Author Contributions
Conceptualization, M.B.C., M.R.M., C.B.A. and J.A.D.L.-L.; methodology, M.B.C., M.R.M., C.B.A. and J.A.D.L.-L. validation, J.A.D.L.-L.; investigation, M.B.C., M.R.M., I.A.M., S.G.T., P.P.R., M.A.-M., C.B.A., M.A.O. and J.A.D.L.-L.; data curation, M.B.C., M.R.M., I.A.M., S.G.T., P.P.R., M.A.-M., C.B.A., M.A.O. and J.A.D.L.-L.; writing—original draft preparation, M.B.C., M.R.M., I.A.M., S.G.T., P.P.R., M.A.-M., C.B.A., M.A.O. and J.A.D.L.-L.; writing—review and editing, M.B.C., M.R.M., I.A.M., S.G.T., P.P.R., M.A.-M., C.B.A., M.A.O. and J.A.D.L.-L.; visualization, M.A.-M., C.B.A., M.A.O. and J.A.D.L.-L.; project administration, M.A.O.; funding acquisition, M.A.-M., M.A.O. and J.A.D.L.-L. All authors have read and agreed to the published version of the manuscript.
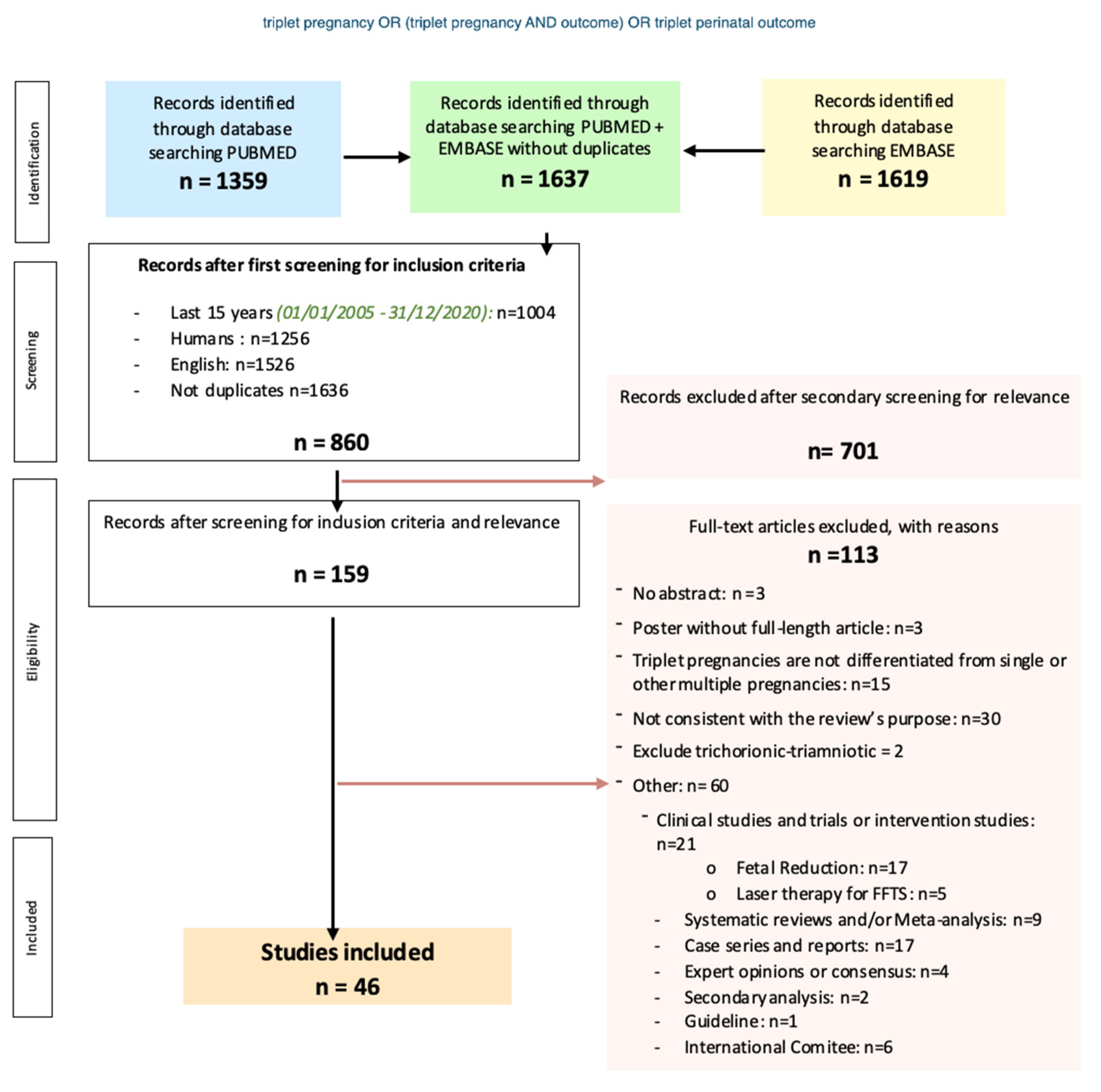
Figure 1.
Flowchart of the systematic review, search strategy, inclusion and exclusion criteria.
Figure 1.
Flowchart of the systematic review, search strategy, inclusion and exclusion criteria.
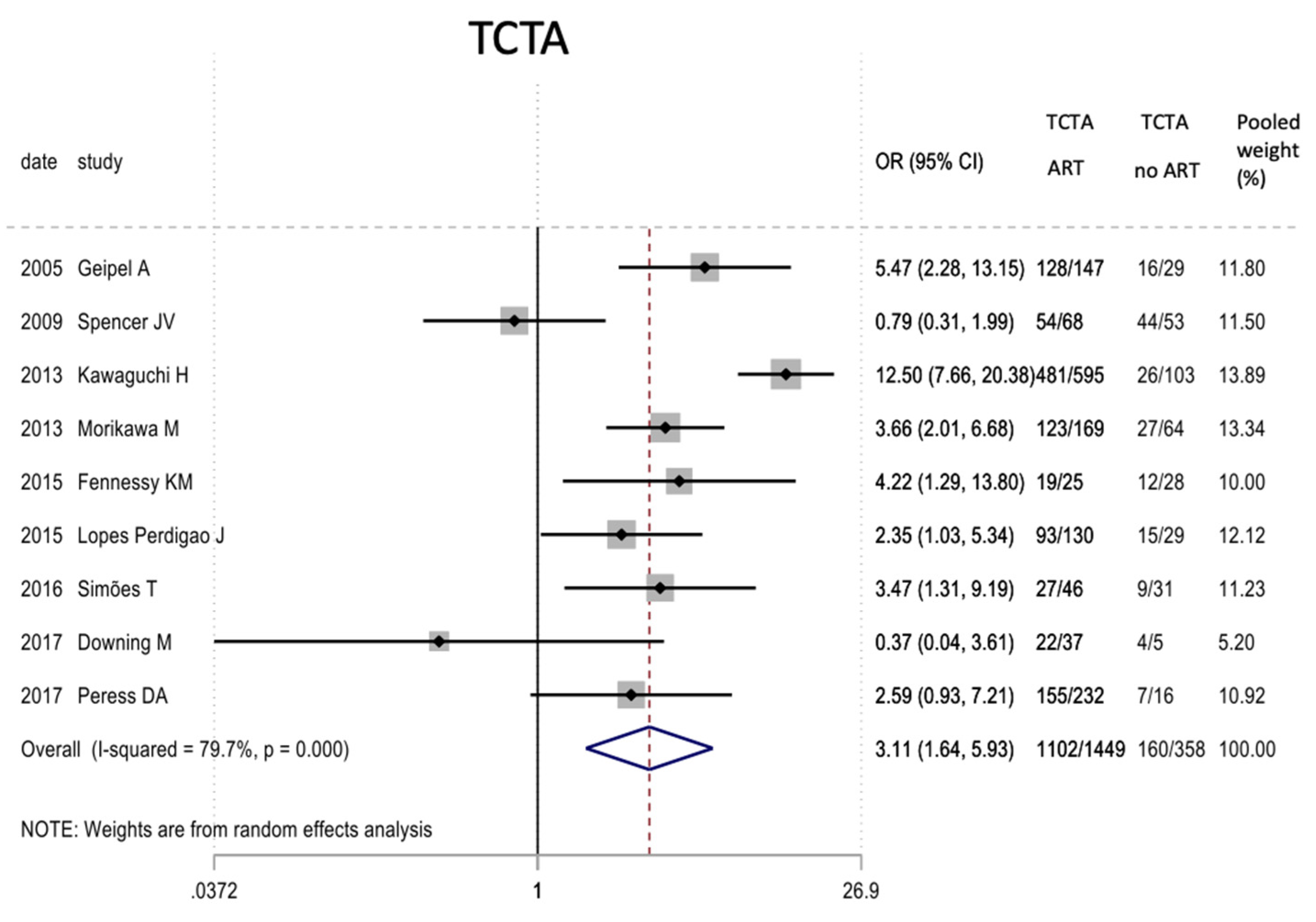
Figure 2.
