The Differential Prognostic Impact of Long-Duration Atrial High-Rate Episodes Detected by Cardiac Implantable Electronic Devices between Patients with and without a History of Atrial Fibrillation
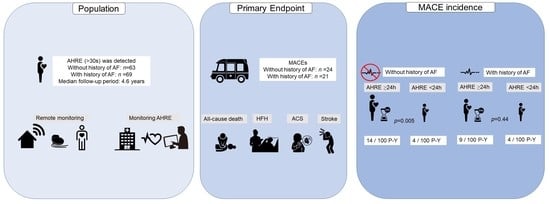
Abstract
:1. Introduction
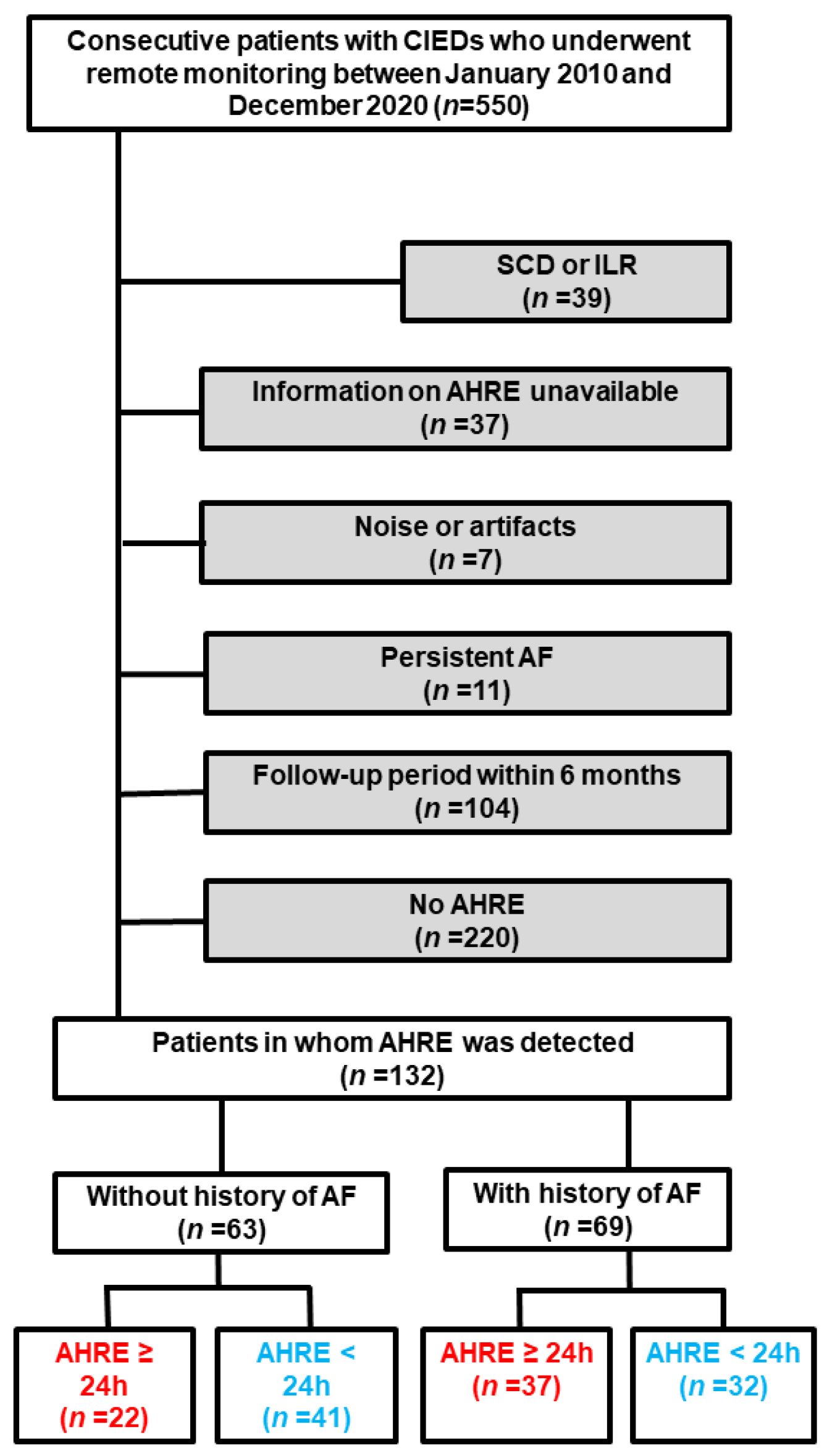
2. Materials and Methods
2.1. Study Design
2.2. Study Endpoints
2.3. Definition of Clinical Events
2.4. Detection of AHRE
2.5. Remote Monitoring
2.6. Data Collection and Patient Follow-Up
2.7. Statistical Analysis
3. Results
3.1. Study Population
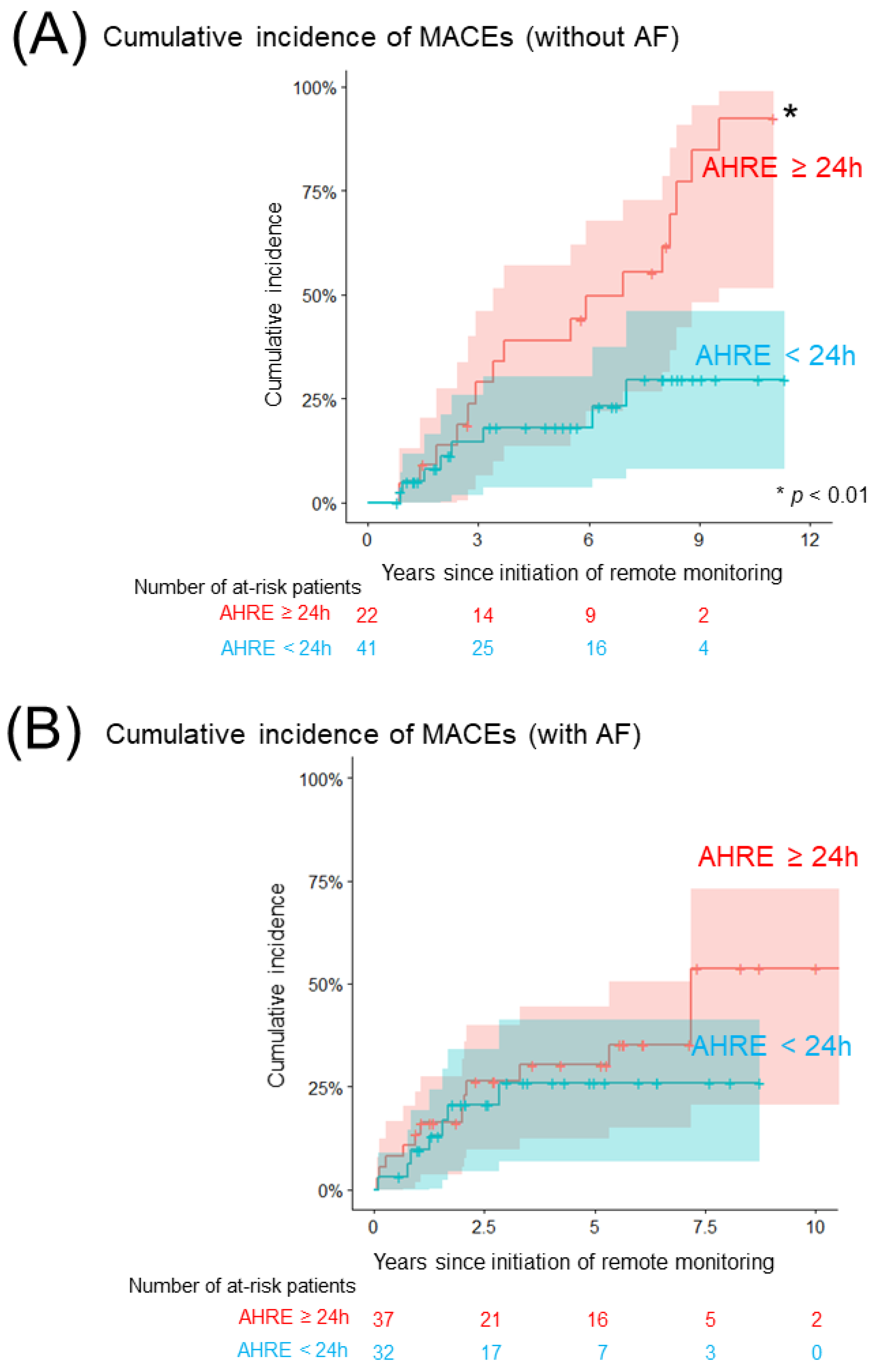
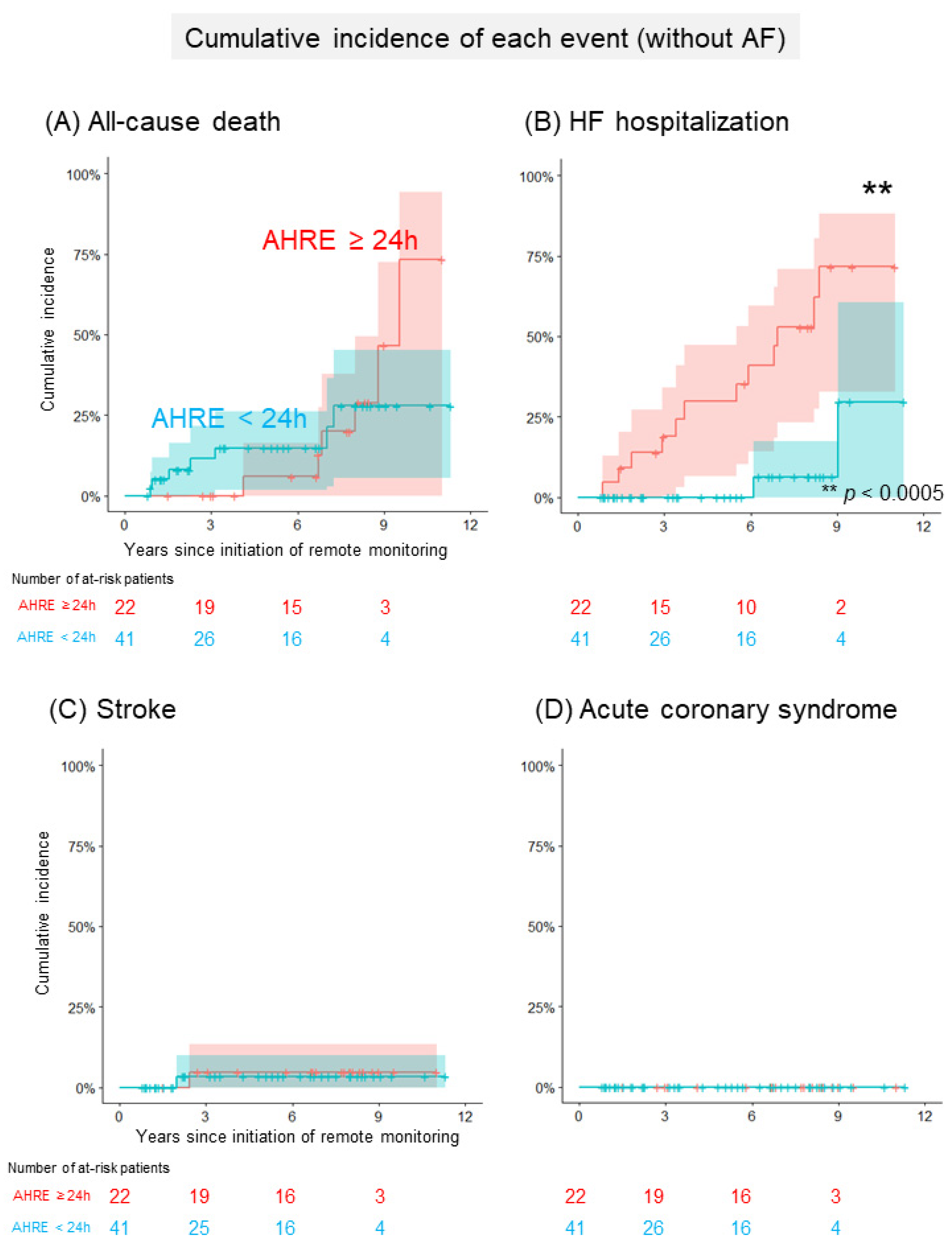
3.2. Cumulative Incidence of MACEs
3.3. Catheter Ablation during the Follow-Up Period
3.4. Anticoagulation Therapy for Patients Who Developed MACEs
3.5. Predictors of MACE Development
4. Discussion
4.1. Main Findings
4.2. The Impact of Long Duration of AHRE for MACE
4.3. Difference in the Impact of AHRE between Patients with and without a History of AF
4.4. Clinical Implications
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hindriks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the Diagnosis and Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the Diagnosis and Management of Atrial Fibrillation of the European Society of Cardiology (ESC) Developed with the Special Contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2020, 2021, 373–498. [Google Scholar] [CrossRef]
- Conen, D.; Chae, C.U.; Glynn, R.J.; Tedrow, U.B.; Everett, B.M.; Buring, J.E.; Albert, C.M. Risk of Death and Cardiovascular Events in Initially Healthy Women with New-Onset Atrial Fibrillation. JAMA 2011, 305, 2080–2087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pokorney, S.D.; Piccini, J.P.; Stevens, S.R.; Patel, M.R.; Pieper, K.S.; Halperin, J.L.; Breithardt, G.; Singer, D.E.; Hankey, G.J.; Hacke, W.; et al. Cause of Death and Predictors of All-Cause Mortality in Anticoagulated Patients with Nonvalvular Atrial Fibrillation: Data from ROCKET AF. J. Am. Heart Assoc. 