Test-Retest Reliability of Ultrasonographic Measurements from the Rectus Femoris Muscle 1–5 Years after Anterior Cruciate Ligament Reconstruction in the Ipsilateral and Contralateral Legs: An Observational, Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
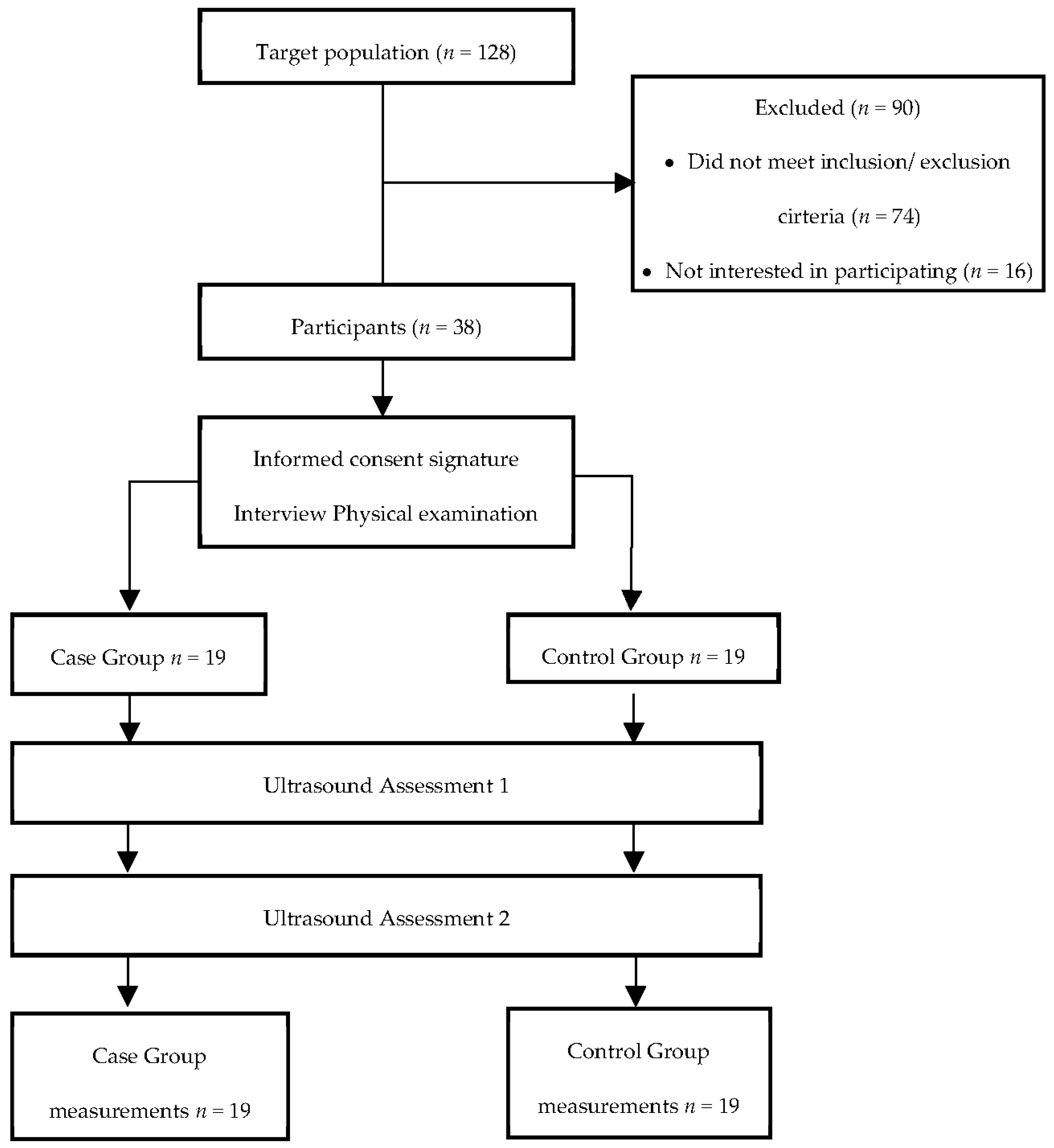
2.2. Participants
2.3. Sample Size
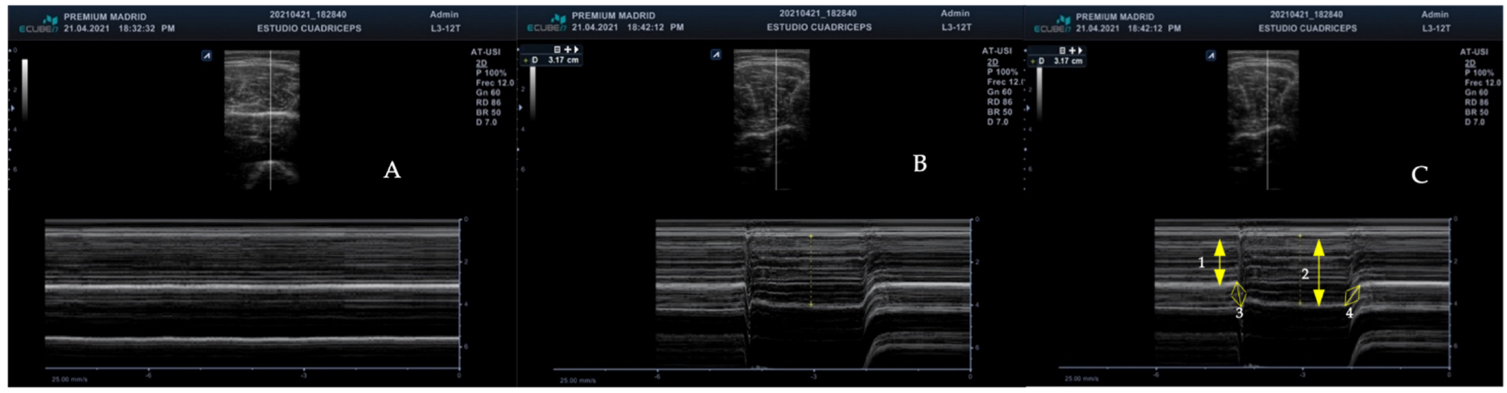
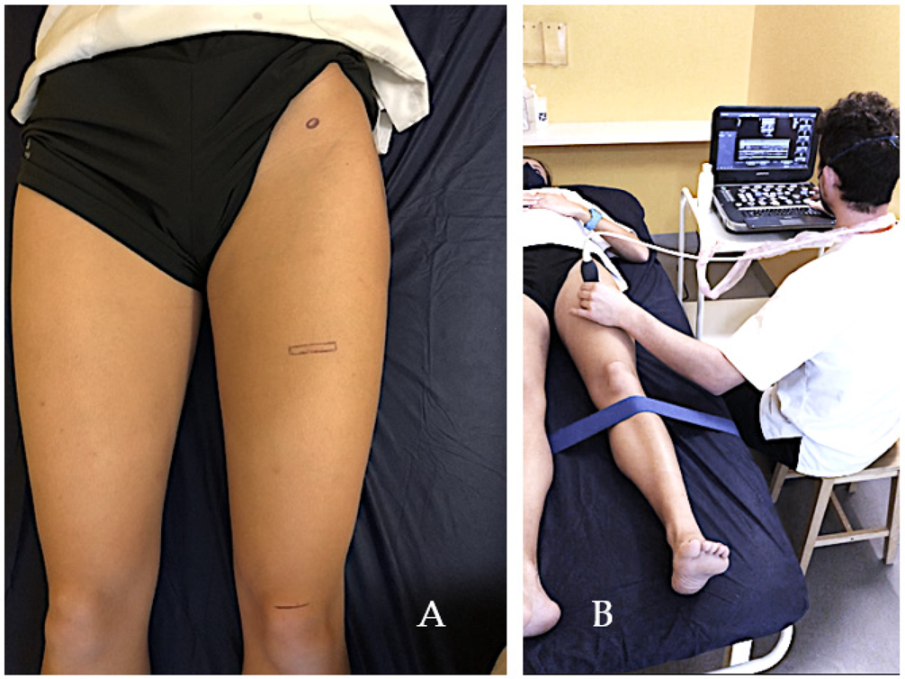
2.3.1. Measurements
2.3.2. Statistical Analysis
3. Results
3.1. Inter-Examiner Reliability
3.2. Differences in Muscle Thickness
3.3. Differences in Contraction and Relaxation Speed
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eurostat. Statistical Office of the European Communities. Sport Statistics—2018 Edition. Available online: https://ec.europa.eu/eurostat/en/web/products-catalogues/-/KS-07-17-123 (accessed on 1 October 2020).
