Macular Blood Flow and Pattern Electroretinogram in Normal Tension Glaucoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Electroretinography
2.3. OCTA Imaging and VD Measurement
2.4. Statistical Analysis
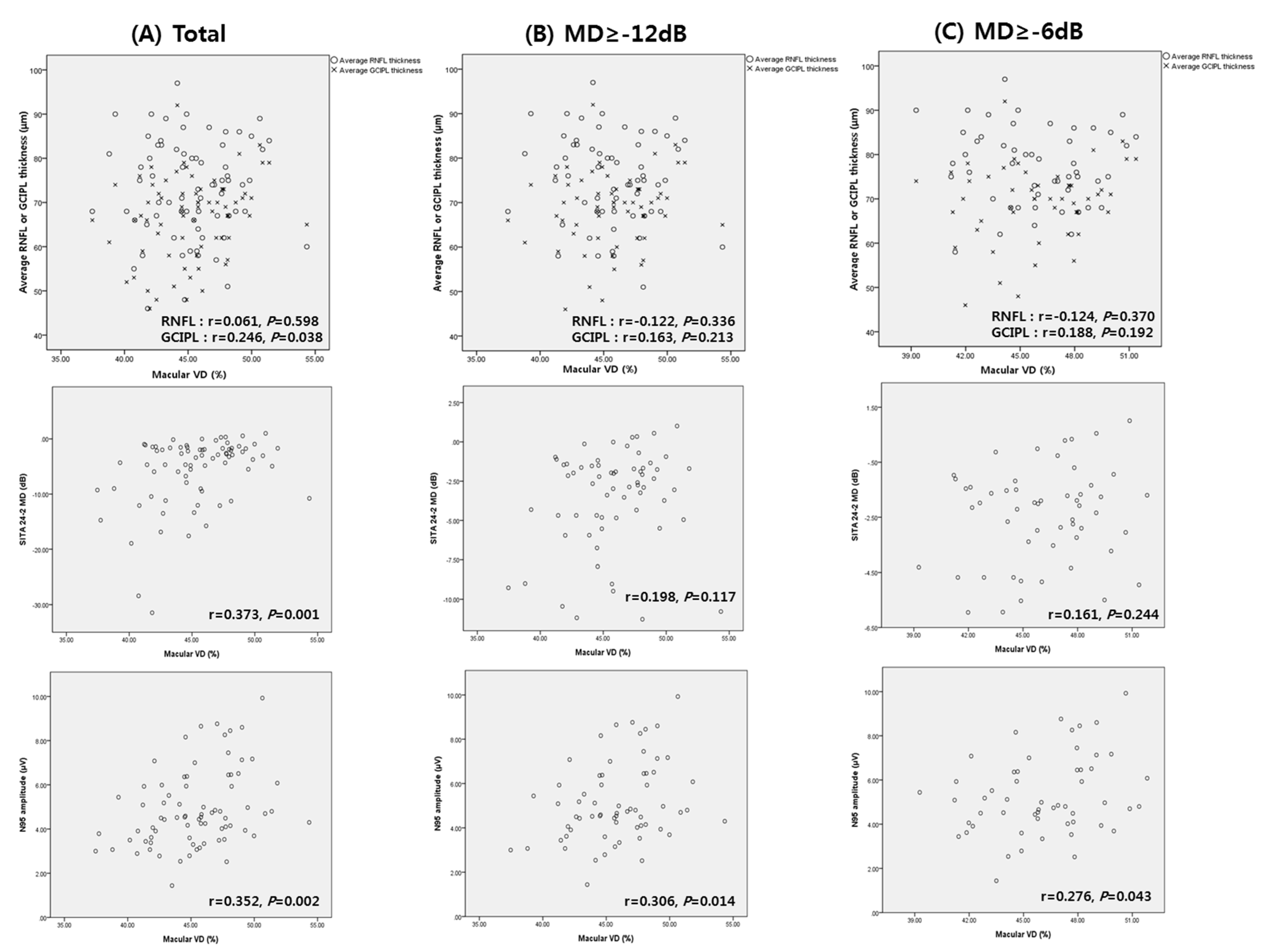
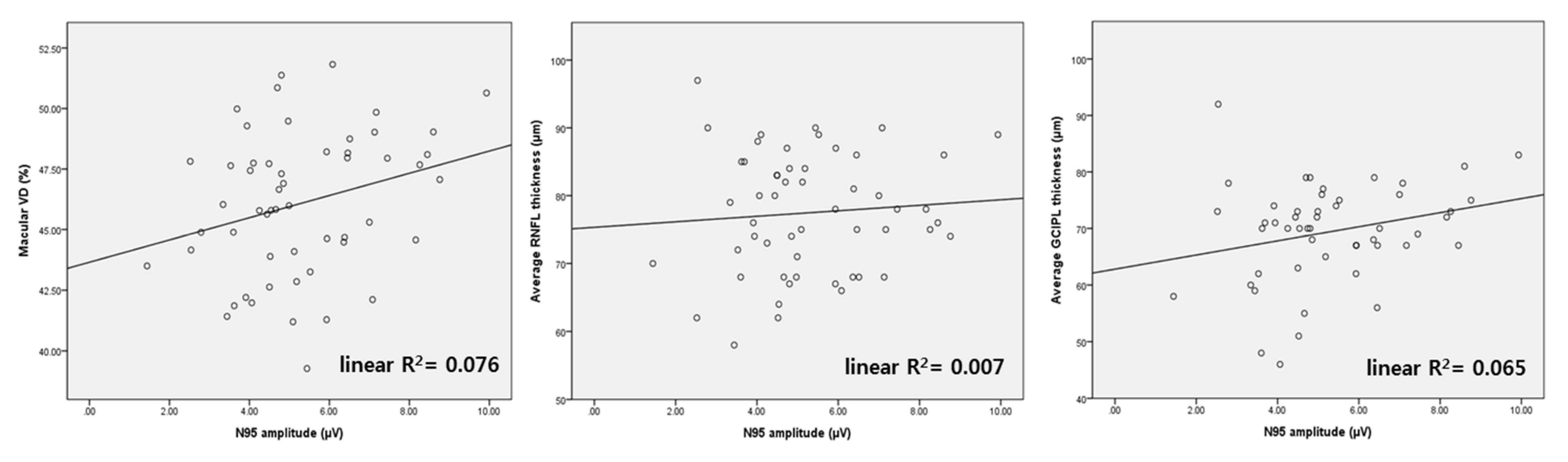
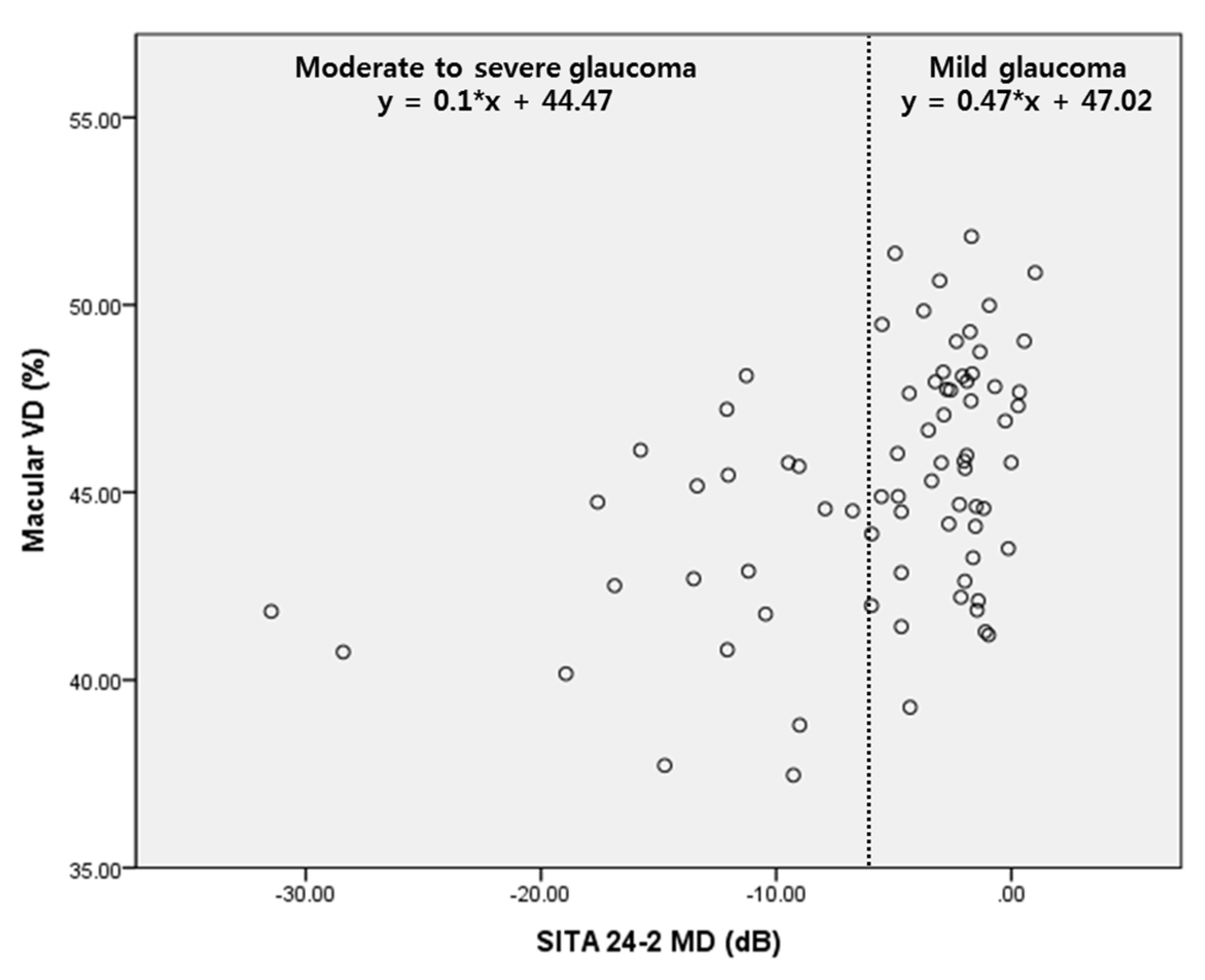
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Foster, P.J.; Buhrmann, R.; Quigley, H.A.; Johnson, G.J. The definition and classification of glaucoma in prevalence surveys. Br. J. Ophthalmol. 2002, 86, 238–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Z.; Medeiros, F.A. Recent developments in visual field testing for glaucoma. Curr. Opin. Ophthalmol. 2018, 29, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, F.A.; Zangwill, L.M.; Bowd, C.; Mansouri, K.; Weinreb, R.N. The structure and function relationship in glaucoma: Implications for detection of progression and measurement of rates of change. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6939–6946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, K.I.; Park, C.K. Detection of Functional Change in Preperimetric and Perimetric Glaucoma Using 10-2 Matrix Perimetry. Am. J. Ophthalmol. 2017, 182, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Ventura, L.M.; Sorokac, N.; De Los Santos, R.; Feuer, W.J.; Porciatti, V. The relationship between retinal ganglion cell function and retinal nerve fiber thickness in early glaucoma. Investig. Ophthalmol. Vis. Sci. 2006, 47, 3904–3911. [Google Scholar] [CrossRef] [Green Version]
- Kerrigan-Baumrind, L.A.; Quigley, H.A.; Pease, M.E.; Kerrigan, D.F.; Mitchell, R.S. Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Investig. Ophthalmol. Vis. Sci. 2000, 41, 741–748. [Google Scholar]
- Chew, S.S.; Kerr, N.M.; Wong, A.B.; Craig, J.P.; Chou, C.Y.; Danesh-Meyer, H.V. Anxiety in visual field testing. Br. J. Ophthalmol. 2016, 100, 1128–1133. [Google Scholar] [CrossRef]
- Glen, F.C.; Baker, H.; Crabb, D.P. A qualitative investigation into patients’ views on visual field testing for glaucoma monitoring. BMJ Open 2014, 4, e003996. [Google Scholar] [CrossRef] [Green Version]
