Future Perspectives in Oxidative Stress in Trisomy 13 and 18 Evaluation
Abstract
1. Introduction
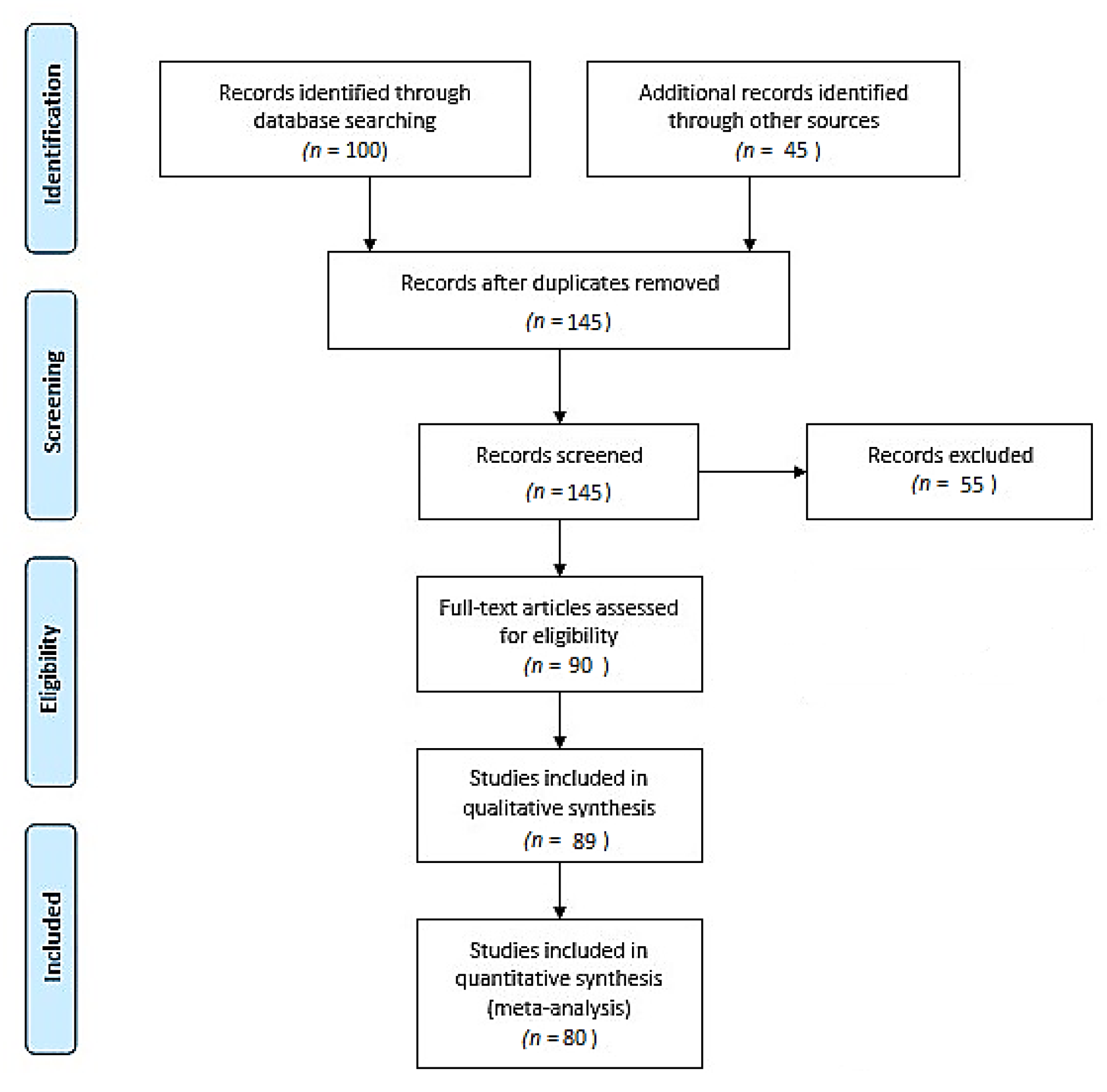
2. Materials and Methods
3. Oxidative Stress: An Overview
4. Previously Established T13 and T18 Pathogenesis—An Indicator for Oxidative Stress Testing
5. Genetic Basis of the T13 and T18 Pathogeneses
6. Uncoupling Oxidative Stress from the Pathogenesis of Trisomies: Future Perspectives
6.1. Oxidative Stress and Lipid Peroxidation
6.2. Mitochondrial Dysfunction
6.3. Oxidative Stress Meets Epigenetics: An Implication in Trisomy Development
7. Perspectives
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Satgé, D.; Nishi, M.; Sirvent, N.; Vekemans, M. A tumor profile in Edwards syndrome (trisomy 18). Am. J. Med. Genet. Part C Semin. Med. Genet. 2016, 172, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Goel, N.; Morris, J.K.; Tucker, D.; De Walle, H.E.K.; Bakker, M.K.; Kancherla, V.; Marengo, L.; Canfield, M.A.; Kallen, K.; Lelong, N.; et al. Trisomy 13 and 18—Prevalence and mortality—A multi-registry population based analysis. Am. J. Med. Genet. Part A 2019, 179, 2382–2392. [Google Scholar] [CrossRef] [PubMed]
- McCaffrey, M.J. Trisomy 13 and 18: Selecting the road previously not taken. Am. J. Med. Genet. Part C Semin. Med. Genet. 2016, 172, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Sifakis, S.; Anagnostopoulou, K.; Plastira, K.; Vrachnis, N.; Konstantinidou, A.; Sklavounou, E. Rare case of XX/XY mosaicism and trisomy 13 in early prenatal diagnosis. Birth Defects Res. Part A Clin. Mol. Teratol. 2012, 94, 245–248. [Google Scholar] [CrossRef]
- Kuznetsova, M.A.; Zaytseva, G.V.; Zryachkin, N.I.; Makarova, O.A.; Khmilevskaya, S.A. Patau Syndrome. Clin. Pract. Pediatrics 2021, 10, 90–93. [Google Scholar] [CrossRef]
- Cereda, A.; Carey, J.C. The trisomy 18 syndrome. Orphanet J. Rare Dis. 2012, 7, 81. [Google Scholar] [CrossRef]
- Balasundaram, P.; Avulakunta, I.D. Edward Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Pont, S.J.; Robbins, J.; Bird, T.; Gibson, J.B.; Cleves, M.A.; Tilford, J.M.; Aitken, M.E. Congenital malformations among liveborn infants with trisomies 18 and 13. Am. J. Med. Genet. Part A 2006, 140A, 1749–1756. [Google Scholar] [CrossRef]
- Peterson, J.; Kochilas, L.K.; Catton, K.G.; Moller, J.H.; Setty, S.P. Long-Term Outcomes of Children With Trisomy 13 and 18 After Congenital Heart Disease Interventions. Ann. Thorac. Surg. 2017, 103, 1941–1949. [Google Scholar] [CrossRef]
- Roberts, W.; Żurada, A.; Zurada-Zielińska, A.; Gielecki, J.; Loukas, M. Anatomy of trisomy 18. Clin. Anat. 2016, 29, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.K.; Savva, G.M. The risk of fetal loss following a prenatal diagnosis of trisomy 13 or trisomy 18. Am. J. Med. Genet. Part A 2008, 146A, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.E.; Punnett, H.H.; Huff, V.; De Chadarévian, J.-P. Characterization of a Wilms tumor in a 9-year-old girl with trisomy 18. Am. J. Med. Genet. Part A 2003, 121A, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Jafri, I. Characterization of a 16-Year-Old Long-Time Survivor of Edwards Syndrome. Cureus 2021, 13, e15205. [Google Scholar] [CrossRef]
- Petek, E.; Pertl, B.; Tschernigg, M.; Bauer, M.; Mayr, J.; Wagner, K.; Kroisel, P.M. Characterisation of a 19-year-old “long-term survivor” with Edwards syndrome. Genet. Couns. 2003, 14, 239–244. [Google Scholar] [PubMed]
- Zoll, B.; Wolf, J.; Lensing-Hebben, D.; Pruggmayer, M.; Thorpe, B. Trisomy 13 (Patau syndrome) with an 11-year survival. Clin. Genet. 1993, 43, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Iliopoulos, D.; Sekerli, E.; Vassiliou, G.; Sidiropoulou, V.; Topalidis, A.; Dimopoulou, D.; Voyiatzis, N. Patau syndrome with a long survival (146 months): A clinical report and review of literature. Am. J. Med. Genet. Part A 2005, 140, 92–93. [Google Scholar] [CrossRef]
- Fogu, G.; Maserati, E.; Cambosu, F.; Moro, M.A.; Poddie, F.; Soro, G.; Bandiera, P.; Serra, G.; Tusacciu, G.; Sanna, G.; et al. Patau syndrome with long survival in a case of unusual mosaic trisomy 13. Eur. J. Med. Genet. 2008, 51, 303–314. [Google Scholar] [CrossRef] [PubMed]
- Arita, A.; Costa, M. Genetics and Genome Research Oxidative Stress and the Epigenome in Human Disease. J. Genet. Genome Res. 2014, 1, 2. [Google Scholar]
- Rosa, R.F.M.; Rosa, R.C.M.; Zen, P.; Graziadio, C.; Paskulin, G.A. Trisomy 18: Review of the clinical, etiologic, prognostic, and ethical aspects. Rev. Paul. Pediatr. 2013, 31, 111–120. [Google Scholar] [CrossRef][Green Version]
- Cammarata-Scalisi, F.; Lacruz-Rengel, M.A.; Araque, D.; Da Silva, G.; Avendaño, A.; Callea, M.; Stock, F.; Guerrero, Y.; Aguilar, E.; Lacruz, M.J.; et al. Mosaic trisomy 18. Series of cases. Arch. Argent. Pediatr. 2017, 115, e183–e186. [Google Scholar] [CrossRef] [PubMed]