- Eurobarometer, S. Sport and Physical Activity; TNS Opinion & Social: Brussels, Belgium, 2007. [Google Scholar]
- Berko, J. Deaths Attributed to Heat, Cold, and Other Weather Events in the United States, 2006–2010. 2014. Available online: https://books.google.es/books?hl=es&lr=&id=m5nVYLfTOD8C&oi=fnd&pg=PA1&dq=Deaths+attributed+to+heat,+cold,+and+other+weather+events+in+the+United+States,+2006-2010&ots=xtWEPmz_io&sig=pOqsxfk792duUob-jXJu9JIDLLs (accessed on 17 November 2021).
- Thorlund, J.B.; Juhl, C.B.; Roos, E.M.; Lohmander, L.S. Arthroscopic surgery for degenerative knee: Systematic review and meta-analysis of benefits and harms. BMJ 2015, 350, h2747. [Google Scholar] [CrossRef] [Green Version]
- Majewski, M.; Susanne, H.; Klaus, S. Epidemiology of athletic knee injuries: A 10-year study. Knee 2006, 13, 184–188. [Google Scholar] [CrossRef]
- Whittaker, J.L.; Warner, M.B.F.; Stokes, M. Comparison of the sonographic features of the abdominal wall muscles and connective tissues in individuals with and without lumbopelvic pain. J. Orthop. Sports Phys. Ther. 2013, 43, 11–19. Available online: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L368375343 (accessed on 1 October 2020). [CrossRef]
- Whittaker, J.L.; Ellis, R.; Hodges, P.W.; OSullivan, C.; Hides, J.; Fernandez-Carnero, S.; Arias-Buria, J.L.; Teyhen, D.S.; Stokes, M.J. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br. J. Sports Med. 2019, 53, 1447–1453. [Google Scholar] [CrossRef]
- Kiesel, K.B.; Underwood, F.B.; Mattacola, C.G.; Nitz, A.J.; Malone, T.R. A comparison of select trunk muscle thickness change between subjects with low back pain classified in the treatment-based classification system and asymptomatic controls. J. Orthop. Sports Phys. Ther. 2007, 37, 596–607. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=17970406& (accessed on 1 October 2020). [CrossRef] [Green Version]
- Strini, P.J.S.A.; Strini, P.J.S.A.; de Souza Barbosa, T.; Gavião, M.B.D. Assessment of thickness and function of masticatory and cervical muscles in adults with and without temporomandibular disorders. Arch. Oral Biol. 2013, 58, 1100–1108. Available online: http://linkinghub.elsevier.com/retrieve/pii/S0003996913001428 (accessed on 19 September 2018). [CrossRef]
- Koppenhaver, S.L.; Hebert, J.J.; Parent, E.C.; Fritz, J.M. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: A systematic review. Aust. J. Physiother. 2009, 55, 153–169. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=43861690& (accessed on 1 October 2020). [CrossRef] [Green Version]
- Eranki, A.; Cortes, N.; Ferencek, Z.G.; Kim, J.J.; Sikdar, S. Real-time measurement of rectus femoris muscle kinematics during drop jump using ultrasound imaging: A preliminary study. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 4851–4854. [Google Scholar]
- Sikdar, S.; Lebiedowska, M.; Eranki, A.; Garmirian, L.; Damiano, D. Measurement of rectus femoris muscle velocities during patellar tendon jerk using vector tissue Doppler imaging. Bone 2011, 23, 1–7. [Google Scholar]
- Belavý, D.L.; Miokovic, T.; Rittweger, J.; Felsenberg, D. Estimation of changes in volume of individual lower-limb muscles using magnetic resonance imaging (during bed-rest). Physiol. Meas. 2011, 32, 35–50. [Google Scholar] [CrossRef]
- Worsley, P.R.; Kitsell, F.; Samuel, D.; Stokes, M. Validity of measuring distal vastus medialis muscle using rehabilitative ultrasound imaging versus magnetic resonance imaging. Man Ther. 2014, 19, 259–263. [Google Scholar] [CrossRef] [Green Version]
- Brown, A.K.; O’Connor, P.J.; Wakefield, R.J.; Roberts, T.E.; Karim, Z.; Emery, P. Practice, training, and assessment among experts performing musculoskeletal ultrasonography: Toward the development of an international consensus of educational standards for ultrasonography for rheumatologists. Arthritis Care Res. 2004, 51, 1018–1022. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. Available online: http://www.ncbi.nlm.nih.gov/pubmed/18038077 (accessed on 28 September 2019). [CrossRef]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D. The CARE guidelines: Consensus-based clinical case reporting guideline development. BMJ Case Rep. 2013, 7, 223. Available online: https://pubmed.ncbi.nlm.nih.gov/24155002/ (accessed on 19 February 2021).
