Estimation of the Surface Dose in Breast Irradiation by the Beam Incident Angle and the 1 cm Depth Dose
Abstract
1. Introduction
2. Materials and Methods
2.1. Linear Accelerator (LA), Anthropomorphic Phantom, and cTPS
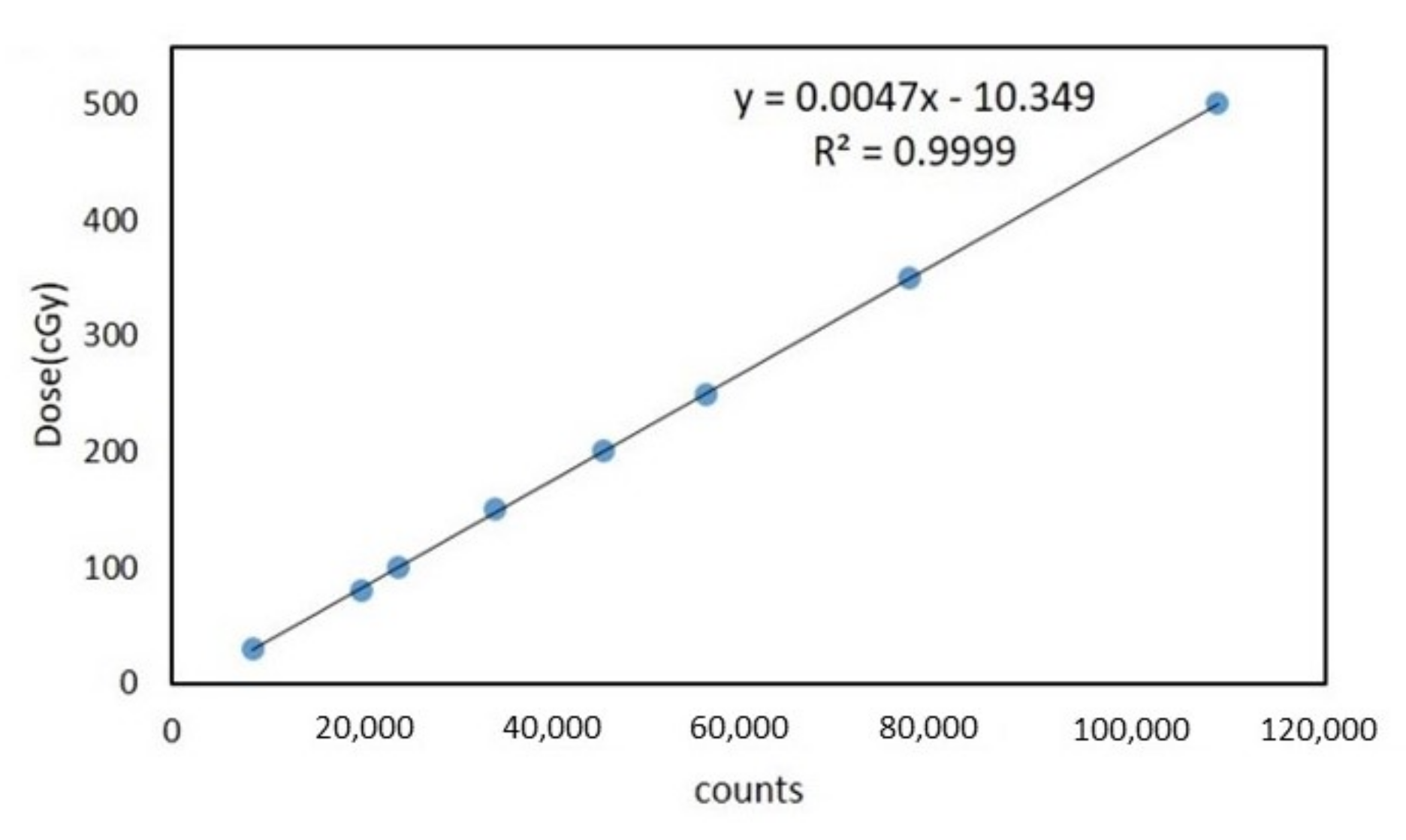
2.2. Thermoluminescent Dosimeter
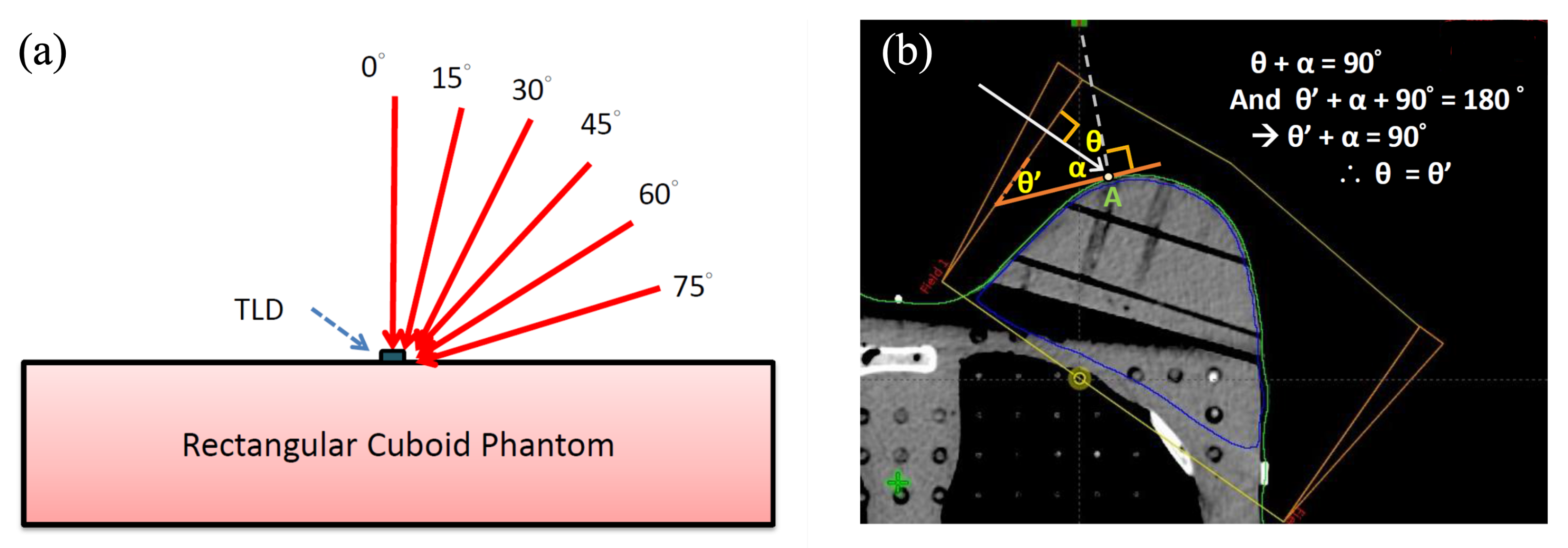