- Phu, J.; Khuu, S.K.; Yapp, M.; Assaad, N.; Hennessy, M.P.; Kalloniatis, M. The value of visual field testing in the era of advanced imaging: Clinical and psychophysical perspectives. Clin. Exp. Optom. 2017, 100, 313–332. [Google Scholar] [CrossRef] [Green Version]
- Berninger, T.A.; Arden, G.B. The pattern electroretinogram. Eye 1988, 2, S257–S283. [Google Scholar] [CrossRef]
- Bach, M.; Poloschek, C.M. Electrophysiology and glaucoma: Current status and future challenges. Cell Tissue Res. 2013, 353, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Bach, M.; Unsoeld, A.S.; Philippin, H.; Staubach, F.; Maier, P.; Walter, H.S.; Bomer, T.G.; Funk, J. Pattern ERG as an early glaucoma indicator in ocular hypertension: A long-term, prospective study. Investig. Ophthalmol. Vis. Sci 2006, 47, 4881–4887. [Google Scholar]
- Wilsey, L.J.; Fortune, B. Electroretinography in glaucoma diagnosis. Curr. Opin. Ophthalmol. 2016, 27, 118–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jafarzadehpour, E.; Radinmehr, F.; Pakravan, M.; Mirzajani, A.; Yazdani, S. Pattern electroretinography in glaucoma suspects and early primary open angle glaucoma. J. Ophthalm. Vis. Res. 2013, 8, 199–206. [Google Scholar]
- Jung, K.I.; Jeon, S.; Shin, D.Y.; Lee, J.; Park, C.K. Pattern Electroretinograms in Preperimetric and Perimetric Glaucoma. Am. J. Ophthalmol. 2020, 215, 118–126. [Google Scholar] [CrossRef]
- Jeon, S.J.; Park, H.L.; Jung, K.I.; Park, C.K. Relationship between pattern electroretinogram and optic disc morphology in glaucoma. PLoS ONE 2019, 14, e0220992. [Google Scholar] [CrossRef] [Green Version]
- Yarmohammadi, A.; Zangwill, L.M.; Diniz-Filho, A.; Suh, M.H.; Manalastas, P.I.; Fatehee, N.; Yousefi, S.; Belghith, A.; Saunders, L.J.; Medeiros, F.A.; et al. Optical Coherence Tomography Angiography Vessel Density in Healthy, Glaucoma Suspect, and Glaucoma Eyes. Investig. Ophthalmol. Vis. Sci. 2016, 57, OCT451–OCT459. [Google Scholar] [CrossRef]
