Predictors of Repeat Medical Emergency Team Activation in Deteriorating Ward Patients: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
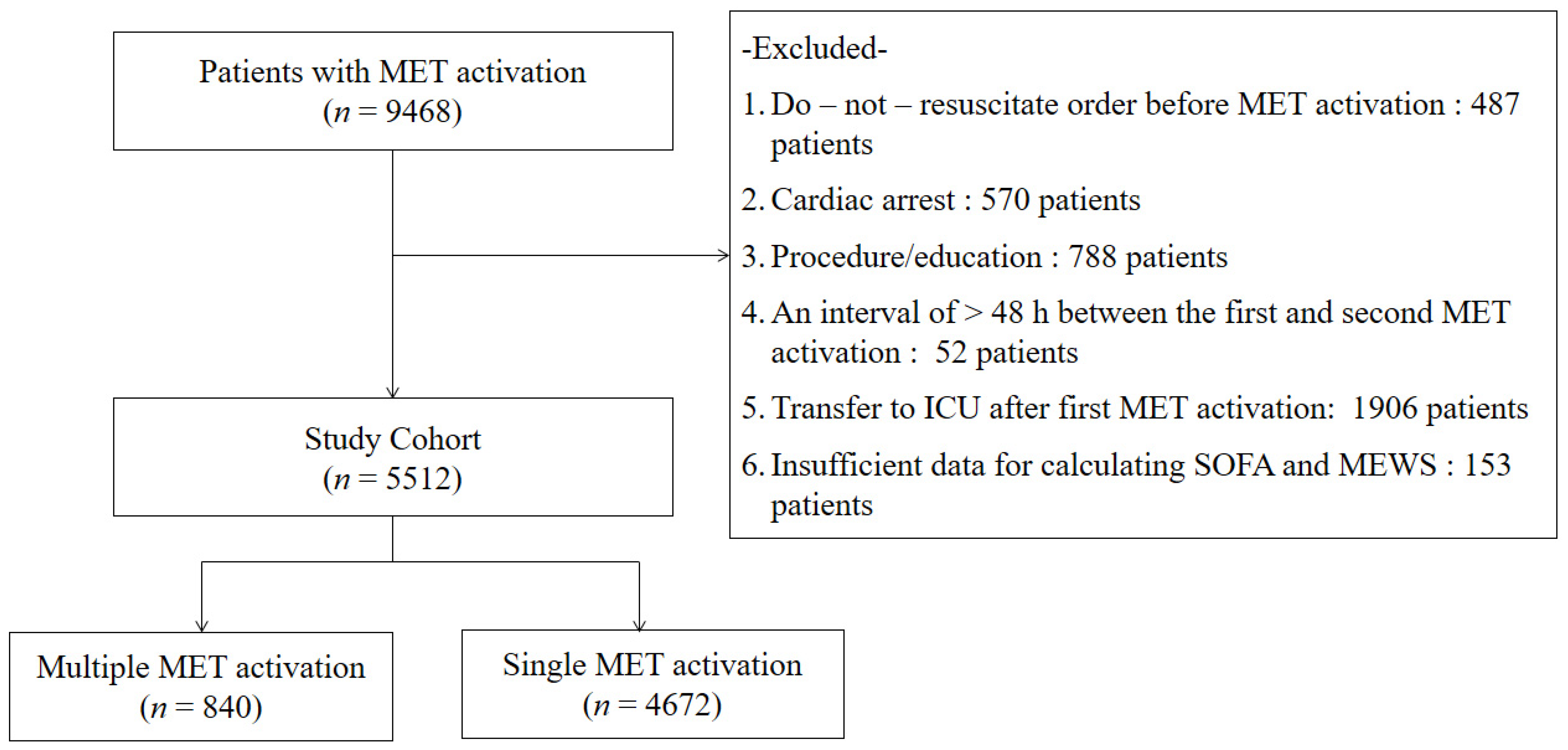
2.1. Study Cohort
2.2. The Medical Emergency Team
2.3. Data Collection
2.4. Statistical Analysis
3. Results
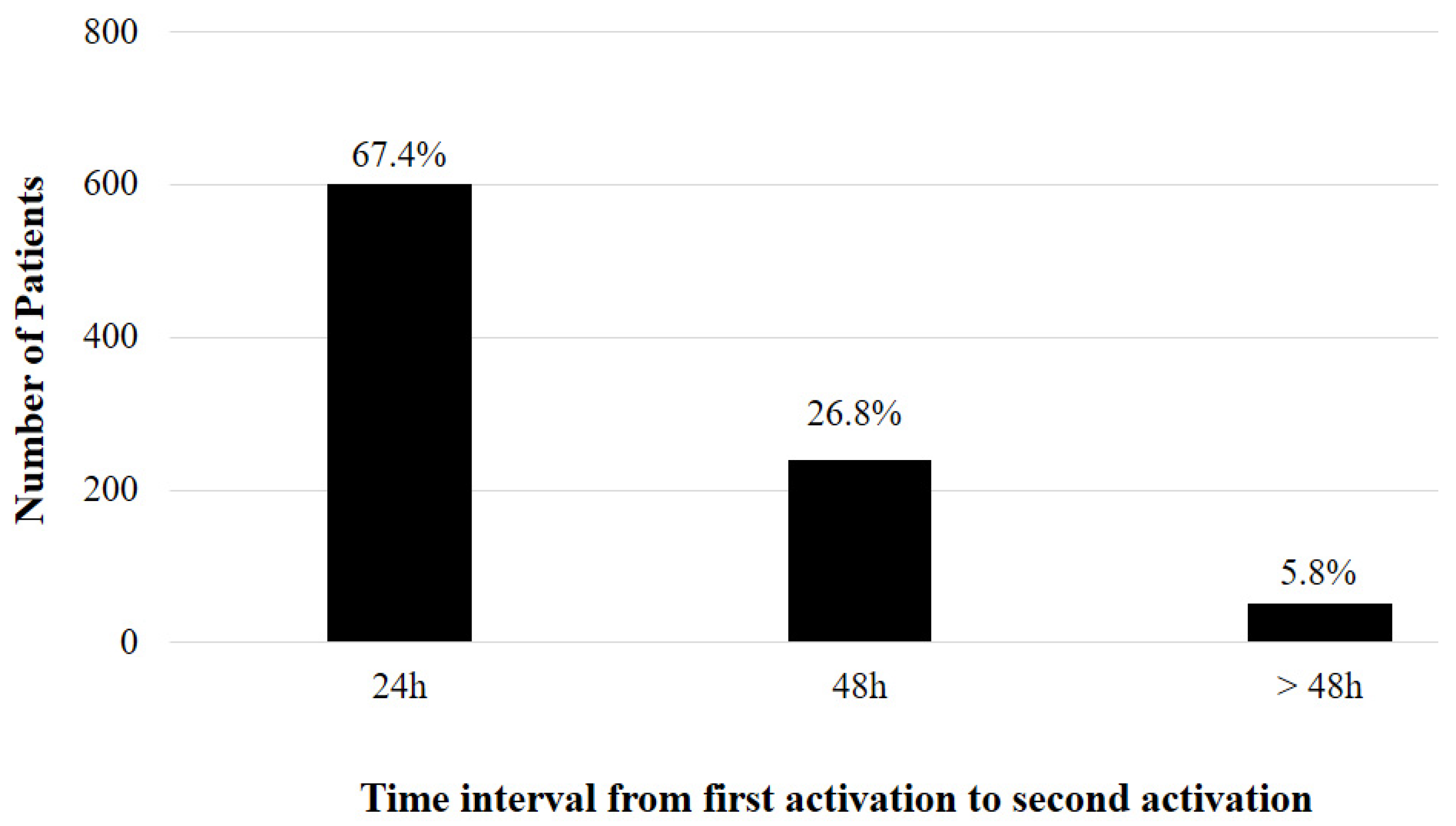
3.1. Patient Characteristics
3.2. Interventions during MET Activation
3.3. Outcomes
3.4. Risk Factors of Repeat MET Activation
3.5. Risk Factors of Repeat MET Activation by Respiratory Causes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jones, D.A.; DeVita, M.A.; Bellomo, R. Rapid-response teams. N. Engl. J. Med. 2011, 365, 139–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stelfox, H.T.; Bagshaw, S.M.; Gao, S. Characteristics and outcomes for hospitalized patients with recurrent clinical deterioration and repeat medical emergency team activation. Crit. Care Med. 2014, 42, 1601–1609. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.M.; Reardon, P.M.; Scales, D.C.; Murphy, K.; Tanuseputro, P.; Heyland, D.K.; Kyeremanteng, K. Prevalence, risk factors, and clinical consequences of recurrent activation of a rapid response team: A multicenter observational study. J. Intensive Care Med. 2019, 34, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Buist, M.D.; Moore, G.E.; Bernard, S.A.; Berthelot, S.; Zygun, D.; Ghali, W.A. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: Preliminary study. BMJ 2002, 324, 387–390. [Google Scholar] [CrossRef] [Green Version]
- Konrad, D.; Jaderling, G.; Bell, M.; Granath, F.; Ekbom, A.; Martling, C.R. Reducing in-hospital cardiac arrests and hospital mortality by introducing a medical emergency team. Intensive Care Med. 2010, 36, 100–106. [Google Scholar] [CrossRef]
- Lee, A.; Bishop, G.; Hillman, K.M.; Daffurn, K. The Medical Emergency Team. Anaesth. Intensive Care 1995, 23, 183–186. [Google Scholar] [CrossRef] [Green Version]
- Jones, D.; Bellomo, R.; DeVita, M.A. Effectiveness of the Medical Emergency Team: The importance of dose. Crit. Care 2009, 13, 313. [Google Scholar] [CrossRef] [Green Version]