2016, 5, e002197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinter, N.; Huang, Q.; Fenger-Grøn, M.; Frost, L.; Benjamin, E.J.; Trinquart, L. Trends in Excess Mortality Associated with Atrial Fibrillation over 45 Years (Framingham Heart Study): Community Based Cohort Study. BMJ 2020, 370, m2724. [Google Scholar] [CrossRef]
- Van Gelder, I.C.; Healey, J.S.; Crijns, H.J.G.M.; Wang, J.; Hohnloser, S.H.; Gold, M.R.; Capucci, A.; Lau, C.P.; Morillo, C.A.; Hobbelt, A.H.; et al. Duration of Device-Detected Subclinical Atrial Fibrillation and Occurrence of Stroke in ASSERT. Eur. Heart J. 2017, 38, 1339–1344. [Google Scholar] [CrossRef]
- Vitolo, M.; Imberti, J.F.; Maisano, A.; Albini, A.; Bonini, N.; Valenti, A.C.; Malavasi, V.L.; Proietti, M.; Healey, J.S.; Lip, G.Y.; et al. Device-Detected Atrial High Rate Episodes and the Risk of Stroke/Thromboembolism and Atrial Fibrillation Incidence: A Systematic Review and Meta-Analysis. Eur. J. Intern. Med. 2021, 92, 101–106. [Google Scholar] [CrossRef]
- Ishiguchi, H.; Shimizu, A.; Ishikura, M.; Yoshida, M.; Imoto, K.; Sonoyama, K.; Kawabata, T.; Sugamori, T.; Ogawa, M.; Uchida, T.; et al. Association between Atrial High-Rate Episodes and Ischemic/Major Bleeding Events in Patients with a Cardiac Implantable Electronic Device—A 10-Year, Single-Center Historical Cohort Study. Circ. J. 2021, 85, 1329–1337. [Google Scholar] [CrossRef]
- Nishinarita, R.; Niwano, S.; Fukaya, H.; Oikawa, J.; Nabeta, T.; Matsuura, G.; Arakawa, Y.; Kobayashi, S.; Shirakawa, Y.; Horiguchi, A.; et al. Burden of Implanted-Device-Detected Atrial High-Rate Episode Is Associated with Future Heart Failure Events-Clinical Significance of Asymptomatic Atrial Fibrillation in Patients with Implantable Cardiac Electronic Devices. Circ. J. 2019, 83, 736–742. [Google Scholar] [CrossRef] [Green Version]
