Profile of Clinical and Analytical Parameters in Bronchiectasis Patients during the COVID-19 Pandemic: A One-Year Follow-Up Pilot Study
Abstract
:1. Introduction
2. Methods
2.1. Clinical Assessment at Baseline and at One-Year Follow-Up Time-Points
2.2. Bronchiectasis Disease Severity Scores
2.3. Radiological Features and Extension
2.4. Microbiological Diagnosis
2.5. Statistical Analysis
3. Results
3.1. General Characteristics at Baseline
3.2. Systemic Inflammatory Parameters and Immunoglobulins (Ig) at Baseline
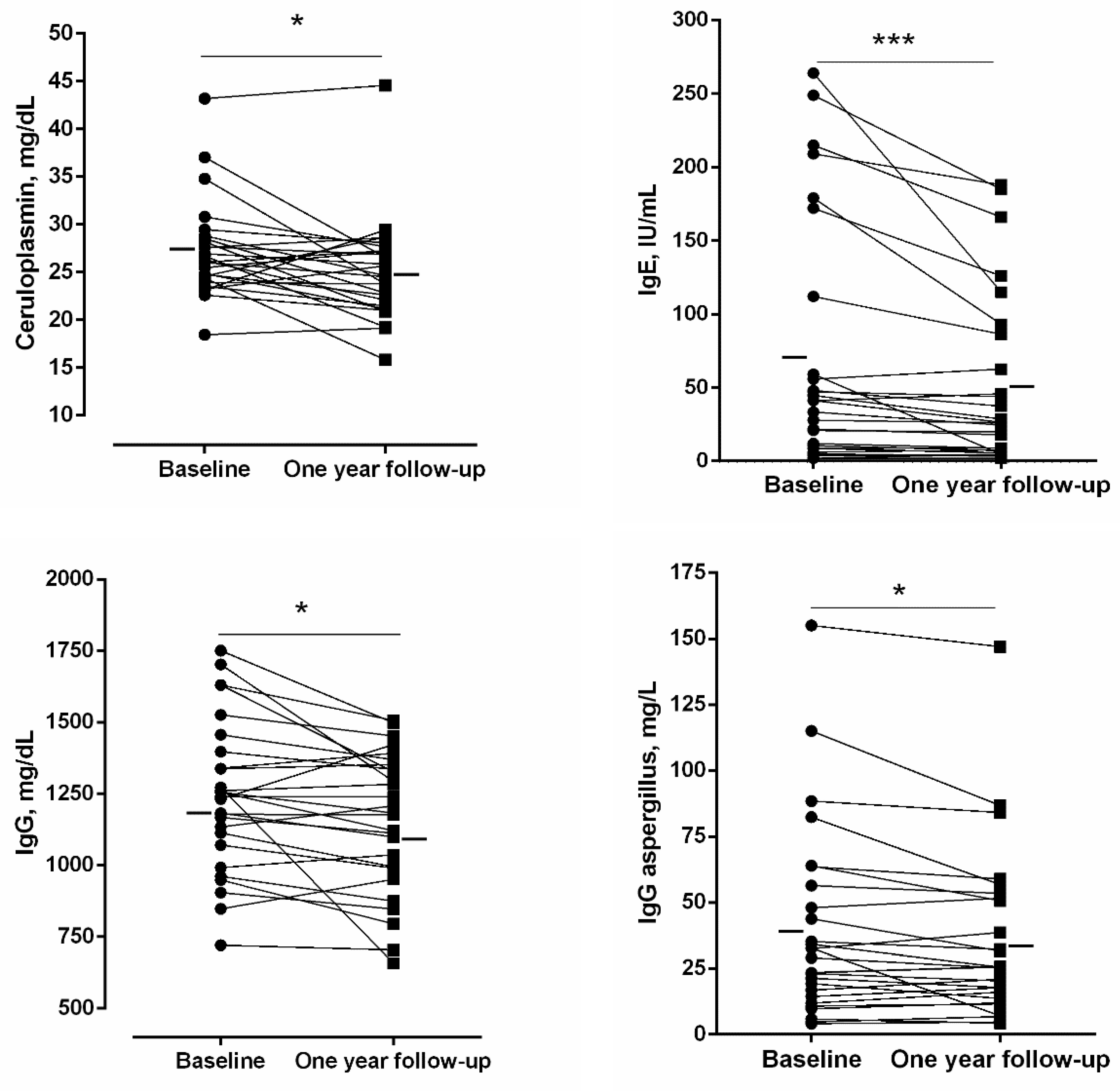
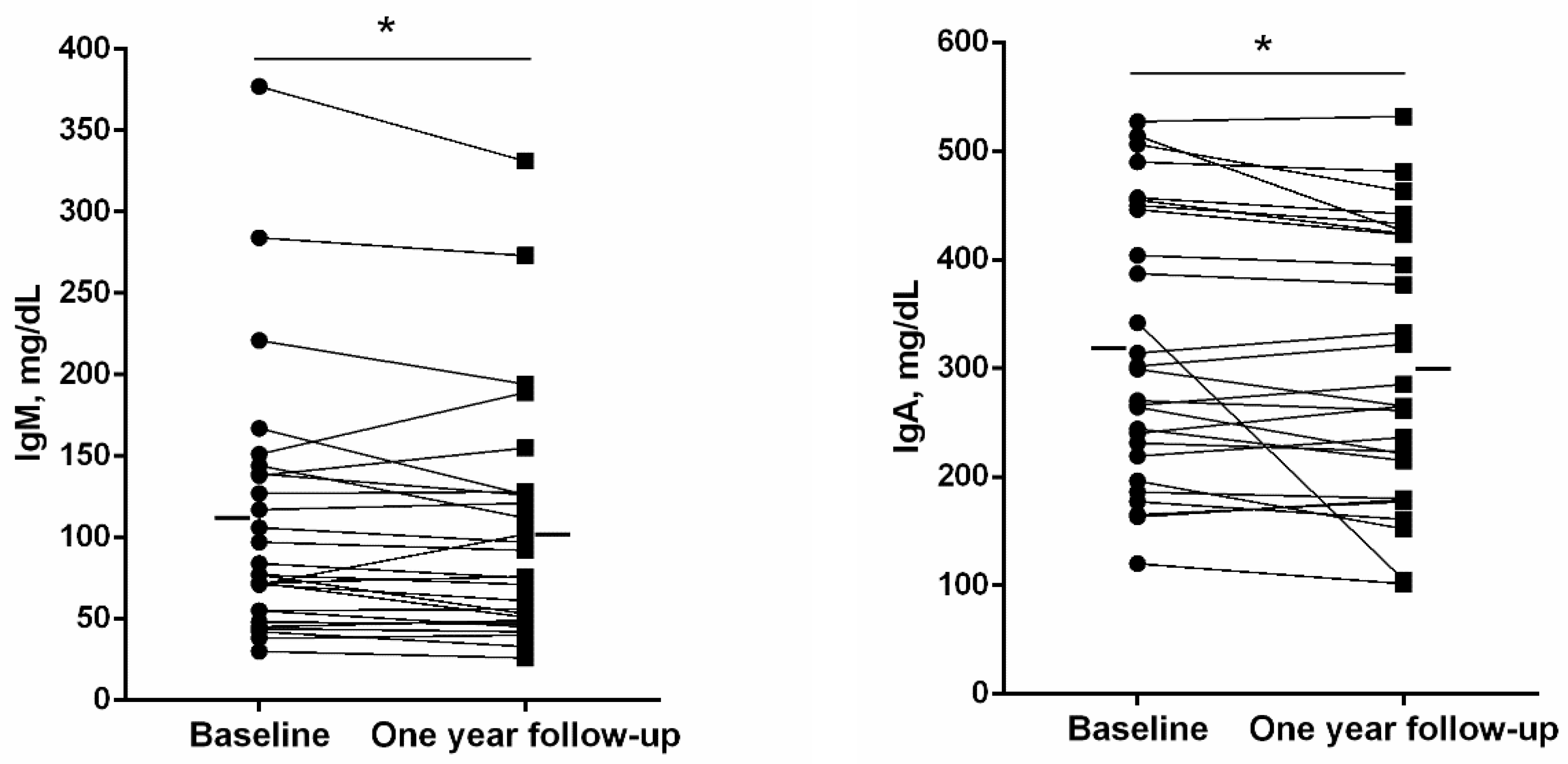
3.3. General Clinical Characteristics at One-Year Follow-Up
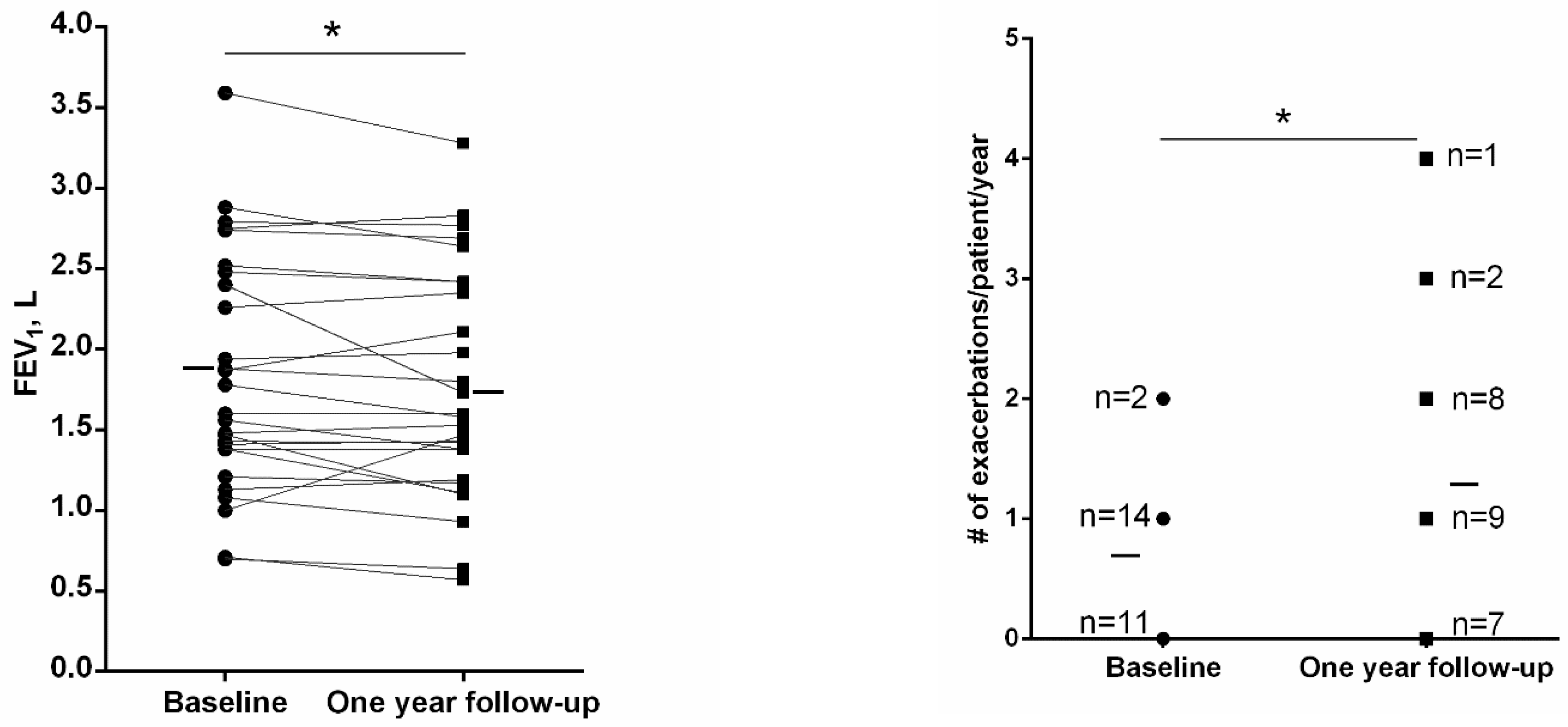
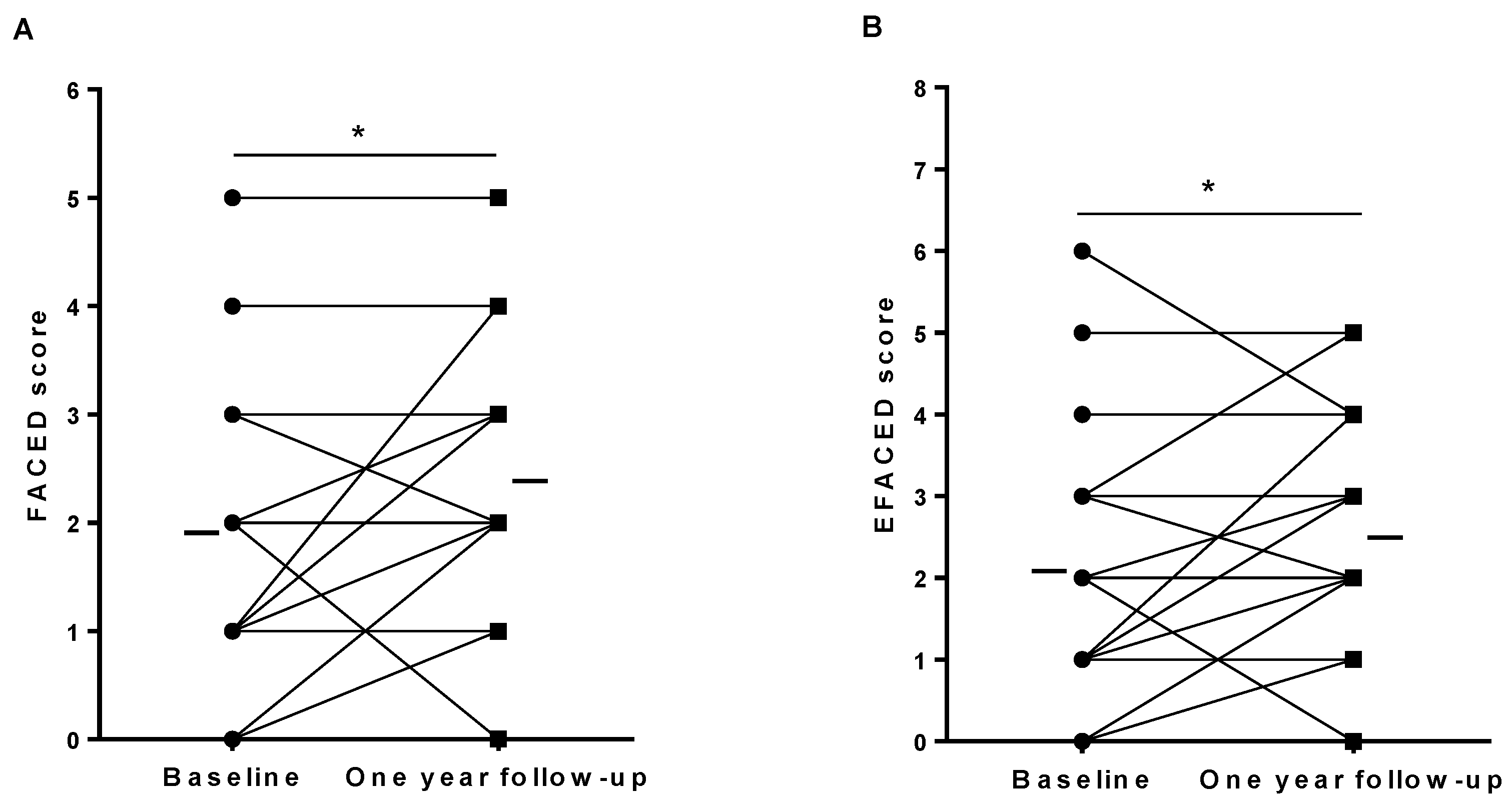
3.4. Systemic Inflammatory Parameters and Immunoglobulins (Ig) at One-Year Follow-Up
3.5. Microbiological Status of the Sputum at Baseline and One-Year Follow-Up
4. Discussion
Study Critique
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martínez-García, M.Á.; Máiz, L.; Olveira, C.; Girón, R.M.; de la Rosa, D.; Blanco, M.; Cantón, R.; Vendrell, M.; Polverino, E.; de Gracia, J.; et al. Spanish Guidelines on the Evaluation and Diagnosis of Bronchiectasis in Adults. Arch. Bronconeumol. 2018, 54, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Martinez-García, M.A.; Villa, C.; Dobarganes, Y.; Girón, R.; Maíz, L.; García-Clemente, M.; Sibila, O.; Golpe, R.; Rodríguez, J.; Barreiro, E.; et al. RIBRON: El Registro Español Informatizado De Bronquiectasias. Caracterización De Los Primeros 1.912 Pacientes. Arch. Bronconeumol. 2021, 57, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Cuartin, G.; Chalmers, J.D.; Sibila, O. Diagnostic Challenges of Bronchiectasis. Respir. Med. 2016, 116, 70–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crimi, C.; Ferri, S.; Campisi, R.; Crimi, N. The Link between Asthma and Bronchiectasis: State of the Art. Respiration 2020, 99, 463–476. [Google Scholar] [CrossRef]