- Calzavacca, P.; Licari, E.; Tee, A.; Mercer, I.; Haase, M.; Haase-Fielitz, A.; Jones, D.; Gutteridge, G.; Bellomo, R. Features and outcome of patients receiving multiple Medical Emergency Team reviews. Resuscitation 2010, 81, 1509–1515. [Google Scholar] [CrossRef]
- Huh, J.W.; Lim, C.M.; Koh, Y.S.; Lee, J.R.; Jung, Y.K.; Seo, H.S.; Hong, S.B. Activation of a medical emergency team using an electronic medical recording–based screening system. Crit. Care Med. 2014, 42, 801–808. [Google Scholar] [CrossRef]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM 2001, 94, 521–526. [Google Scholar] [CrossRef] [Green Version]
- Kwack, W.G.; Lee, D.S.; Min, H.; Choi, Y.Y.; Yun, M.; Kim, Y.; Lee, S.H.; Song, I.; Park, J.S.; Cho, Y.J.; et al. Evaluation of the SpO2/FiO2 ratio as a predictor of intensive care unit transfers in respiratory ward patients for whom the rapid response system has been activated. PLoS ONE 2018, 13, e0201632. [Google Scholar] [CrossRef] [PubMed]
- Rice, T.W.; Wheeler, A.P.; Bernard, G.R.; Hayden, D.L.; Schoenfeld, D.A.; Ware, L.B. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 2007, 132, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Stelfox, H.T.; Hemmelgarn, B.R.; Bagshaw, S.M.; Gao, S.; Doig, C.J.; Nijssen-Jordan, C.; Manns, B. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch. Intern. Med. 2012, 172, 467–474. [Google Scholar] [CrossRef] [Green Version]
- Bellomo, R.; Ackerman, M.; Bailey, M.; Beale, R.; Clancy, G.; Danesh, V.; Hvarfner, A.; Jimenez, E.; Konrad, D.; Lecardo, M.; et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit. Care Med. 2012, 40, 2261–2349. [Google Scholar] [CrossRef] [PubMed]
- Hosein, F.S.; Bobrovitz, N.; Berthelot, S.; Zygun, D.; Ghali, W.A.; Stelfox, H.T. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit. Care 2013, 3, R102. [Google Scholar] [CrossRef] [Green Version]
- Schneider, A.G.; Calzavacca, P.; Mercer, I.; Hart, G.; Jones, D.; Bellomo, R. The epidemiology and outcome of medical emergency team call patients treated with non-invasive ventilation. Resuscitation 2011, 82, 1218–1223. [Google Scholar] [CrossRef]