Results of the meta-analysis on the effect of assisted reproductive therapies on the chorionicity of pregnancies (TCTA vs. non-TCTA). TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 2.
Results of the meta-analysis on the effect of assisted reproductive therapies on the chorionicity of pregnancies (TCTA vs. non-TCTA). TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 3.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on cesarean as the mode of delivery. TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 3.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on cesarean as the mode of delivery. TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
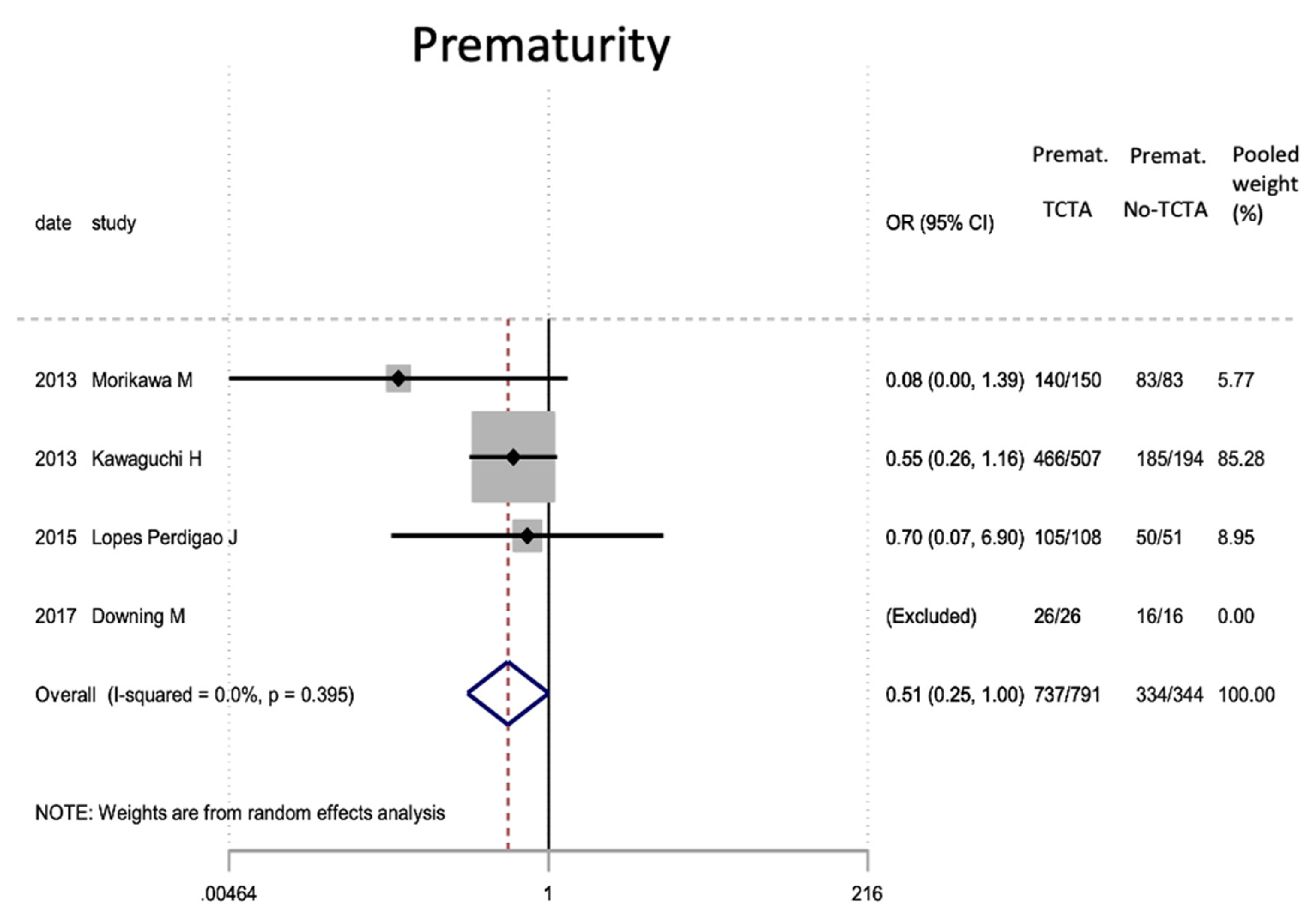
Figure 4.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on prematurity in newborns (under 37 weeks). Premat: prematurity, TCTA: tricorial-triamniotic, non-TCTA: non-tricorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 4.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on prematurity in newborns (under 37 weeks). Premat: prematurity, TCTA: tricorial-triamniotic, non-TCTA: non-tricorial-triamniotic. OR = odds ratio, CI = confidence interval.