- Lu, W.D.; Chen, J.Y. Atrial High-Rate Episodes and Risk of Major Adverse Cardiovascular Events in Patients with Dual Chamber Permanent Pacemakers: A Retrospective Study. Sci. Rep. 2021, 11, 5753. [Google Scholar] [CrossRef]
- Pastori, D.; Miyazawa, K.; Li, Y.; Székely, O.; Shahid, F.; Farcomeni, A.; Lip, G.Y.H. Atrial High-Rate Episodes and Risk of Major Adverse Cardiovascular Events in Patients with Cardiac Implantable Electronic Devices. Clin. Res. Cardiol. 2020, 109, 96–102. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D.; Joint ESC/ACCF/AHA/WHF Task Force for Universal Definition of Myocardial Infarction; Task Force Members Chairpersons; Thygesen, K.; Alpert, J.S.; et al. Third Universal Definition of Myocardial Infarction. J. Am. Coll. Cardiol. 2012, 60, 1581–1598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez, M.; Keating, R.J.; Markowitz, S.M.; Liu, C.F.; Thomas, G.; Ip, J.E.; Lerman, B.B.; Cheung, J.W. Newly Detected Atrial High Rate Episodes Predict Long-Term Mortality Outcomes in Patients with Permanent Pacemakers. Heart Rhythm. 2014, 11, 2214–2221. [Google Scholar] [CrossRef] [PubMed]
- Ogino, Y.; Ishikawa, T.; Ishigami, T.; Matsumoto, K.; Hosoda, J.; Iguchi, K.; Matsushita, H.; Taguchi, Y.; Horiguchi, Y.; Kimura, K. Characteristics and Prognosis of Pacemaker-Identified New-Onset Atrial Fibrillation in Japanese People. Circ. J. 2017, 81, 794–798. [Google Scholar] [CrossRef] [Green Version]
- Arai, S.; Kawamura, M.; Gokan, T.; Yoshikawa, K.; Ogawa, K.; Ochi, A.; Munetsugu, Y.; Ito, H.; Shinke, T. Relationship between Device-Detected Subclinical Atrial Fibrillation and Heart Failure in Patients with Cardiac Resynchronization Therapy Defibrillator. Clin. Cardiol. 2020, 43, 1517–1523. [Google Scholar] [CrossRef] [PubMed]