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Crofts, G.; Angin, S.; Mickle, K.J.; Hill, S.; Nester, C.J. Reliability of ultrasound for measurement of selected foot structures. Gait Posture 2014, 39, 35–39. [Google Scholar] [CrossRef]
- Mechelli, F. Ultrasound imaging for measuring muscle and subcutaneous fat tissue thickness of the anterior thigh: A two-year longitudinal study in middle age. JCSM Clin. Rep. 2019, 4, 3–7. [Google Scholar] [CrossRef]
- Blazevich, A.J.; Gill, N.D.; Zhou, S. Intra- and intermuscular variation in human quadriceps femoris architecture assessed in vivo. J. Anat. 2006, 209, 289–310. Available online: https://pubmed.ncbi.nlm.nih.gov/16928199/ (accessed on 25 January 2022).
- Field, A. Discovering statistics using R. Choice Rev. Online 2012, 50, 50–2114. [Google Scholar]
- Grissom, R.J. Statistical Analysis of Ordinal Categorical Status After Therapies. J. Consult Clin. Psychol. 1994, 62, 281–284. [Google Scholar] [CrossRef]
- Grissom, R.J.; Kim, J.J. Review of assumptions and problems in the appropriate conceptualization of effect size. Psychol. Methods 2001, 6, 135–146. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [PubMed]
- Flansbjer, U.B.; Holmbäck, A.M.; Downham, D.; Patten, C.; Lexell, J. Reliability of gait performance tests in men and women with hemiparesis after stroke. J. Rehabil. Med. 2005, 37, 75–82. [Google Scholar] [PubMed] [Green Version]
- Trevino, M.A.; Sterczala, A.J.; Miller, J.D.; Wray, M.E.; Dimmick, H.L.; Ciccone, A.B.; Weir, J.P.; Gallagher, P.M.; Fry, A.C.; Herda, T.J. Sex-related differences in muscle size explained by amplitudes of higher-threshold motor unit action potentials and muscle fibre typing. Acta Physiol. 2019, 225, e13151. [Google Scholar] [CrossRef] [PubMed]
- Perkisas, S.; Bastijns, S.; Baudry, S.; Bauer, J.; Beaudart, C.; Beckwée, D.; Cruz-Jentoft, A.; Gasowski, J.; Hobbelen, H.; Jager-Wittenaar, H.; et al. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur. Geriatr. Med. 2021, 12, 45–59. Available online: https://pubmed.ncbi.nlm.nih.gov/33387359/ (accessed on 11 November 2021). [CrossRef]
- Hides, J.A.; Richardson, C.A.; Jull, G.A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 1996, 21, 2763–2769. [Google Scholar] [CrossRef]
- Stokes, M.; Rankin, G.; Newham, D.J. Ultrasound imaging of lumbar multifidus muscle: Normal reference ranges for measurements and practical guidance on the technique. Man Ther. 2005, 10, 116–126. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Childs, J.D.; Stokes, M.J.; Wright, A.C.; Dugan, J.L.; George, S.Z. Abdominal and lumbar multifidus muscle size and symmetry at rest and during contracted States. Normative reference ranges. J. Ultrasound Med. 2012, 31, 1099–1110. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=22733859& (accessed on 1 October 2020). [CrossRef]
- Lobo, C.C.; Morales, C.R.; Sanz, D.R.; Corbalán, I.S.; Marín, A.G.; López, D.L. Ultrasonography Comparison of Peroneus Muscle Cross-sectional Area in Subjects With or Without Lateral Ankle Sprains. J. Manip. Physiol. Ther. 2016, 39, 635–644. [Google Scholar] [CrossRef] [Green Version]
- Calvo-Lobo, C.; Almazán-Polo, J.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Palomo-López, P.; Rodríguez-Sanz, D.; López-López, D. Ultrasonography comparison of diaphragm thickness and excursion between athletes with and without lumbopelvic pain. Phys. Ther. Sport 2019, 37, 128–137. [Google Scholar] [CrossRef]