- Wang, X.; Jiang, C.; Ko, T.; Kong, X.; Yu, X.; Min, W.; Shi, G.; Sun, X. Correlation between optic disc perfusion and glaucomatous severity in patients with open-angle glaucoma: An optical coherence tomography angiography study. Graefes Arch. Clin. Exp. Ophthalmol. 2015, 253, 1557–1564. [Google Scholar] [CrossRef]
- Wu, J.; Sebastian, R.T.; Chu, C.J.; McGregor, F.; Dick, A.D.; Liu, L. Reduced Macular Vessel Density and Capillary Perfusion in Glaucoma Detected Using OCT Angiography. Curr. Eye Res. 2019, 44, 533–540. [Google Scholar] [CrossRef] [Green Version]
- Yarmohammadi, A.; Zangwill, L.M.; Diniz-Filho, A.; Suh, M.H.; Yousefi, S.; Saunders, L.J.; Belghith, A.; Manalastas, P.I.; Medeiros, F.A.; Weinreb, R.N. Relationship between Optical Coherence Tomography Angiography Vessel Density and Severity of Visual Field Loss in Glaucoma. Ophthalmology 2016, 123, 2498–2508. [Google Scholar] [CrossRef] [Green Version]
- Mills, R.P.; Budenz, D.L.; Lee, P.P.; Noecker, R.J.; Walt, J.G.; Siegartel, L.R.; Evans, S.J.; Doyle, J.J. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am. J. Ophthalmol. 2006, 141, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Vigo, J.I.; Kudsieh, B.; Shi, H.; Arriola-Villalobos, P.; Donate-Lopez, J.; Garcia-Feijoo, J.; Ruiz-Moreno, J.M.; Fernandez-Vigo, J.A. Normative database and determinants of macular vessel density measured by optical coherence tomography angiography. Clin. Exp. Ophthalmol. 2020, 48, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, F.A.; Alencar, L.M.; Zangwill, L.M.; Bowd, C.; Sample, P.A.; Weinreb, R.N. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch. Ophthalmol. 2009, 127, 1250–1256. [Google Scholar]
- Harwerth, R.S.; Carter-Dawson, L.; Smith, E.L., 3rd; Barnes, G.; Holt, W.F.; Crawford, M.L. Neural losses correlated with visual losses in clinical perimetry. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3152–3160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hood, D.C.; Kardon, R.H. A framework for comparing structural and functional measures of glaucomatous damage. Prog. Retin. Eye Res. 2007, 26, 688–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ventura, L.M.; Porciatti, V. Restoration of retinal ganglion cell function in early glaucoma after intraocular pressure reduction: A pilot study. Ophthalmology 2005, 112, 20–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yarmohammadi, A.; Zangwill, L.M.; Diniz-Filho, A.; Saunders, L.J.; Suh, M.H.; Wu, Z.; Manalastas, P.I.C.; Akagi, T.; Medeiros, F.A.; Weinreb, R.N. Peripapillary and Macular Vessel Density in Patients with Glaucoma and Single-Hemifield Visual Field Defect. Ophthalmology 2017, 124, 709–719. [Google Scholar] [CrossRef] [Green Version]
- Gaier, E.D.; Wang, M.; Gilbert, A.L.; Rizzo, J.F., 3rd; Cestari, D.M.; Miller, J.B. Quantitative analysis of optical coherence tomographic angiography (OCT-A) in patients with non-arteritic anterior ischemic optic neuropathy (NAION) corresponds to visual function. PLoS ONE 2018, 13, e0199793. [Google Scholar] [CrossRef]
- Shoji, T.; Zangwill, L.M.; Akagi, T.; Saunders, L.J.; Yarmohammadi, A.; Manalastas, P.I.C.; Penteado, R.C.; Weinreb, R.N. Progressive Macula Vessel Density Loss in Primary Open-Angle Glaucoma: A Longitudinal Study. Am. J. Ophthalmol. 2017, 182, 107–117. [Google Scholar] [CrossRef]
- Hou, H.; Moghimi, S.; Proudfoot, J.A.; Ghahari, E.; Penteado, R.C.; Bowd, C.; Yang, D.; Weinreb, R.N. Ganglion Cell Complex Thickness and Macular Vessel Density Loss in Primary Open-Angle Glaucoma. Ophthalmology 2020, 127, 1043–1052. [Google Scholar] [CrossRef]
- Baltan, S.; Inman, D.M.; Danilov, C.A.; Morrison, R.S.; Calkins, D.J.; Horner, P.J. Metabolic vulnerability disposes retinal ganglion cell axons to dysfunction in a model of glaucomatous degeneration. J. Neurosci. 