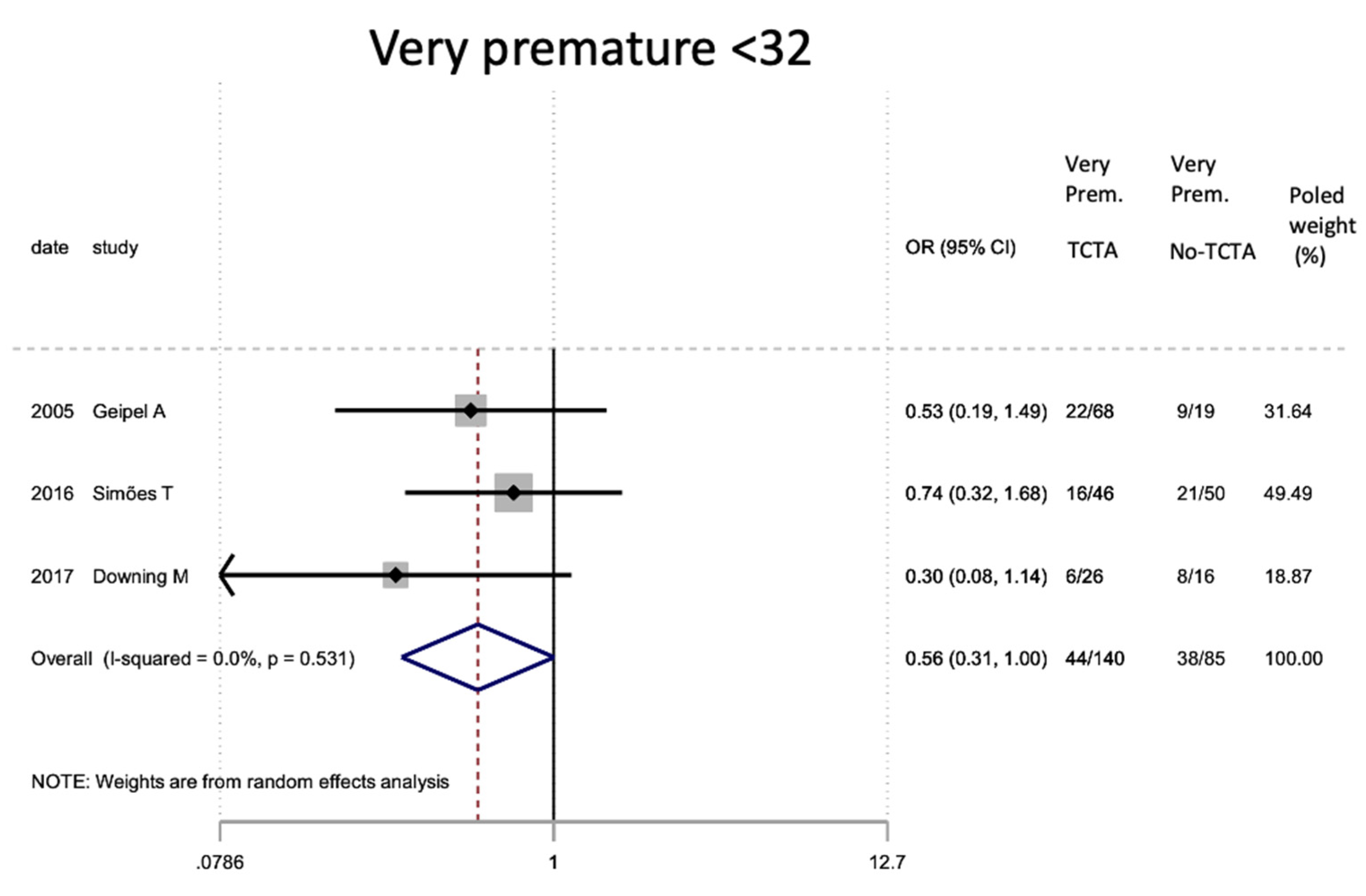
Figure 5.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on very preterm newborns (under 32 weeks). Very Prem: very premature; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 5.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on very preterm newborns (under 32 weeks). Very Prem: very premature; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
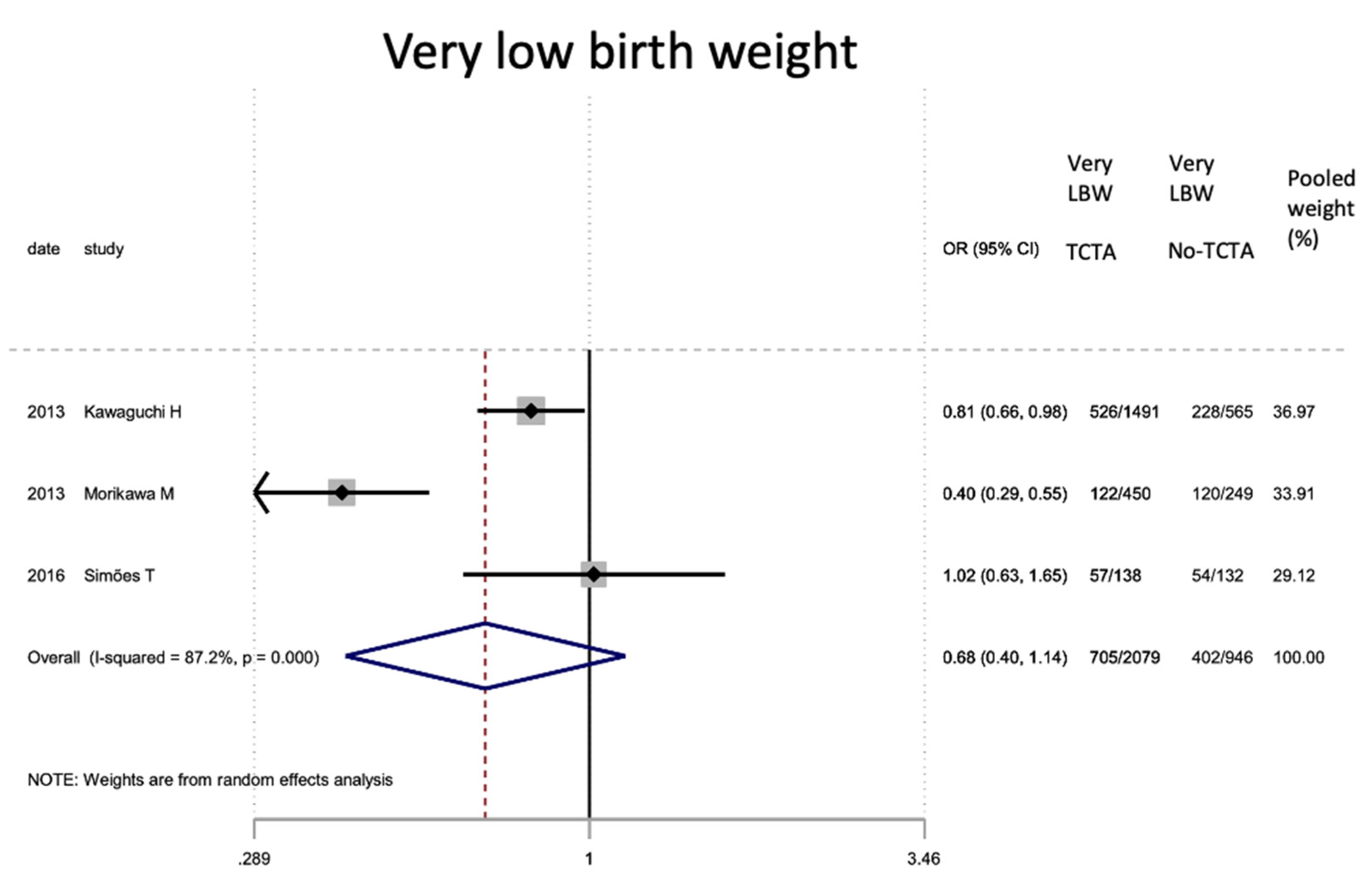
Figure 6.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on very low birth weight newborns (below 1500 g). Very LBW: very low birth weight; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 6.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on very low birth weight newborns (below 1500 g). Very LBW: very low birth weight; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
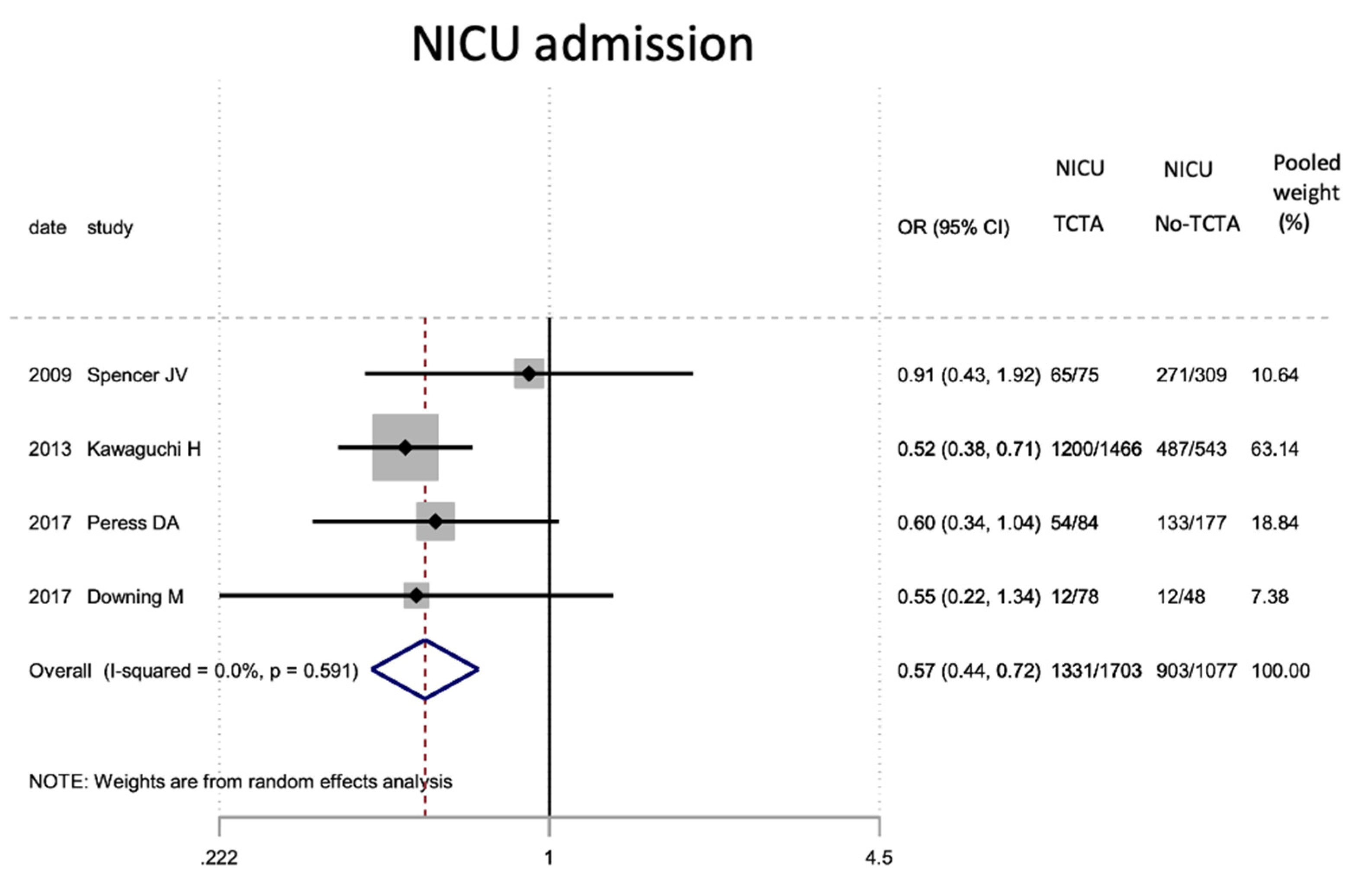
Figure 7.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on NICU admission. NICU: neonatal inten-sive care unit; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 7.