- Abe, K.; Itoh, N.H.; Hirakawa, O.; Niikawa, N. Trisomy 13/trisomy 18 mosaicism in an infant. Clin. Genet. 1996, 50, 300–303. [Google Scholar] [CrossRef]
- Perluigi, M.; di Domenico, F.; Fiorini, A.; Cocciolo, A.; Giorgi, A.; Foppoli, C.; Butterfield, D.A.; Giorlandino, M.; Giorlandino, C.; Schininà, M.E.; et al. Oxidative stress occurs early in Down syndrome pregnancy: A redox proteomics analysis of amniotic fluid. Proteom.—Clin. Appl. 2011, 5, 167–178. [Google Scholar] [CrossRef]
- Laforgia, N.; Di Mauro, A.; Guarnieri, G.F.; Varvara, D.; De Cosmo, L.; Panza, R.; Capozza, M.; Baldassarre, M.E.; Resta, N. The Role of Oxidative Stress in the Pathomechanism of Congenital Malformations. Oxidative Med. Cell. Longev. 2018, 2018, 7404082. [Google Scholar] [CrossRef] [PubMed]
- Roper, R.J.; Reeves, R.H. Understanding the Basis for Down Syndrome Phenotypes. PLoS Genet. 2006, 2, e50. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, K.; Archer, K.J.; Turner, K.; Brown, R.; Jackson-Cook, C. Trisomy 21-associated increases in chromosomal instability are unmasked by comparing isogenic trisomic/disomic leukocytes from people with mosaic Down syndrome. PLoS ONE 2021, 16, e0254806. [Google Scholar] [CrossRef] [PubMed]
- Perluigi, M.; Butterfield, D.A. Oxidative Stress and Down Syndrome: A Route toward Alzheimer-Like Dementia. Curr. Gerontol. Geriatr. Res. 2012, 2012, 724904. [Google Scholar] [CrossRef] [PubMed]
- Barone, E.; Arena, A.; Head, E.; Butterfield, D.A.; Perluigi, M. Disturbance of redox homeostasis in Down Syndrome: Role of iron dysmetabolism. Free Radic. Biol. Med. 2018, 114, 84–93. [Google Scholar] [CrossRef]
- Izzo, A.; Mollo, N.; Nitti, M.; Paladino, S.; Calì, G.; Genesio, R.; Bonfiglio, F.; Cicatiello, R.; Barbato, M.; Sarnataro, V.; et al. Mitochondrial dysfunction in down syndrome: Molecular mechanisms and therapeutic targets. Mol. Med. 2018, 24, 2. [Google Scholar] [CrossRef] [PubMed]
- Muchová, J.; Žitňanová, I.; Ďuračková, Z. Oxidative stress and Down syndrome. do antioxidants play a role in therapy? Physiol. Res. 2014, 63, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.-Y.; Lin, H.; Hung, H.-N.; Yang, K.D.; Ou, C.-Y.; Tsai, C.-C.; Cheng, H.-H.; Chung, S.-H.; Cheng, B.-H.; Wong, Y.-H.; et al. Two-Dimensional Differential Gel Electrophoresis to Identify Protein Biomarkers in Amniotic Fluid of Edwards Syndrome (Trisomy 18) Pregnancies. PLoS ONE 2016, 11, e0145908. [Google Scholar] [CrossRef] [PubMed]
- Vrachnis, N.; Dalakli, E.; Zygouris, D.; Vlachadis, N.; Salakos, N.; Botsis, D.; Kalantaridou, S.; Drakoulis, N.; Mastorakos, G.; Creatsas, G.; et al. Altered Resistin Concentrations in Mid-trimester Amniotic Fluid of Fetuses With Trisomies 18 and 13: A Window onto the Pathophysiology of Trisomies 18 and 13. In Vivo 2019, 33, 433–439. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef] [PubMed]
- Buczyńska, A.; Sidorkiewicz, I.; Rogucki, M.; Siewko, K.; Adamska, A.; Kościuszko, M.; Maliszewska, K.; Kozłowska, G.; Szumowski, P.; Myśliwiec, J.; et al. Oxidative stress and radioiodine treatment of differentiated thyroid cancer. Sci. Rep. 2021, 11, 17126. [Google Scholar] [CrossRef] [PubMed]
- Zorov, D.B.; Juhaszova, M.; Sollott, S.J. Mitochondrial Reactive Oxygen Species (ROS) and ROS-Induced ROS Release. Physiol. Rev. 2014, 94, 909–950. [Google Scholar] [CrossRef]
- Fernandez-Marcos, P.J.; Nóbrega-Pereira, S. NADPH: New oxygen for the ROS theory of aging. Oncotarget 2016, 7, 50814–50815. [Google Scholar] [CrossRef]
- Bartesaghi, R.; Haydar, T.F.; Delabar, J.M.; Dierssen, M.; Martínez-Cué, C.; Bianchi, D.W. New Perspectives for the Rescue of Cognitive Disability in Down Syndrome. J. Neurosci. 2015, 35, 13843–13852. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.T.; Beal, M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 2006, 443, 787–795. [Google Scholar] [CrossRef]
- Guo, C.; Sun, L.; Chen, X.; Zhang, D. Oxidative stress, mitochondrial damage and neurodegenerative diseases. Neural Regen. Res. 2013, 8, 2003–2014. [Google Scholar] [CrossRef]
- Capone, G.; Kim, P.; Jovanovich, S.; Payne, L.; Freund, L.; Welch, K.; Miller, E.; Trush, M. Evidence for increased mitochondrial superoxide production in Down syndrome. Life Sci. 2002, 70, 2885–2895. [Google Scholar] [CrossRef]
- Laudanski, P.; Zbucka-Kretowska, M.; Charkiewicz, K.; Wolczynski, S.; Wojcik, D.; Charkiewicz, R. Maternal Plasma and Amniotic Fluid Chemokines Screening in Fetal Down Syndrome. Mediat. Inflamm. 2014, 2014, 835837. [Google Scholar] [CrossRef] [PubMed]
- Mange, A.; Desmetz, C.; Bellet, V.; Molinari, N.; Maudelonde, T.; Solassol, J. Proteomic profile determination of autosomal aneuploidies by mass spectrometry on amniotic fluids. Proteome Sci. 2008, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Underwood, M.A.; Gilbert, W.M.; Sherman, M.P. Amniotic Fluid: Not Just Fetal Urine Anymore. J. Perinatol. 2005, 25, 341–348. [Google Scholar] [CrossRef]