- Jin, J.; Yu, W.; Li, S.; Lu, L.; Liu, X.; Sun, Y. Factors Associated with Bronchiectasis in Patients with Moderate-Severe Chronic Obstructive Pulmonary Disease. Medicine 2016, 95, e4219. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.Á.; Soler-Cataluña, J.J.; Donat Sanz, Y.; Catalán Serra, P.; Agramunt Lerma, M.; Ballestín Vicente, J.; Perpiñá-Tordera, M. Factors Associated with Bronchiectasis in Patients with COPD. Chest 2011, 140, 1130–1137. [Google Scholar] [CrossRef]
- Polverino, E.; Dimakou, K.; Hurst, J.; Martinez-Garcia, M.-A.; Miravitlles, M.; Paggiaro, P.; Shteinberg, M.; Aliberti, S.; Chalmers, J.D. The Overlap between Bronchiectasis and Chronic Airway Diseases: State of the Art and Future Directions. Eur. Respir. J. 2018, 52, 1800328. [Google Scholar] [CrossRef] [Green Version]
- Maselli, D.J.; Amalakuhan, B.; Keyt, H.; Diaz, A.A. Suspecting Non-Cystic Fibrosis Bronchiectasis: What the Busy Primary Care Clinician Needs to Know. Int. J. Clin. Pract. 2017, 71, e12924. [Google Scholar] [CrossRef] [Green Version]
- Monteagudo, M.; Rodríguez-Blanco, T.; Barrecheguren, M.; Simonet, P.; Miravitlles, M. Prevalence and Incidence of Bronchiectasis in Catalonia, Spain: A Population-Based Study. Respir. Med. 2016, 121, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Weycker, D.; Hansen, G.L.; Seifer, F.D. Prevalence and Incidence of Noncystic Fibrosis Bronchiectasis among US Adults in 2013. Chron. Respir. Dis. 2017, 14, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Ringshausen, F.C.; de Roux, A.; Pletz, M.W.; Hämäläinen, N.; Welte, T.; Rademacher, J. Bronchiectasis-Associated Hospitalizations in Germany, 2005–2011: A Population-Based Study of Disease Burden and Trends. PLoS ONE 2013, 8, e71109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez-Muñoz, G.; López de Andrés, A.; Jiménez-García, R.; Carrasco-Garrido, P.; Hernández-Barrera, V.; Pedraza-Serrano, F.; Puente-Maestu, L.; de Miguel-Díez, J. Time Trends in Hospital Admissions for Bronchiectasis: Analysis of the Spanish National Hospital Discharge Data (2004 to 2013). PLoS ONE 2016, 11, e0162282. [Google Scholar] [CrossRef]