- Andersson, B.; Lomsky, M.; Waagstein, F. The link between acute haemodynamic adrenergic beta-blockade and long-term effects in patients with heart failure. A study on diastolic function, heart rate and myocardial metabolism following intravenous metoprolol. Eur. Heart J. 1993, 14, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Pozzoli, M.; Cioffi, G.; Traversi, E.; Pinna, G.D.; Cobelli, F.; Tavazzi, L. Predictors of primary atrial fibrillation and concomitant clinical and hemodynamic changes in patients with chronic heart failure: A prospective study in 344 patients with baseline sinus rhythm. J. Am. Coll. Cardiol. 1998, 32, 197–204. [Google Scholar] [CrossRef] [Green Version]
- Santhanakrishnan, R.; Wang, N.; Larson, M.G.; Magnani, J.W.; McManus, D.D.; Lubitz, S.A.; Ellinor, P.T.; Cheng, S.; Vasan, R.S.; Lee, D.S.; et al. Atrial Fibrillation Begets Heart Failure and Vice Versa: Temporal Associations and Differences in Preserved versus Reduced Ejection Fraction. Circulation 2016, 133, 484–492. [Google Scholar] [CrossRef] [Green Version]
- Jabre, P.; Roger, V.L.; Murad, M.H.; Chamberlain, A.M.; Prokop, L.; Adnet, F.; Jouven, X. Mortality Associated with Atrial Fibrillation in Patients with Myocardial Infarction: A Systematic Review and Meta-Analysis. Circulation 2011, 123, 1587–1593. [Google Scholar] [CrossRef]
- Crossley, G.H.; Chen, J.; Choucair, W.; Cohen, T.J.; Gohn, D.C.; Johnson, W.B.; Kennedy, E.E.; Mongeon, L.R.; Serwer, G.A.; Qiao, H.; et al. Clinical Benefits of Remote versus Transtelephonic Monitoring of Implanted Pacemakers. J. Am. Coll. Cardiol. 2009, 54, 2012–2019. [Google Scholar] [CrossRef] [Green Version]