- Fernández-Carnero, S.; Martin-Saborido, C.; Achalandabaso Ochoa-Ruiz de Mendoza, A.; Ferragut-Garcias, A.; Cuenca-Zaldivar, J.N.; Leal-Quiñones, A.; Calvo-Lobo, C.; Gallego-Izquierdo, T. The Role of Rehabilitative Ultrasound Imaging Technique in the Lumbopelvic Region as a Diagnosis and Treatment Tool in Physiotherapy: Systematic Review, Meta-Analysis and Meta-Regression. J. Clin. Med. 2021, 10, 5699. [Google Scholar] [CrossRef]
- Romero-Morales, C.; Calvo-Lobo, C.; Navarro-Flores, E.; Mazoteras-Pardo, V.; García-Bermejo, P.; López-López, D.; Martínez-Jiménez, E.M.; De-la-Cruz-Torres, B. M-Mode Ultrasound Examination of Soleus Muscle in Healthy Subjects: Intra- and Inter-Rater Reliability Study. Healthcare 2020, 8, 555. Available online: https://pubmed.ncbi.nlm.nih.gov/33322505/ (accessed on 15 February 2022). [CrossRef] [PubMed]
- Laursen, P.B. Training for intense exercise performance: High-intensity or high-volume training? Scand J. Med. Sci. Sport 2010, 20 (Suppl. S2), 1–10. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.L.; Baxter, C.J.; Benya, K. Muscle thickness measurements of the lower trapezius with rehabilitative ultrasound imaging are confounded by scapular dyskinesis. Man Ther. 2015, 20, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Seymour, J.M.; Ward, K.; Sidhu, P.S.; Puthucheary, Z.; Steier, J.; Jolley, C.J.; Rafferty, G.; Polkey, M.I.; Moxham, J. Ultrasound measurement of rectus femoris cross-sectional area and the relationship with quadriceps strength in COPD. Thorax 2009, 64, 418–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gellhorn, A.C.; Carlson, M.J. Inter-Rater, Intra-Rater, and Inter-Machine Reliability of Quantitative Ultrasound Measurements of the Patellar Tendon. Ultrasound Med. Biol. 2013, 39, 791–796. [Google Scholar] [CrossRef] [PubMed]
| Variable | Control (n = 19) | Case (n = 19) | p-Value |
|---|---|---|---|
| Age, years | 33.84 (7.00) | 32.47 (9.01) | 0.60 |
| Height, cm | 170.21 (7.83) | 173.47 (7.96) | 0.21 |
| Weight, kg | 69.21 (7.55) | 74.89 (9.09) | 0.04 |
| BMI, kg/m2 | 20.31 (1.78) | 21.56 (2.18) | 0.06 |
| Sex, woman (%) | 9 (47.4) | 3 (15.8) | 0.04 |
| Dominant side, n (%) | |||
| Dominant | 16 (84.2) | 3 (15.8) | |
| Non-dominant | 16 (84.2) | 3 (15.8) | |
| Operated side, n (%) | |||
| Right | 11 (57.9) | - | |
| Left | 8 (42.1) | - | |
| Associated injury, n (%) | |||
| ACL | 15 (39.5) | - | |
| ACL + IM | 2 (10.5) | - | |
| ACL + EM | 2 (10.5) | - | |
| Time, years, median (IQR) | 2 (1.00–3.50) | ||
| IPAQ | 0.10 | ||
| High | 8 (41.1) | 13 (68.4) | |
| Moderate | 11 (57.9) | 6 (31.6) | |
| Low | 0 | 0 |
| Variable | Examiner 1 * | Examiner 2 * | ICC3,3 (95% CI) | SEM (%) | MDC95 (%) |
|---|---|---|---|---|---|
| Resting thickness | |||||
| Right | 2.24 (0.24) | 2.23 (0.24) | 0.99 (0.99–1.00) | 0.03 (1.16%) | 0.07 (3.21%) |
| Left | 2.26 (0.24) | 2.24 (0.24) | 0.99 (0.98–1.00) | 0.03 (1.21%) | 0.08 (3.37%) |
| Contraction thickness | |||||
| Right | 2.72 (0.17) | 2.71 (0.17) | 0.99 (0.99–1.00) | 0.01 (0.46%) | 0.03 (1.28%) |
| Left | 2.69 (0.17) | 2.68 (0.17) | 0.99 (0.99–1.00) | 0.01 (0.33%) | 0.02 (0.90%) |
| Muscle relaxation time | |||||