- Menéndez, R.; Méndez, R.; Polverino, E.; Rosales-Mayor, E.; Amara-Elori, I.; Reyes, S.; Posadas, T.; Fernández-Barat, L.; Torres, A. Factors Associated with Hospitalization in Bronchiectasis Exacerbations: A One-Year Follow-Up Study. Respir. Res. 2017, 18, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, P.T.; Holdsworth, S.R.; Freezer, N.J.; Villanueva, E.; Gallagher, M.; Holmes, P.W. Outcome in Adult Bronchiectasis. COPD 2005, 2, 27–34. [Google Scholar] [CrossRef]
- King, P.T.; Holdsworth, S.R.; Freezer, N.J.; Villanueva, E.; Holmes, P.W. Microbiologic Follow-Up Study in Adult Bronchiectasis. Respir. Med. 2007, 101, 1633–1638. [Google Scholar] [CrossRef] [Green Version]
- McDonnell, M.J.; Aliberti, S.; Goeminne, P.C.; Restrepo, M.I.; Finch, S.; Pesci, A.; Dupont, L.J.; Fardon, T.C.; Wilson, R.; Loebinger, M.R.; et al. Comorbidities and the Risk of Mortality in Patients with Bronchiectasis: An International Multicentre Cohort Study. Lancet. Respir. Med. 2016, 4, 969–979. [Google Scholar] [CrossRef] [Green Version]
- Gorbalenya, A.E.; Baker, S.C.; Baric, R.S.; de Groot, R.J.; Drosten, C.; Gulyaeva, A.A.; Haagmans, B.L.; Lauber, C.; Leontovich, A.M.; Neuman, B.W.; et al. Severe Acute Respiratory Syndrome-Related Coronavirus: The Species and Its Viruses—A Statement of the Coronavirus Study Group. bioRxiv 2020, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Kumar, A.; Singh, R.; Kaur, J.; Pandey, S.; Sharma, V.; Thakur, L.; Sati, S.; Mani, S.; Asthana, S.; Sharma, T.K.; et al. Wuhan to World: The COVID-19 Pandemic. Front. Cell. Infect. Microbiol. 2021, 11, 242. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Chalmers, J.D.; Chang, A.B.; Chotirmall, S.H.; Dhar, R.; McShane, P.J. Bronchiectasis. Nat. Rev. Dis. Primers 2018, 4, 45. [Google Scholar] [CrossRef]