- Boriani, G.; Tukkie, R.; Manolis, A.S.; Mont, L.; Pürerfellner, H.; Santini, M.; Inama, G.; Serra, P.; De Sousa, J.; Botto, G.L.; et al. Atrial Antitachycardia Pacing and Managed Ventricular Pacing in Bradycardia Patients with Paroxysmal or Persistent Atrial Tachyarrhythmias: The Minerva Randomized Multicentre International Trial. Eur. Heart J. 2014, 35, 2352–2362. [Google Scholar] [CrossRef] [Green Version]
- Marrouche, N.F.; Brachmann, J.; Andresen, D.; Siebels, J.; Boersma, L.; Jordaens, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Proff, J.; et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N. Engl. J. Med. 2018, 378, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Camm, A.J.; Goette, A.; Brandes, A.; Eckardt, L.; Elvan, A.; Fetsch, T.; van Gelder, I.C.; Haase, D.; Haegeli, L.M.; et al. Early Rhythm-Control Therapy in Patients with Atrial Fibrillation. N. Engl. J. Med. 2020, 383, 1305–1316. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 63) | AHRE ≥24 h (n = 22) | AHRE <24 h (n = 41) | p-Value | |
|---|---|---|---|---|
| Age (years), mean ± SD | 68 ± 16 | 67 ± 14 | 69 ± 16 | 0.51 |
| Male sex, n (%) | 45 (71) | 18 (82) | 27 (66) | 0.18 |
| BW (kg), mean ± SD | 60 ± 10 | 63 ± 9 | 59 ± 10 | 0.14 |
| † ICD/CRT, n (%) | 35 (56) | 16 (73) | 19 (46) | 0.04 |
| SBP (mmHg), mean ± SD | 127 ± 28 | 118 ± 21 | 132 ± 30 | 0.06 |
| HR (min−1), mean ± SD | 66 ± 12 | 67 ± 10 | 65 ± 13 | 0.51 |
| NYHA class, mean ± SD | 1.4 ± 0.6 | 1.6 ± 0.6 | 1.4 ± 0.6 | 0.1 |
| History of HFH, n (%) | 9 (14) | 5 (23) | 4 (10) | 0.16 |
| CHA2DS2-VASc, mean ± SD | 3 ± 1.8 | 2.9 ± 1.8 | 3 ± 1.8 | 0.78 |
| HAS-BLED, mean ± SD | 1.4 ± 1.2 | 1.4 ± 1 | 1.5 ± 1.2 | 0.85 |
| Etiology of SHD | ||||
| CAD, n (%) | 9 (14) | 5 (23) | 4 (10) | 0.16 |
| DCM/DHCM, n (%) | 8 (13) | 2 (9) | 6 (15) | 0.52 |
| HCM, n (%) | 12 (19) | 6 (27) | 6 (15) | 0.22 |
| VHD, n (%) | 3 (5) | 1 (5) | 2 (5) | 0.95 |
| CHD, n (%) | 4 (6) | 3 (14) | 1 (2) | 0.08 |
| Echocardiographic parameter | ||||