- Zbucka-Kretowska, M.; Charkiewicz, K.; Czerniecki, J.; Goscik, J.; Wolczynski, S.; Laudanski, P. Amniotic Fluid Angiogenic and Inflammatory Factor Profiling in Foetal Down Syndrome. Fetal Diagn. Ther. 2017, 44, 44–50. [Google Scholar] [CrossRef]
- Buczyńska, A.; Sidorkiewicz, I.; Ławicki, S.; Krętowski, A.; Zbucka-Krętowska, M. The Significance of Apolipoprotein E Measurement in the Screening of Fetal Down Syndrome. J. Clin. Med. 2020, 9, 3995. [Google Scholar] [CrossRef]
- Buczyńska, A.; Sidorkiewicz, I.; Trochimiuk, A.; Ławicki, S.; Krętowski, A.J.; Zbucka-Krętowska, M. Novel Approaches to an Integrated Route for Trisomy 21 Evaluation. Biomolecules 2021, 11, 1328. [Google Scholar] [CrossRef]
- Sheppard, O.; Wiseman, F.K.; Ruparelia, A.; Tybulewicz, V.L.J.; Fisher, E.M.C. Mouse Models of Aneuploidy. Sci. World J. 2012, 2012, 214078. [Google Scholar] [CrossRef]
- Laurikka, A.; Vuolteenaho, K.; Toikkanen, V.; Rinne, T.; Leppänen, T.; Tarkka, M.; Laurikka, J.; Moilanen, E. Adipocytokine resistin correlates with oxidative stress and myocardial injury in patients undergoing cardiac surgery. Eur. J. Cardio-Thoracic Surg. 2014, 46, 729–736. [Google Scholar] [CrossRef]
- Chen, C.; Jiang, J.; Lu, J.-M.; Chai, H.; Wang, X.; Lin, P.H.; Yao, Q. Resistin decreases expression of endothelial nitric oxide synthase through oxidative stress in human coronary artery endothelial cells. Am. J. Physiol. Circ. Physiol. 2010, 299, H193–H201. [Google Scholar] [CrossRef]
- Calió, M.L.; Marinho, D.S.; Ko, G.M.; Porcionatto, M. Antioxidant Effect of Leptin on Neurogenic Niches in a Model of Alzheimer’s Disease. Free Radic. Biol. Med. 2016, 100, S159. [Google Scholar] [CrossRef]
- Chistiakov, D.A.; Orekhov, A.N.; Bobryshev, Y.V. ApoA1 and ApoA1-specific self-antibodies in cardiovascular disease. Lab. Investig. 2016, 96, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Elliott, D.A.; Weickert, C.S.; Garner, B. Apolipoproteins in the brain: Implications for neurological and psychiatric disorders. Clin. Lipidol. 2010, 5, 555–573. [Google Scholar] [CrossRef]
- Perrone, S.; Longini, M.; Bellieni, C.; Centini, G.; Kenanidis, A.; De Marco, L.; Petraglia, F.; Buonocore, G. Early oxidative stress in amniotic fluid of pregnancies with Down syndrome. Clin. Biochem. 2007, 40, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Buczyńska, A.; Sidorkiewicz, I.; Ławicki, S.; Krętowski, A.; Zbucka-Krętowska, M. Prenatal Screening of Trisomy 21: Could Oxidative Stress Markers Play a Role? J. Clin. Med. 2021, 10, 2382. [Google Scholar] [CrossRef]
- Nuszkiewicz, J.; Woźniak, A.; Szewczyk-Golec, K. Ionizing Radiation as a Source of Oxidative Stress—The Protective Role of Melatonin and Vitamin D. Int. J. Mol. Sci. 2020, 21, 5804. [Google Scholar] [CrossRef] [PubMed]
- Polidoro, L.; Properzi, G.; Marampon, F.; Gravina, G.L.; Festuccia, C.; Di Cesare, E.; Scarsella, L.; Ciccarelli, C.; Zani, B.M.; Ferri, C. Vitamin D Protects Human Endothelial Cells from H2O2 Oxidant Injury through the Mek/Erk-Sirt1 Axis Activation. J. Cardiovasc. Transl. Res. 2012, 6, 221–231. [Google Scholar] [CrossRef]
- Wiesli, P.; Zwimpfer, C.; Zapf, J.; Schmid, C. Pregnancy-induced changes in insulin-like growth factor I (IGF-I), insulin-like growth factor binding protein 3 (IGFBP-3), and acid-labile subunit (ALS) in patients with growth hormone (GH) deficiency and excess. Acta Obstet. Gynecol. Scand. 2006, 85, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Liu, C.; Zhang, Z. Transthyretin and Normal Human Pregnancy: Mini Review. Crit. Rev. Eukaryot. Gene Expr. 2016, 26, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Brás, A.; Monteiro, C.; Rueff, J. Oxidative stress in trisomy 21: A possible role in cataractogenesis. Ophthalmic Paediatr. Genet. 1989, 10, 271–277. [Google Scholar] [CrossRef]
- Friedenson, B. The BRCA1/2 pathway prevents hematologic cancers in addition to breast and ovarian cancers. BMC Cancer 2007, 7, 152. [Google Scholar] [CrossRef]
- Salahuddin, P.; Rabbani, G.; Khan, R.H. The role of advanced glycation end products in various types of neurodegenerative disease: A therapeutic approach. Cell. Mol. Biol. Lett. 2014, 19, 407–437. [Google Scholar] [CrossRef]
- Dong, Y.; Shi, X.; Du, K.; Xu, R.; Jia, T.; Wang, J.; Wang, L.; Han, R. First Chinese patient with mental retardation-40 due to a de novo CHAMP1 frameshift mutation: Case report and literature review. Exp. Ther. Med. 2021, 22, 902. [Google Scholar] [CrossRef] [PubMed]
- Eldomery, M.K.; Akdemir, Z.C.; Vögtle, F.-N.; Charng, W.-L.; Mulica, P.; Rosenfeld, J.A.; Gambin, T.; Gu, S.; Burrage, L.C.; Al Shamsi, A.; et al. MIPEP recessive variants cause a syndrome of left ventricular non-compaction, hypotonia, and infantile death. Genome Med. 2016, 8, 106. [Google Scholar] [CrossRef] [PubMed]