2.3. Surface Dose Measurement in Different Beam Angles by Rectangular Cuboid Phantom
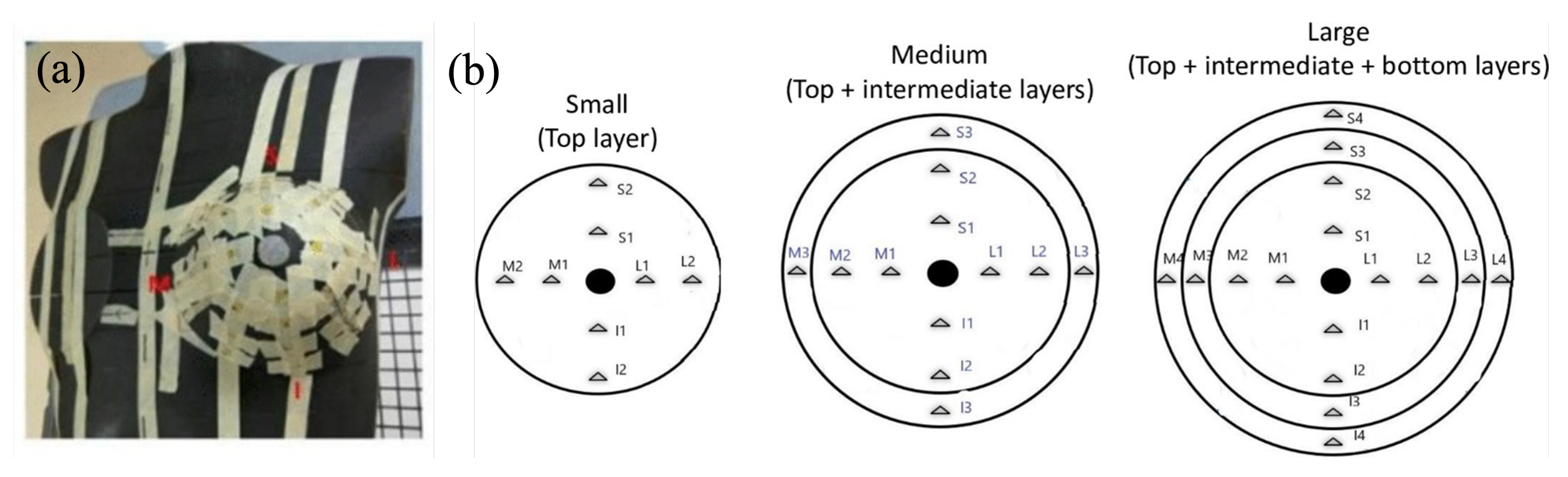
2.4. Measuring Points of Surface Dose Measurement for Different Breast Sizes Using Phantom Accessories
2.5. Measurement of Incident Angle and Irradiation Dose at Each Designated Point by Computerized TPS
2.6. Percentage of Skin Surface Dose Reference to a Depth of 1 cm (PSDR1cm)
2.7. Statistical Methods
3. Results
3.1. Surface Dose on a Rectangular Cuboid Solid-Water Phantom and Its Relationship to the Incident Angle
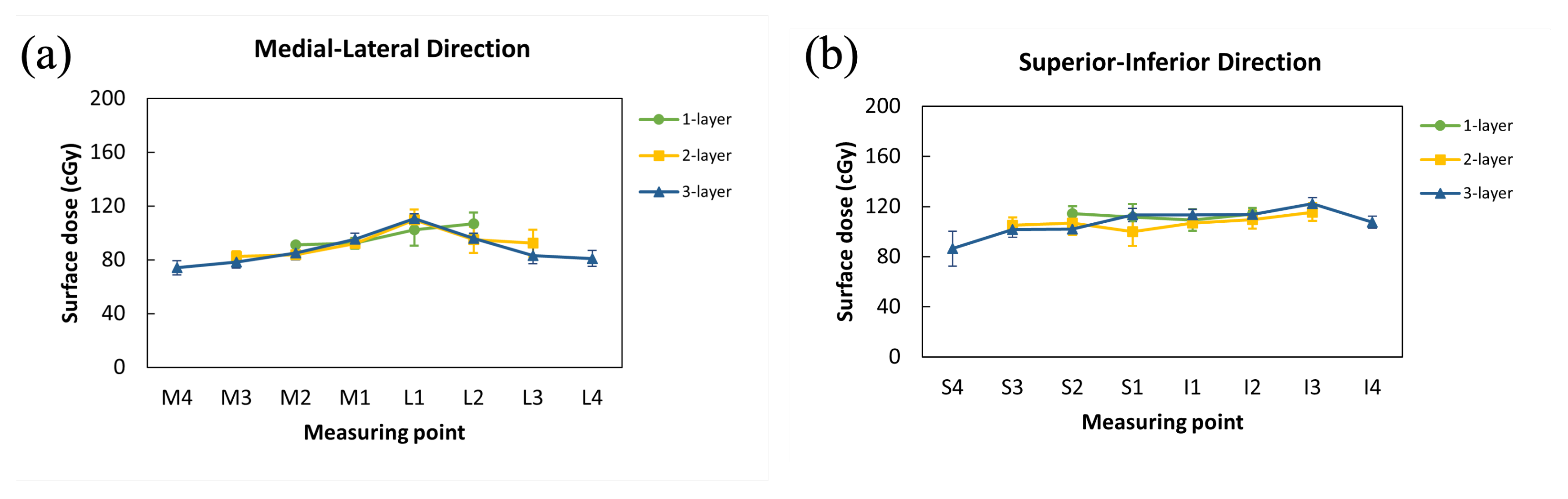
3.2. Surface Dose to Breast Accessories Measured by TLDs
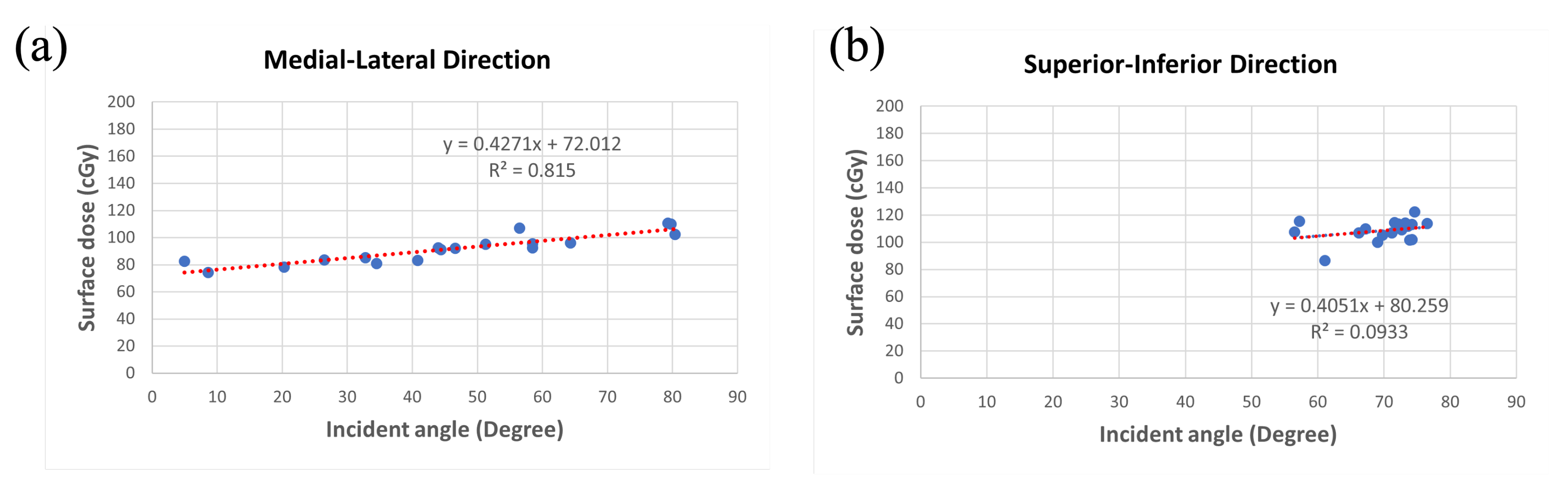
3.3. Relationship between Incident Angle and Surface Dose among Various Sizes of Breast Accessories
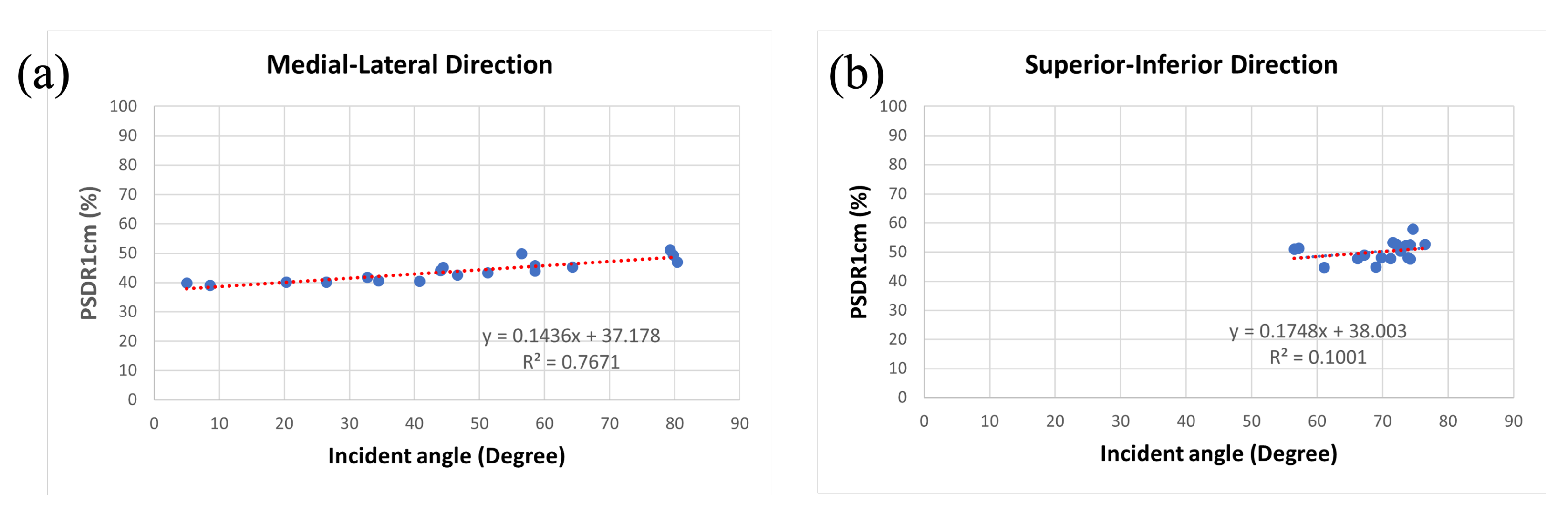
3.4. Relationship between Incident Angle and PSDR1cm among Various Sizes of Breast Accessories
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer Registry Annual Report of Taiwan (CRART) 2019. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=119 (accessed on 24 March 2022).
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG); Darby, S.; McGale, P.; Correa, C.; Taylor, C.; Arriagada, R.; Clarke, M.; Cutter, D.; Davies, C.; Ewertz, M.; et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011, 378, 1707–1716. [Google Scholar]
- Fisher, B.; Redmond, C.; Poisson, R.; Margolese, R.; Wolmark, N.; Wickerham, L.; Fisher, E.; Deutsch, M.; Caplan, R.; Pilch, Y.; et al. Eight-year results of a randomized clinical trial comparing total mastectomy and lumpectomy with or without irradiation in the treatment of breast cancer. N. Engl. J. Med. 1989, 320, 822–828. [Google Scholar] [CrossRef] [PubMed]
- Kole, A.J.; Kole, L.; Moran, M.S. Acute radiation dermatitis in breast cancer patients: Challenges and solutions. Breast Cancer 2007, 9, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.L. Ionizing radiation: The good, the bad, and the ugly. J. Invest. Dermatol. 2012, 132, 985–993. [Google Scholar] [CrossRef]
- Sun, L.M.; Huang, C.J.; Chen, H.Y.; Chang, G.H.; Tsao, M.J. Evaluating the consistency of location of the most severe acute skin reaction and highest skin dose measured by thermoluminescent dosimeter during radiotherapy for breast cancer. Med. Dosim. 2016, 41, 216–220. [Google Scholar] [CrossRef]
- Fraass, B.; Doppke, K.; Hunt, M.; Kutcher, G.; Starkschall, G.; Stern, R.; Van Dyke, J. American Association of Physicists in Medicine Radiation Therapy Committee Task Group 53: Quality assurance for clinical radiotherapy treatment planning. Med. Phys. 1998, 25, 1773–1829. [Google Scholar] [CrossRef]
- Devic, S.; Seuntjens, J.; Abdel-Rahman, W.; Evans, M.; Olivares, M.; Podgorsak, E.B.; Vuong, T.; Soares, C.G. Accurate skin dose measurements using radiochromic film in clinical applications. Med. Phys. 2006, 33, 1116–1124. [Google Scholar] [CrossRef]
- Hsu, S.H.; Roberson, P.L.; Chen, Y.; Marsh, R.B.; Pierce, L.J.; Moran, J.M. Assessment of skin dose for breast chest wall radiotherapy as a function of bolus material. Phys. Med. Biol. 2008, 53, 2593–2606. [Google Scholar] [CrossRef]
- Nakano, M.; Hill, R.F.; Whitaker, M.; Kim, J.H.; Kuncic, Z. A study of surface dosimetry for breast cancer radiotherapy treatments using Gafchromic EBT2 film. J. Appl. Clin. Med. Phys. 2012, 13, 3727. [Google Scholar] [CrossRef]
- Qin, S.; Chen, T.; Wang, L.; Tu, Y.; Yue, N.; Zhou, J. Angular dependence of the MOSFET dosimeter and its impact on in vivo surface dose measurement in breast cancer treatment. Technol. Cancer Res. Treat. 2014, 13, 345–352. [Google Scholar] [CrossRef]
- Almberg, S.S.; Lindmo, T.; Frengen, J. Superficial doses in breast cancer radiotherapy using conventional and IMRT techniques: A film-based phantom study. Radiother. Oncol. 2011, 100, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Rudat, V.; Nour, A.; Alaradi, A.A.; Mohamed, A.; Altuwaijri, S. In vivo surface dose measurement using GafChromic film dosimetry in breast cancer radiotherapy: Comparison of 7-field IMRT, tangential IMRT and tangential 3D-CRT. Radiat. Oncol. 2014, 9, 1569. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, L.B.; Silva, H.L.L.; de Campos, T.P.R. Experimental dosimetry in conformal breast teletherapy compared with the planning system. Appl. Radiat. Isot. 2015, 97, 93–100. [Google Scholar] [CrossRef]
- Coltman, C.E.; Steele, J.R.; McGhee, D.E. Breast volume is affected by body mass index but not age. Ergonomics 2017, 60, 1576–1585. [Google Scholar] [CrossRef]
- Coltman, C.E.; Steele, J.R.; McGhee, D.E. Effects of age and body mass index on breast characteristics: A cluster analysis. Ergonomics 2018, 61, 1232–1245. [Google Scholar] [CrossRef]
- Fern, I.N.; Ford, H.T.; Powles, T.J.; Ashley, S.; Glees, J.P.; Torr, M.; Grafton, D.; Harmer, C.L. Factors affecting acute skin toxicity in patients having breast irradiation after conservative surgery: A prospective study of treatment practice at the Royal Marsden Hospital. Clin. Oncol. 1996, 8, 226–233. [Google Scholar]
- Brierley, J.D.; Paterson, I.C.; Lallem, R.C.; Rostom, A.Y. The influence of breast size on late radiation reaction following excision and radiotherapy for early breast cancer. Clin. Oncol. 1991, 3, 6–9. [Google Scholar] [CrossRef]
- Behroozian, T.; Milton, L.; Li, N.; Zhang, L.; Lou, J.; Karam, I.; Wronski, M.; McKenzie, E.; Mawdsley, G.; Razvi, Y.; et al. Predictive factors associated with radiation dermatitis in breast cancer. Cancer Treat. Res. Commun. 2021, 28, 100403. [Google Scholar] [CrossRef]
- Southworth, A.; Clough, H.; Roberts, N. An audit of radiation-induced skin reactions in the inframammary fold; does breast size impact on the severity of the reaction? Radiography 2020, 26, 192–197. [Google Scholar] [CrossRef]
- Qian, X.; Vaidya, K.; Puckett, L.; Diaz, F.; Tang, X.; Lee, L.; Klein, E. A Post-Mastectomy Radiation Therapy Dose Distribution Study. Int. J. Med. Phys. Clin. Eng. Radiat. Oncol. 2017, 6, 457–467. [Google Scholar] [CrossRef][Green Version]
- Moncion, A.; Wilson, M.; Ma, R.; Marsh, R.; Burmeister, J.; Dryden, D.; Lack, D.; Grubb, M.; Mayville, A.; Jursinic, P.; et al. Evaluation of Dose Accuracy in the Near-Surface Region for Whole Breast Irradiation Techniques in a Multi-Institutional Consortium. Pract. Radiat. Oncol. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- McDermott, P.N. Surface dose and acute skin reactions in external beam breast radiotherapy. Med. Dosim. 2020, 45, 153–158. [Google Scholar] [CrossRef] [PubMed]
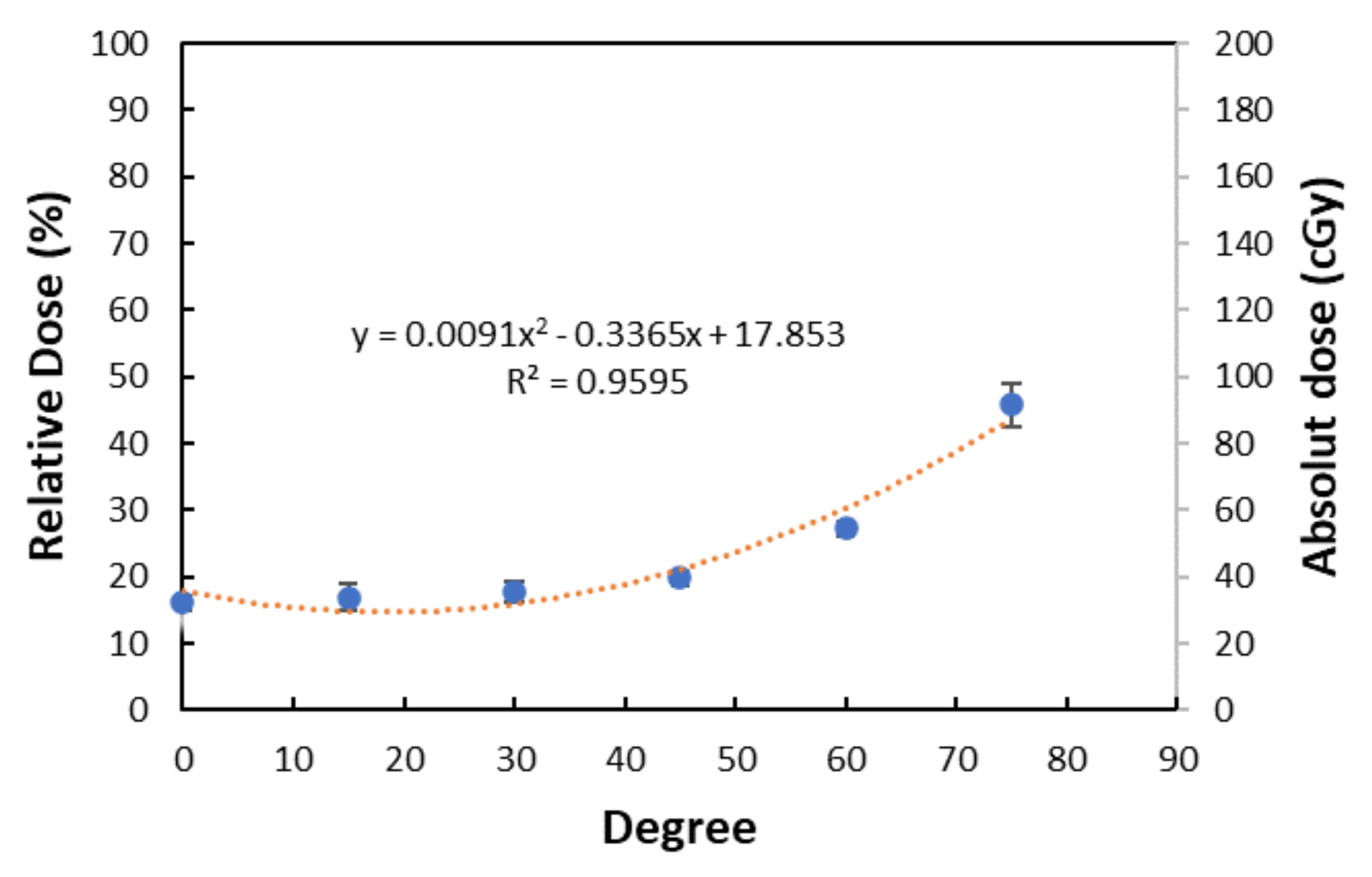

| Incident Angle (Degree) | Absolute Dose of Surface (cGy) | Relative Dose of Surface (%) |
|---|---|---|
| 0 | 32.27 ± 2.18 | 16.14 ± 1.09 |
| 15 | 33.91 ± 4.21 | 16.96 ± 2.15 |
| 30 | 35.67 ± 3.11 | 17.84 ± 1.56 |
| 45 | 39.65 ± 2.29 | 19.83 ± 1.15 |
| 60 | 54.53 ± 2.18 | 27.27 ± 1.09 |
| 75 | 91.51 ± 6.35 | 45.76 ± 3.18 |
| Layer(s) of Accessory | Measuring Point | Surface Dose (cGy) | Dose at 1 cm Depth (cGy) | PSDR1cm (%) | Incident Angle (Degree) |
|---|---|---|---|---|---|
| M1 | 92.32 ± 3.97 | 210.2 | 43.92 | 58.5 | |
| 1-layer | M2 | 91.23 ± 1.63 | 202.3 | 45.10 | 44.4 |
| (small) | L1 | 102.26 ± 11.61 | 217.6 | 46.99 | 80.4 |
| L2 | 106.84 ± 8.37 | 214.5 | 49.81 | 56.5 | |
| M1 | 92.15 ± 0.99 | 217.1 | 42.45 | 46.6 | |
| M2 | 83.63 ± 3.18 | 208.4 | 40.13 | 26.5 | |
| 2-layer | M3 | 82.50 ± 3.93 | 207.6 | 39.74 | 5.0 |
| (moderate) | L1 | 109.76 ± 7.79 | 222.1 | 49.42 | 79.8 |
| L2 | 94.90 ± 9.85 | 219.7 | 43.20 | 51.3 | |
| L3 | 92.27 ± 9.99 | 209.4 | 44.07 | 44.0 | |
| M1 | 95.38 ± 4.50 | 208.5 | 45.75 | 58.5 | |
| M2 | 85.14 ± 5.16 | 203.6 | 41.82 | 32.8 | |
| M3 | 78.26 ± 4.31 | 195.5 | 40.03 | 20.3 | |
| 3-layer | M4 | 74.12 ± 5.25 | 190.3 | 38.95 | 8.6 |
| (big) | L1 | 110.72 ± 3.47 | 217.0 | 51.02 | 79.3 |
| L2 | 96.02 ± 3.90 | 212.2 | 45.25 | 64.3 | |
| L3 | 83.19 ± 5.99 | 205.6 | 40.46 | 40.8 | |
| L4 | 80.93 ± 5.90 | 199.6 | 40.55 | 34.5 |
| Layer(s) of Accessory | Measuring Point | Surface Dose (cGy) | Dose at 1 cm Depth (cGy) | PSDR1cm (%) | Incident Angle (Degree) |
|---|---|---|---|---|---|
| S1 | 111.71 ± 10.37 | 212.9 | 52.4 | 73.6 | |
| 1-layer | S2 | 114.25 ± 6.09 | 214.7 | 53.3 | 71.6 |
| I1 | 102.26 ± 11.61 | 217.4 | 50.3 | 72.7 | |
| I2 | 114.20 ± 4.57 | 220.1 | 51.9 | 73.2 | |
| S1 | 99.87 ± 11.30 | 222.5 | 44.9 | 69.0 | |
| S2 | 106.78 ± 9.75 | 223.6 | 47.8 | 66.2 | |
| 2-layer | S3 | 105.05 ± 6.34 | 218.6 | 48.1 | 69.8 |
| I1 | 106.70 ± 2.98 | 223.7 | 47.7 | 71.2 | |
| I2 | 109.68 ± 7.37 | 224.5 | 48.9 | 67.2 | |
| I3 | 115.51 ± 7.03 | 225.3 | 51.3 | 57.2 | |
| S1 | 113.28 ± 5.37 | 214.8 | 52.7 | 72.1 | |
| S2 | 102.05 ± 2.57 | 214.5 | 47.6 | 74.2 | |
| S3 | 101.57 ± 6.23 | 211.7 | 48.0 | 73.9 | |
| 3-layer | S4 | 86.44 ± 13.86 | 193.6 | 44.6 | 61.1 |
| I1 | 113.24 ± 4.68 | 215.5 | 52.5 | 74.2 | |
| I2 | 113.66 ± 3.10 | 216.2 | 52.6 | 76.5 | |
| I3 | 122.18 ± 4.91 | 211.2 | 57.8 | 74.6 | |
| I4 | 107.56 ± 4.81 | 211.0 | 51.0 | 56.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yen, T.-Y.; Chuang, K.-C.; Fu, H.-M.; Feng, C.-J.; Lien, K.-Y.; Hsu, S.-M. Estimation of the Surface Dose in Breast Irradiation by the Beam Incident Angle and the 1 cm Depth Dose. J. Clin. Med. 2022, 11, 2154. https://doi.org/10.3390/jcm11082154
Yen T-Y, Chuang K-C, Fu H-M, Feng C-J, Lien K-Y, Hsu S-M. Estimation of the Surface Dose in Breast Irradiation by the Beam Incident Angle and the 1 cm Depth Dose. Journal of Clinical Medicine. 2022; 11(8):2154. https://doi.org/10.3390/jcm11082154
Chicago/Turabian StyleYen, Tsung-Yu, Kai-Cheng Chuang, Hsiao-Mei Fu, Chen-Ju Feng, Ke-Yu Lien, and Shih-Ming Hsu. 2022. "Estimation of the Surface Dose in Breast Irradiation by the Beam Incident Angle and the 1 cm Depth Dose" Journal of Clinical Medicine 11, no. 8: 2154. https://doi.org/10.3390/jcm11082154
APA StyleYen, T.-Y., Chuang, K.-C., Fu, H.-M., Feng, C.-J., Lien, K.-Y., & Hsu, S.-M. (2022). Estimation of the Surface Dose in Breast Irradiation by the Beam Incident Angle and the 1 cm Depth Dose. Journal of Clinical Medicine, 11(8), 2154. https://doi.org/10.3390/jcm11082154