| † LVDd (mm), mean ± SD | 53 ± 11 | 56 ± 11 | 51 ± 11 | 0.03 |
| LVEF (%), mean ± SD | 55 ± 18 | 51 ± 19 | 57 ± 18 | 0.16 |
| LAD (mm), mean ± SD | 42 ± 7 | 43 ± 9 | 41 ± 6 | 0.14 |
| Therapeutic agent | ||||
| ACEI/ARB, n (%) | 37 (59) | 15 (68) | 22 (54) | 0.26 |
| Beta blocker, n (%) | 36 (57) | 15 (68) | 21 (51) | 0.19 |
| MRA, n (%) | 19 (30) | 6 (27) | 13 (31) | 0.71 |
| Diuretics, n (%) | 24 (38) | 10 (45) | 14 (34) | 0.38 |
| Amiodarone, n (%) | 15 (24) | 8 (36) | 7 (17) | 0.09 |
| VKA/DOAC, n (%) | 14 (22) | 7 (32) | 7 (17) | 0.18 |
| Laboratory data | ||||
| eGFR (mL/min/1.73 m2), mean ± SD | 59 ± 23 | 54 ± 20 | 62 ± 24 | 0.17 |
| BNP level (pg/mL), median (IQR) | 183 (72, 379) | 258 (72, 417) | 131 (64, 372) | 0.29 |
| Total (n = 69) | AHRE ≥24 h (n = 37) | AHRE <24 h (n = 32) | p-Value | |
|---|---|---|---|---|
| Age (years), mean ± SD | 71 ± 11 | 71 ± 11 | 70 ± 12 | 0.57 |
| Male sex, n (%) | 43 (62) | 22 (59) | 21 (66) | 0.6 |
| BW (kg), mean ± SD | 58 ± 12 | 56 ± 11 | 59 ± 13 | 0.38 |
| ICD/CRT, n (%) | 31 (45) | 19 (51) | 12 (38) | 0.25 |
| SBP (mmHg), mean ± SD | 124 ± 17 | 123 ± 17 | 125 ± 17 | 0.38 |
| HR (min−1), mean ± SD | 67 ± 12 | 69 ± 11 | 65 ± 14 | 0.1 |
| NYHA class, mean ± SD | 1.5 ± 0.7 | 1.6 ± 0.7 | 1.4 ± 0.7 | 0.24 |
| History of HFH, n (%) | 14 (20) | 8 (22) | 6 (19) | 0.76 |
| CHA2DS2-VASc, mean ± SD | 3.5 ± 1.7 | 3.8 ± 1.8 | 3.1 ± 1.6 | 0.14 |
| HAS-BLED, mean ± SD | 1.9 ± 1.4 | 2.3 ± 1.6 | 1.5 ± 1 | 0.06 |
| Etiology of SHD | ||||
| CAD, n (%) | 11 (16) | 8 (22) | 3 (9) | 0.16 |
| DCM/DHCM, n (%) | 2 (3) | 2 (5) | 0 | 0.18 |
| HCM, n (%) | 10 (14) | 6 (16) | 4 (12) | 0.66 |
| VHD, n (%) | 7 (10) | 6 (16) | 1 (3) | 0.07 |
| CHD, n (%) | 2 (3) | 1 (3) | 1 (3) | 0.91 |
| Echocardiographic parameter | ||||
| LVDd (mm), mean ± SD | 50 ± 7 | 50 ± 8 | 49 ± 6 | 0.79 |
| LVEF (%), mean ± SD | 56 ± 14 | 54 ± 14 | 58 ± 13 | 0.14 |