- Balsano, C.; Porcu, C.; Sideri, S. Is copper a new target to counteract the progression of chronic diseases? Metallomics 2018, 10, 1712–1722. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, C.; Zlatic, S.A.; Wallin, M.; Vrailas-Mortimer, A.; Fahrni, C.J.; Faundez, V. Trafficking mechanisms of P-type ATPase copper transporters. Curr. Opin. Cell Biol. 2019, 59, 24–33. [Google Scholar] [CrossRef]
- Yurkova, I.L.; Arnhold, J.; Fitzl, G.; Huster, D. Fragmentation of mitochondrial cardiolipin by copper ions in the Atp7b−/− mouse model of Wilson’s disease. Chem. Phys. Lipids 2011, 164, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Renaudin, X.; Lee, M.; Shehata, M.; Surmann, E.-M.; Venkitaraman, A.R. BRCA2 deficiency reveals that oxidative stress impairs RNaseH1 function to cripple mitochondrial DNA maintenance. Cell Rep. 2021, 36, 109478. [Google Scholar] [CrossRef] [PubMed]
- Chew, A.; Buck, E.A.; Peretz, S.; Sirugo, G.; Rinaldo, P.; Isaya, G. Cloning, Expression, and Chromosomal Assignment of the Human Mitochondrial Intermediate Peptidase Gene (MIPEP). Genomics 1997, 40, 493–496. [Google Scholar] [CrossRef]
- MacLeod, K.F. The role of the RB tumour suppressor pathway in oxidative stress responses in the haematopoietic system. Nat. Rev. Cancer 2008, 8, 769–781. [Google Scholar] [CrossRef]
- Hoskins, E.E.; Gunawardena, R.W.; Habash, K.B.; Wise-Draper, T.M.; Jansen, M.; Knudsen, E.S.; Wells, S.I. Coordinate regu-lation of Fanconi anemia gene expression occurs through the Rb/E2F pathway. Oncogene 2008, 27, 4798–4808. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, A.; Shaukat, I.; Rajput, S.A.; Shukat, R.; Hanif, S.; Jiang, K.; Zhang, T.; Akhtar, M.; Ma, X.; Liu, J.; et al. Ginsenoside Rb1 protects from Staphylococcus aureus-induced oxidative damage and apoptosis through endoplasmic reticulum-stress and death receptor-mediated pathways. Ecotoxicol. Environ. Saf. 2021, 219, 112353. [Google Scholar] [CrossRef]
- Wang, A.-H.; Li, D.-W.; Zhou, F.-Z.; Sun, X.-C.; Li, S.-C.; Yang, J.-B.; Sun, H.-H. Ginsenoside Rb1 protects dopaminergic neurons from inflammatory injury induced by intranigral lipopolysaccharide injection. Neural Regen. Res. 2019, 14, 1814–1822. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Gu, X.; Yu, M.; Zi, Y.; Yu, H.; Wang, Y.U.; Xie, Y.; Xiang, L. Effects of ginsenoside Rb1 on oxidative stress injury in rat spinal cords by regulating the eNOS/Nrf2/HO-1 signaling pathway. Exp. Ther. Med. 2018, 16, 1079–1086. [Google Scholar] [CrossRef]
- Hempel, M.; Cremer, K.; Ockeloen, C.; Lichtenbelt, K.D.; Herkert, J.C.; Denecke, J.; Haack, T.B.; Zink, A.M.; Becker, J.; Wohlleber, E.; et al. De Novo Mutations in CHAMP1 Cause Intellectual Disability with Severe Speech Impairment. Am. J. Hum. Genet. 2015, 97, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Menarim, B.C.; Ali, H.E.-S.; Loux, S.C.; Scoggin, K.E.; Kalbfleisch, T.S.; MacLeod, J.N.; Dahlgren, L.A. Transcriptional and Histochemical Signatures of Bone Marrow Mononuclear Cell-Mediated Resolution of Synovitis. Front. Immunol. 2021, 12, 5042. [Google Scholar] [CrossRef]
- Kobayashi, M.; Takeda, K.; Narita, T.; Nagai, K.; Okita, N.; Sudo, Y.; Miura, Y.; Tsumoto, H.; Nakagawa, Y.; Shimano, H.; et al. Mitochondrial intermediate peptidase is a novel regulator of sirtuin-3 activation by caloric restriction. FEBS Lett. 2017, 591, 4067–4073. [Google Scholar] [CrossRef] [PubMed]
- Bause, A.S.; Haigis, M.C. SIRT3 regulation of mitochondrial oxidative stress. Exp. Gerontol. 2013, 48, 634–639. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, J.; Lin, Y.; Lei, Q.; Guan, K.-L.; Zhao, S.; Xiong, Y. Tumour suppressor SIRT3 deacetylates and activates manganese superoxide dismutase to scavenge ROS. EMBO Rep. 2011, 12, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Renaudin, X.; Venkitaraman, A.R. A mitochondrial response to oxidative stress mediated by unscheduled RNA-DNA hybrids (R-loops). Mol. Cell. Oncol. 2021, 8, 2007028. [Google Scholar] [CrossRef]
- Izzo, A.; Manco, R.; De Cristofaro, T.; Bonfiglio, F.; Cicatiello, R.; Mollo, N.; De Martino, M.; Genesio, R.; Zannini, M.; Conti, A.; et al. Overexpression of Chromosome 21 miRNAs May Affect Mitochondrial Function in the Hearts of Down Syndrome Fetuses. J. Genom. 2017, 2017, 8737649. [Google Scholar] [CrossRef] [PubMed]
- Kallol, S.; Albrecht, C. Materno-fetal cholesterol transport during pregnancy. Biochem. Soc. Trans. 2020, 48, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Andrabi, S.; Bekheirnia, M.R.; Robbins-Furman, P.; Lewis, R.A.; Prior, T.W.; Potocki, L. SMAD4 mutation segregating in a family with juvenile polyposis, aortopathy, and mitral valve dysfunction. Am. J. Med. Genet. Part A 2011, 155, 1165–1169. [Google Scholar] [CrossRef] [PubMed]
- MedlinePlus. FECH Gene: MedlinePlus Genetics. Available online: https://medlineplus.gov/genetics/gene/fech/ (accessed on 27 October 2021).