- Celli, B.R.; MacNee, W.; Agusti, A.; Anzueto, A.; Berg, B.; Buist, A.S.; Calverley, P.M.A.; Chavannes, N.; Dillard, T.; Fahy, B.; et al. Standards for the Diagnosis and Treatment of Patients with COPD: A Summary of the ATS/ERS Position Paper. Eur. Respir. J. 2004, 23, 932–946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalmers, J.D.; Goeminne, P.; Aliberti, S.; McDonnell, M.J.; Lonni, S.; Davidson, J.; Poppelwell, L.; Salih, W.; Pesci, A.; Dupont, L.J.; et al. The Bronchiectasis Severity Index. An International Derivation and Validation Study. Am. J. Respir. Crit. Care Med. 2014, 189, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Aliboni, L.; Pennati, F.; Gelmini, A.; Colombo, A.; Ciuni, A.; Milanese, G.; Sverzellati, N.; Magnani, S.; Vespro, V.; Blasi, F.; et al. Detection and Classification of Bronchiectasis through Convolutional Neural Networks. J. Thorac. Imaging 2022, 37, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.A.; De Gracia, J.; Relat, M.V.; Girón, R.M.; Carro, L.M.; De La Rosa Carrillo, D.; Olveira, C.; Martinez-Garcia, M.A.; De Gracia, J.; Vendrell Relat, M.; et al. Multidimensional Approach to Non-Cystic Fibrosis Bronchiectasis: The FACED Score. Eur. Respir. J. 2014, 43, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Garcia, M.A.; Athanazio, R.A.; Girón, R.; Máiz-Carro, L.; de la Rosa, D.; Olveira, C.; de Gracia, J.; Vendrell, M.; Prados-Sánchez, C.; Gramblicka, G.; et al. Predicting High Risk of Exacerbations in Bronchiectasis: The E-FACED Score. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 12, 275–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sancho-Muñoz, A.; Guitart, M.; Rodríguez, D.A.; Gea, J.; Martínez-Llorens, J.; Barreiro, E. Deficient Muscle Regeneration Potential in Sarcopenic COPD Patients: Role of Satellite Cells. J. Cell. Physiol. 2021, 236, 3083–3098. [Google Scholar] [CrossRef]