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on NICU admission. NICU: neonatal inten-sive care unit; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
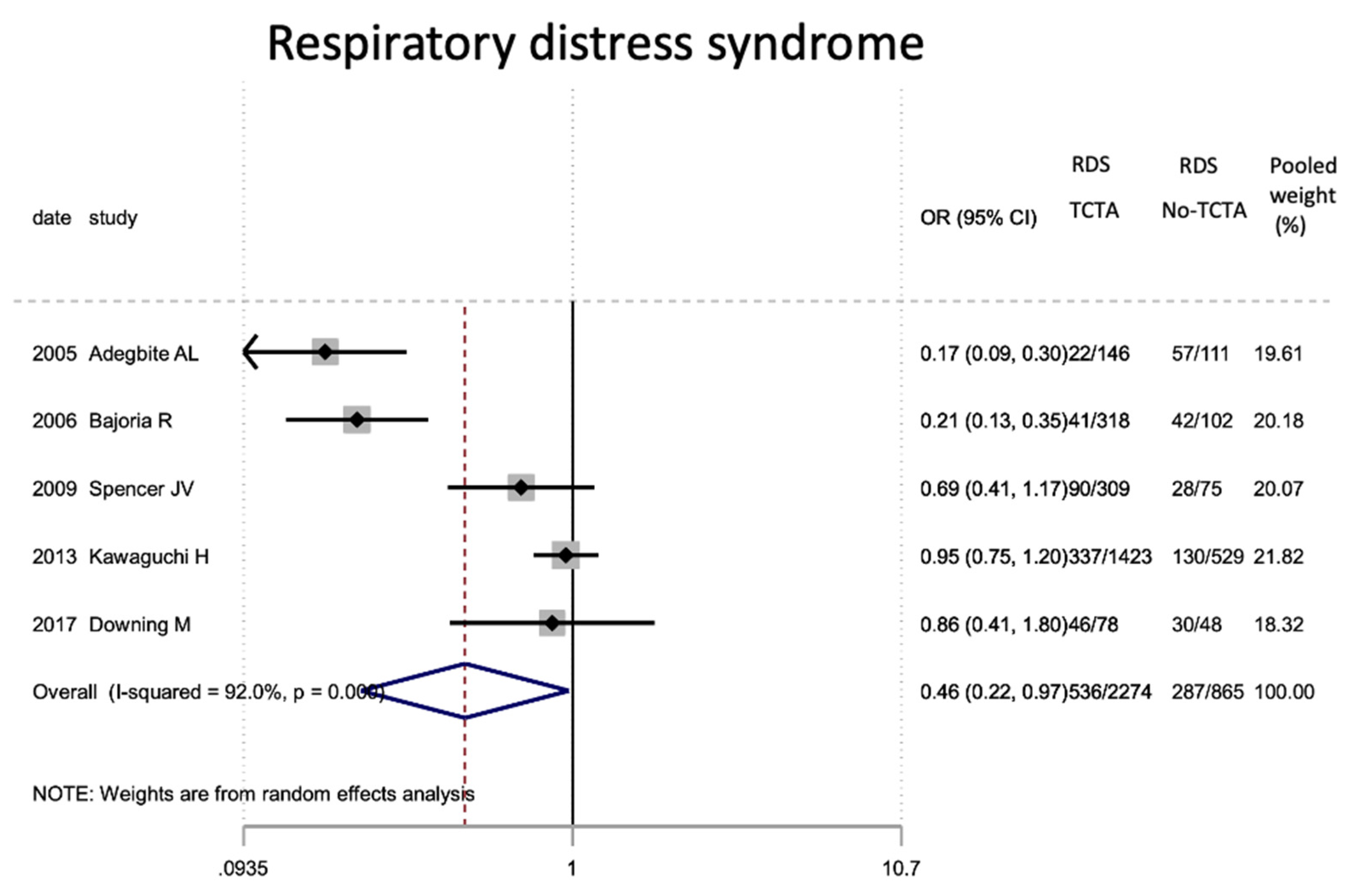
Figure 8.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on neonatal respiratory distress. RDS: respiratory distress; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 8.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on neonatal respiratory distress. RDS: respiratory distress; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 9.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal bronchopulmonary dysplasia. BPD: bronchopulmonary dysplasia; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 9.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal bronchopulmonary dysplasia. BPD: bronchopulmonary dysplasia; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
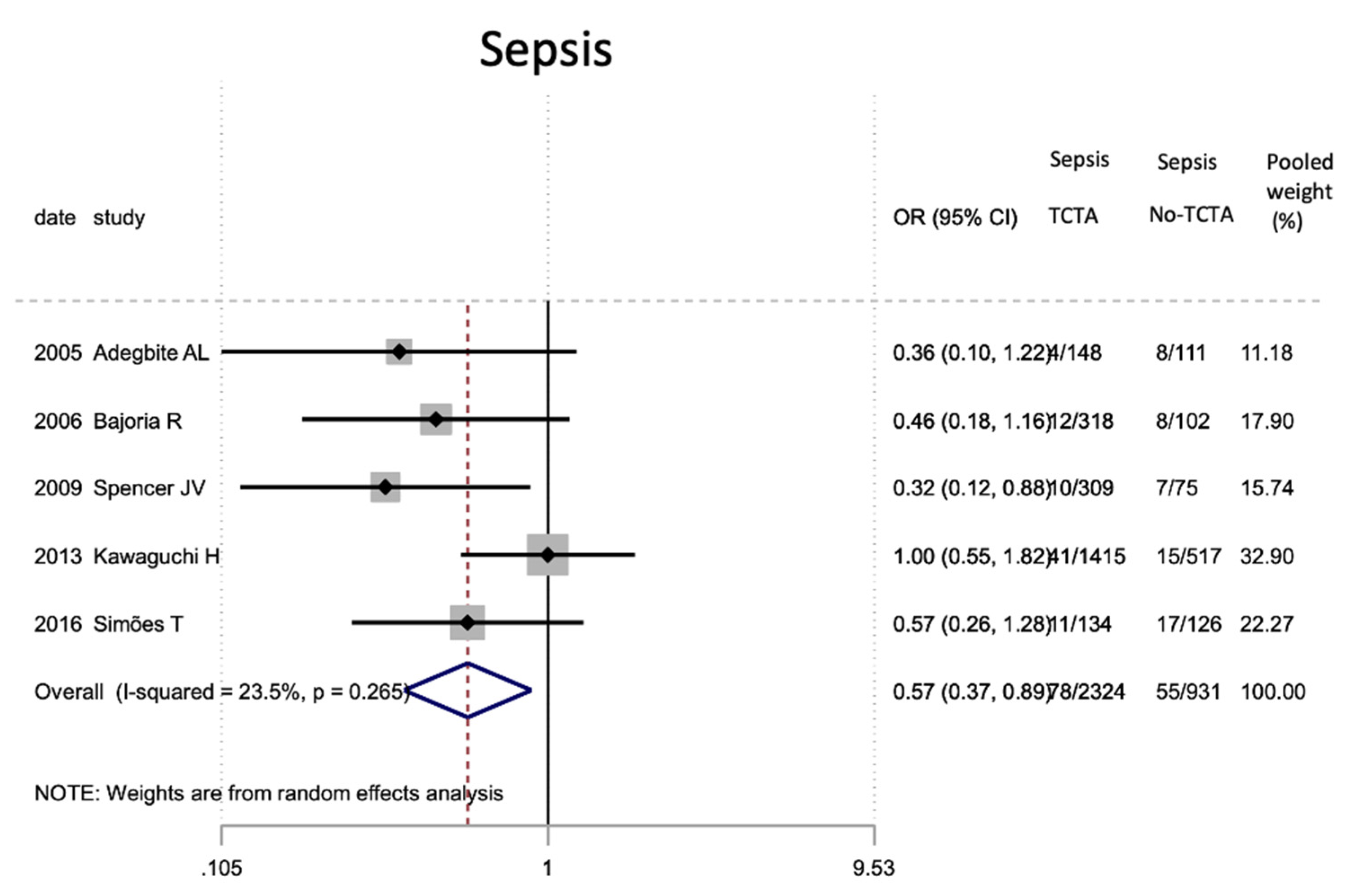
Figure 10.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal sepsis; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 10.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal sepsis; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