- Ribeiro, I.; Marcão, A.; Amaral, O.; Miranda, M.C.P.S.; Vanier, M.T.; Millat, G. Niemann-Pick type C disease: NPC1 mutations associated with severe and mild cellular cholesterol trafficking alterations. Hum. Genet. 2001, 109, 24–32. [Google Scholar] [CrossRef]
- Hameed, A.; Mojsak, P.; Buczynska, A.; Suleria, H.A.R.; Kretowski, A.; Ciborowski, M. Altered Metabolome of Lipids and Amino Acids Species: A Source of Early Signature Biomarkers of T2DM. J. Clin. Med. 2020, 9, 2257. [Google Scholar] [CrossRef] [PubMed]
- Zampieri, S.; Mellon, S.H.; Butters, T.D.; Nevyjel, M.; Covey, D.F.; Bembi, B.; Dardis, A. Oxidative stress in NPC1 deficient cells: Protective effect of allopregnanolone. J. Cell. Mol. Med. 2009, 13, 3786–3796. [Google Scholar] [CrossRef]
- Qin, B.Y.; Chacko, B.M.; Lam, S.S.; de Caestecker, M.P.; Correia, J.J.; Lin, K. Structural Basis of Smad1 Activation by Receptor Kinase Phosphorylation. Mol. Cell 2001, 8, 1303–1312. [Google Scholar] [CrossRef]
- Shintani, M.; Yagi, H.; Nakayama, T.; Saji, T.; Matsuoka, R. A new nonsense mutation of SMAD8 associated with pulmonary arterial hypertension. J. Med. Genet. 2009, 46, 331–337. [Google Scholar] [CrossRef]
- Xiu, D.; Wang, Z.; Cui, L.; Jiang, J.; Yang, H.; Liu, G. Sumoylation of SMAD 4 ameliorates the oxidative stress-induced apoptosis in osteoblasts. Cytokine 2018, 102, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Schneider-Yin, X.; Gouya, L.; Dorsey, M.; Rufenacht, U.; Deybach, J.-C.; Ferreira, G.C. Mutations in the iron-sulfur cluster ligands of the human ferrochelatase lead to erythropoietic protoporphyria. Blood 2000, 96, 1545–1549. [Google Scholar] [CrossRef]
- Gouya, L.; Schmitt, C.; Robreau, A.-M.; Austerlitz, F.; Da Silva, V.; Brun, P.; Simonin, S.; Lyoumi, S.; Grandchamp, B.; Beaumont, C.; et al. Contribution of a Common Single-Nucleotide Polymorphism to the Genetic Predisposition for Erythropoietic Protoporphyria. Am. J. Hum. Genet. 2006, 78, 2–14. [Google Scholar] [CrossRef]
- Ma, Y.-S.; Wu, S.-B.; Lee, W.-Y.; Cheng, J.-S.; Wei, Y.-H. Response to the increase of oxidative stress and mutation of mitochondrial DNA in aging. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2009, 1790, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Rogucki, M.; Buczyńska, A.; Krętowski, A.J.; Popławska-Kita, A. The Importance of miRNA in the Diagnosis and Prognosis of Papillary Thyroid Cancer. J. Clin. Med. 2021, 10, 4738. [Google Scholar] [CrossRef] [PubMed]
- Pallardó, F.V.; Lloret, A.; Lebel, M.; D’Ischia, M.; Cogger, V.C.; Le Couteur, D.; Gadaleta, M.N.; Castello, G.; Pagano, G. Mitochondrial dysfunction in some oxidative stress-related genetic diseases: Ataxia-Telangiectasia, Down Syndrome, Fanconi Anaemia and Werner Syndrome. Biogerontology 2010, 11, 401–419. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.P. Investigating Clustering in Trisomy 18 and Trisomy 13. Ph.D. Thesis, Queen Mary University of London, London, UK, 2013. [Google Scholar]
- Parfieniuk, E.; Samczuk, P.; Kowalczyk, T.; Pietrowska, K.; Niemira, M.; Paczkowska-Abdulsalam, M.; Wolczynski, S.; Kretowski, A.; Ciborowski, M.; Zbucka-Kretowska, M. Maternal plasma metabolic fingerprint indicative for fetal Down syndrome. Prenat. Diagn. 2018, 38, 876–882. [Google Scholar] [CrossRef]
- Pinto, J.; Almeida, L.M.; Martins, A.S.; Duarte, D.; Domingues, M.R.M.; Barros, A.S.; Galhano, E.; Pita, C.; Almeida, M.D.C.; Carreira, I.M.; et al. Impact of fetal chromosomal disorders on maternal blood metabolome: Toward new biomarkers? Am. J. Obstet. Gynecol. 2015, 213, 841.e1–841.e15. [Google Scholar] [CrossRef]
- Nemutlu, E.; Orgul, G.; Recber, T.; Aydin, E.; Ozkan, E.; Turgal, M.; Alikasifoglu, M.; Kir, S.; Beksac, M.S. Metabolic Infrastructure of Pregnant Women With Trisomy 21 Fetuses; Metabolomic Analysis. Zeitschrift für Geburtshilfe und Neonatologie 2019, 223, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Witters, G.; Van Robays, J.; Willekes, C.; Coumans, A.; Peeters, H.; Gyselaers, W.; Fryns, J. Trisomy 13, 18, 21, Triploidy and Turner syndrome: The 5T’s. Look at the hands. Facts Views Vis. ObGyn 2011, 3, 15–21. [Google Scholar]
- Katerji, M.; Filippova, M.; Duerksen-Hughes, P. Approaches and Methods to Measure Oxidative Stress in Clinical Samples: Research Applications in the Cancer Field. Oxidative Med. Cell. Longev. 2019, 2019, 1279250. [Google Scholar] [CrossRef]
- Palmieri, B.; Sblendorio, V. Current Status of Measuring Oxidative Stress. Methods Mol. Biol. 2010, 594, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.S.; Duggina, P.; Vedhantam, M.; Manne, M.; Varma, N.; Nagaram, S. Maternal serum and fetal cord-blood ischemia-modified albumin concentrations in normal pregnancy and preeclampsia: A systematic review and meta-analysis. J. Matern.-Fetal Neonatal Med. 2017, 31, 3255–3266. [Google Scholar] [CrossRef]
- Vyakaranam, S.; Bhongir, A.V.; Patlolla, D.; Chintapally, R. Maternal serum ischemia modified albumin as a marker for hypertensive disorders of pregnancy: A pilot study. Int. J. Reprod. Contracept. Obstet. Gynecol. 2015, 4, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Bahinipati, J.; Mohapatra, P.C. Ischemia Modified Albumin as a Marker of Oxidative Stress in Normal Pregnancy. J. Clin. Diagn. Res. 2016, 10, BC15–BC17. [Google Scholar] [CrossRef]
- Islam, M.T. Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol. Res. 2017, 39, 73–82. [Google Scholar] [CrossRef]
- Baierle, M.; Nascimento, S.N.; Moro, A.M.; Brucker, N.; Freitas, F.; Gauer, B.; Durgante, J.; Bordignon, S.; Zibetti, M.; Trentini, C.M.; et al. Relationship between Inflammation and Oxidative Stress and Cognitive Decline in the Institutionalized Elderly. Oxidative Med. Cell. Longev. 2015, 2015, 804198. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.P.; Al-Hasan, Y. Impact of Oxidative Stress in Fetal Programming. J. Pregnancy 2012, 2012, 582748. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B. Antioxidants: The Basics-what they are and how to Evaluate them. Adv. Pharmacol. 1996, 38, 3–20. [Google Scholar] [CrossRef]