- Puig-Vilanova, E.; Martínez-Llorens, J.; Ausin, P.; Roca, J.; Gea, J.; Barreiro, E. Quadriceps Muscle Weakness and Atrophy Are Associated wth a Differential Epigenetic Profile in Advanced COPD. Clin. Sci. 2015, 128, 905–921. [Google Scholar] [CrossRef]
- Puig-Vilanova, E.; Rodriguez, D.A.; Lloreta, J.; Ausin, P.; Pascual-Guardia, S.; Broquetas, J.; Roca, J.; Gea, J.; Barreiro, E. Oxidative Stress, Redox Signaling Pathways, and Autophagy in Cachectic Muscles of Male Patients with Advanced COPD and Lung Cancer. Free Radic. Biol. Med. 2015, 79, 91–108. [Google Scholar] [CrossRef]
- Puig-Vilanova, E.; Ausin, P.; Martinez-Llorens, J.; Gea, J.; Barreiro, E. Do Epigenetic Events Take Place in the Vastus Lateralis of Patients with Mild Chronic Obstructive Pulmonary Disease? PLoS ONE 2014, 9, e102296. [Google Scholar] [CrossRef] [Green Version]
- Barreiro, E.; Salazar-Degracia, A.; Sancho-Muñoz, A.; Gea, J. Endoplasmic Reticulum Stress and Unfolded Protein Response Profile in Quadriceps of Sarcopenic Patients with Respiratory Diseases. J. Cell. Physiol. 2019, 234, 11315–11329. [Google Scholar] [CrossRef]
- Rodriguez, D.A.; Kalko, S.; Puig-Vilanova, E.; Perez-Olabarría, M.; Falciani, F.; Gea, J.; Cascante, M.; Barreiro, E.; Roca, J. Muscle and Blood Redox Status after Exercise Training in Severe COPD Patients. Free Radic. Biol. Med. 2012, 52, 88–94. [Google Scholar] [CrossRef]
- Bhalla, M.; Turcios, N.; Aponte, V.; Jenkins, M.; Leitman, B.S.; McCauley, D.I.; Naidich, D.P. Cystic Fibrosis: Scoring System with Thin-Section CT. Radiology 1991, 179, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.R. Airflow Obstruction in Bronchiectasis: Correlation between Computed Tomography Features and Pulmonary Function Tests. Thorax 2000, 55, 198–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, P.R.; Washington, J.A. Microscopic and Bacteriologic Analysis of Expectorated Sputum. Mayo Clin. Proc. 1975, 50, 339–344. [Google Scholar] [PubMed]
- EUCAST: AST of Bacteria. Available online: https://www.eucast.org/ast_of_bacteria/ (accessed on 31 May 2021).
- Martínez-García, M.Á.; Máiz, L.; Olveira, C.; Girón, R.M.; de la Rosa, D.; Blanco, M.; Cantón, R.; Vendrell, M.; Polverino, E.; de Gracia, J.; et al. Spanish Guidelines on Treatment of Bronchiectasis in Adults. Arch. Bronconeumol. (Engl. Ed.) 2018, 54, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Kerstjens, H.A.M.; Rijcken, B.; Schouten, J.P.; Postma, D.S. Decline of FEV1 by Age and Smoking Status: Facts, Figures, and Fallacies. Thorax 1997, 52, 820–827. [Google Scholar] [CrossRef] [Green Version]
- Bhatt, S.P.; Soler, X.; Wang, X.; Murray, S.; Anzueto, A.R.; Beaty, T.H.; Boriek, A.M.; Casaburi, R.; Criner, G.J.; Diaz, A.A.; et al. Association between Functional Small Airway Disease and FEV1 Decline in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2016, 194, 178–184. [Google Scholar] [CrossRef] [Green Version]
- Amati, F.; Simonetta, E.; Gramegna, A.; Tarsia, P.; Contarini, M.; Blasi, F.; Aliberti, S. The Biology of Pulmonary Exacerbations in Bronchiectasis. Eur. Respir. Rev. 2019, 28, 190055. [Google Scholar] [CrossRef] [Green Version]
- Rosales-Mayor, E.; Polverino, E.; Raguer, L.; Alcaraz, V.; Gabarrus, A.; Ranzani, O.; Menendez, R.; Torres, A. Comparison of Two Prognostic Scores (BSI And FACED) in a Spanish Cohort of Adult Patients with Bronchiectasis and Improvement of the FACED Predictive Capacity for Exacerbations. PLoS ONE 2017, 12, e0175171. [Google Scholar] [CrossRef]
- Ellis, H.C.; Cowman, S.; Fernandes, M.; Wilson, R.; Loebinger, M.R. Predicting Mortality in Bronchiectasis Using Bronchiectasis Severity Index and FACED Scores: A 19-Year Cohort Study. Eur. Respir. J. 2016, 47, 482–489. [Google Scholar] [CrossRef] [Green Version]
- Go, D.J.; Lee, E.Y.; Lee, E.B.; Song, Y.W.; Konig, M.F.; Park, J.K. Elevated Erythrocyte Sedimentation Rate Is Predictive of Interstitial Lung Disease and Mortality in Dermatomyositis: A Korean Retrospective Cohort Study. J. Korean Med. Sci. 2016, 31, 389–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarrar, A.; Zaibi, H.; Guediri, N.; Fessi, R.; Ferchichi, M.; Dhahri, B.; Ben Amar, J.; Aouina, H. The association between bronchiectasis and systemic inflammation. Eur. Respir. J. 2019, 54, PA2681. [Google Scholar]
- Gitlin, J.D. Transcriptional Regulation of Ceruloplasmin Gene Expression during Inflammation. J. Biol. Chem. 1988, 263, 6281–6287. [Google Scholar] [CrossRef]
- Mohiuddin, S.S. Role of Ceruloplasmin as a Low Grade Chronic Inflammatory Marker and Activated Innate Immune System in Pathogenesis of Diabetes Mellitus. J. Diabetes Metab. Disord. Control 2018, 5, 148–153. [Google Scholar] [CrossRef] [Green Version]
- Stiller-Winkler, R.; Idel, H.; Leng, G.; Spix, C.; Dolgner, R. Influence of Air Pollution on Humoral Immune Response. J. Clin. Epidemiol. 1996, 49, 527–534. [Google Scholar] [CrossRef]

| Score | Epithelial Cells | Leukocytes | Quality | Culture |
|---|---|---|---|---|
| 1 | >25 | <10 | Very poor | No |
| 2 | >25 | 18–25 | Poor | No |
| 3 | >25 | >25 | Dubious | Yes |
| 4 | 18–25 | >25 | Sufficient | Yes |
| 5 | <10 | >25 | Good | Yes |
| 6 | <25 | <25 | Uncertain | Yes |