2010, 30, 5644–5652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swanson, R.A.; Sagar, S.M.; Sharp, F.R. Regional brain glycogen stores and metabolism during complete global ischaemia. Neurol. Res. 1989, 11, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Seo, D.R.; Kim, J.Y.; Choi, W.; Lee, S.Y.; Lee, J.M.; Seong, G.J.; Kim, C.Y.; Bae, H.W. Relationship between N95 Amplitude of Pattern Electroretinogram and Optical Coherence Tomography Angiography in Open-Angle Glaucoma. J. Clin. Med. 2020, 9, 3854. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Son, N.H.; Bae, H.W.; Seong, G.J.; Kim, C.Y. The role of pattern electroretinograms and optical coherence tomography angiography in the diagnosis of normal-tension glaucoma. Sci. Rep. 2021, 11, 12257. [Google Scholar] [CrossRef] [PubMed]
- Barry, C.J.; Cooper, R.L.; Eikelboom, R.H. Optic disc haemorrhages and vascular abnormalities in a glaucoma population. Aust. N. Z. J. Ophthalmol. 1997, 25, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Leung, D.Y.; Tham, C.C.; Li, F.C.; Kwong, Y.Y.; Chi, S.C.; Lam, D.S. Silent cerebral infarct and visual field progression in newly diagnosed normal-tension glaucoma: A cohort study. Ophthalmology 2009, 116, 1250–1256. [Google Scholar] [CrossRef]
- Suzuki, J.; Tomidokoro, A.; Araie, M.; Tomita, G.; Yamagami, J.; Okubo, T.; Masumoto, T. Visual field damage in normal-tension glaucoma patients with or without ischemic changes in cerebral magnetic resonance imaging. Jpn. J. Ophthalmol. 2004, 48, 340–344. [Google Scholar] [CrossRef]
| Age (years) | 57.47 (±12.78) |
| Axial length (mm) | 25.26 (±1.70) |
| Male:Female | 33:45 |
| Hypertension | 21 (27.63%) |
| Diabetes | 6 (7.89%) |
| Systemic vascular dysregulation * | 14 (18.42%) |
| Disc hemorrhage | 5 (6.58%) |
| Intraocular pressure (mmHg) | 14.07 (±2.63) |
| SITA 24-2 MD (dB) | −5.70 (±6.27) |
| SITA 24-2 PSD (dB) | 5.44 (±4.25) |
| Average RNFL thickness (μm) | 73.16 (±11.22) |
| Average GCIPL thickness (μm) | 66.79 (±9.38) |
| Pattern ERG | |
| P50 latency (ms) | 50.41 (±3.53) |
| N95 latency (ms) | 102.42 (±7.34) |
| P50 amplitude (μV) | 2.83 (±0.92) |
| N95 amplitude (μV) | 4.92 (±1.75) |
| Macular VD (%) | |
| Superior | 47.91 (±5.29) |
| Nasal | 42.34 (±5.96) |
| Inferior | 47.48 (±5.67) |
| Temporal | 43.73 (±4.23) |