- Egol, A.; Fromm, R.; Guntupalli, K.K.; Fitzpatrick, M.; Kaufman, D.; Nasraway, S.; Ryon, D.; Zimmerman, J. Task Force of the American College of Critical Care Medicine. Crit. Care Med. 1999, 27, 633–638. [Google Scholar]
- Sprung, C.L.; Danis, M.; Baily, M.A.; Chalfin, D.B.; Dagi, T.F.; Davila, F.; De Vita, M.; Engelhardt, H.T.; Grenvik, A.; Hofmann, P.B. Consensus statement on the triage of critically ill patients: Society of Critical Care Medicine Ethics Committee. JAMA 1994, 271, 1200–1203. [Google Scholar] [CrossRef]
- Helviz, Y.; Einav, S. A Systematic Review of the High-flow Nasal Cannula for Adult Patients. Crit. Care 2018, 22, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Carratala Perales, J.M.; Llorens, P.; Brouzet, B.; Albert Jiménez, A.R.; Fernández-Cañadas, J.M.; Carbajosa Dalmau, J.; Martínez Beloqui, E.; Ramos Forner, S. High-flow therapy via nasal cannula in acute heart failure. Rev. Esp. Cardiol. 2011, 64, 723–725. [Google Scholar] [CrossRef]
- Frat, J. Clinical Effect of the Association of Non-invasive Ventilation and High Flow Nasal Oxygen Therapy in Resuscitation of Patients with Acute Lung Injury. A Randomised study (FLORALI Study). 2014. Available online: http://clinicaltrials.gov/show/NCT01320384 (accessed on 8 October 2021).
- Kang, B.J.; Koh, Y.; Lim, C.M.; Huh, J.W.; Baek, S.; Han, M.; Seo, H.S.; Suh, H.J.; Kim, G.J.; Seo, G.J.; et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015, 41, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.R.; Jung, Y.K.; Kim, H.J.; Koh, Y.; Lim, C.M.; Hong, S.B.; Huh, J.W. Derivation and validation of modified early warning score plus SpO2/FiO2 score for predicting acute deterioration of patients with hematological malignancies. Korean J. Intern. Med. 2020, 35, 1477–1488. [Google Scholar] [CrossRef] [PubMed]
| Variables | Repeat MET Activation | p | |
|---|---|---|---|
| Yes (n = 840) | No (n = 4672) | ||
| Age, years | 64 (52–73) | 64 (53–73) | 0.739 |
| Male gender | 548 (65.2) | 2943 (63.0) | 0.432 |