| Right | 0.98 (0.32) | 0.99 (0.34) | 0.99 (0.96–1.00) | 0.06 (5.78%) | 0.16 (16.01%) |
| Left | 0.89 (0.38) | 0.91 (0.37) | 0.99 (0.98–1.00) | 0.05 (5.54%) | 0.14 (15.36%) |
| Muscle contraction time+ | |||||
| Right | 1.12 (0.37) | 1.13 (0.38) | 0.99 (0.97–1.00) | 0.06 (5.38%) | 0.17 (14.92%) |
| Left | 1.02 (0.45) | 1.05 (0.43) | 0.99 (0.98–1.00) | 0.05 (5.22%) | 0.15 (14.47%) |
| State | Control # | Case # | Difference, Mean (CI 95%) |
|---|---|---|---|
| Operated side | |||
| Rest | 2.26 ± 0.05 | 2.08 ± 0.05 | −0.17 * (−0.33 to −0.02) |
| Contraction | 2.69 ± 0.05 | 2.50 ± 0.05 | −0.19 * (−0.32 to −0.05) |
| Difference, mean (CI 95%) | 0.43 * (0.36 to 0.50) | 0.42 * (0.35 to 0.49) | |
| Non-operated side | |||
| Rest | 2.26 ± 0.05 | 2.22 (0.04) | −0.04 (−0.17 to 0.09) |
| Contraction | 2.69 ± 0.05 | 2.63 (0.04) | −0.06 (−0.19 to 0.07) |
| Difference, mean (CI 95%) | 0.44 * (0.37 to 0.51) | 0.41 * (0.34 to 0.48) | |
| State | Control # | Case # | Difference, Mean (CI 95%) |
|---|---|---|---|
| Operated side | |||
| Contraction | 1.06 ± 0.08 | 0.92 ± 0.08 | −0.15 (−0.38 to 0.09) |
| Rest | 0.93 ± 0.07 | 0.88 ± 0.08 | −0.04 (−0.26 to 0.17) |
| Non-operated side | |||
| Contraction | 1.07 ± 0.08 | 1.02 ± 0.08 | −0.07 (−0.31 to 0.17) |
| Rest | 0.93 ± 0.07 | 0.89 ± 0.07 | −0.04 (−0.25 to 0.17) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buelga-Suarez, J.; Alba-Martin, P.; Cuenca-Zaldívar, N.; García-Escudero, M.; Bierge-Sanclemente, P.; Almazán-Polo, J.; Fernández-Carnero, S.; Pecos-Martín, D. Test-Retest Reliability of Ultrasonographic Measurements from the Rectus Femoris Muscle 1–5 Years after Anterior Cruciate Ligament Reconstruction in the Ipsilateral and Contralateral Legs: An Observational, Case-Control Study. J. Clin. Med. 2022, 11, 1867. https://doi.org/10.3390/jcm11071867
Buelga-Suarez J, Alba-Martin P, Cuenca-Zaldívar N, García-Escudero M, Bierge-Sanclemente P, Almazán-Polo J, Fernández-Carnero S, Pecos-Martín D. Test-Retest Reliability of Ultrasonographic Measurements from the Rectus Femoris Muscle 1–5 Years after Anterior Cruciate Ligament Reconstruction in the Ipsilateral and Contralateral Legs: An Observational, Case-Control Study. Journal of Clinical Medicine. 2022; 11(7):1867. https://doi.org/10.3390/jcm11071867
Chicago/Turabian StyleBuelga-Suarez, Jorge, Pablo Alba-Martin, Nicolas Cuenca-Zaldívar, María García-Escudero, Pilar Bierge-Sanclemente, Jaime Almazán-Polo, Samuel Fernández-Carnero, and Daniel Pecos-Martín. 2022. "Test-Retest Reliability of Ultrasonographic Measurements from the Rectus Femoris Muscle 1–5 Years after Anterior Cruciate Ligament Reconstruction in the Ipsilateral and Contralateral Legs: An Observational, Case-Control Study" Journal of Clinical Medicine 11, no. 7: 1867. https://doi.org/10.3390/jcm11071867
APA StyleBuelga-Suarez, J., Alba-Martin, P., Cuenca-Zaldívar, N., García-Escudero, M., Bierge-Sanclemente, P., Almazán-Polo, J., Fernández-Carnero, S., & Pecos-Martín, D. (2022). Test-Retest Reliability of Ultrasonographic Measurements from the Rectus Femoris Muscle 1–5 Years after Anterior Cruciate Ligament Reconstruction in the Ipsilateral and Contralateral Legs: An Observational, Case-Control Study. Journal of Clinical Medicine, 11(7), 1867. https://doi.org/10.3390/jcm11071867