| FAZ | 14.71 (±5.36) |
| Average (excluding FAZ) † | 45.36 (±3.39) |
| Higher VD (n = 36) | Lower VD (n = 28) | p Value | |
|---|---|---|---|
| Average RNFL thickness (μm) | 73.92 (±9.74) | 77.75 (±10.22) | 0.132 |
| Average GCIPL thickness (μm) | 68.97 (±6.97) | 68.14 (±10.07) | 0.711 |
| SITA 24-2 MD (dB) | −2.99 (±3.00) | −4.23 (±3.12) | 0.346 |
| SITA 24-2 PSD (dB) | 3.92 (±3.17) | 4.52 (±3.21) | 0.632 |
| Pattern ERG | |||
| P50 latency (ms) | 50.35 (±3.31) | 50.91 (±3.49) | 0.514 |
| N95 latency (ms) | 103.60 (±7.71) | 101.19 (±7.18) | 0.206 |
| P50 amplitude (μV) | 2.95 (±1.01) | 2.75 (±0.93) | 0.415 |
| N95 amplitude (μV) | 5.52 (±1.88) | 4.65 (±1.56) | 0.048 * |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| ß ± SE | p Value | ß ± SE | p Value | |
| Average RNFL thickness | 0.019 ± 0.035 | 0.598 | ||
| Average GCIPL thickness | 0.085 ± 0.040 | 0.038 * | 0.013 ± 0.049 | 0.798 |
| SITA 24-2 MD | 0.202 ± 0.058 | 0.001 * | 0.170 ± 0.088 | 0.057 |
| SITA 24-2 PSD | −0.216 ± 0.089 | 0.018 * | 0.131 ± 0.128 | 0.308 |
| Pattern ERG | ||||
| P50 latency | −0.094 ± 0.111 | 0.402 | ||
| N95 latency | 0.016 ± 0.054 | 0.77 | ||
| P50 amplitude | 0.696 ± 0.420 | 0.102 | ||
| N95 amplitude | 0.683 ± 0.211 | 0.002 * | 0.498 ± 0.231 | 0.035 * |
| Univariate | Multivariate Model 1 | Multivariate Model 2 | Multivariate Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| ß ± SE | p Value | ß ± SE | p Value | ß ± SE | p Value | ß ± SE | p Value | |
| Average RNFL thickness | −0.040 ± 0.041 | 0.336 | −0.091 ± 0.047 | 0.058 | ||||
| Average GCIPL thickness | 0.063 ± 0.050 | 0.213 | 0.086 ± 0.057 | 0.138 | ||||
| SITA 24-2 MD | 0.212 ± 0.133 | 0.117 | 0.171 ± 0.136 | 0.212 | 0.139 ± 0.133 | 0.301 | ||
| SITA 24-2 PSD | −0.120 ± 0.132 | 0.364 | ||||||
| Pattern ERG | ||||||||
| P50 latency | −0.149 ± 0.123 | 0.231 | ||||||
| N95 latency | 0.035 ± 0.056 | 0.528 | ||||||
| P50 amplitude | 0.702 ± 0.424 | 0.103 | 0.580 ± 0.433 | 0.185 | ||||
| N95 amplitude | 0.568 ± 0.224 | 0.014 * | 0.509 ± 0.231 | 0.032 * | 0.510 ± 0.234 | 0.033 * | ||
| Univariate | Multivariate | |||
|---|---|---|---|---|
| ß ± SE | p Value | ß ± SE | p Value | |
| Average RNFL thickness | 0.039 ± 0.018 | 0.030 * | 0.019 ± 0.022 | 0.383 |
| Average GCIPL thickness | 0.076 ± 0.021 | 0.001 * | 0.049 ± 0.027 | 0.074 |
| Macular VD | ||||
| Superior | 0.133 ± 0.035 | <0.001 * | ||
| Nasal | 0.022 ± 0.034 | 0.521 | ||
| Inferior | 0.058 ± 0.035 | 0.106 | ||
| Temporal | 0.113 ± 0.046 | 0.017 * | ||
| FAZ | −0.045 ± 0.038 | 0.230 | ||
| Average (excluding FAZ) † | 0.181 ± 0.056 | 0.002 * | 0.148 ± 0.061 | 0.019 * |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| ß ± SE | p Value | ß ± SE | p Value | |
| Average RNFL thickness | 0.020 ± 0.022 | 0.377 | ||
| Average GCIPL thickness | 0.064 ± 0.027 | 0.020 * | 0.055 ± 0.026 | 0.042 * |
| Macular VD | ||||
| Superior | 0.137 ± 0.041 | 0.001 * | ||
| Nasal | 0.032 ± 0.036 | 0.376 | ||
| Inferior | 0.020 ± 0.044 | 0.644 | ||
| Temporal | 0.105 ± 0.052 | 0.046 * | ||
| FAZ | −0.017 ± 0.044 | 0.697 | ||
| Average (excluding FAZ) † | 0.165 ± 0.065 | 0.014 * | 0.143 ± 0.068 | 0.040 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, S.J.; Jung, K.I.; Park, C.K.; Park, H.-Y.L. Macular Blood Flow and Pattern Electroretinogram in Normal Tension Glaucoma. J. Clin. Med. 2022, 11, 1790. https://doi.org/10.3390/jcm11071790
Jeon SJ, Jung KI, Park CK, Park H-YL. Macular Blood Flow and Pattern Electroretinogram in Normal Tension Glaucoma. Journal of Clinical Medicine. 2022; 11(7):1790. https://doi.org/10.3390/jcm11071790
Chicago/Turabian StyleJeon, Soo Ji, Kyoung In Jung, Chan Kee Park, and Hae-Young Lopilly Park. 2022. "Macular Blood Flow and Pattern Electroretinogram in Normal Tension Glaucoma" Journal of Clinical Medicine 11, no. 7: 1790. https://doi.org/10.3390/jcm11071790
APA StyleJeon, S. J., Jung, K. I., Park, C. K., & Park, H.-Y. L. (2022). Macular Blood Flow and Pattern Electroretinogram in Normal Tension Glaucoma. Journal of Clinical Medicine, 11(7), 1790. https://doi.org/10.3390/jcm11071790