| Department | |||
| Medicine | 752 (89.5) | 3931 (84.1) | <0.001 |
| Surgery | 88 (10.5) | 741 (15.9) | |
| Comorbidities | |||
| Solid tumor | 267 (31.8) | 1635 (35.0) | 0.382 |
| Hematological malignancies | 210 (25.0) | 435 (9.3) | <0.001 |
| Chronic lung disease | 141 (16.8) | 500 (10.7) | <0.001 |
| Chronic heart disease | 383 (45.6) | 1961 (42.0) | 0.058 |
| Chronic liver disease | 95 (11.3) | 696 (14.9) | 0.053 |
| Chronic renal disease | 55 (6.5) | 246 (5.3) | 0.138 |
| Cause for MET activation | |||
| Respiratory distress | 599 (71.3) | 2162 (46.3) | <0.001 |
| Sepsis/septic shock | 116 (13.8) | 938 (20.1) | <0.001 |
| Hypovolemic shock | 18 (2.1) | 323 (6.9) | <0.001 |
| Arrhythmia | 11 (1.3) | 107 (2.3) | 0.071 |
| Altered mental status | 21 (2.5) | 140 (3.0) | 0.587 |
| Metabolic acidosis | 48 (5.7) | 378 (8.1) | 0.053 |
| Provider worried | 27 (3.2) | 491 (10.5) | <0.001 |
| Vital parameter at first MET activation | |||
| Systolic blood pressure (mmHg) | 119 (100–137) | 110 (90–132) | <0.001 |
| Heart rate (beats/min) | 110 (94–128) | 106 (88–122) | <0.001 |
| Respiratory rate (breaths/min) | 26 (22–32) | 22 (20–28) | <0.001 |
| Body temperature (°C) | 36.9 (36.5–37.7) | 36.8 (36.4–37.5) | <0.001 |
| SpO2 (%) | 95 (91–98) | 96 (92–98) | 0.059 |
| FiO2 (%) | 0.37 (0.25–0.45) | 0.28 (0.21–0.45) | <0.001 |
| SpO2/FiO2 ratio | 213 (169–338) | 350 (218–452) | <0.001 |
| Modified Early Warning Score | 5 (3–7) | 4 (3–6) | <0.001 |
| SOFA | 7 (4–9) | 4 (3–7) | <0.001 |
| Variables | Repeat MET Activation | p | |
|---|---|---|---|
| Yes (n = 840) | No (n = 4672) | ||
| Noninvasive mechanical ventilation | 34 (4.0) | 98 (2.1) | 0.001 |
| High-flow nasal cannula application | 274 (32.6) | 224 (4.8) | <0.001 |
| Supply oxygen | 161 (19.2) | 980 (20.0) | 0.273 |
| Suctioning of the airway | 242 (28.8) | 217 (4.6) | <0.001 |
| Arterial catheter inserted | 36 (4.3) | 265 (5.7) | 0.117 |
| Central IV catheter inserted | 74 (8.8) | 354 (7.6) | 0.234 |
| Peripheral IV catheter inserted | 94 (11.2) | 398 (8.5) | 0.015 |
