D.; et al. HER2 loss in HER2-positive gastric or gastroesophageal cancer after trastuzumab therapy: Implication for further clinical research. Int. J. Cancer 2016, 139, 2859–2864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shitara, K.; Bang, Y.; Iwasa, S.; Sugimoto, N.; Ryu, M.; Sakai, D.; Chung, H.; Omuro, Y.; Kawakami, H.; Yabusaki, H.; et al. O-14 Exploratory Biomarker Analysis of Trastuzumab Deruxtecan in DESTINY-Gastric01, a Randomized, phase 2, Multicenter, Open-Label Study in Patients with HER2-Positive or -Low Advanced Gastric or Gastroesophageal Junction Adenocarcinoma. Ann. Oncol. 2021, 32, S224. [Google Scholar] [CrossRef]
- Suzuki, H.; Yamada, T.; Sugaya, A.; Ueyama, S.; Yamamoto, Y.; Moriwaki, T.; Hyodo, I. Retrospective Analysis for the Efficacy and Safety of Nivolumab in Advanced Gastric Cancer Patients According to Ascites Burden. Int. J. Clin. Oncol. 2021, 26, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Sanchez-Vega, F.; Jonsson, P.; Chatila, W.K.; Hechtman, J.F.; Ku, G.Y.; Riches, J.C.; Tuvy, Y.; Kundra, R.; Bouvier, N.; et al. Genetic Predictors of Response to Systemic Therapy in Esophagogastric Cancer. Cancer Discov. 2018, 8, 49–58. [Google Scholar] [CrossRef] [Green Version]



| All (n = 18) | ||
|---|---|---|
| Age | Median (range) | 71 (51–85) |
| Sex | Male | 13 (72%) |
| ECOG PS | 0 | 9 (50%) |
| 1 | 6 (33%) | |
| 2/3 | 3 (17%) | |
| Primary site | Gastric | 14 (78%) |
| EGJ | 4 (4%) | |
| Histology | Diffuse type | 10 (56%) |
| Intestinal type | 8 (44%) | |
| HER2 status | IHC 3+ | 14 (78%) |
| IHC 2+, FISH (+) | 4 (22%) | |
| Prior gastrectomy | Yes | 9 (50%) |
| Number of metastatic sites | ≥2 | 15 (83%) |
| Liver metastasis | Yes | 7 (39%) |
| Peritoneal dissemination | Yes | 11 (61%) |
| Ascites | Yes | 8 (44%) |
| Massive ascites | Yes | 7 (39%) |
| Measurable lesion | Yes | 17 (94%) |
| Number of prior regimens | 2 | 6 (33%) |
| Over 2 | 12 (67%) | |
| Prior 5-FU | Yes | 18 (100%) |
| Prior Platinum | Yes | 18 (100%) |
| Prior taxane | Yes | 16 (89%) |
| Prior irinotecan | Yes | 3 (20%) |
| Prior ramucirumab | Yes | 16 (89%) |
| Prior immune check point inhibitors | Yes | 11 (61%) |
| Efficacy of Prior Tmab regimen | PR/SD/PD | 14/3/1 |
| Response rate of prior Tmab | PR | 14 (78%) |
| Tmab Free interval (months) | Median (range) | 7.7 (2.8–28.6) |
| ALL | G1/2 | G3/4 | |
|---|---|---|---|
| Neutropenia | 5 (28%) | 2 (11%) | 3 (17%) |
| Anemia | 6 (33%) | 4 (22%) | 2 (11%) |
| Platelet decreased | 2 (11%) | 2 (11%) | 0 |
| Fatigue | 11 (61%) | 11 (61%) | 0 |
| Anorexia | 7 (39%) | 6 (33%) | 1 (6%) |
| Nausea | 5 (28%) | 4 (22%) | 1 (6%) |
| Diarrhea | 3 (20%) | 3 (20%) | 0 |
| Heart failure | 2 (11%) | 2 (11%) | 0 |
| Pneumoniae | 1 (6%) | 1 (6%) | 0 |
| Rush | 1 (6%) | 1 (6%) | 0 |
| Constipation | 1 (6%) | 1 (6%) | 0 |
| Fever | 1 (6%) | 1 (6%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, T.; Yamamura, S.; Ikoma, T.; Kurioka, Y.; Doi, K.; Boku, S.; Shibata, N.; Nagai, H.; Shimada, T.; Tsuduki, T.; et al. Real-World Data of Trastuzumab Deruxtecan for Advanced Gastric Cancer: A Multi-Institutional Retrospective Study. J. Clin. Med. 2022, 11, 2247. https://doi.org/10.3390/jcm11082247
Matsumoto T, Yamamura S, Ikoma T, Kurioka Y, Doi K, Boku S, Shibata N, Nagai H, Shimada T, Tsuduki T, et al. Real-World Data of Trastuzumab Deruxtecan for Advanced Gastric Cancer: A Multi-Institutional Retrospective Study. Journal of Clinical Medicine. 2022; 11(8):2247. https://doi.org/10.3390/jcm11082247
Chicago/Turabian StyleMatsumoto, Toshihiko, Shogo Yamamura, Tatsuki Ikoma, Yusuke Kurioka, Keitaro Doi, Shogen Boku, Nobuhiro Shibata, Hiroki Nagai, Takanobu Shimada, Takao Tsuduki, and et al. 2022. "Real-World Data of Trastuzumab Deruxtecan for Advanced Gastric Cancer: A Multi-Institutional Retrospective Study" Journal of Clinical Medicine 11, no. 8: 2247. https://doi.org/10.3390/jcm11082247
APA StyleMatsumoto, T., Yamamura, S., Ikoma, T., Kurioka, Y., Doi, K., Boku, S., Shibata, N., Nagai, H., Shimada, T., Tsuduki, T., Tsumura, T., Takatani, M., Yasui, H., & Satake, H. (2022). Real-World Data of Trastuzumab Deruxtecan for Advanced Gastric Cancer: A Multi-Institutional Retrospective Study. Journal of Clinical Medicine, 11(8), 2247. https://doi.org/10.3390/jcm11082247