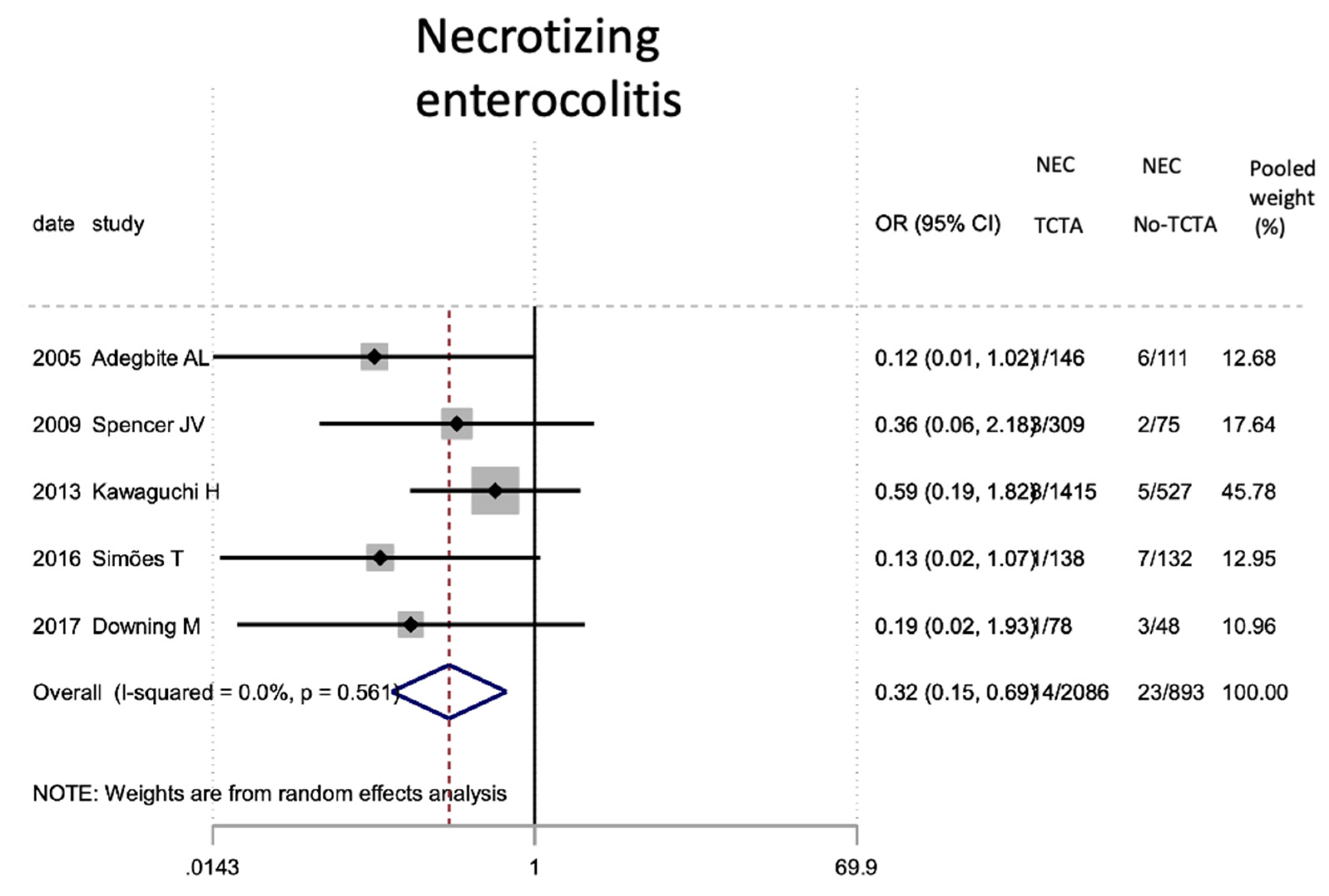
Figure 11.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal necrotizing enterocolitis. NEC: necrotizing enterocolitis; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 11.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of neonatal necrotizing enterocolitis. NEC: necrotizing enterocolitis; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 12.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of retinopathy of prem-aturity. ROP: retinopathy of prematurity; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 12.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of retinopathy of prem-aturity. ROP: retinopathy of prematurity; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
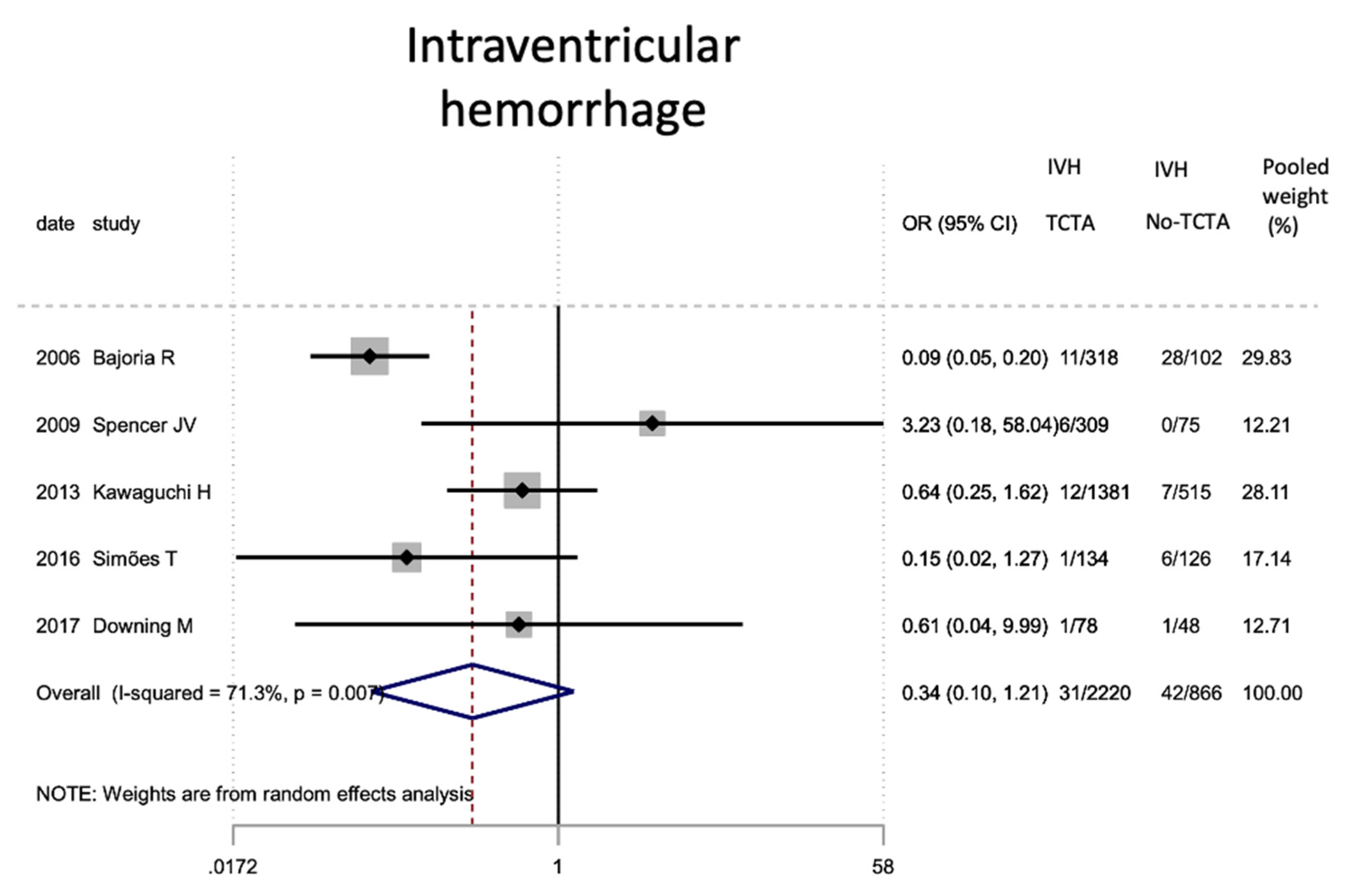
Figure 13.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of severe stage III-IV intraventricular hemorrhage. IVH: intraventricular hemorrhage; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 13.