| LAD (mm), mean ± SD | 43 ± 7 | 44 ± 7 | 43 ± 7 | 0.55 |
| Therapeutic agent | ||||
| ACEI/ARB, n (%) | 46 (67) | 24 (65) | 22 (69) | 0.59 |
| Beta blocker, n (%) | 43 (62) | 21 (57) | 22 (69) | 0.22 |
| MRA, n (%) | 15 (22) | 9 (24) | 6 (19) | 0.62 |
| Diuretics, n (%) | 30 (43) | 17 (46) | 13 (41) | 0.74 |
| Amiodarone, n (%) | 15 (22) | 11 (30) | 4 (13) | 0.09 |
| VKA/DOAC, n (%) | 66 (96) | 34 (92) | 32 (100) | 0.1 |
| Laboratory data | ||||
| eGFR (mL/min/1.73 m2), mean ± SD | 52 ± 20 | 49 ± 21 | 55 ± 19 | 0.3 |
| † BNP level (pg/mL), median (IQR) | 138 (57, 315) | 172 (102, 382) | 90 (40, 216) | 0.04 |
| (a) Without a History of AF | |||
| AHRE ≥24 h | AHRE <24 h | p-Value | |
| † MACE, % (95% CI) | 92 (78, 100) | 30 (11, 49) | 0.005 |
| All-cause death, % (95% CI) | 73 (33, 100) | 28 (8, 48) | 0.88 |
| † HFH, % (95% CI) | 72 (48, 97) | 30 (0, 70) | 0.0003 |
| Stroke, % (95% CI) | 5 (0, 14) | 4 (0, 10) | 0.86 |
| ACS, % (95% CI) | 0 | 0 | N/A |
| (b) With a History of AF | |||
| AHRE ≥24 h | AHRE <24 h | p-Value | |
| MACE, % (95% CI) | 54 (29, 79) | 26 (9, 43) | 0.44 |
| All-cause death, % (95% CI) | 24 (1, 47) | 19 (1, 38) | 0.51 |
| HFH, % (95% CI) | 46 (22, 71) | 14 (1, 27) | 0.12 |
| Stroke, % (95% CI) | 0 | 0 | N/A |
| ACS, % (95% CI) | 0 | 4 (0, 12) | 0.25 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age >75 years | 2.1 | 0.92–4.8 | 0.08 | 1.5 | 0.61–3.4 | 0.39 |
| Male sex | 2.2 | 0.77–6.5 | 0.14 | |||
| † AHRE ≥24 h | 3.2 | 1.3–7.4 | 0.007 | 3.0 | 1.1–8.1 | 0.03 |
| NYHA >2 | 3.8 | 0.48–31 | 0.2 | |||
| CHA2DS2-VASc ≥3 | 1.3 | 0.59–3 | 0.48 | |||
| HAS-BLED ≥3 | 1.6 | 0.5–4.8 | 0.41 | |||
| LVDd >55 mm | 1.5 | 0.63–3.7 | 0.35 | |||
| VKA/DOAC | 1.5 | 0.6-3.8 | 0.37 | |||
| LVEF <40% | 2.3 | 0.9–5.9 | 0.08 | 1.6 | 0.52–4.7 | 0.42 |
| LAD >45 mm | 1.7 | 0.77–3.8 | 0.18 | |||
| eGFR <30 mL/min/1.73 m2 | 1.9 | 0.84–4.6 | 0.11 | |||