- Ghiselli, A.; Serafini, M.; Natella, F.; Scaccini, C. Total antioxidant capacity as a tool to assess redox status: Critical view and experimental data. Free Radic. Biol. Med. 2000, 29, 1106–1114. [Google Scholar] [CrossRef]
- Marques, S.S.; Magalhães, L.M.; Tóth, I.V.; Segundo, M.A. Insights on Antioxidant Assays for Biological Samples Based on the Reduction of Copper Complexes—The Importance of Analytical Conditions. Int. J. Mol. Sci. 2014, 15, 11387–11402. [Google Scholar] [CrossRef]
- Kohen, R.; Nyska, A. Invited Review: Oxidation of Biological Systems: Oxidative Stress Phenomena, Antioxidants, Redox Reactions, and Methods for Their Quantification. Toxicol. Pathol. 2002, 30, 620–650. [Google Scholar] [CrossRef] [PubMed]
- Siwik, D.A.; Pagano, P.J.; Colucci, W.S. Oxidative stress regulates collagen synthesis and matrix metalloproteinase activity in cardiac fibroblasts. Am. J. Physiol.-Cell Physiol. 2001, 280, C53–C60. [Google Scholar] [CrossRef] [PubMed]
- Angelova, P.R.; Esteras, N.; Abramov, A.Y. Mitochondria and lipid peroxidation in the mechanism of neurodegeneration: Finding ways for prevention. Med. Res. Rev. 2021, 41, 770–784. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef]
- Kumar, J.; Haldar, C.; Verma, R. Fluoride Compromises Testicular Redox Sensor, Gap Junction Protein, and Metabolic Status: Amelioration by Melatonin. Biol. Trace Elem. Res. 2020, 196, 552–564. [Google Scholar] [CrossRef]
- Chan, C.K.; Zhao, Y.; Liao, S.Y.; Zhang, Y.L.; Lee, M.Y.K.; Xu, A.; Tse, H.F.; Vanhoutte, P.M. A-FABP and Oxidative Stress Underlie the Impairment of Endothelium-Dependent Relaxations to Serotonin and the Intima-Medial Thickening in the Porcine Coronary Artery with Regenerated Endothelium. ACS Chem. Neurosci. 2013, 4, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Lockman, K.A.; Htun, V.; Sinha, R.; Treskes, P.; Nelson, L.J.; Martin, S.F.; Rogers, S.M.; Le Bihan, T.; Hayes, P.C.; Plevris, J.N. Proteomic profiling of cellular steatosis with concomitant oxidative stress in vitro. Lipids Health Dis. 2016, 15, 114. [Google Scholar] [CrossRef]
- Li, H.; Xiao, Y.; Tang, L.; Zhong, F.; Huang, G.; Xu, J.-M.; Xu, A.-M.; Dai, R.-P.; Zhou, Z.-G. Adipocyte Fatty Acid-Binding Protein Promotes Palmitate-Induced Mitochondrial Dysfunction and Apoptosis in Macrophages. Front. Immunol. 2018, 9, 81. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.T.; Yudell, B.E.; Loor, J. Regulation of energy metabolism by long-chain fatty acids. Prog. Lipid Res. 2014, 53, 124–144. [Google Scholar] [CrossRef]
- Grimes, S.B.; Wild, R. Effect of Pregnancy on Lipid Metabolism and Lipoprotein Levels. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2018. [Google Scholar]
- Herrera, E. Lipid Metabolism in Pregnancy and its Consequences in the Fetus and Newborn. Endocrine 2002, 19, 43–55. [Google Scholar] [CrossRef]
- Picca, A.; Calvani, R.; Coelho-Júnior, H.J.; Landi, F.; Bernabei, R.; Marzetti, E. Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation: Intertwined Roads to Neurodegeneration. Antioxidants 2020, 9, 647. [Google Scholar] [CrossRef] [PubMed]
- Arbuzova, S.; Hutchin, T.; Cuckle, H. Mitochondrial dysfunction and Down’s syndrome. Bioessays 2002, 24, 681–684. [Google Scholar] [CrossRef]
- Thakur, S.; Daley, B.; Gaskins, K.; Vasko, V.V.; Boufraqech, M.; Patel, D.; Sourbier, C.; Reece, J.M.; Cheng, S.-Y.; Kebebew, E.; et al. Metformin Targets Mitochondrial Glycerophosphate Dehydrogenase to Control Rate of Oxidative Phosphorylation and Growth of Thyroid Cancer In Vitro and In Vivo. Clin. Cancer Res. 2018, 24, 4030–4043. [Google Scholar] [CrossRef] [PubMed]
- Blacker, T.S.; Duchen, M.R. Investigating mitochondrial redox state using NADH and NADPH autofluorescence. Free Radic. Biol. Med. 2016, 100, 53–65. [Google Scholar] [CrossRef]
- Connolly, N.M.C.; Theurey, P.; Adam-Vizi, V.; Bazan, N.G.; Bernardi, P.; Bolanos, J.; Culmsee, C.; Dawson, V.L.; Deshmukh, M.; Duchen, M.R.; et al. Guidelines on experimental methods to assess mitochondrial dysfunction in cellular models of neurodegenerative diseases. Cell Death Differ. 2018, 25, 542–572. [Google Scholar] [CrossRef] [PubMed]
- Naia, L.; Pinho, C.M.; Dentoni, G.; Liu, J.; Leal, N.S.; Ferreira, D.M.S.; Schreiner, B.; Filadi, R.; Fão, L.; Connolly, N.M.C.; et al. Neuronal cell-based high-throughput screen for enhancers of mitochondrial function reveals luteolin as a modulator of mitochondria-endoplasmic reticulum coupling. BMC Biol. 2021, 19, 57. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, I.; Fournier, T.; Chissey, A.; Therond, P.; Slama, A.; Beaudeux, J.-L.; Zerrad-Saadi, A. NADPH oxidase is the major source of placental superoxide in early pregnancy: Association with MAPK pathway activation. Sci. Rep. 2019, 9, 13962. [Google Scholar] [CrossRef] [PubMed]
- Koc, E.C.; Burkhart, W.; Blackburn, K.; Moyer, M.B.; Schlatzer, D.M.; Moseley, A.; Spremulli, L.L. The Large Subunit of the Mammalian Mitochondrial Ribosome: Analysis of the complement of ribosomal proteins present. J. Biol. Chem. 2001, 276, 43958–43969. [Google Scholar] [CrossRef]
- Impellizzeri, A.; Giannantoni, I.; Polimeni, A.; Barbato, E.; Galluccio, G. Epidemiological characteristic of Orofacial clefts and its associated congenital anomalies: Retrospective study. BMC Oral Health 2019, 19, 290. [Google Scholar] [CrossRef]
- Masotti, C.; Brito, L.; Nica, A.; Ludwig, K.; Nunes, K.; Savastano, C.; Malcher, C.; Ferreira, S.; Kobayashi, G.; Bueno, D.F.; et al. MRPL53, a New Candidate Gene for Orofacial Clefting, Identified Using an eQTL Approach. J. Dent. Res. 2018, 97, 33–40. [Google Scholar] [CrossRef]
- Lee, C.; Kim, K.H.; Cohen, P. MOTS-c: A novel mitochondrial-derived peptide regulating muscle and fat metabolism. Free Radic. Biol. Med. 2016, 100, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Herzig, S.; Shaw, R.J. AMPK: Guardian of metabolism and mitochondrial homeostasis. Nat. Rev. Mol. Cell Biol. 2018, 19, 121–135. [Google Scholar] [CrossRef]