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on the development of severe stage III-IV intraventricular hemorrhage. IVH: intraventricular hemorrhage; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
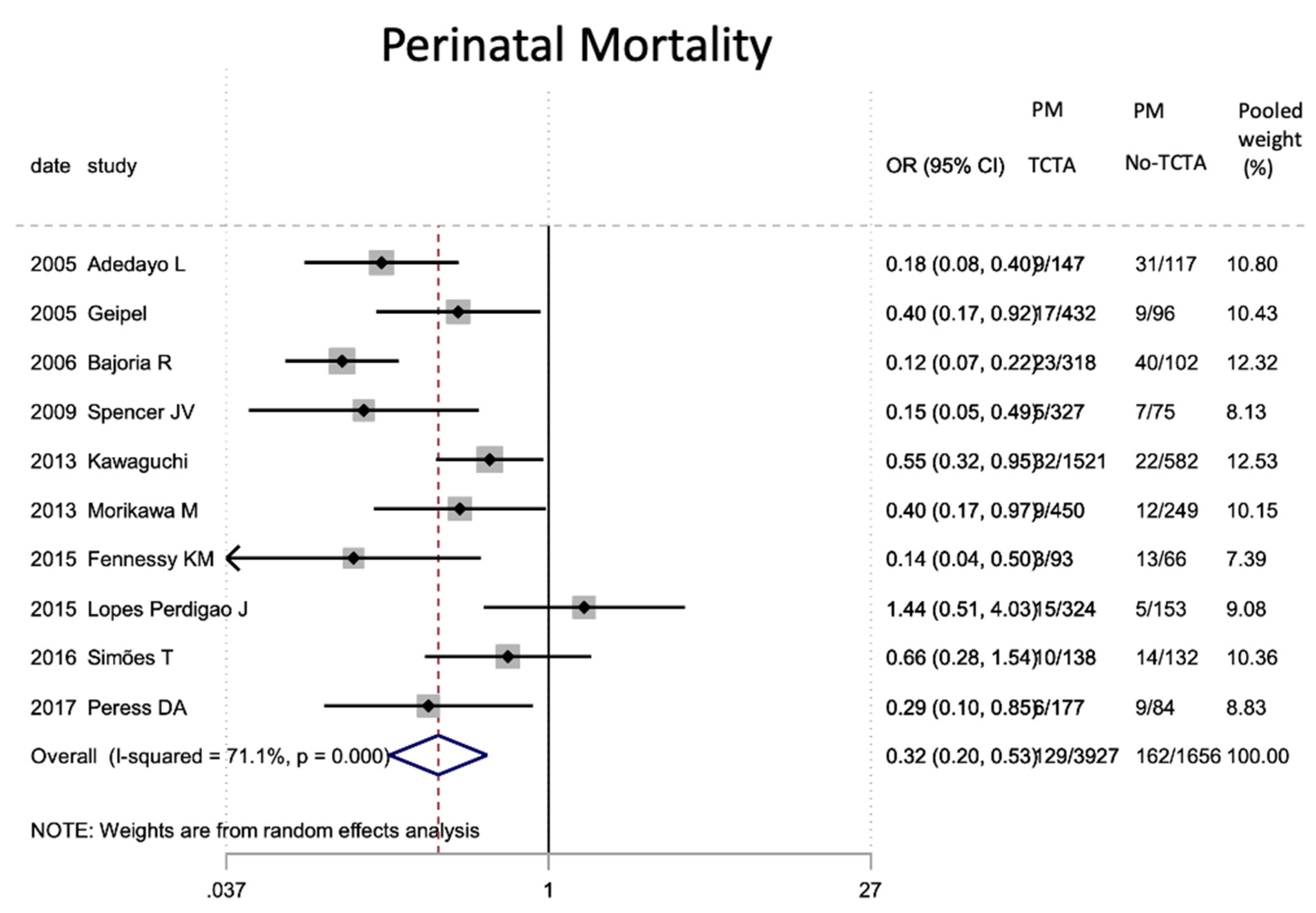
Figure 14.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on perinatal mortality. PM: perinatal mortal-ity; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 14.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on perinatal mortality. PM: perinatal mortal-ity; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 15.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on intrauterine fetal mortality. MFIU: intrau-terine fetal mortality; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 15.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on intrauterine fetal mortality. MFIU: intrau-terine fetal mortality; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
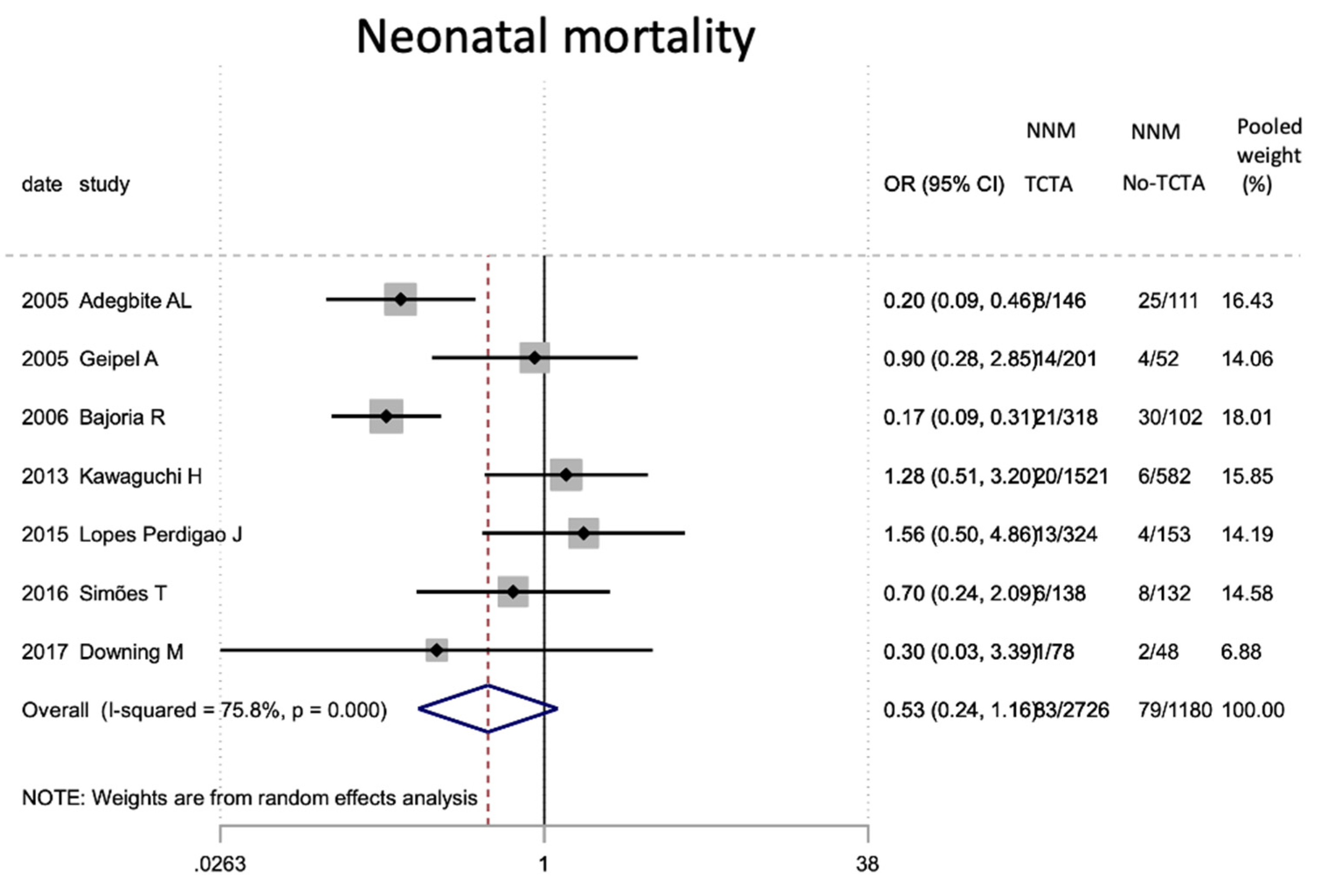
Figure 16.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on neonatal mortality. NNM: neonatal mor-tality; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Figure 16.