| BNP level >200 pg/mL | 2.7 | 1.1–6.3 | 0.02 | 2.1 | 0.74–6.1 | 0.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishiguchi, H.; Yoshiga, Y.; Shimizu, A.; Ueyama, T.; Ono, M.; Fukuda, M.; Kato, T.; Fujii, S.; Hisaoka, M.; Uchida, T.; et al. The Differential Prognostic Impact of Long-Duration Atrial High-Rate Episodes Detected by Cardiac Implantable Electronic Devices between Patients with and without a History of Atrial Fibrillation. J. Clin. Med. 2022, 11, 1732. https://doi.org/10.3390/jcm11061732
Ishiguchi H, Yoshiga Y, Shimizu A, Ueyama T, Ono M, Fukuda M, Kato T, Fujii S, Hisaoka M, Uchida T, et al. The Differential Prognostic Impact of Long-Duration Atrial High-Rate Episodes Detected by Cardiac Implantable Electronic Devices between Patients with and without a History of Atrial Fibrillation. Journal of Clinical Medicine. 2022; 11(6):1732. https://doi.org/10.3390/jcm11061732
Chicago/Turabian StyleIshiguchi, Hironori, Yasuhiro Yoshiga, Akihiko Shimizu, Takeshi Ueyama, Makoto Ono, Masakazu Fukuda, Takayoshi Kato, Shohei Fujii, Masahiro Hisaoka, Tomoyuki Uchida, and et al. 2022. "The Differential Prognostic Impact of Long-Duration Atrial High-Rate Episodes Detected by Cardiac Implantable Electronic Devices between Patients with and without a History of Atrial Fibrillation" Journal of Clinical Medicine 11, no. 6: 1732. https://doi.org/10.3390/jcm11061732
APA StyleIshiguchi, H., Yoshiga, Y., Shimizu, A., Ueyama, T., Ono, M., Fukuda, M., Kato, T., Fujii, S., Hisaoka, M., Uchida, T., Omuro, T., Okamura, T., Kobayashi, S., & Yano, M. (2022). The Differential Prognostic Impact of Long-Duration Atrial High-Rate Episodes Detected by Cardiac Implantable Electronic Devices between Patients with and without a History of Atrial Fibrillation. Journal of Clinical Medicine, 11(6), 1732. https://doi.org/10.3390/jcm11061732