| Fluid resuscitation | 187 (22.3) | 981 (20.1) | 0.063 |
| Transfusion | 23 (2.7) | 152 (3.3) | 0.521 |
| Vasopressor support | 89 (10.6) | 222 (4.8) | <0.001 |
| Outcomes | Repeat MET Activation | Unadjusted OR | Adjusted OR | |||
|---|---|---|---|---|---|---|
| Yes | No | OR (95% CI) | p | OR (95% CI) | p | |
| 28 day mortality overall | 329/840 (37.2) | 1111/4671 (23.8) | 2.06 (1.77–2.41) | <0.001 | 1.34 (1.03–1.74) | 0.028 |
| 28 day mortality (no DNR patients) | 142/577 (24.6) | 560/3422 (16.4) | 1.67 (1.35–2.06) | <0.001 | 1.56 (1.19–2.04) | <0.001 |
| In-hospital mortality overall | 461/840 (54.9) | 1406/4671 (30.1) | 2.83 (2.43–3.28) | <0.001 | 2.05 (1.61–2.61) | <0.001 |
| In-hospital mortality (no DNR patients) | 193/577 (33.4) | 729/3422 (21.3) | 1.86 (1.53–2.25) | <0.001 | 1.75 (1.37–2.24) | <0.001 |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.00 (0.99–1.00) | 0.484 | 1.00 (0.99–1.00) | 0.196 |
| Male (reference: female) | 1.01 (0.88–1.35) | 0.437 | 1.11 (0.88–1.40) | 0.365 |
| Medical department | 1.61 (1.27–2.04) | <0.001 | 1.38 (0.98–1.94) | 0.070 |
| Hematological malignancies | 3.25 (2.70–3.91) | <0.001 | 2.07 (1.54–2.79) | <0.001 |
| Chronic lung disease | 1.68 (1.37–2.06) | <0.001 | 1.49 (1.07–2.06) | 0.017 |
| Chronic liver disease | 0.73 (0.58–0.92) | 0.007 | 0.98 (0.68–1.48) | 0.869 |
| Chronic heart disease | 1.16 (1.00–1.34) | 0.052 | 1.13 (0.89–1.43) | 0.313 |
| Respiratory distress | 2.89 (2.46–3.39) | <0.001 | 1.76 (1.19–2.60) | <0.001 |
| Sepsis/septic shock | 0.64 (0.52–0.79) | 0.001 | 0.97 (0.62–1.50) | 0.887 |
| Hypovolemic shock | 0.30 (0.18–0.48) | <0.001 | 0.53 (0.22–1.29) | 0.162 |
| Metabolic acidosis | 0.69 (0.51–0.94) | 0.018 | 0.88 (0.98–1.38) | 0.382 |
| provider worried | 0.79 (1.00–6.47) | 0.830 | 0.97 (0.95–1.06) | 0.682 |
| MEWS | 1.15 (1.01–1.19) | <0.001 | 0.99 (0.93–1.04) | 0.571 |
| SpO2/FiO2 ratio | 0.98 (0.98–0.99) | <0.001 | 0.97 (0.95–0.98) | <0.001 |
| Noninvasive mechanical ventilation | 1.97 (1.32–2.93) | 0.001 | 1.52 (1.07–2.52) | <0.001 |
| High-flow nasal cannula | 9.61 (7.89–11.71) | <0.001 | 4.52 (3.56–5.74) | <0.001 |