Results of the meta-analysis on the effect of chorionicity (TCTA vs no TCTA) on neonatal mortality. NNM: neonatal mor-tality; TCTA: trichorial-triamniotic, non-TCTA: non-trichorial-triamniotic. OR = odds ratio, CI = confidence interval.
Table 1.
Characteristics of the studies included in the systematic review and meta-analysis.
Table 1.
Characteristics of the studies included in the systematic review and meta-analysis.
| Number | Authors | Country | Year of Publication | Recruitment Period | Study Type | Center | Live Newborn | Triplet Pregnancies |
|---|
| 1 | Adegbite et al. * | United Kingdom | 2005 | 1986–2000 | ROC | M | 257 | 88 |
| 2 | Day et al. | USA | 2005 | 1995–2004 | POC | M | 7024 | 2545 |
| 3 | Geipel et al. * | Germany | 2005 | 1998–2003 | ROC | M | 253 | 176 |
| 4 | Salihu, Aliyu et al. | USA | 2005 | 1995–1997 | PS | M | 15,021 | 5265 |
| 5 | Salihu, Bagchi et al. | USA | 2005 | 1995–1998 | PS | M | 21,676 | 7225 |
| 6 | Al-Suleiman et al. | Saudi Arabia | 2006 | 1990–2004 | ROC | U | 104 | 35 |
| 7 | Bajoria et al. * | United Kingdom | 2006 | 1986–2000 | ROC | M | 408 | 140 |
| 8 | Luke et al. | USA | 2006 | 1996–2001 | ROC | U | 24 | 8 |
| 9 | Eddib et al. | USA | 2007 | 1999–2003 | ROC | U | NR | 56 |
| 10 | Luke et al. | USA | 2007 | 1989–2001 | PS | M | 26,829 | 8943 |
| 11 | Luke et al. | USA | 2007 | 1995–2000 | PS | M | 36,579 | 12,193 |
| 12 | Zuppa et al. | Italia | 2007 | 1994–2003 | ROC | U | 71 | 24 |
| 13 | Mazhar et al. | Pakistan | 2008 | 2000–2006 | ROC | U | 50 | 18 |
| 14 | Battin et al. | New Zealand | 2009 | 1995–2005 | ROC | U | 155 | 55 |
| 15 | Kraemer et al. | Germany | 2009 | 1980–1997 | ROC | U | 77 | 26 |
| 16 | Spencer et al. * | USA | 2009 | 1995–2007 | ROC | M | 379 | 128 |
| 17 | Tandberg et al. | Norway | 2010 | 1967–2006 | ROC | M | 1344 | 448 |
| 18 | Al-Sunaidi et al. | Saudi Arabia | 2011 | 2007–2009 | ROC | U | 87 | 32 |
| 19 | Arlettaz et al. | Switzerland | 2011 | 2005–2008 | ROC | M | 290 | 100 |
| 20 | Machtinger et al. | Israel | 2011 | 1997–2005 | ROC | U | 219 | 73 |
| 21 | Moore et al. | USA | 2012 | 1989–2010 | POC | U | 417 | 139 |
| 22 | Chibber et al. | Kuwait | 2013 | 2001–2011 | ROC | U | 278 | 100 |
| 23 | Kawaguchi et al. * | Japan | 2013 | 1999–2009 | ROC | M | 2076 | 701 |
| 24 | Morikawa et al. * | Japan | 2013 | 2005–2008 | ROC | M | 960 | 320 |
| 25 | Revello et al. | Spain | 2013 | 2000–2010 | ROC | U | 428 | 147 |
| 26 | Weissman et al. | Israel | 2013 | 2001–2011 | ROC | U | 102 | 34 |
| 27 | Almeida et al. * | Portugal | 2014 | 1996–2011 | POC | U | 96 | 33 |
| 28 | Fennessy et al. * | Australia | 2015 | 1999–2011 | ROC | U | 150 | 53 |
| 29 | Lopes et al. * | USA | 2015 | 1999–2010 | ROC | M | 474 | 159 |
| 30 | Lappen et al. | USA | 2016 | 2002–2008 | ROC | M | 240 | 80 |
| 31 | Maia et al. | Brazil | 2016 | 1998–2012 | ROC | U | 185 | 67 |
| 32 | Morency et al. | Canada | 2016 | 2000–2013 | ROC | U | 690 | 230 |
| 33 | Simões et al. * | Portugal | 2016 | 1994–2014 | ROC | U | 260 | 90 |
| 34 | AlBasri et al. | Saudi Arabia | 2017 | 2004–2011 | ROC | U | 62 | 21 |
| 35 | Downing et al. * | USA | 2017 | 2009–2015 | ROC | U | 123 | 42 |
| 36 | Lachowska et al. | Polonia | 2017 | 2006–2015 | ROC | U | 99 | 34 |
| 37 | Peress et al. * | USA | 2017 | 2005–2016 | ROC | U | NR | 258 |
| 38 | Razavi et al. | USA | 2017 | 2003–2015 | ROC | U | 240 | 80 |
| 39 | Ko et al. | South Korea | 2018 | 2009–2015 | PS | M | 1865 | 621 |
| 40 | Rajan et al. | India | 2018 | 2000–2014 | ROC | U | 225 | 82 |
| 41 | Shah et al. | Intercontinental | 2018 | 2007–2013 | ROC | M | 6079 | 2026 |
| 42 | Shah et al. | USA | 2018 | 2004–2006 | ROC | M | 381 | 127 |
| 43 | Dudenhausen et al. | Europe | 2019 | 2011–2012 | PS | M | 258 | 97 |
| 44 | Kyeong et al. | South Korea | 2019 | 1992–2012 | ROC | M | 185 | 65 |
| 45 | Mol et al. | Netherlands | 2019 | 1999–2008 | ROC | M | 1158 | 386 |
| 46 | Peress et al. | USA | 2019 | 2005–2016 | ROC | U | 249 | 83 |
| | All articles included in sistematic review | | | | 128,127 | 43,653 |
| | All articles included in the meta-analysis * | | | | 5441 | 2188 |
Table 2.
Maternal and gestational characteristics of the triplet pregnancies included in the systematic review.
Table 2.
Maternal and gestational characteristics of the triplet pregnancies included in the systematic review.
| Maternal and Gestational Characteristics | Number of Studies | Number of Pregnancies | n (%) or Mean |
|---|
| Maternal age (median, SD) | 39 | 28,415 | 31.6 |
| Primipara | 31 | 32,537 | 14,890 (45.76%) |
| BMI | 12 | 1858 | 26.7 |
| Maternal medical conditions | 7 | 18,194 | 832.4 (4.58%) |
| Assisted reproductive technology | 31 | 4352 | 2962 (68.06%) |
| Triamniotic-trichorionic | 25 | 3616 | 2318 (64.10%) |
| Triamniotic-dichorionic | 22 | 3276 | 815 (24.88%) |
| Triamniotic-monochorionic | 21 | 3035 | 129 (4.25%) |
Table 3.