| All Patients N = 30 | Non-Pseudomonas aeruginosa N = 21 | Pseudomonas aeruginosa N = 9 | |
|---|---|---|---|
| Age, years | 66 (12) | 69 (11) | 61 (12) * |
| Female, N/male, N | 23/7 | 18/3 | 5/4 |
| Body weight, kg | 64 (16) | 63 (18) | 66 (11) |
| Height, cm | 158 (10) | 157 (11) | 162 (8) |
| BMI (kg/m2) | 25 (4) | 25.5 (4.9) | 24.9 (2.8) |
| Etiology | |||
| Post-infectious, N (%) | 22 (73) | 14 (67) | 8 (89) |
| COPD, N (%) | 1 (3) | 1 (4) | 0 (0) |
| Unknown etiology, N (%) | 7 (24) | 6 (29) | 1 (11) |
| SD) | |||
| FEV1, L | 1.78 (0.71) | 1.76 (0.71) | 1.84 (0.75) |
| FEV1, % predicted | 76 (25) | 80 (25) | 65 (21) |
| FVC, L | 2.68 (0.92) | 2.52 (0.78) | 3.05 (1.15) |
| FVC, % predicted | 85 (18) | 87.9 (18.5) | 78.9 (16.5) |
| FEV1/FVC | 68 (11) | 68.6 (11.2) | 65.6 (12.3) |
| 6-min walking distance, meters | 473 (96) | 450 (95) | 534 (71) * |
| Distance, % predicted | 98 (17) | 96 (16) | 105 (19) |
| Smoking history | |||
| Ex-smokers, N (%) | 9 (30) | 6 (29) | 3 (33) |
| Never smokers, N (%) | 21 (70) | 15 (71) | 6 (67) |
| Packs-year, | 22 (15) | 23 (18) | 12 (3) |
| Disease severity | |||
| FACED score, | 1.9 (1.3) | 1.95 (1.43) | 1.89 (1.05) |
| Mild, N | 20 | 13 | 7 |
| Moderate, N | 8 | 6 | 2 |
| Severe, N | 2 | 2 | 0 |
| EFACED score, | 2.1 (1.5) | 2.05 (1.50) | 2.33 (1.73) |
| Mild, N | 25 | 18 | 7 |
| Moderate, N | 5 | 3 | 2 |
| Severe, N | 0 | 0 | 0 |
| SD) | 5.5 (3.2) | 5.19 (2.62) | 6.33 (4.36) |
| Mild, N | 14 | 10 | 4 |
| Moderate, N | 11 | 8 | 3 |
| Severe, N | 5 | 3 | 2 |
| SD) | 0.63 (0.67) | 0.71 (0.46) | 0.22 (0.44) * |
| # exacerbations/patient/year, | 0.87 (1.00) | 0.86 (0.66) | 0.89 (1.62) |
| # hospitalizations/patient for exacerbations in the previous year, | 0.10 (0.31) | 0.05 (0.22) | 0.22 (0.44) |
| SD) | |||
| Hemoglobin, g/dL | 13.9 (11.1) | 13.7 (1.1) | 14.3 (1.2) |
| Hematocrit, % | 42.0 (3.7) | 41.4 (3.6) | 43.4 (3.8) |
| Glucose, mg/dL | 94.4 (25.5) | 98.8 (29.1) | 84.1 (8.8) |
| Creatinine, mg/dL | 0.7 (0.3) | 0.71 (0.17) | 0.79 (0.18) |
| Albumin, g/dL | 4.4 (0.3) | 4.4 (0.3) | 4.3 (0.3) |
| Total proteins, g/dL | 7.3 (0.4) | 7.2 (0.3) | 7.5 (0.5) |
| Prealbumin, g/dL | 22.1 (5.0) | 22.4 (4.6) | 21.4 (6.1) |
| SD) | |||
| Total extension score | 8.1 (3.3) | 7.1 (3.0) | 10.2 (3.0) * |
| Bronchial dilatation score | 1.2 (0.2) | 1.2 (0.2) | 1.2 (0.2) |
| Bronchial wall thickness score | 1.3 (0.3) | 1.3 (0.4) | 1.3 (0.3) |
| Global score | 10.6 (3.4) | 9.6 (3.2) | 12.8 (2.9) * |
| Treatments | |||
| Bronchodilators, N | 23 (77%) | 16 (76%) | 7 (78%) |
| Inhaled corticoids, N | 10 (33%) | 6 (29%) | 4 (44%) |
| Mucolytics, N | 2 (7%) | 2 (10%) | 0 |
| Eradication protocol for PA | 9 (30%) | NA | 9 (100%) |
| Respiratory physiotherapy, N | 14 (47%) | 12 (57%) | 2 (22%) |
| All Patients N = 30 | Non-Pseudomonas aeruginosa N = 21 | Pseudomonas aeruginosa N = 9 | |
|---|---|---|---|
| Total leukocytes, ×103/µL | 6.4 (1.6) | 6.4 (1.5) | 6.3 (1.9) |
| Total neutrophils, ×103/µL | 4.1 (1.4) | 4.1 (1.3) | 4.0 (1.5) |
| Neutrophils, % | 63.2 (7.8) | 63.7 (7.7) | 62.0 (8.2) |
| Total lymphocytes, ×103/µL | 1.5 (0.4) | 1.5 (0.4) | 1.5 (0.4) |