| Suctioning of the airway | 8.31 (6.79–10.17) | <0.001 | 4.63 (3.59–5.98) | <0.001 |
| Vasopressor support | 2.34 (1.84–3.07) | <0.001 | 1.76 (1.22–2.54) | 0.002 |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.00 (0.99–1.01) | 0.704 | 1.00 (0.99–1.00) | 0.263 |
| Male (reference: female) | 1.17 (0.96–1.44)) | 0.112 | 1.19 (0.93–1.51) | 0.172 |
| Hematological malignancies | 2.70 (2.11–3.46) | <0.001 | 2.65 (1.94–3.62) | <0.001 |
| Chronic lung disease | 1.37 (1.08–1.72) | 0.008 | 1.32 (1.00–1.76) | 0.055 |
| Chronic heart disease | 1.14 (0.95–1.38) | 0.166 | 1.22 (0.96–1.56) | 0.109 |
| MEWS | 1.11 (1.06–1.17) | <0.001 | 1.01 (0.95–1.07) | 0.755 |
| SpO2/FiO2 ratio | 0.98 (0.98–0.99) | <0.001 | 0.98 (0.98–0.99) | <0.001 |
| High-flow nasal cannula | 5.14 (4.10–6.45) | <0.001 | 2.86 (2.22–3.72) | <0.001 |
| Noninvasive mechanical ventilation | 1.04 (0.65–1.67) | 0.862 | 1.09 (0.62–1.91) | 0.767 |
| Suctioning of the airway | 5.64 (4.42–7.19) | <0.001 | 4.98 (3.69–6.71) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-R.; Jung, Y.-K.; Hong, S.-B.; Huh, J.W. Predictors of Repeat Medical Emergency Team Activation in Deteriorating Ward Patients: A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 1736. https://doi.org/10.3390/jcm11061736
Lee J-R, Jung Y-K, Hong S-B, Huh JW. Predictors of Repeat Medical Emergency Team Activation in Deteriorating Ward Patients: A Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(6):1736. https://doi.org/10.3390/jcm11061736
Chicago/Turabian StyleLee, Ju-Ry, Youn-Kyung Jung, Sang-Bum Hong, and Jin Won Huh. 2022. "Predictors of Repeat Medical Emergency Team Activation in Deteriorating Ward Patients: A Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 6: 1736. https://doi.org/10.3390/jcm11061736
APA StyleLee, J.-R., Jung, Y.-K., Hong, S.-B., & Huh, J. W. (2022). Predictors of Repeat Medical Emergency Team Activation in Deteriorating Ward Patients: A Retrospective Cohort Study. Journal of Clinical Medicine, 11(6), 1736. https://doi.org/10.3390/jcm11061736