Obstetric complications in the triplet pregnancies included in the systematic review.
Table 3.
Obstetric complications in the triplet pregnancies included in the systematic review.
| Obstetric Complications | Number of Studies | Number of Pregnancies | n (%) |
|---|
| Antenatal corticosteroids | 19 | 4310 | 3336 (77.4%) |
| Cervical cerclage | 11 | 1366 | 566 (41.43%) |
| Intrauterine growth restriction/low birth weight | 19 | 13,989 | 4884.8 (34.92%) |
| Threatened preterm labor | 24 | 14,848 | 3918.7 (26.39%) |
| Hipertensive disorders | 34 | 25,571 | 3626.7 (14.18%) |
| Preterm rupture of membranes | 25 | 14,997 | 1725.8 (11.51%) |
| Diabetes | 22 | 22,764 | 1493.6 (6.56%) |
| Fetal malformation | 17 | 1866 | 122 (6.54%) |
| Postpartum hemorrhage | 7 | 12,764 | 584.6 (4.58%) |
| Twin to twin transfusion syndrome | 18 | 2649 | 74 (2.79%) |
| Antenatal bleeding | 10 | 12,914 | 315.8 (2.45%) |
Table 4.
Perinatal results of the triplet pregnancies included in the systematic review.
Table 4.
Perinatal results of the triplet pregnancies included in the systematic review.
| Perinatal Results | Number of Studies | Number of Pregnancies * or Newborns + | n(%) or Mean |
|---|
| Cesarean section | 34 | 23,791 * | 21,169.8 (88.98%) |
| GA at delivery | 41 | 22,247 * | 32.3 |
| GA <37weeks | 16 | 24,001 * | 22,284.7 (92.85%) |
| GA <34 weeks | 8 | 1537 * | 885 (57.58%) |
| GA <32 weeks | 17 | 11,136 * | 4559.6 (40.94%) |
| GA <28 weeks | 15 | 11,418 * | 1475.7 (12.92%) |
| Birth weight (g) | 41 | 28,529 + | 1638 |
| Very low birth weight (<1500 g) | 11 | 41,383 + | 14,375 (34.74%) |
| Extremely low birth weight (<1000 g) | 7 | 4403 + | 505 (11.47%) |
| APGAR 1min | 7 | 1113 + | 6.8 |
| APGAR 5min | 9 | 1526 + | 8.1 |
| APGAR 5min <7 | 10 | 24,781 + | 2076 (8.38%) |
| Male | 8 | 8573 | 4194 (48.92%) |
Table 5.
Neonatal results of the triplet pregnancies included in the systematic review.
Table 5.
Neonatal results of the triplet pregnancies included in the systematic review.
| Neonatal Results | Number of Studies | Number of Newborns | n (%) |
|---|
| Neonatal intensive care unit | 17 | 5308 | 4177 (78.69%) |
| Respiratory distress | 21 | 6685 | 1906 (28.51%) |
| Hyaline membrane disease | 3 | 191 | 84 (43.98%) |
| Surfactant administration | 5 | 3212 | 729 (22.7%) |
| Bronchopulmonary dysplasia | 15 | 10,148 | 997 (9.82%) |
| Assisted ventilation | 16 | 5845 | 2016 (34.49%) |
| Sepsis | 15 | 5652 | 310 (5.48%) |
| Necrotizing enterocolitis | 17 | 6032 | 102 (1.69%) |
| Retinopaty | 14 | 10,708 | 440.9 (4.12%) |
| Intraventricular hemorrhage III-IV | 22 | 12,923 | 601 (4.65%) |
| Mortality composite | 12 | 9336 | 2103 (22.53%) |
Table 6.
Mortality and morbidity results of the triplet pregnancies included in the systematic review.
Table 6.
Mortality and morbidity results of the triplet pregnancies included in the systematic review.
| Mortality and Morbidity | Number of Studies | Number of Pregnancies *, Fetus or Newborns + | n (%) |
|---|
| Miscarriage <22 weeks | 9 | 3870 * | 187 (4.83%) |
| Intrauterine mortality | 29 | 40,347 + | 2015 (5%) |
| Neonatal mortality | 34 | 44,089 + | 1947.4 (4.42%) |
| Perinatal mortality | 31 | 40,575 + | 700 (1.73%) |
| Maternal mortality | 6 | 721 * | 1 (0.4%) |
| Maternal morbidity | 1 | 35 * | 32 (91.43%) |
Table 7.
Maternal y perinatal characteristics of the triplet pregnancies included in the meta-analysis according to chorionicity.
Table 7.
Maternal y perinatal characteristics of the triplet pregnancies included in the meta-analysis according to chorionicity.
| Maternal and Perinatal Characteristics | Number of Studies | Number of Pregnancies * or Newborns + | Combined OR (CI 95%) | OR Test (p) | Heterogenenicity 12% | Heterogeneicidad χ2 (p) | Egger Test (p) |
|---|
| Reproductive assited techniques | 9 | 1807 * | 3.115 (1.635–5.933) | 0.001 # | 79.7 | 0.000 | 0.034 # |
| Cesarean section | 8 | 1624 * | 1.658 (0.928–2.965) | 0.088 | 30.6 | 0.184 | 0.846 |
| GA <37 weeks | 3 | 1135* | 0.51 (0.25–1.00) | 0.051 | 0.0 | 0.395 | 0.581 |
| GA <32 weeks | 3 | 225* | 0.56 (0.31–1.00) | 0.051 | 0.0 | 0.531 | 0.032 # |
| Very low birth weight (<1500 g) | 3 | 3025+ | 0.68 (0.40–1.14) | 0.144 | 87.2 | 0.000 | 0.892 |
Table 8.
Neonatal results of the triplet pregnancies included in the meta-analysis according to chorionicity.
Table 8.
Neonatal results of the triplet pregnancies included in the meta-analysis according to chorionicity.
| Neonatal Results | Number of Studies | Number of Newborns | Combined OR (CI 95%) | OR Test (p) | Heterogenenicity 12% | Heterogeneicidad χ2 (p) | Egger Test (p) |
|---|
| Neonatal intensive care unit | 4 | 2780 | 0.57 (0.44–0.72) | 0 # | 0.0 | 0.591 | 0.332 |
| Respiratory distress | 5 | 3139 | 0.46 (0.22–0.97) | 0.043 # | 92 | 0.000 | 0.239 |
| Hyaline membrane disease | 3 | 1062 | 0.52 (0.21–1.27) | 0.151 | 67.3 | 0.047 | 0.371 |
| Sepsis | 5 | 3255 | 0.57 (0.37–0.89) | 0.013 # | 23.5 | 0.265 | 0.016 # |
| Necrotizing enterocolitis | 5 | 2979 | 0.32 (0.15–0.69) | 0.003 # | 0.0 | 0.561 | 0.022 # |
| Retinopaty | 4 | 2754 | 0.38 (0.11–1.29) | 0.123 | 64.4 | 0.038 | 0.108 |
| Intraventricular hemorrhage III–IV | 5 | 3086 | 0.34 (0.10–1.21) | 0.097 | 71.3 | 0.007 | 0.386 |
Table 9.
Mortality results of the triplet pregnancies included in the meta-analysis according to chorionicity.
Table 9.
Mortality results of the triplet pregnancies included in the meta-analysis according to chorionicity.
| Mortality | Number of Studies | Number of Live Newborns | Combined OR (CI 95%) | OR Test (p) | Heterogenenicity 12% | Heterogeneicidad χ2 (p) | Egger Test (p) |
|---|
| Intrauterine mortality | 9 | 5367 | 0.29 (0.14–0.62) | 0.001 # | 64.9 | 0.004 | 0.165 |
| Neonatal mortality | 7 | 3906 | 0.53 (0.24–1.16) | 0.114 | 75.8 | 0.000 | 0.224 |
| Perinatal mortality | 10 | 5583 | 0.32 (0.20–0.53) | <0.001 # | 71.1 | 0.000 | 0.882 |