Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in Patients with Multiple Sclerosis: Factor Structure, Reliability, Correlates, and Discrimination
Abstract
1. Introduction
2. Materials and Methods
2.1. General Procedures
2.2. Participants
2.3. Questionnaires
2.3.1. Pittsburgh Sleep Quality Index (PSQI)
2.3.2. Multiple Sclerosis Impact Scale (MSIS-29)
2.4. Validation Procedure
2.5. Data Analysis and Statistics
2.6. PSQI Structure Procedure
3. Results
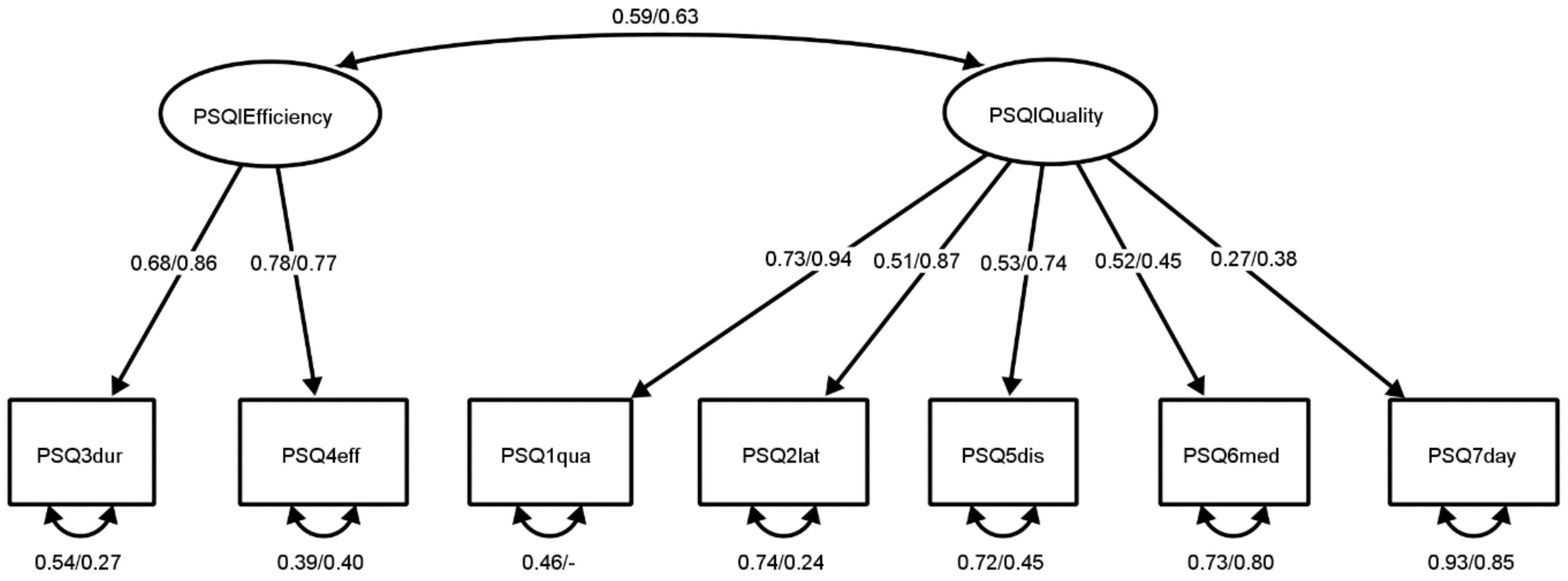
3.1. PSQI Structure
3.2. PSQI Reliability
3.3. PSQI Relations with Other Variables
3.4. PSQI Discrimination
| Variable | Mms (SDms) | Mcon (SDcon) | Levene’s Test F (p) | t (p) |
|---|---|---|---|---|
| PSQI global score | 7.36 (4.678) | 5.60 (3.100) | 29.74 (0.000) | 3.08 (0.002) |
| PSQI sleep quality | 5.65 (3.263) | 4.16 (2.096) | 21.68 (0.000) | 3.72 (0.000) |
| PSQI sleep efficiency | 1.96 (2.003) | 1.45 (1.500) | 14.56 (0.000) | 2.01 (0.046) |
| Present Research | Lobentanz et al. [31] | Ma et al. [32] | Pinar et al. [33] | |||||
|---|---|---|---|---|---|---|---|---|
| pwMS | Con | pwMS | Con | pwMS | Con | |||
| n | 388 | 991 | 231 | 265 | 50 | 50 | ||
| n | M | 7.00 (3.900) | 4.55 (3.710) | 8.90 (5.200) | 5.80 (4.800) | 7.90 (3.500) | 6.02 (3.220) | |
| (SD) | ||||||||
| M (SD) | ||||||||
| pwMS | 87 | 7.36 (4.678) | 0.996 | 0.000 ** | 0.052 | 0.041 * | 0.995 | 0.583 |
| Con | 134 | 5.60 (3.100) | 0.014 * | 0.090 | 0.000 ** | 1.000 | 0.015 * | 0.999 |
3.5. MS and PSQI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Howard, J.; Trevick, S.; Younger, D.S. Epidemiology of multiple sclerosis. Neurol. Clin. 2016, 34, 919–939. [Google Scholar] [CrossRef] [PubMed]
- Glaser, A.; Stahmann, A.; Meissner, T.; Flachenecker, P.; Horáková, D.; Zaratin, P.; Brichetto, G.; Pugliatti, M.; Rienhoff, O.; Vukusic, S.; et al. Multiple sclerosis registries in Europe—An updated mapping survey. Mult. Scler. Relat. Disord. 2019, 27, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Kotterba, S.; Neusser, T.; Norenberg, C.; Bussfeld, P.; Glaser, T.; Dörner, M.; Schürks, M. Sleep quality, daytime sleepiness, fatigue, and quality of life in patients with multiple sclerosis treated with interferon beta-1b: Results from a prospective observational cohort study. BMC Neurol. 2018, 18, 123. [Google Scholar] [CrossRef]
- Vitkova, M.; Gdovinova, Z.; Rosenberger, J.; Szilasiova, J.; Nagyová, I.; Mikula, P.; Krokavcova, M.; Groothoff, J.W.; van Dijk, J.P. Factors associated with poor sleep quality in patients with multiple sclerosis differ by disease duration. Disabil. Health J. 2014, 7, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Taphoorn, M.; Van Someren, E.; Snoek, F.; Strijers, R.L.M.; Swaab, D.; Visscher, F.; De Waal, L.P.; Polman, C.H. Fatigue, sleep disturbances and circadian rhythm in multiple sclerosis. J. Neurol. 1993, 240, 446–448. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Merlino, G.; Fratticci, L.; Lenchig, C.; Valente, M.; Cargnelutti, D.; Picello, M.; Serafini, A.; Dolso, P.; Gigli, G. Prevalence of ‘poor sleep’ among patients with multiple sclerosis: An independent predictor of mental and physical status. Sleep Med. 2009, 10, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Gavidia, R.; Dunietz, G.L.; Washnock-Schmid, E.; Romeo, A.R.; Hershner, S.; Chervin, R.D.; Braley, T.J. Validation of an obstructive sleep apnea symptom inventory in persons with multiple sclerosis. Mult. Scler. 2021, 28, 280–288. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193e213. [Google Scholar] [CrossRef]
- Curcio, G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurol. Sci. 2013, 34, 511–519. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Kirsteen Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef]
- Tsai, P.S.; Wang, S.Y.; Wang, M.Y.; Su, C.-T.; Yang, T.-T.; Huang, C.-J.; Fang, S.-C. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. 2005, 14, 1943–1952. [Google Scholar] [CrossRef]
- Bertolazi, A.N.; Fagondes, S.C.; Hoff, L.S.; Dartora, E.G.; Miozzo, I.C.D.S.; de Barba, M.E.F.; Barreto, S.S.M. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011, 12, 70–75. [Google Scholar] [CrossRef]
- Farrahi Moghaddam, J.; Nakhaee, N.; Sheibani, V.; Garrusi, B.; Amirkafi, A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath. 2012, 16, 79–82. [Google Scholar] [CrossRef]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012, 16, 803–812. [Google Scholar] [CrossRef]
- Kalcina Lusic, L.; Valic, M.; Pecotic, R.; Pavlinac Dodig, I.; Dogas, Z. Good and poor sleepers among OSA patients: Sleep quality and overnight polysomnography findings. Neurol. Sci. 2017, 38, 1299–1306. [Google Scholar] [CrossRef]
- Buratti, L.; Iacobucci, D.E.; Viticchi, G.; Falsetti, L.; Lattanzi, S.; Pulcini, A.; Silvestrini, M. Sleep quality can influence the outcome of patients with multiple sclerosis. Sleep Med. 2019, 58, 56–60. [Google Scholar] [CrossRef]
- Motolese, F.; Rossi, M.; Albergo, G.; Stelitano, D.; Villanova, M.; Di Lazzaro, V.; Capone, F. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front. Neurol. 2020, 11, 580507. [Google Scholar] [CrossRef]
- Rocchi, C.; Pulcini, A.; Vesprini, C.; Totaro, V.; Viticchi, G.; Falsetti, L.; Danni, M.C.; Bartolini, M.; Silvestrini, M.; Buratti, L. Sleep in multiple sclerosis patients treated with interferon beta: An actigraphic study. Neurol. Res. 2020, 42, 744–748. [Google Scholar] [CrossRef]
- Zhang, G.X.; Zhang, W.T.; Gao, S.S.; Zhao, R.Z.; Yu, W.J.; Izquierdo, G. Sleep disorders in patients with multiple sclerosis in Spain. Neurologia 2021, S0213-4853(21)00080-3. [Google Scholar] [CrossRef]
- Bøe Lunde, H.M.; Aae, T.F.; Indrevåg, W.; Aarseth, J.; Bjorvatn, B.; Myhr, K.-M.; Bø, L. Poor sleep in patients with multiple sclerosis. PLoS ONE 2012, 7, e49996. [Google Scholar] [CrossRef]
- Hobart, J.; Lamping, D.; Fitzpatrick, R.; Riazi, A.; Thompson, A. The Multiple Sclerosis Impact Scale (MSIS-29); a new patient-based outcome measure. Brain 2001, 124, 962–973. [Google Scholar] [CrossRef]
- Rogić Vidaković, M.; Šimić, N.; Poljičanin, A.; Ivanišević, M.N.; Ana, J.; Đogaš, Z. Psychometric properties of the Croatian version of the depression, anxiety, and stress scale-21 and multiple sclerosis impact scale-29 in multiple sclerosis patients. Mult. Scler. Relat. Disord. 2021, 50, 102850. [Google Scholar] [CrossRef]
- Cole, J.C.; Motivala, S.J.; Buysse, D.J.; Oxman, M.N.; Levin, M.J.; Irwin, M. Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep 2006, 29, 112–116. [Google Scholar] [CrossRef]
- Manzar, M.D.; BaHammam, A.S.; Hameed, U.A. Dimensionality of the Pittsburgh sleep quality index: A systematic review. Health Qual. Life Outcomes 2018, 16, 89. [Google Scholar] [CrossRef]
- Benhayon, D.; Youk, A.; McCarthy, F.N.; Davis, S.; Keljo, D.J.; Bousvaros, A.; Fairclough, D.; Kupfer, D.; Buysse, D.J.; Szigethy, E.M. Characterization of relationships between sleep, inflammation, and psychiatric dysfunction in depressed youth with Crohn’s disease. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 335–343. [Google Scholar] [CrossRef]
- Manzar, M.D.; Zannat, W.; Hussain, M.E.; Pandi-Perumal, S.R.; Bahammam, A.S.; Barakat, D.; Ojike, N.I.; Olaish, A.; Spence, D.W. Dimensionality of the Pittsburgh sleep quality index in the young collegiate adults. Springerplus 2016, 5, 1550. [Google Scholar] [CrossRef]
- Jia, Y.; Chen, S.; Deutz, N.; Bukkapatnam, S.T.S.; Woltering, S. Examining the structure validity of the Pittsburgh sleep quality index. Sleep Biol. Rhythms. 2019, 17, 209–221. [Google Scholar] [CrossRef]
- Kmetec, S.; Fekonja, Z.; Davey, A.; Mlinar Reljić, N.; Lorber, M. Development of a slovenian version of the pittsburgh sleep quality index (PSQI-SLO) for use with older adults. Int. J. Older People Nurs. 2021, 17, e12411. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh sleep quality index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Longfeng, L.; Sheehan, C.M.; Thompson, M.S. Measurement invariance and sleep quality differences between men and women in the Pittsburgh sleep quality index. J. Clin. Sleep Med. 2019, 5, 1769–1776. [Google Scholar] [CrossRef]
- Lobentanz, I.S.; Asenbaum, S.; Vass, K.; Sauter, C.; Klosch, G.; Kollegger, H.; Kristoferitsch, W.; Zeitlhofer, J. Factors influencing quality of life in multiple sclerosis patients: Disability, depressive mood, fatigue and sleep quality. Acta Neurol. Scand. 2004, 110, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Rui, X.; Qi, P.; Liu, G.; Yang, J. Sleep disorders in patients with multiple sclerosis in China. Sleep Breath. 2017, 21, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Pinar, Ö.; Gönül, V.; Mehmet, Ö.; Şadiye, G. The relationship between quality of life and disability in multiple sclerosis patients and pain, sleep quality, mood and fatigue. Biomed. J. Sci. Tech. Res. 2018, 2, 2559–2565. [Google Scholar] [CrossRef][Green Version]
- Streiner, D.L.; Cairney, J. What’s under the ROC? An introduction to receiver operating characteristics curves. Can. J. Psychiatry 2007, 52, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Unal, I. Defining an optimal cut-point value in ROC analysis: An alternative approach. Comput. Math. Methods Med. 2017, 2017, 3762651. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Korkmaz, S.; Goksuluk, D.; Zararsiz, G. MVN: An R package for assessing multivariate normality. R J. 2014, 6, 151–162. [Google Scholar] [CrossRef]
- Jorgensen, T.D.; Pornprasertmanit, S.; Schoemann, A.M.; Rosseel, Y. semTools: Useful Tools for Structural Equation Modeling. R Package Version 0.5-3. Available online: https://CRAN.R-project.org/package=semTools (accessed on 6 November 2021).
- Pezzullo, J.C. Analysis of Variance from Summary Data. Available online: http://statpages.info/anova1sm.html (accessed on 6 November 2021).
- Dunn, T.J.; Baguley, T.; Brunsde, V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. Br. J. Psychol. 2014, 105, 399–412. [Google Scholar] [CrossRef]
- Reise, S.P.; Bonifay, W.E.; Haviland, M.G. Scoring and modeling psychological measures in the presence of multidimensionality. J. Pers. Assess. 2013, 95, 129–140. [Google Scholar] [CrossRef]
- Cederberg, K.J.; Jeng, B.; Sasaki, J.E.; Sikes, E.M.; Silveira, S.L.; Cutter, G.; Motl, R.W. Demographic, clinical, and symptomatic correlates of subjective sleep quality in adults with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 55, 103204. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Gavrilov, Y.V.; Shkilnyuk, G.G.; Valko, P.O.; Stolyarov, I.D.; Ivashkova, E.V.; Ilves, A.G.; Nikiforova, I.G.; Shchelkova, O.Y.; Vasserman, L.I.; Vais, E.E.; et al. Validation of the Russian version of the fatigue impact scale and fatigue severity scale in multiple sclerosis patients. Acta Neurol. Scand. 2018, 138, 408–416. [Google Scholar] [CrossRef]
- Armutlu, K.; Korkmaz, N.C.; Keser, I.; Sumbuloglu, V.; Akbiyik, D.I.; Guney, Z.; Karabudak, R. The validity and reliability of the fatigue severity scale in Turkish multiple sclerosis patients. Int. J. Rehabil. Res. 2007, 30, 81–85. [Google Scholar] [CrossRef]
- Rosti-Otajärvi, E.; Hämäläinen, P.; Wiksten, A.; Hakkarainen, T.; Ruutiainen, J. Validity and reliability of the fatigue severity scale in Finnish multiple sclerosis patients. Brain Behav. 2017, 7, e00743. [Google Scholar] [CrossRef]
- Valko, P.O.; Bassetti, C.L.; Bloch, K.E.; Held, U.; Baumann, C.R. Validation of the fatigue severity scale in a Swiss cohort. Sleep 2008, 31, 1601–1607. [Google Scholar] [CrossRef]
- Jerković, A.; Proroković, A.; Matijaca, M.; Katić, A.; Košta, V.; Mihalj, M.; Dolić, K.; Đogaš, Z.; Vidaković, M.R. Validation of the fatigue severity scale in Croatian population of patients with multiple sclerosis disease: Factor structure, internal consistency, and correlates. Mult. Scler. Relat. Disord. 2021, 58, 103397. [Google Scholar] [CrossRef]
- Karimi, S.; Andayeshgar, B.; Khatony, A. Prevalence of Anxiety, depression, and stress in patients with multiple sclerosis in Kermanshah-Iran: A cross-sectional study. BMC Psychiatry 2020, 20, 166. [Google Scholar] [CrossRef]
- Jerković, A.; Proroković, A.; Matijaca, M.; Vuko, J.; Poljičanin, A.; Mastelić, A.; Katić, A.; Košta, V.; Kustura, L.; Dolić, K.; et al. Psychometric Properties of the HADS measure of anxiety and depression among multiple sclerosis patients in Croatia. Front. Psychol. 2021, 12, 794353. [Google Scholar] [CrossRef]
- Benedict, R.H.; DeLuca, J.; Phillips, G.; LaRocca, N.; Hudson, L.D.; Rudick, R. Multiple sclerosis outcome assessments consortium. Validity of the symbol digit modalities test as a cognition performance outcome measure for multiple sclerosis. Mult. Scler. 2017, 23, 721–733. [Google Scholar] [CrossRef]
- Jerković, A.; Matijaca, M.; Ana Proroković, A.; Šikić, A.; Košta, V.; Katić, A.; Dolić, K.; Glavor, K.D.; Šoda, J.; Đogaš, Z.; et al. Information processing speed assessed with letter digit substitution test in Croatian sample of multiple sclerosis patients. Diagnostics 2022, 12, 111. [Google Scholar] [CrossRef]
- Hämäläinen, P.; Vera Leo, V.; Sebastian Therman, S.; Juhani Ruutiainen, J. Validation of the Finnish version of the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) and evaluation of the applicability of the Multiple Sclerosis Neuropsychological Questionnaire (MSNQ) and the Fatigue Scale for Motor and Cognitive Functions (FSMC). Brain Behav. 2021, 11, e02087. [Google Scholar] [CrossRef]
- Kahraman, T.; Ozdogar, A.T.; Abasiyanik, Z.; Ozakbas, S. Multiple sclerosis research group. Associations between smoking and walking, fatigue, depression, and health-related quality of life in persons with multiple sclerosis. Acta Neurol. Belg. 2021, 121, 1199–1206. [Google Scholar] [CrossRef]
- Ozdogar, A.T.; Turhan Kahraman, T.; Ozakbas, S.; Achiron, A.; Kalron, A. Fatigue is associated with physical inactivity in people with multiple sclerosis despite different environmental backgrounds: Merging and comparing cohorts from Turkey and Israel. Mult. Scler. Relat. Disord. 2021, 57, 103456. [Google Scholar] [CrossRef]
| Variable | Category | pwMS | All Control Subjects | Control Group | pwMS—Control Group Comparison |
|---|---|---|---|---|---|
| Gender | Women | 81.6 | 50.5 | 81.3 | χ2(1) = 0.002 p = 0.960 |
| Men | 18.4 | 49.5 | 18.7 | ||
| Right hand dominance | Yes | 93.1 | 90.7 | 93.3 | χ2(1) = 0.004 p = 0.951 |
| No | 5.7 | 8.8 | 6 | ||
| Education | Primary school | 3.4 | 2.8 | 3 | χ2(3) = 5.453 p = 0.141 |
| High school | 65.5 | 60.2 | 51.5 | ||
| Undergraduate study | 9.2 | 10.2 | 11.2 | ||
| Graduate study | 20.7 | 26.9 | 34.3 | ||
| Marriage status | Single | 21.8 | 22.2 | 20.9 | χ2(3) = 3.282 p = 0.350 |
| Marriage/cohabitation | 63.2 | 68.1 | 71.6 | ||
| Divorced/separated | 10.3 | 7.5 | 4.5 | ||
| Widow(er) | 3.4 | 2.3 | 3 | ||
| Working status | Student | 6.9 | 6 | 6.7 | χ2(7) = 52.819 p < 0.001 |
| Employee | 32.2 | 76.9 | 76.1 | ||
| Unemployed | 18.4 | 7.9 | 9.7 | ||
| Temporary sick leave | 6.9 | 0.5 | 0.7 | ||
| Permanent incapacity for work | 5.7 | 0 | 0 | ||
| A person who runs the household | 3.4 | 0 | 0 | ||
| Disability pension | 23 | 8.3 | 6.7 | ||
| Other | 2.3 | 0.5 | 0 | ||
| Comorbidity | No | 64.4 | 80.1 | 78.4 | χ2(1) = 4.663 p = 0.031 |
| Yes | 28.7 | 15.3 | 17.2 | ||
| Age | M (SD) | 42.57 (12.2) | 43.8 (12.632) | 43.78 (12.749) | t(219) = 0.700 p = 0.484 |
| Range | 19–73 | 18–81 | 22–73 |
| Model | χ2 (p) | df | CFI | RMSEA (0% CI) | SRMR | Δχ2 (p) | Δdf |
|---|---|---|---|---|---|---|---|
| One-factor | 75.83 (0.000) | 32 | 0.862 | 0.097 [0.069, 0.126] | 0.073 | ||
| Two-factor (2F) | 46.03 (0.031) | 30 | 0.949 | 0.061 [0.019, 0.094] | 0.052 | 20.06 (<0.001) | 2 |
| Three-factor | 34.45 (0.124) | 26 | 0.973 | 0.047 [0.000, 0.086] | 0.045 | 9.64 (0.047) | 4 |
| Bifactor | 13.28 (0.774) | 18 | 1.000 | 0.000 [0.000, 0.051] | 0.022 | 20.33 (0.061) | 12 |
| 2F with free loadings | 29.16 (0.404) | 28 | 0.996 | 0.017 [0.000, 0.067] | 0.036 | 6.55 (0.038) | 2 |
| Loadings invariance 2F | 40.62 (0.141) | 32 | 0.973 | 0.043 [0.000, 0.079] | 0.052 | 7.21 (0.125) | 4 |
| Partial intercept invariance 2F | 44.33 (0.160) | 36 | 0.974 | 0.040 [0.000, 0.075] | 0.054 | 3.75 (0.441) | 4 |
| Intercept invariance 2F | 58.44 (0.014) | 37 | 0.932 | 0.063 [0.029, 0.093] | 0.061 | 18.61 (<0.001) | 1 |
| Variable | pwMS | Control |
|---|---|---|
| PSQI global score | –/0.83 | –/0.69 |
| PSQI sleep quality | 0.80/0.81 | 0.64/0.61 |
| PSQI sleep efficiency | 0.79/0.79 | 0.69/0.69 |
| Variable | Mf (SDf) | Mm (SDm) | Levene’s Test F (p) | t (p) |
|---|---|---|---|---|
| PSQI global score | 6.37(3.928) | 5.08(3.243) | 7.45(0.007) | 3.12(0.002) |
| PSQI sleep quality | 4.89(2.797) | 3.57(2.125) | 9.31(0.002) | 4.61(0.000) |
| PSQI sleep efficiency | 1.58(1.648) | 1.57(1.671) | 0.01(0.935) | 0.09(0.930) |
| Variable | Age a | EDSS b | MSIS-29 psy c | MSIS-29 phy c | Duration d |
|---|---|---|---|---|---|
| PSQI global score | 0.241 ** | 0.248 * | 0.772 ** | 0.601 ** | −0.135 |
| PSQI sleep quality | 0.148 * | 0.084 | 0.826 ** | 0.664 ** | −0.074 |
| PSQI sleep efficiency | 0.294 ** | 0.330 ** | 0.461 ** | 0.319 ** | −0.143 |
| Variable | Cut-Off | Criteria | Sens | Spec | pwMS | Con | ||
|---|---|---|---|---|---|---|---|---|
| High PSQI | Low PSQI | High PSQI | Low PSQI | |||||
| PSQI global score | 5 | Curcio et al. | 0.671 | 0.429 | 0.644 | 0.356 | 0.575 | 0.425 |
| 6 | IuO/Φ | 0.633 | 0.571 | 0.598 | 0.402 | 0.433 | 0.567 | |
| 10 | Youden | 0.392 | 0.895 | 0.368 | 0.632 | 0.104 | 0.896 | |
| PSQI sleep quality | 5 | IuO/Φ | 0.595 | 0.609 | 0.590 | 0.410 | 0.391 | 0.609 |
| 7 | Youden | 0.367 | 0.880 | 0.361 | 0.639 | 0.120 | 0.880 | |
| Variable | Category | n | PSQI Global Score | PSQI Sleep Quality | PSQI Sleep Efficiency | |||
|---|---|---|---|---|---|---|---|---|
| M (SD) | t/F (p) | M (SD) | t/F (p) | M (SD) | t/F (p) | |||
| Type of MS | Relapsing-remitting | 64–69 | 7.00 (4.462) | −1.40 (0.166) | 5.61 (3.243) | −0.24 (0.808) | 1.63 (1.768) | −2.58 (0.017) |
| Other MS types | 17–18 | 8.72 (5.345) | 5.82 (3.432) | 3.17 (2.358) | ||||
| Gender | Women | 66–71 | 7.46 (4.601) | 0.45 (0.651) | 5.90 (3.299) | 1.41 (0.163) | 1.89 (1.890) | −0.54 (0.595) |
| Men | 16 | 6.88 (5.136) | 4.63 (2.986) | 2.25 (2.463) | ||||
| Marriage status | Married/cohabitating | 53–55 | 7.02 (4.148) | −1.05 (0.298) | 5.45 (2.978) | −0.73 (0.466) | 1.70 (1.846) | −1.64 (0.105) |
| Single/separated/widowed | 29–31 | 8.19 (5.388) | 6.00 (3.742) | 2.45 (2.213) | ||||
| Working status | Active | 33–34 | 6.12 (4.617) | 6.39 (0.003) | 4.82 (3.264) | 2.69 (0.074) | 1.41 (1.725) | 8.36 (0.001) |
| Temporarily inactive | 19–22 | 6.27 (4.366) | 5.30 (3.246) | 1.32 (1.827) | ||||
| Permanently inactive | 24–25 | 9.92 (3.947) | 6.72 (2.880) | 3.25 (2.069) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jerković, A.; Mikac, U.; Matijaca, M.; Košta, V.; Ćurković Katić, A.; Dolić, K.; Vujović, I.; Šoda, J.; Đogaš, Z.; Pavelin, S.; et al. Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in Patients with Multiple Sclerosis: Factor Structure, Reliability, Correlates, and Discrimination. J. Clin. Med. 2022, 11, 2037. https://doi.org/10.3390/jcm11072037
Jerković A, Mikac U, Matijaca M, Košta V, Ćurković Katić A, Dolić K, Vujović I, Šoda J, Đogaš Z, Pavelin S, et al. Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in Patients with Multiple Sclerosis: Factor Structure, Reliability, Correlates, and Discrimination. Journal of Clinical Medicine. 2022; 11(7):2037. https://doi.org/10.3390/jcm11072037
Chicago/Turabian StyleJerković, Ana, Una Mikac, Meri Matijaca, Vana Košta, Ana Ćurković Katić, Krešimir Dolić, Igor Vujović, Joško Šoda, Zoran Đogaš, Sanda Pavelin, and et al. 2022. "Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in Patients with Multiple Sclerosis: Factor Structure, Reliability, Correlates, and Discrimination" Journal of Clinical Medicine 11, no. 7: 2037. https://doi.org/10.3390/jcm11072037
APA StyleJerković, A., Mikac, U., Matijaca, M., Košta, V., Ćurković Katić, A., Dolić, K., Vujović, I., Šoda, J., Đogaš, Z., Pavelin, S., & Rogić Vidaković, M. (2022). Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in Patients with Multiple Sclerosis: Factor Structure, Reliability, Correlates, and Discrimination. Journal of Clinical Medicine, 11(7), 2037. https://doi.org/10.3390/jcm11072037









