COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
2.4. Materials
2.5. The 7-Day Self-Help Protocol
2.6. The Secret Garden Video
2.7. Procedure
3. Results
3.1. Demographics
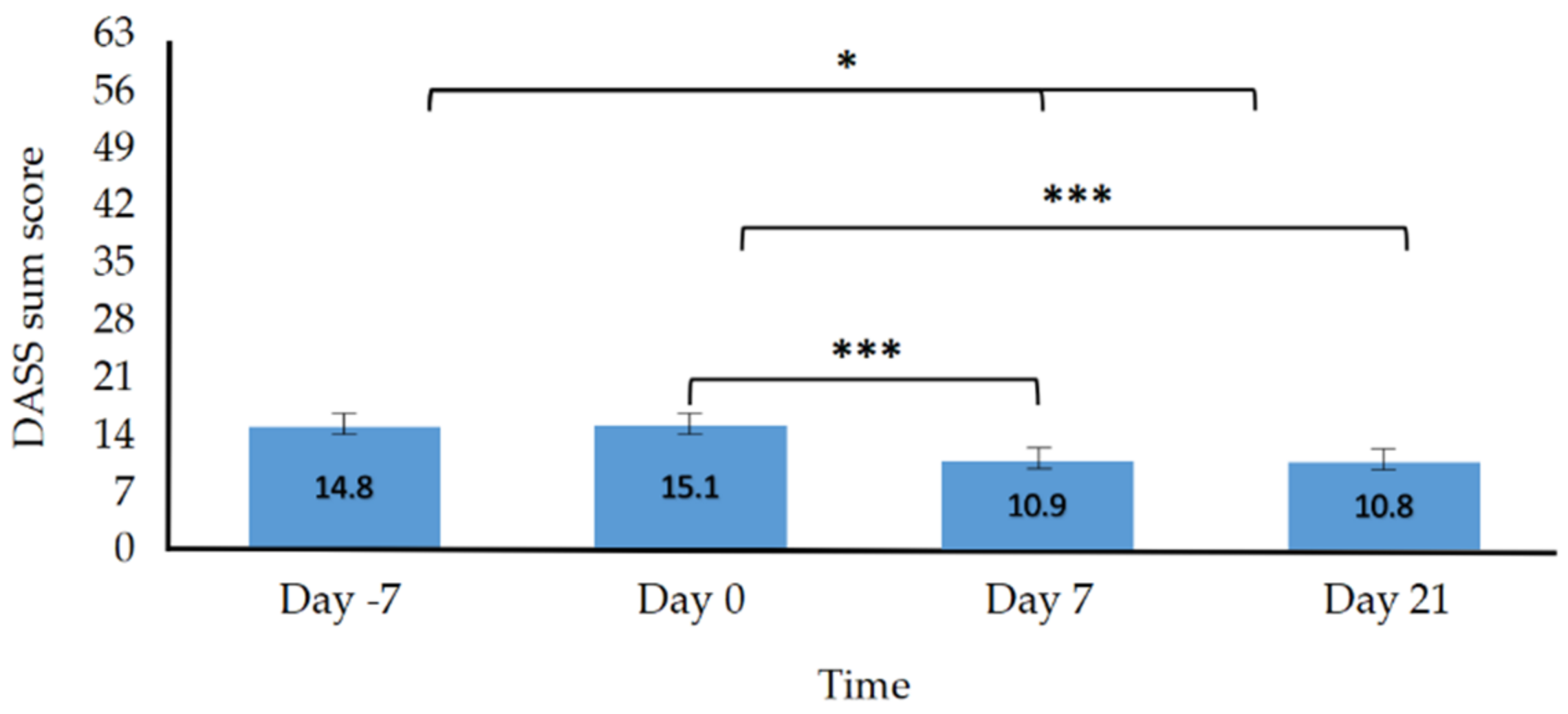
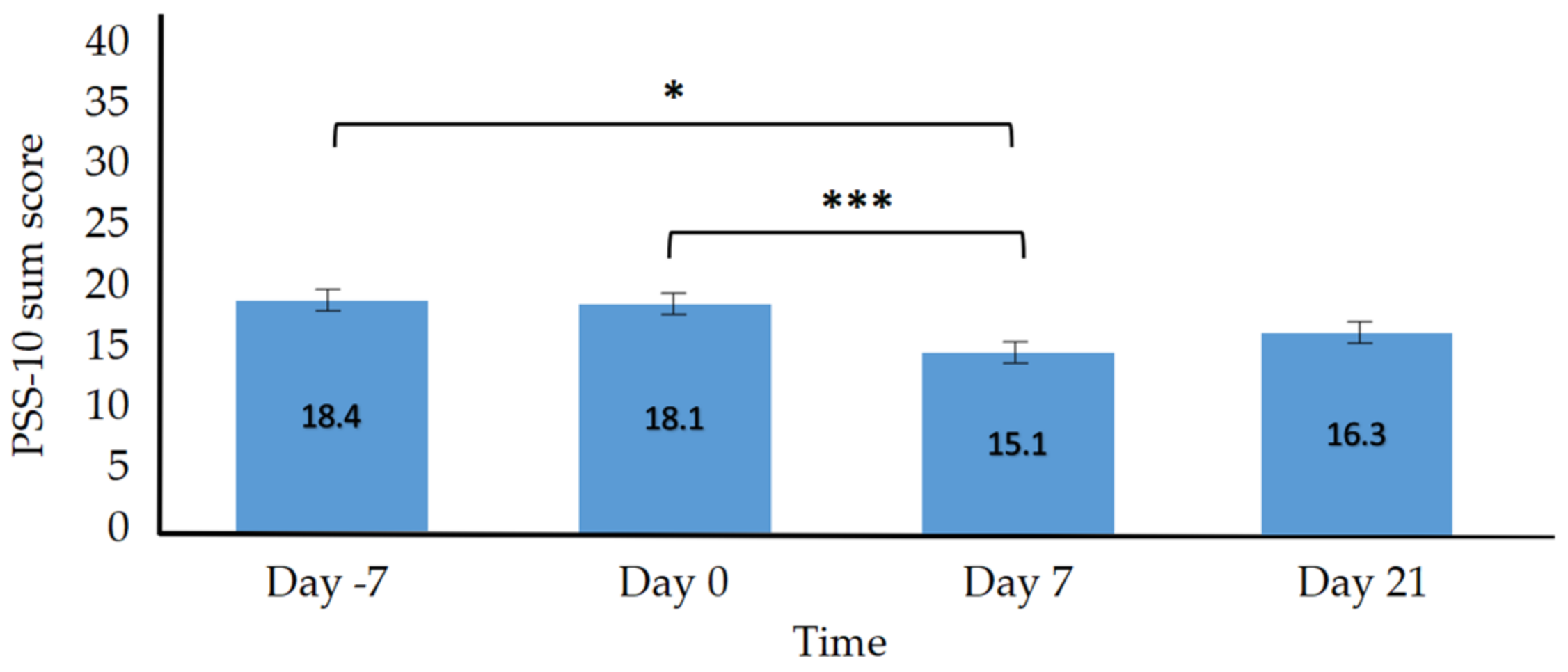
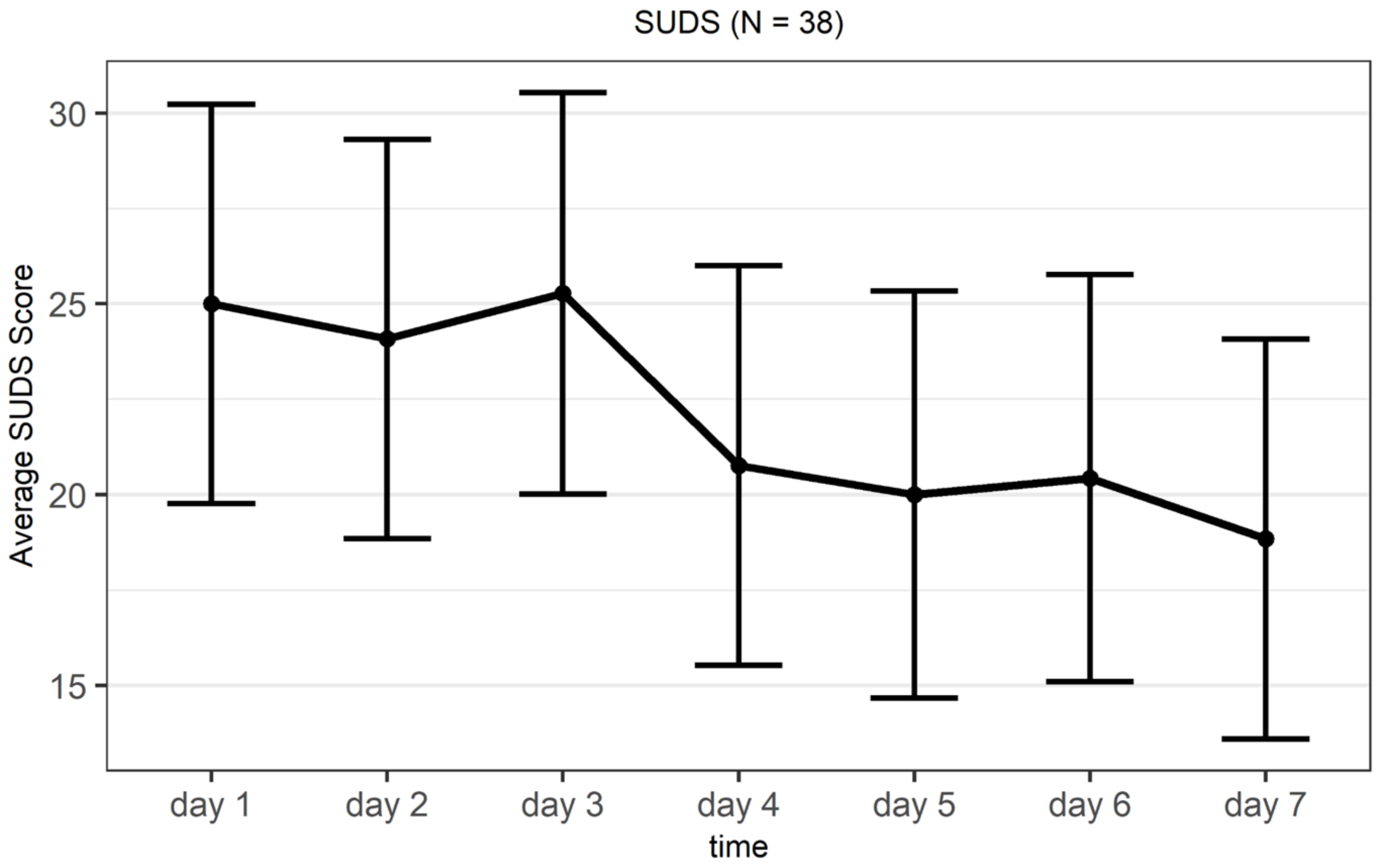
3.2. Hypothesis Testing
4. Discussion
4.1. Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Marital Status | N (Male) | N (Female) | N (Total) |
|---|---|---|---|
| Divorced | 0 (0.00%) | 3 (10.71%) | 3 (7.89%) |
| Married | 6 (60.00%) | 7 (25.00%) | 13 (34.21%) |
| Separated | 0 (0.00%) | 1 (3.57%) | 1 (2.63%) |
| Single | 4 (40.00%) | 17 (60.71%) | 21 (55.26%) |
| Total | 10 (100%) | 28 (100%) | 38 (100%) |
| Employment Status | |||
| Office employee | 1 (10.00%) | 4 (14.29%) | 5 (13.16%) |
| Pensioners | 1 (10.00%) | 2 (7.14%) | 3 (7.89%) |
| Student | 0 (0.00%) | 6 (21.43%) | 6 (15.79%) |
| Unemployed | 0 (0.00%) | 1 (3.54%) | 1 (2.63%) |
| Worker | 8 (80.00%) | 15 (53.57%) | 23 (60.53%) |
| Total | 10 (100%) | 28 (100%) | 38 (100%) |
| State | |||
| Berlin | 0 (0.00%) | 3 (11.11%) | 3 (8.11%) |
| Baden-Wuerttemberg | 0 (0.00%) | 0 (0.00%) | 2 (5.41%) |
| Bavaria | 2 (20.00%) | 1 (3.78%) | 1 (2.70%) |
| Hesse | 0 (0.00%) | 1 (3.78%) | 2 (5.41%) |
| Hamburg | 1 (10.00%) | 2 (7.44%) | 4 (10.81%) |
| Lower Saxony | 2 (20.00%) | 15 (50.56%) | 19 (51.35%) |
| North Rhine Westphalia | 4 (40.00%) | 1 (3.78%) | 1 (2.70%) |
| Rhineland-Palatinate | 0 (0.00%) | 0 (0.00%) | 1 (2.70%) |
| Schleswig-Holstein | 1 (10.00%) | 4 (14.81%) | 4 (10.81%) |
| Total | 10 (100%) | 27 (100%) | 37 (100%) |
| Known Disorder | |||
| No | 10 (100%) | 23 (82.14%) | 33 (86.84%) |
| Yes | 0 (0.00%) | 5 (17.86%) | 5 (13.16%) |
| Total | 10 (100%) | 28 (100%) | 38 (100%) |
| Type of Disorder | |||
| Depression | 0 (0.00%) | 2 (100%) | 2 (5.26%) |
| Anxiety | 0 (0.00%) | 2 (100%) | 2 (5.26%) |
| Substance Addiction | 0 (0.00%) | 1 (100%) | 1 (2.63%) |
| Contrasts | Estimate | p-Value | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
| Depression | Day −7 | Day 0 | −0.26 | 1.00 | −2.35 | Inf |
| Day 7 | 2.47 * | 0.03 | 0.02 | Inf | ||
| Day 21 | 3.11 * | 0.00 | 0.63 | Inf | ||
| Day 0 | Day 7 | 2.73 * | 0.01 | 0.35 | Inf | |
| Day 21 | 3.69 * | 0.00 | 0.99 | Inf | ||
| Day 7 | Day 21 | 0.63 | 1.00 | −1.82 | Inf | |
| Anxiety | Day −7 | Day 0 | 0.00 | 1.00 | −1.38 | Inf |
| Day 7 | 1.47 | 0.08 | −0.29 | Inf | ||
| Day 21 | 2.21 * | 0.00 | 0.61 | Inf | ||
| Day 0 | Day 7 | 1.47 | 0.04 | −0.12 | Inf | |
| Day 21 | 2.21 * | 0.00 | 0.61 | Inf | ||
| Day 7 | Day 21 | 0.74 | 0.42 | −0.62 | Inf | |
| Stress | Day −7 | Day 0 | −0.42 | 1.00 | −3.01 | Inf |
| Day 7 | 3.79 * | 0.01 | 0.63 | Inf | ||
| Day 21 | 2.68 | 0.13 | −0.91 | Inf | ||
| Day 0 | Day 7 | 4.21 * | 0.00 | 1.32 | Inf | |
| Day 21 | 3.11 * | 0.02 | 0.17 | Inf | ||
| Day 7 | Day 21 | −1.11 | 1.00 | −4.45 | Inf |
| Contrasts | Estimate | p-Value | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
| Rest/refresh | Day 1 | Day 7 | −0.34 | 0.078 | −Inf | 0.06 |
| Energized | Day 1 | Day 7 | −0.39 | 0.027 * | −Inf | −0.06 |
| Physical Relaxation | Day 1 | Day 7 | −0.14 | 0.197 | −Inf | 0.14 |
| At Ease/Peace | Day 1 | Day 7 | −0.24 | 0.059 | −Inf | 0.01 |
| Joy | Day 1 | Day 7 | −0.25 | 0.066 | −Inf | 0.02 |
| Mental Quiet | Day 1 | Day 7 | −0.39 | 0.014 * | −Inf | −0.1 |
| Awareness | Day 1 | Day 7 | −0.34 | 0.057 | −Inf | 0.01 |
| Somatic Stress | Day 1 | Day 7 | −0.05 | 0.661 | −0.27 | Inf |
| Emotional Stress | Day 1 | Day 7 | 0.02 | 0.445 | −0.24 | Inf |
| Cognitive Stress | Day 1 | Day 7 | −0.25 | 0.93 | −0.54 | Inf |
References
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Brown, E.G.; Gallagher, S.; Creaven, A.M. Loneliness and acute stress reactivity: A systematic review of psychophysiological studies. Psychophysiology 2018, 55, e13031. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Cacioppo, S.; Capitanio, J.P.; Cole, S.W. The neuroendocrinology of social isolation. Annu. Rev. Psychol. 2015, 66, 733–767. [Google Scholar] [CrossRef] [Green Version]
- Grewen, K.M.; Anderson, B.J.; Girdler, S.S.; Light, K.C. Warm partner contact is related to lower cardiovascular reactivity. Behav. Med. 2003, 29, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Steptoe, A.; Owen, N.; Kunz-Ebrecht, S.R.; Brydon, L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology 2004, 29, 593–611. [Google Scholar] [CrossRef]
- Gopal, A.; Sharma, A.J.; Subramanyam, M.A. Dynamics of psychological responses to COVID-19 in India: A longitudinal study. PLoS ONE 2020, 15, e0240650. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bernardelli, L.; Browning, M.H.; Castelnuovo, G.; Cavedoni, S.; Chirico, A.; Cipresso, P.; de Paula, D.M.B.; Di Lernia, D.; Fernandez-Alvarez, J.; et al. COVID feel good—An easy self-help virtual reality protocol to overcome the psychological burden of coronavirus. Front. Psychiatry 2020, 11, 996. [Google Scholar] [CrossRef] [PubMed]
- Slavich, G.M.; Shields, G.S. Assessing lifetime stress exposure using the Stress and Adversity Inventory for Adults (Adult STRAIN): An overview and initial validation. Psychosom. Med. 2018, 80, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiely, K.M.; Leach, L.S.; Olesen, S.C.; Butterworth, P. How financial hardship is associated with the onset of mental health problems over time. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 909–918. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Su, M. A preliminary assessment of the impact of COVID-19 on environment—A case study of China. Sci. Total Environ. 2020, 728, 138915. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Ozamiz-Etxebarria, N.; Idoiaga Mondragon, N.; Dosil Santamaría, M.; Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in Northern Spain. Front. Psychol. 2020, 11, 1491. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Rospleszcz, S.; Greiser, K.H.; Dallavalle, M.; Berger, K. The Impact of the COVID-19 Pandemic on Self-Reported Health: Early Evidence from the German National Cohort. Dtsch. Ärzteblatt Int. 2020, 117, 861. [Google Scholar] [CrossRef]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Mascarell Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, 10, e01745. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, L.T.; Cohen, A.K.; Dull, B.; Castro, E.M.; Yazdani, N. “Constant stress has become the new normal”: Stress and anxiety inequalities among US College students in the time of COVID-19. J. Adolesc. Health 2021, 68, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Wei, N.; Huang, B.-C.; Lu, S.-J.; Hu, J.-B.; Zhou, X.-Y.; Hu, C.-C.; Chen, J.-K.; Huang, J.-W.; Li, S.-G.; Wang, Z.; et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J. Zhejiang Univ. Sci. B 2020, 21, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Rauschenberg, C.; Schick, A.; Hirjak, D.; Seidler, A.; Paetzold, I.; Apfelbacher, C.; Riedel-Heller, S.G.; Reininghaus, U. Evidence synthesis of digital interventions to mitigate the negative impact of the COVID-19 pandemic on public mental health: Rapid meta-review. J. Med. Internet Res. 2021, 23, e23365. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, P.; Kowshik, C.S.; Manjunath, M.; Shettar, M. COVID 19: Impact of lock-down on mental health and tips to overcome. Asian J. Psychiatry 2020, 51, 102088. [Google Scholar] [CrossRef]
- Dan, Z. China adopts non-contact free consultation to help the public cope with the psychological pressure caused by new coronavirus pneumonia. Asian J. Psychiatry 2020, 52, 119–138. [Google Scholar] [CrossRef] [PubMed]
- Losada-Baltar, A.; Martínez-Huertas, J.Á.; Jiménez-Gonzalo, L.; del Sequeros Pedroso-Chaparro, M.; Gallego-Alberto, L.; Fernandes-Pires, J.; Márquez-González, M. Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 4, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P. Introducing compassion-focused therapy. Adv. Psychiatr. Treat. 2009, 15, 199–208. [Google Scholar] [CrossRef] [Green Version]
- Craig, C.; Hiskey, S.; Spector, A. Compassion focused therapy: A systematic review of its effectiveness and acceptability in clinical populations. Expert Rev. Neurother. 2020, 20, 385–400. [Google Scholar] [CrossRef]
- Frostadottir, A.D.; Dorjee, D. Effects of Mindfulness Based Cognitive Therapy (MBCT) and Compassion Focused Therapy (CFT) on Symptom Change, Mindfulness, Self-Compassion, and Rumination in Clients with Depression, Anxiety, and Stress. Front. Psychol. 2019, 10, 1099. [Google Scholar] [CrossRef] [PubMed]
- Leaviss, J.; Uttley, L. Psychotherapeutic benefits of compassion-focused therapy: An early systematic review. Psychol. Med. 2015, 45, 927–945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bratman, G.N.; Hamilton, J.P.; Daily, G.C. The impacts of nature experience on human cognitive function and mental health. Ann. N. Y. Acad. Sci. 2012, 1249, 118–136. [Google Scholar] [CrossRef]
- Weng, P.Y.; Chiang, Y.C. Psychological restoration through indoor and outdoor leisure activities. J. Leis. Res. 2014, 46, 203–217. [Google Scholar] [CrossRef]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with Nature Improves Cognition and Affect for Individuals with Depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korpela, K.M.; Stengård, E.; Jussila, P. Nature Walks as a Part of Therapeutic Intervention for Depression. Ecopsychology 2016, 8, 8–15. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Mimnaugh, K.J.; van Riper, C.J.; Laurent, H.K.; LaValle, S.M. Can Simulated Nature Support Mental Health? Comparing Short, Single-Doses of 360-Degree Nature Videos in Virtual Reality with the Outdoors. Front. Psychol. 2020, 10, 2667. [Google Scholar] [CrossRef] [Green Version]
- White, M.P.; Yeo, N.L.; Vassiljev, P.; Lundstedt, R.; Wallergård, M.; Albin, M.; Lõhmus, M. A prescription for “nature”—The potential of using virtual nature in therapeutics. Neuropsychiatr. Dis. Treat. 2018, 14, 3001–3013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calogiuri, G.; Litleskare, S.; Fagerheim, K.A.; Rydgren, T.L.; Brambilla, E.; Thurston, M. Experiencing Nature through Immersive Virtual Environments: Environmental Perceptions, Physical Engagement, and Affective Responses during a Simulated Nature Walk. Front. Psychol. 2017, 8, 2321. [Google Scholar] [CrossRef] [Green Version]
- Diemer, J.; Alpers, G.W.; Peperkorn, H.M.; Shiban, Y.; Mühlberger, A. The impact of perception and presence on emotional reactions: A review of research in virtual reality. Front. Psychol. 2015, 6, 26. [Google Scholar] [CrossRef] [Green Version]
- Riva, G.; Wiederhold, B.K.; Mantovani, F. Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 82–96. [Google Scholar] [CrossRef] [PubMed]
- Winch, G. Emotional First Aid: Healing Rejection, Guilt, Failure, and Other Everyday Hurts; Penguin: New York, NY, USA, 2013. [Google Scholar]
- Nitschke, J.P.; Forbes, P.A.G.; Ali, N.; Cutler, J.; Apps, M.A.J.; Lockwood, P.L.; Lamm, C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021, 26, 553–569. [Google Scholar] [CrossRef]
- Sibley, C.G.; Greaves, L.M.; Satherley, N.; Wilson, M.S.; Overall, N.C.; Lee, C.H.J.; Milojev, P.; Bulbulia, J.; Osborne, D.; Milfont, T.L.; et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 2020, 75, 618–630. [Google Scholar] [CrossRef] [PubMed]
- Bendau, A.; Plag, J.; Kunas, S.; Wyka, S.; Ströhle, A.; Petzold, M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2021, 11, e01964. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Mergel, E.; Schützwohl, M. A longitudinal study on the COVID-19 pandemic and its divergent effects on social participation and mental health across different study groups with and without mental disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 56, 1459–1468. [Google Scholar] [CrossRef] [PubMed]
- Park, C.L.; Finkelstein-Fox, L.; Russell, B.S.; Fendrich, M.; Hutchison, M.; Becker, J. Americans’ distress early in the COVID-19 pandemic: Protective resources and coping strategies. Psychol. Trauma Theory Res. Pract. Policy 2021, 13, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Tham, S.-G.; Ibrahim, S.; Hunt, I.M.; Kapur, N.; Gooding, P. Examining the mechanisms by which adverse life events affect having a history of self-harm, and the protective effect of social support. J. Affect. Disord. 2020, 263, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Saricali, M.; Satici, S.A.; Satici, B.; Gocet-Tekin, E.; Griffiths, M.D. Fear of COVID-19, Mindfulness, Humor, and Hopelessness: A Multiple Mediation Analysis. Int. J. Ment. Health Addict. 2020, 57, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bernardelli, L.; Castelnuovo, G.; Di Lernia, D.; Tuena, C.; Clementi, A.; Pedroli, E.; Malighetti, C.; Sforza, F.; Wiederhold, B.K.; et al. A Virtual Reality-Based Self-Help Intervention for Dealing with the Psychological Distress Associated with the COVID-19 Lockdown: An Effectiveness Studywith a Two-Week Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 8188. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Schneider, E.E.; Schönfelder, S.S.; Domke-Wolf, M.; Wessa, M. Measuring stress in clinical and nonclinical subjects using a German adaptation of the Perceived Stress Scale. Int. J. Clin. Health Psychol. 2020, 20, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Nilges, P.; Essau, C. Die Depressions-Angst-Stress-Skalen. Schmerz 2015, 29, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Nilges, P.; Essau, C. DASS. Depressions-Angst-Stress-Skalen—deutschsprachige Kurzfassung [Verfahrensdokumentation und Fragebogen mit Auswertung]. In Leibniz-Institut für Psychologie (ZPID) (Hrsg.), Open Test Archive; ZPID: Trier, Germany, 2021. [Google Scholar] [CrossRef]
- Lee, R.M.; Robbins, S.B. Measuring belongingness: The social connectedness and the social assurance scales. J. Couns. Psychol. 1995, 42, 232–241. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A. Manual for the Beck Hopelessness Scale; Psychological Corporation: San Antonio, TX, USA, 1988. [Google Scholar]
- Kliem, S.; Brähler, E. Beck-Hoffnungslosigkeits-Skala (BHS): Deutsche Fassung; Pearson: Frankfurt am Main, Germany, 2016. [Google Scholar]
- Kliem, S.; Lohmann, A.; Mößle, T.; Brähler, E. Psychometric properties and measurement invariance of the Beck hopelessness scale (BHS): Results from a German representative population sample. BMC Psychiatry 2018, 18, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 67, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, J.C. Smith Relaxation States Inventory 3 (SRSI3); Lulu Press: Raleigh, NC, USA, 2010. [Google Scholar]
- McCabe, R.E. Subjective units of distress scale. J. Phobias. Psychol. Irrational. Fear 2015, 18, 361. [Google Scholar]
- Riva, G.; Baños, R.M.; Botella, C.; Mantovani, F.; Gaggioli, A. Transforming Experience: The Potential of Augmented Reality and Virtual Reality for Enhancing Personal and Clinical Change. Front. Psychiatry 2016, 7, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Rozental, A.; Carlbring, P. Negative Effekte und Auswirkungen von Psychotherapie: Version 32 Items Adult (German). 2017. Available online: http://neqscale.com/download/NEQ_German_20_Items_2019.pdf (accessed on 30 January 2022).
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Fischer, R.; Bortolini, T.; Karl, J.A.; Zilberberg, M.; Robinson, K.; Rabelo, A.; Gemal, L.; Wegerhoff, D.; Nguyễn, T.B.T.; Irving, B.; et al. Rapid review and meta-meta-analysis of self-guided interventions to address anxiety, depression, and stress during COVID-19 social distancing. Front. Psychol. 2020, 11, 2795. [Google Scholar] [CrossRef]
- Rackoff, G.N.; Fitzsimmons-Craft, E.E.; Taylor, C.B.; Eisenberg, D.; Wilfley, D.E.; Newman, M.G. A Randomized Controlled Trial of Internet-Based Self-Help for Stress During the COVID-19 Pandemic. J. Adolesc. Health 2022. [Google Scholar] [CrossRef]
- Charbonnier, E.; Trémolière, B.; Baussard, L.; Goncalves, A.; Lespiau, F.; Philippe, A.G.; Le Vigouroux, S. Effects of an online self-help intervention on university students’ mental health during COVID-19: A non-randomized controlled pilot study. Comput. Hum. Behav. Rep. 2022, 5, 100175. [Google Scholar] [CrossRef] [PubMed]
- Zabini, F.; Albanese, L.; Becheri, F.R.; Gavazzi, G.; Giganti, F.; Giovanelli, F.; Gronchi, G.; Guazzini, A.; Laurino, M.; Li, Q.; et al. Comparative study of the restorative effects of forest and urban videos during COVID-19 lockdown: Intrinsic and benchmark values. Int. J. Environ. Res. Public Health 2020, 17, 8011. [Google Scholar] [CrossRef] [PubMed]
- Imperatori, C.; Dakanalis, A.; Farina, B.; Pallavicini, F.; Colmegna, F.; Mantovani, F.; Clerici, M. Global storm of stress-related psychopathological symptoms: A brief overview on the usefulness of virtual reality in facing the mental health impact of COVID-19. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 782–788. [Google Scholar] [CrossRef]
- Orne, M.T. On the social psychology of the psychological experiment: With particular reference to demand characteristics and their implications. Am. Psychol. 1962, 17, 776–783. [Google Scholar] [CrossRef]
- Cuijpers, P.; Koole, S.; Van Dijke, A.; Roca, M.; Li, J.; Reynolds, C. Psychotherapy for subclinical depression: Meta-analysis. Br. J. Psychiatry 2014, 205, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Robert Koch Institut. Aktueller Lage-/Situationsbericht des RKI zu COVID-19; Robert Koch Institut: Berlin, Germany, 2021; Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Gesamt.html (accessed on 30 January 2022).
- Hövermann, A. Corona-Zweifel, Unzufriedenheit und Verschwörungsmythen: Erkenntnisse aus zwei Wellen der HBS-Erwerbspersonenbefragung 2020 zu Einstellungen zur Pandemie und den Politischen Schutzmaßnahmen; WSI Policy Brief No. 48; WSI: Düsseldorf, Germany, 2020. [Google Scholar]
- Liebig, S.; Buchinger, L.; Entringer, T.M.; Kühne, S. Ost-und Westdeutschland in der Corona-Krise: Nachwendegeneration im Osten erweist sich als resilient. DIW Wochenber. 2020, 87, 721–729. [Google Scholar] [CrossRef]
- Rosen, L.N.; Targum, S.D.; Terman, M.; Bryant, M.J.; Hoffman, H.; Kasper, S.F.; Hamovit, J.R.; Docherty, J.P.; Welch, B.; Rosenthal, N.E. Prevalence of seasonal affective disorder at four latitudes. Psychiatry Res. 1990, 31, 131–144. [Google Scholar] [CrossRef]
- Rosenthal, N.E. Winter Blues: Everything You Need to Know to Beat Seasonal Affective Disorder; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Vitman-Schorr, A.; Ayalon, L.; Tamir, S. The relationship between satisfaction with the accessibility of the living environment and depressive symptoms. J. Environ. Psychol. 2020, 72, 101527. [Google Scholar] [CrossRef]
- Daly, M.; Sutin, A.; Robinson, E. Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK Household Longitudinal Study. Psychol. Med. 2020, 212, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lal, S.; Adair, C.E. E-mental health: A rapid review of the literature. Psychiatr. Serv. 2014, 65, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Weightman, M. Digital psychotherapy as an effective and timely treatment option for depression and anxiety disorders: Implications for rural and remote practice. J. Int. Med. Res. 2020, 48, 0300060520928686. [Google Scholar] [CrossRef] [PubMed]

| Day 1: Fight rumination. Support to cope with stress, worries, and negative intrusive thoughts related to the COVID-19 pandemic through imagination exercises. |
| Day 2: Awaken self-esteem. Increase self-esteem by listing five aspects of one’s own character and personality that one appreciates. |
| Day 3: Awaken autobiographical memory. Aims at creating a stable representation of themselves over time, as well as increase intimacy and connectedness by sharing personal memories. |
| Day 4: Awaken sense of community. Aims at reducing the feeling of loneliness by focusing on the five most important people in one’s life. |
| Day 5: Awaken goals and dreams. Promote conscious self-regulation and self-organization of life goals by listing concrete goals, dreams, and aspirations. |
| Day 6: Boost empathy. Increase in empathy by attributing feelings to last significant interactions with the most significant people in one’s life. |
| Day 7: Plan change. Support a long-term psychological change by finding solutions for life dissatisfactions. |
| Primary Outcome Measures | Day −7 Mean (SD) | Day 0 Mean (SD) | Day 7 Mean (SD) | Day 21 Mean (SD) |
|---|---|---|---|---|
| DASS | 14.79 (8.44) | 15.13 (8.87) | 10.92 (8.01) | 10.79 (7.34) |
| PSS-10 | 18.39 (6.62) | 18.08 (6.83) | 15.11 (7.20) | 16.26 (6.92) |
| BHS | 4.84 (3.90) | 4.68 (4.27) | 3.92 (3.92) | 4.13 (4.32) |
| Secondary Outcome Measures | Day −7 Mean (SD) | Day 0 Mean (SD) | Day 7 Mean (SD) | Day 21 Mean (SD) |
| SCS | 35.84 (7.90) | 36.34 (9.26) | 38.79 (8.97) | 38.00 (9.38) |
| FCV-19S | 14.47 (4.30) | 13.34 (4.39) | 12.66 (5.27) | 11.87 (4.52) |
| Subscales | Day −7 Mean (SD) | Day 0 Mean (SD) | Day 7 Mean (SD) | Day 21 Mean (SD) |
|---|---|---|---|---|
| Depression | 9.16 (7.32) | 9.42 (7.23) | 6.68 (6.63) | 6.05 (5.72) |
| Anxiety | 4.95 (4.89) | 4.95 (5.34) | 3.47 (3.80) | 2.74 (2.99) |
| Stress | 15.47 (7.82) | 15.89 (7.89) | 11.68 (7.17) | 12.79 (7.61) |
| Contrasts | Estimate | p-Value | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
| DASS | Day −7 | Day 0 | −0.34 | 1.00 | −1.70 | Inf |
| Day 7 | 3.87 * | 0.05 | 2.07 | Inf | ||
| Day 21 | 4.00 * | 0.04 | 2.19 | Inf | ||
| Day 0 | Day 7 | 4.21 * | 0.00 | 2.61 | Inf | |
| Day 21 | 4.34 * | 0.00 | 2.81 | Inf | ||
| Day 7 | Day 21 | 0.13 | 1.00 | −1.68 | Inf | |
| PSS-10 | Day −7 | Day 0 | 0.34 | 1.00 | −0.98 | Inf |
| Day 7 | 3.29 * | 0.02 | 1.34 | Inf | ||
| Day 21 | 2.13 | 0.22 | 0.20 | Inf | ||
| Day 0 | Day 7 | 2.97 * | 0.00 | 1.54 | Inf | |
| Day 21 | 1.82 | 0.22 | 0.17 | Inf | ||
| Day 7 | Day 21 | −1.16 | 1.00 | −2.99 | Inf | |
| BHS | Day −7 | Day 0 | 0.16 | 1.00 | −0.27 | Inf |
| Day 7 | 0.92 | 0.06 | 0.29 | Inf | ||
| Day 21 | 0.71 | 0.38 | −0.06 | Inf | ||
| Day 0 | Day 7 | 0.76 | 0.09 | −0.19 | Inf | |
| Day 21 | 0.55 | 0.50 | −0.22 | Inf | ||
| Day 7 | Day 21 | −0.21 | 1.00 | −0.83 | Inf | |
| SCS | Day −7 | Day 0 | −0.50 | 1.00 | −Inf | 0.79 |
| Day 7 | −2.95 * | 0.01 | −Inf | −1.49 | ||
| Day 21 | −2.16 | 0.16 | −Inf | −0.32 | ||
| Day 0 | Day 7 | −2.45 * | 0.00 | −Inf | −1.44 | |
| Day 21 | −1.66 | 0.16 | −Inf | −0.24 | ||
| Day 7 | Day 21 | 0.79 | 1.00 | −Inf | 2.10 | |
| FCV-19S | Day −7 | Day 0 | 1.13 * | 0.02 | 0.50 | Inf |
| Day 7 | 1.82 * | 0.01 | 0.91 | Inf | ||
| Day 21 | 2.61 * | 0.00 | 1.74 | Inf | ||
| Day 0 | Day 7 | 0.68 | 0.43 | −0.08 | Inf | |
| Day 21 | 1.47 * | 0.01 | 0.67 | Inf | ||
| Day 7 | Day 21 | 0.79 | 0.30 | 0.01 | Inf |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meyer, M.L.; Kaesler, A.; Wolffgramm, S.; Perić, N.L.; Bunjaku, G.; Dickmann, L.; Serino, S.; Di Lernia, D.; Tuena, C.; Bernardelli, L.; et al. COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample. J. Clin. Med. 2022, 11, 2080. https://doi.org/10.3390/jcm11082080
Meyer ML, Kaesler A, Wolffgramm S, Perić NL, Bunjaku G, Dickmann L, Serino S, Di Lernia D, Tuena C, Bernardelli L, et al. COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample. Journal of Clinical Medicine. 2022; 11(8):2080. https://doi.org/10.3390/jcm11082080
Chicago/Turabian StyleMeyer, Marie Lisa, Arne Kaesler, Stefanie Wolffgramm, Nicolina Laura Perić, Gentian Bunjaku, Lilith Dickmann, Silvia Serino, Daniele Di Lernia, Cosimo Tuena, Luca Bernardelli, and et al. 2022. "COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample" Journal of Clinical Medicine 11, no. 8: 2080. https://doi.org/10.3390/jcm11082080
APA StyleMeyer, M. L., Kaesler, A., Wolffgramm, S., Perić, N. L., Bunjaku, G., Dickmann, L., Serino, S., Di Lernia, D., Tuena, C., Bernardelli, L., Pedroli, E., Wiederhold, B. K., Riva, G., & Shiban, Y. (2022). COVID Feel Good: Evaluation of a Self-Help Protocol to Overcome the Psychological Burden of the COVID-19 Pandemic in a German Sample. Journal of Clinical Medicine, 11(8), 2080. https://doi.org/10.3390/jcm11082080