| Lymphocytes, % | 24.5 (6.2) | 24.6 (7.0) | 24.2 (3.8) |
| Total eosinophils, ×103/µL | 0.16 (0.09) | 0.15 (0.07) | 0.20 (0.14) |
| Eosinophils, % | 2.5 (1.4) | 2.4 (1.1) | 2.9 (2.0) |
| Platelets, ×103/µL | 257 (69) | 254 (63) | 265 (86) |
| CRP, mg/dL | 0.70 (0.9) | 0.76 (1.07) | 0.60 (0.37) |
| ESR, mm/h | 15 (12) | 16 (14) | 13 (10) |
| Fibrinogen, mg/dL | 370 (84) | 370 (89) | 369 (75) |
| Alpha-1 antitrypsin, mg/dL | 132.5 (25.4) | 132.8 (26.7) | 131.7 (23.7) |
| Ceruloplasmin, mg/dL | 27.0 (5.4) | 27.2 (6.3) | 26.7 (2.9) |
| IgE, IU/mL | 66 (81) | 57 (75) | 85 (95) |
| IgG, mg/dL | 1273 (384) | 1161 (259) | 1535 (506) * |
| IgG aspergillus, mg/L | 37 (35) | 37 (37) | 36 (30) |
| IgM, mg/dL | 112 (85) | 83 (42) | 150 (94) * |
| IgA, mg/dL | 330 (134) | 295 (120) | 390 (152) * |
| Patients | # Exacerbations/Patient/Year | # Hospitalizations/Patient for Exacerbations in the Previous Year | ||
|---|---|---|---|---|
| Baseline | One-Year Follow-Up | Baseline | One-Year Follow-Up | |
| Patient # 1 | 1 | 1 | 0 | 0 |
| Patient # 2 | 1 | 2 | 0 | 0 |
| Patient # 3 | 0 | 2 | 0 | 0 |
| Patient # 4 | 1 | 0 | 1 | 0 |
| Patient # 5 | 1 | 0 | 0 | 0 |
| Patient # 6 | 1 | 2 | 0 | 0 |
| Patient # 7 | 0 | 1 | 0 | 0 |
| Patient # 8 | 0 | 1 | 0 | 0 |
| Patient # 9 | 0 | 4 | 0 | 0 |
| Patient # 10 | 2 | NA | 0 | NA |
| Patient # 11 | 1 | 2 | 0 | 0 |
| Patient # 12 | 1 | 2 | 0 | 0 |
| Patient # 13 | 0 | 0 | 0 | 0 |
| Patient # 14 | 0 | 3 | 0 | 0 |
| Patient # 15 | 0 | 0 | 0 | 0 |
| Patient # 16 | 1 | 1 | 0 | 0 |
| Patient # 17 | 0 | 2 | 0 | 0 |
| Patient # 18 | 1 | 0 | 0 | 0 |
| Patient # 19 | 1 | 1 | 1 | 1 |
| Patient # 20 | 0 | 1 | 0 | 0 |
| Patient # 21 | 1 | 1 | 0 | 0 |
| Patient # 22 | 2 | 0 | 0 | 0 |
| Patient # 23 | 2 | 3 | 0 | 0 |
| Patient # 24 | 2 | NA | 0 | NA |
| Patient # 25 | 1 | 2 | 0 | 1 |
| Patient # 26 | 1 | 2 | 0 | 0 |
| Patient # 27 | 3 | NA | 1 | NA |
| Patient # 28 | 0 | 0 | 0 | 0 |
| Patient # 29 | 0 | 1 | 0 | 0 |
| Patient # 30 | 1 | 1 | 0 | 0 |
| Baseline | One-Year Follow-Up | |
|---|---|---|
| Age, years | 66 (12) | 67 (12) *** |
| Female, N/male, N | 20/7 | 20/7 |
| Body weight, kg | 65 (17) | 65 (17) |
| Height, cm | 159 (10) | 159 (10) |
| BMI (kg/m2) | 25.4 (4.4) | 25.3 (4.5) |
| Etiology | ||
| Post-infectious, N (%) | 20 (74) | 20 (74) |
| COPD, N (%) | 0 (0) | 0 (0) |
| Unknown etiology, N (%) | 7 (26) | 7 (26) |
| SD) | ||
| FEV1, % predicted | 76.1 (24.8) | 74.4 (25.5) |
| FVC, L | 2.69 (0.95) | 2.54 (0.86) |
| FVC, % predicted | 85 (19) | 85 (18) |
| FEV1/FVC | 68.3 (11.8) | 67.4 (12.4) |
| 6-min walking distance, meters | 490 (89) | 477 (96) |
| Distance, % predicted | 101 (16) | 97 (16) |
| Smoking history | ||
| Ex-smokers, N (%) | 7 (26) | 7 (26) |
| Never smokers, N (%) | 20 (74) | 20 (74) |
| SD) | 23 (16) | 23 (16) |
| Disease severity | ||
| SD) | 5.2 (2.9) | 5.7 (2.1) |
| SD) | 0.67 (0.68) | 0.70 (0.78) |
| SD) | 0.07 (0.27) | 0.07 (0.27) |
| SD) | ||
| Hemoglobin, g/dL | 14.0 (1.2) | 13.5 (1.0) * |
| Hematocrit, % | 42.0 (3.5) | 39.2 (10.4) |
| Glucose, mg/dL | 94.3 (26.3) | 97.0 (23.8) |
| