Dynamic Ultrasound Assessment of the Anterior Tibial Translation for Anterior Cruciate Ligament Tears Diagnostic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
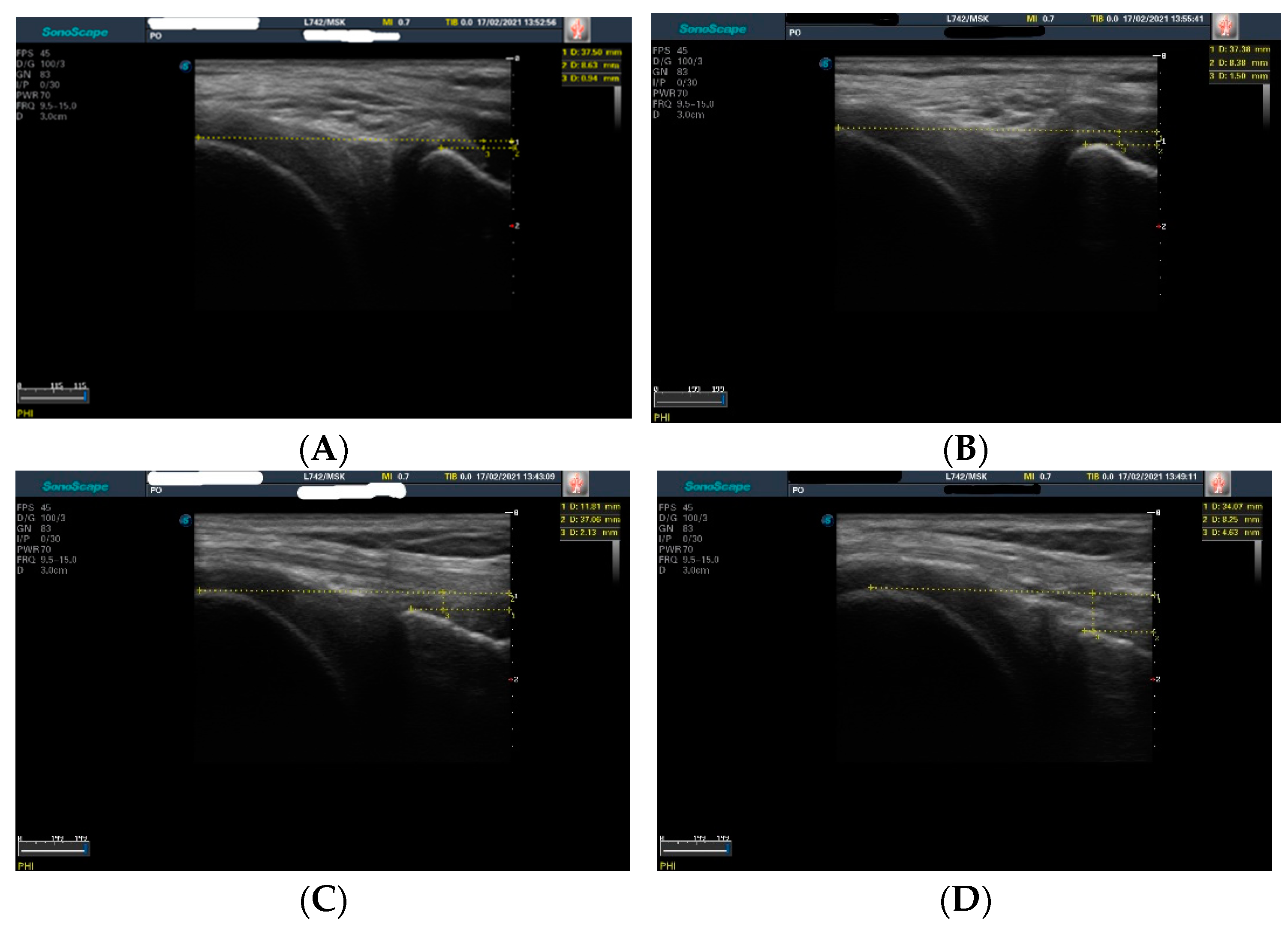
2.2. Assessments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abram, S.G.F.; Price, A.J.; Judge, A.; Beard, D.J. Anterior Cruciate Ligament (ACL) Reconstruction and Meniscal Repair Rates Have Both Increased in the Past 20 Years in England: Hospital Statistics from 1997 to 2017. Br. J. Sports Med. 2020, 54, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- The Romanian Arthroplasty Register. Summary Findings on ACL/PCL Reconstruction Register. Available online: https://www.rne.ro/rnemedia/download/lia_lip1.pdf (accessed on 15 December 2021).
- Shea, K.G.; Carey, J.L. Management of Anterior Cruciate Ligament Injuries: Evidence-Based Guideline. JAAOS-J. Am. Acad. Orthop. Surg. 2015, 23, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Lyu, J.; Liu, C.; Wu, J.; Xia, J.; Huang, G. A Modified Anterior Drawer Test for Anterior Cruciate Ligament Ruptures. J. Orthop. Surg. Res. 2021, 16, 260. [Google Scholar] [CrossRef]
- Crawford, R.; Walley, G.; Bridgman, S.; Maffulli, N. Magnetic Resonance Imaging versus Arthroscopy in the Diagnosis of Knee Pathology, Concentrating on Meniscal Lesions and ACL Tears: A Systematic Review. Br. Med. Bull. 2007, 84, 5–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Yun, S.J. Efficiency of Knee Ultrasound for Diagnosing Anterior Cruciate Ligament and Posterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis. Skelet. Radiol. 2019, 48, 1599–1610. [Google Scholar] [CrossRef]
- Ji, C.; Chen, Y.; Zhu, L.; Zhang, J. Arthroscopic Anterior Cruciate Ligament Injury in Clinical Treatment of Joint Complications and CT Observation. J. Healthc. Eng. 2021, 2021, 6667046. [Google Scholar] [CrossRef]
- Grassi, W.; Filippucci, E.; Farina, A.; Cervini, C. Sonographic Imaging of Tendons. Arthritis Rheum. 2000, 43, 969–976. [Google Scholar] [CrossRef]
- Ahmad, A.; Bandpei, M.A.M.; Gilani, S.A.; Munawar, A.; Ahmed, I.; Tanveer, F. Reliability of Musculoskeletal Ultrasound Imaging to Measure Supraspinatus Tendon Thickness in Healthy Subjects. J. Phys. Ther. Sci. 2017, 29, 1394–1398. [Google Scholar] [CrossRef] [Green Version]
- Gellhorn, A.C.; Carlson, M.J. Inter-Rater, Intra-Rater, and Inter-Machine Reliability of Quantitative Ultrasound Measurements of the Patellar Tendon. Ultrasound Med. Biol. 2013, 39, 791–796. [Google Scholar] [CrossRef]
- Gessl, I.; Balint, P.V.; Filippucci, E.; Keen, H.I.; Pineda, C.; Terslev, L.; Wildner, B.; D’Agostino, M.A.; Mandl, P. Structural Damage in Rheumatoid Arthritis Assessed by Musculoskeletal Ultrasound: A Systematic Literature Review by the Structural Joint Damage Task Force of the OMERACT Ultrasound Working Group. Semin. Arthritis Rheum. 2021, 51, 627–639. [Google Scholar] [CrossRef]
- del Baño-Aledo, M.E.; Martínez-Payá, J.J.; Ríos-Díaz, J.; Mejías-Suárez, S.; Serrano-Carmona, S.; de Groot-Ferrando, A. Ultrasound Measures of Tendon Thickness: Intra-Rater, Inter-Rater and Inter-Machine Reliability. Muscles Ligaments Tendons J. 2017, 7, 192–199. [Google Scholar] [CrossRef] [Green Version]
- Rossi, F.; Zaottini, F.; Picasso, R.; Martinoli, C.; Tagliafico, A.S. Ankle and Foot Ultrasound: Reliability of Side-to-Side Comparison of Small Anatomic Structures. J. Ultrasound Med. 2019, 38, 2143–2153. [Google Scholar] [CrossRef] [PubMed]
- Stracciolini, A.; Boucher, L.; Jackson, S.; Brown, N.; Magrini, D.; McKee-Proctor, M.; d’Hemecourt, P.; Delzell, P. Feasibility and Reliability of Musculoskeletal Ultrasound Measurement of the Medial Patellofemoral Ligament. Orthop. J. Sports Med. 2020, 8, 2325967120S00185. [Google Scholar] [CrossRef]
- Kandel, M.; Cattrysse, E.; de Maeseneer, M.; Lenchik, L.; Paantjens, M.; Leeuw, M. Inter-Rater Reliability of an Ultrasound Protocol to Evaluate the Anterolateral Ligament of the Knee. J. Ultrason. 2019, 19, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, H.; Dong, F.; Li, B.; Wei, Z.; Peng, Q.; Dong, D.; Li, M.; Xu, J. The Role of Ultrasonography in the Diagnosis of Anterior Cruciate Ligament Injury: A Systematic Review and Meta-Analysis. Eur. J. Sport Sci. 2018, 18, 579–586. [Google Scholar] [CrossRef]
- Poboży, T.; Kielar, M. A Review of Ultrasonographic Methods for the Assessment of the Anterior Cruciate Ligament in Patients with Knee Instability—Diagnostics Using a Posterior Approach. J. Ultrason. 2016, 16, 288–295. [Google Scholar] [CrossRef]
- Schwarz, W.; Hagelstein, J.; Minholz, R.; Schierlinger, M.; Danz, B.; Gerngroß, H. Manuelle Sonometrie Des KniegelenksEine Praxisnahe Methode Zur Diagnostik Der Frischen Ruptur Des Vorderen Kreuzbandes. Der Unfallchirurg 1997, 100, 280–285. [Google Scholar] [CrossRef]
- Palm, H.-G.; Bergenthal, G.; Ehry, P.; Schwarz, W.; Schmidt, R.; Friemert, B. Functional Ultrasonography in the Diagnosis of Acute Anterior Cruciate Ligament Injuries: A Field Study. Knee 2009, 16, 441–446. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Atkinson, G.; Nevill, A. Statistical Methods for Assssing Measurement Error (Reliability) in Variables Relevant to Sports Medicine. Sports Med. 1998, 26, 217–238. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [PubMed]
- Hyong, I.H.; Kim, J.H. Test of Intrarater and Interrater Reliability for the Star Excursion Balance Test. J. Phys. Ther. Sci. 2014, 26, 1139–1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Yi, P.H.; Curry, E.J.; Murakami, A.M. Ultrasonography as a Diagnostic, Therapeutic, and Research Tool in Orthopaedic Surgery. JAAOS-J. Am. Acad. Orthop. Surg. 2018, 26, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Özçakar, L.; Kara, M.; Chang, K.-V.; Lew, H.L.; Franchignoni, F. Musculoskeletal Ultrasound Liberating Physical and Rehabilitation Medicine: A Reinforcement for “Runners,” a Reminder for “Walkers” and the Last Call for “Couch Potatoes”. Am. J. Phys. Med. Rehabil. 2018, 97, e73–e74. [Google Scholar] [CrossRef]
- Wojtys, E.M.; Wylie, B.B.; Huston, L.J. The Effects of Muscle Fatigue on Neuromuscular Function and Anterior Tibial Translation in Healthy Knees. Am. J. Sports Med. 1996, 24, 615–621. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, A.; Kumar, S.; Kumar, P. Functional Ultrasonography in Diagnosing Anterior Cruciate Ligament Injury as Compared to Magnetic Resonance Imaging. Indian J. Orthop. 2018, 52, 638–644. [Google Scholar] [CrossRef]
- Gebhard, F.; Authenrieth, M.; Strecker, W.; Kinzl, L.; Hehl, G. Ultrasound Evaluation of Gravity Induced Anterior Drawer Following Anterior Cruciate Ligament Lesion. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 166–172. [Google Scholar] [CrossRef]
- Teng, P.S.P.; Leong, K.F.; Yi Xian Phua, P.; Kong, P.W. An Exploratory Study of the Use of Ultrasound in the Measurement of Anterior Tibial Translation under Gastrocnemius Muscle Stimulation. Res. Sports Med. 2021, 29, 103–115. [Google Scholar] [CrossRef]
- Wu, W.-T.; Lee, T.-M.; Mezian, K.; Naňka, O.; Chang, K.-V.; Özçakar, L. Ultrasound Imaging of the Anterior Cruciate Ligament: A Pictorial Essay and Narrative Review. Ultrasound Med. Biol. 2021, 48, 377–396. [Google Scholar] [CrossRef]
- Grzelak, P.; Podgórski, M.T.; Stefańczyk, L.; Domżalski, M. Ultrasonographic Test for Complete Anterior Cruciate Ligament Injury. Indian J. Orthop. 2015, 49, 143–149. [Google Scholar] [CrossRef] [PubMed]


| Injured Knee | p * | Uninjured Knee | p ** | |
|---|---|---|---|---|
| Anterior tibial translation (D2 − D1), mm (mean ± SD) | 3.34 ± 1.48 | 0.0002 | 0.86 ± 0.78 | 0.01 |
| Anterior tibial translation (D2 − D1) − retest, mm (mean ± SD) | 3.66 ± 1.64 | 0.95 ± 0.78 |
| ICC3,1 | 95%CI | SEM | SDC95 | |
|---|---|---|---|---|
| D1 injured knee | 0.99 | 0.997–0.999 | 0.23 | 0.63 |
| D2 injured knee | 0.99 | 0.98–0.99 | 0.31 | 0.85 |
| D1 uninjured knee | 0.99 | 0.991–0.998 | 0.08 | 0.22 |
| D2 uninjured knee | 0.98 | 0.973–0.995 | 0.18 | 0.49 |
| ΔD | 0.97 | 0.945–0.99 | 0.22 | 0.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoianov, A.G.; Pătrașcu, J.M.; Hogea, B.G.; Andor, B.; Mișcă, L.C.; Florescu, S.; Onofrei, R.R.; Pătrașcu, J.M., Jr. Dynamic Ultrasound Assessment of the Anterior Tibial Translation for Anterior Cruciate Ligament Tears Diagnostic. J. Clin. Med. 2022, 11, 2152. https://doi.org/10.3390/jcm11082152
Stoianov AG, Pătrașcu JM, Hogea BG, Andor B, Mișcă LC, Florescu S, Onofrei RR, Pătrașcu JM Jr. Dynamic Ultrasound Assessment of the Anterior Tibial Translation for Anterior Cruciate Ligament Tears Diagnostic. Journal of Clinical Medicine. 2022; 11(8):2152. https://doi.org/10.3390/jcm11082152
Chicago/Turabian StyleStoianov, Anca Gabriela, Jenel Marian Pătrașcu, Bogdan Gheorghe Hogea, Bogdan Andor, Liviu Coriolan Mișcă, Sorin Florescu, Roxana Ramona Onofrei, and Jenel Marian Pătrașcu, Jr. 2022. "Dynamic Ultrasound Assessment of the Anterior Tibial Translation for Anterior Cruciate Ligament Tears Diagnostic" Journal of Clinical Medicine 11, no. 8: 2152. https://doi.org/10.3390/jcm11082152
APA StyleStoianov, A. G., Pătrașcu, J. M., Hogea, B. G., Andor, B., Mișcă, L. C., Florescu, S., Onofrei, R. R., & Pătrașcu, J. M., Jr. (2022). Dynamic Ultrasound Assessment of the Anterior Tibial Translation for Anterior Cruciate Ligament Tears Diagnostic. Journal of Clinical Medicine, 11(8), 2152. https://doi.org/10.3390/jcm11082152