- Xu, W.; Zhao, T.; Xiao, H. The Implication of Oxidative Stress and AMPK-Nrf2 Antioxidative Signaling in Pneumonia Path-ogenesis. Front. Endocrinol. 2020, 11, 400. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Zeng, J.; Drew, B.G.; Sallam, T.; Martin-Montalvo, A.; Wan, J.; Kim, S.-J.; Mehta, H.; Hevener, A.L.; de Cabo, R.; et al. The Mitochondrial-Derived Peptide MOTS-c Promotes Metabolic Homeostasis and Reduces Obesity and Insulin Resistance. Cell Metab. 2015, 21, 443–454. [Google Scholar] [CrossRef]
- Wojciechowska, M.; Pruszyńska-Oszmałek, E.; Kołodziejski, P.A.; Krauss, H.; Leciejewska, N.; Szczepankiewicz, D.; Bień, J.; Skrzypski, M.; Wilczak, M.; Sassek, M. Changes in MOTS-c Level in the Blood of Pregnant Women with Metabolic Disorders. Biology 2021, 10, 1032. [Google Scholar] [CrossRef]
- Hu, X.-Q.; Zhang, L. Hypoxia and Mitochondrial Dysfunction in Pregnancy Complications. Antioxidants 2021, 10, 405. [Google Scholar] [CrossRef] [PubMed]
- Ahn, C.S.; Metallo, C.M. Mitochondria as biosynthetic factories for cancer proliferation. Cancer Metab. 2015, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Gryder, B.E.; Wu, L.; Woldemichael, G.M.; Pomella, S.; Quinn, T.R.; Park, P.M.C.; Cleveland, A.; Stanton, B.Z.; Song, Y.; Rota, R.; et al. Chemical genomics reveals histone deacetylases are required for core regulatory transcription. Nat. Commun. 2019, 10, 3004. [Google Scholar] [CrossRef]
- De Ruijter, A.J.; Van Gennip, A.H.; Caron, H.N.; Kemp, S.; Van Kuilenburg, A.B. Histone deacetylases (HDACs): Characterization of the classical HDAC family. Biochem. J. 2003, 370, 737–749. [Google Scholar] [CrossRef]
- He, K.; Hu, J.; Yu, H.; Wang, L.; Tang, F.; Gu, J.; Ge, L.; Wang, H.; Li, S.; Hu, P.; et al. Serine/Threonine Kinase 40 (Stk40) Functions as a Novel Regulator of Skeletal Muscle Differentiation. J. Biol. Chem. 2017, 292, 351–360. [Google Scholar] [CrossRef]
- Muskens, I.S.; Li, S.; Jackson, T.; Elliot, N.; Hansen, H.M.; Myint, S.S.; Pandey, P.; Schraw, J.M.; Roy, R.; Anguiano, J.; et al. The genome-wide impact of trisomy 21 on DNA methylation and its implications for hematopoiesis. Nat. Commun. 2021, 12, 821. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Kang, Y.-J.; Lee, B.Y.; Han, Y.J.; Chung, J.H.; Kim, M.Y.; Kim, M.H.; Kim, J.W.; Cho, Y.-H.; Ryu, H.M. Epigenome-wide base-resolution profiling of DNA methylation in chorionic villi of fetuses with Down syndrome by methyl-capture sequencing. Clin. Epigenetics 2019, 11, 180. [Google Scholar] [CrossRef] [PubMed]
- Laan, L.; Klar, J.; Sobol, M.; Hoeber, J.; Shahsavani, M.; Kele, M.; Fatima, A.; Zakaria, M.; Annerén, G.; Falk, A.; et al. DNA methylation changes in Down syndrome derived neural iPSCs uncover co-dysregulation of ZNF and HOX3 families of transcription factors. Clin. Epigenetics 2020, 12, 9–14. [Google Scholar] [CrossRef] [PubMed]
- El-Osta, A.; Wolffe, A.P. DNA Methylation and Histone Deacetylation in the Control of Gene Expression: Basic Biochemistry to Human Development and Disease. Gene Expr. 2001, 9, 63–75. [Google Scholar] [CrossRef]
- Delcuve, G.P.; Khan, D.H.; Davie, J.R. Roles of histone deacetylases in epigenetic regulation: Emerging paradigms from studies with inhibitors. Clin. Epigenetics 2012, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Groth, A.; Rocha, W.; Verreault, A.; Almouzni, G. Chromatin Challenges during DNA Replication and Repair. Cell 2007, 128, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Staals, E.L.; Palmerini, E.; Ferrari, S.; Mercuri, M. Non-surgical Treatment of Chondrosarcoma: Current Concepts and Future Perspectives. Bone Cancer 2010, 375–383. [Google Scholar] [CrossRef]
- Fargo, K.; Pak, T.; Foecking, E.; Jones, K. Molecular Biology of Androgen Action: Perspectives on Neuroprotective and Neurotherapeutic Effects. Horm. Brain Behav. 2009, 1219–1246. [Google Scholar] [CrossRef]
- Jin, Z.; Liu, Y. DNA methylation in human diseases. Genes Dis. 2018, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.R.; Ali, F.E.; Abd-Elhamid, T.; Hassanein, E. Coenzyme Q10 protects hepatocytes from ischemia reperfusion-induced apoptosis and oxidative stress via regulation of Bax/Bcl-2/PUMA and Nrf-2/FOXO-3/Sirt-1 signaling pathways. Tissue Cell 2019, 60, 1–13. [Google Scholar] [CrossRef]
- Morshneva, A.; Gnedina, O.; Svetlikova, S.; Pospelov, V.; Igotti, M. Time-dependent modulation of FoxO activity by HDAC inhibitor in oncogene-transformed E1A+Ras cells. AIMS Genet. 2018, 5, 41–52. [Google Scholar] [CrossRef]
- Stojanovic, N.; Hassan, Z.; Wirth, M.; Wenzel, P.; Beyer, M.; Schäfer, C.; Brand, P.; Kroemer, A.; Stauber, R.H.; Schmid, R.M.; et al. HDAC1 and HDAC2 integrate the expression of p53 mutants in pancreatic cancer. Oncogene 2017, 36, 1804–1815. [Google Scholar] [CrossRef]
- Liu, X.; Gan, W.; Zou, Y.; Yang, B.; Su, Z.; Deng, J.; Wang, L.; Cai, J. Elevated Levels of Urinary Markers of Oxidative DNA and RNA Damage in Type 2 Diabetes with Complications. Oxidative Med. Cell. Longev. 2016, 2016, 4323198. [Google Scholar] [CrossRef] [PubMed]
- Badeau, M.; Lindsay, C.; Blais, J.; Nshimyumukiza, L.; Takwoingi, Y.; Langlois, S.; Légaré, F.; Giguère, Y.; Turgeon, A.F.; Witteman, W.; et al. Genomics-based non-invasive prenatal testing for detection of fetal chromosomal aneuploidy in pregnant women. Cochrane Database Syst. Rev. 2017, 11, CD011767. [Google Scholar] [CrossRef] [PubMed]
- Galeva, S.; Konstantinidou, L.; Gil, M.M.; Akolekar, R.; Nicolaides, K. Routine first-trimester screening for fetal trisomies in twin pregnancy: Cell-free DNA test contingent on results from combined test. Ultrasound Obstet. Gynecol. 2019, 53, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Gil, M.M.; Accurti, V.; Santacruz, B.; Plana, M.N.; Nicolaides, K.H. Analysis of cell-free DNA in maternal blood in screening for aneuploidies: Updated meta-analysis. Ultrasound Obstet. Gynecol. 2017, 50, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Nachvak, S.M.; Neyestani, T.R.; Mahboob, S.A.; Sabour, S.; Keshawarz, S.A.; Speakman, J.R. α-Tocopherol supplementation reduces biomarkers of oxidative stress in children with Down syndrome: A randomized controlled trial. Eur. J. Clin. Nutr. 2014, 68, 1119–1123. [Google Scholar] [CrossRef] [PubMed]
- Narasimhan, K.; Lin, S.L.; Tong, T.; Baig, S.; Ho, S.; Sukumar, P.; Biswas, A.; Hahn, S.; Bajic, V.; Choolani, M.A. Maternal serum protein profile and immune response protein subunits as markers for non-invasive prenatal diagnosis of trisomy 21, 18, and 13. Prenat. Diagn. 2013, 33, 223–231. [Google Scholar] [CrossRef]
- Lott, I.T. Antioxidants in Down syndrome. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2012, 1822, 657–663. [Google Scholar] [CrossRef]
- Corrales, A.; Parisotto, E.B.; Vidal, V.; García-Cerro, S.; Lantigua, S.; Diego, M.; Filho, D.W.; Sanchez-Barceló, E.J.; Martínez-Cué, C.; Rueda, N. Pre- and post-natal melatonin administration partially regulates brain oxidative stress but does not improve cognitive or histological alterations in the Ts65Dn mouse model of Down syndrome. Behav. Brain Res. 2017, 334, 142–154. [Google Scholar] [CrossRef]
- Zińczuk, J.; Maciejczyk, M.; Zaręba, K.; Romaniuk, W.; Markowski, A.R.; Kędra, B.; Zalewska, A.; Pryczynicz, A.; Matowicka-Karna, J.; Guzińska-Ustymowicz, K. Antioxidant Barrier, Redox Status, and Oxidative Damage to Biomolecules in Patients with Colorectal Cancer. Can Malondialdehyde and Catalase Be Markers of Colorectal Cancer Advancement? Biomolecules 2019, 9, 637. [Google Scholar] [CrossRef]
- Samouda, H.; De Beaufort, C.; Gilson, G.; Schritz, A.; Vaillant, M.; Ghaddhab, C.; Ruiz-Castell, M.; Huiart, L.; Dohet, F.; Weber, B.; et al. Relationship of oxidative stress to visceral adiposity in youth and role played by vitamin D. Pediatr. Diabetes 2020, 21, 758–765. [Google Scholar] [CrossRef]
- Shichiri, M.; Yoshida, Y.; Ishida, N.; Hagihara, Y.; Iwahashi, H.; Tamai, H.; Niki, E. α-Tocopherol suppresses lipid peroxidation and behavioral and cognitive impairments in the Ts65Dn mouse model of Down syndrome. Free Radic. Biol. Med. 2011, 50, 1801–1811. [Google Scholar] [CrossRef] [PubMed]
- Revilla, N.R.; Martínez-Cué, C. Antioxidants in Down Syndrome: From Preclinical Studies to Clinical Trials. Antioxidants 2020, 9, 692. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, K.; Amano, K.; Takaki, E.; Ebrahim, A.S.; Shimohata, A.; Shibazaki, N.; Inoue, I.; Takaki, M.; Ueda, Y.; Sago, H.; et al. Increased lipid peroxidation in Down’s syndrome mouse models. J. Neurochem. 2009, 110, 1965–1976. [Google Scholar] [CrossRef] [PubMed]
- Guedj, F.; Siegel, A.E.; Pennings, J.L.; Alsebaa, F.; Massingham, L.J.; Tantravahi, U.; Bianchi, D.W. Apigenin as a Candidate Prenatal Treatment for Trisomy 21: Effects in Human Amniocytes and the Ts1Cje Mouse Model. Am. J. Hum. Genet. 2020, 107, 911–931. [Google Scholar] [CrossRef]
- Guedj, F.; Bianchi, D.W.; Delabar, J.M. Prenatal treatment of Down syndrome: A reality? Curr. Opin. Obstet. Gynecol. 2014, 26, 92–103. [Google Scholar] [CrossRef]
- Zamponi, E.; Zamponi, N.; Coskun, P.; Quassollo, G.; Lorenzo, A.; Cannas, S.; Pigino, G.; Chialvo, D.; Gardiner, K.; Busciglio, J.; et al. Nrf2 stabilization prevents critical oxidative damage in Down syndrome cells. Aging Cell 2018, 17, e12812. [Google Scholar] [CrossRef]
| Material | Protein | Full Name | Form of Dysregulation | Reference |
|---|---|---|---|---|
| Amniotic fluid T18 pregnancy | A1AT | alpha-1-antitrypsin | down | [30] |
| Amniotic fluid T18 pregnancy | ApoA | apolipoprotein A | up | [30] |
| Amniotic fluid T18 pregnancy | IGFBP-1 | insulin-like growth factor-binding protein 1 | down | [30] |
| Amniotic fluid T13 and T18 pregnancy | leptin | - | down | [31] |
| Amniotic fluid T13 and T18 pregnancy | resistin | - | down | [31] |
| Amniotic fluid T18 pregnancy | TTR | transthyretin | down | [30] |
| Amniotic fluid T18 pregnancy | VDBP | vitamin D binding protein | down | [30] |
| Gene Location | Gene | Full Name | Function |
|---|---|---|---|
| Chromosome 13 | ATP7B | ATPase Copper Transporting Beta | copper transport |
| Chromosome 13 | BRCA2 | Breast Cancer 2 | tumor suppression |
| Chromosome 13 | CHAMP1 | Chromosome Alignment-Maintaining Phosphoprotein 1 | chromosome alignment maintenance with zinc finger protein regulations of chromosome segregation in mitosis |
| Chromosome 13 | MIPEP | Mitochondrial Intermediate Peptidase | oxidative mitochondrial processes |
| Chromosome 13 | RB1 | Retinoblastoma Transcriptional Corepressor 1 | inhibition of cell cycle processes, chromatin remodeling |
| Chromosome 18 | FECH | Ferrochelatase | mitochondrial membrane function |
| Chromosome 18 | NPC1 | Niemann–Pick C1 Protein | intracellular cholesterol trafficking |
| Chromosome 18 | SMAD | Mothers Against Decapentaplegic Homolog | transcription and signal transduction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buczyńska, A.; Sidorkiewicz, I.; Hameed, A.; Krętowski, A.J.; Zbucka-Krętowska, M. Future Perspectives in Oxidative Stress in Trisomy 13 and 18 Evaluation. J. Clin. Med. 2022, 11, 1787. https://doi.org/10.3390/jcm11071787
Buczyńska A, Sidorkiewicz I, Hameed A, Krętowski AJ, Zbucka-Krętowska M. Future Perspectives in Oxidative Stress in Trisomy 13 and 18 Evaluation. Journal of Clinical Medicine. 2022; 11(7):1787. https://doi.org/10.3390/jcm11071787
Chicago/Turabian StyleBuczyńska, Angelika, Iwona Sidorkiewicz, Ahsan Hameed, Adam Jacek Krętowski, and Monika Zbucka-Krętowska. 2022. "Future Perspectives in Oxidative Stress in Trisomy 13 and 18 Evaluation" Journal of Clinical Medicine 11, no. 7: 1787. https://doi.org/10.3390/jcm11071787
APA StyleBuczyńska, A., Sidorkiewicz, I., Hameed, A., Krętowski, A. J., & Zbucka-Krętowska, M. (2022). Future Perspectives in Oxidative Stress in Trisomy 13 and 18 Evaluation. Journal of Clinical Medicine, 11(7), 1787. https://doi.org/10.3390/jcm11071787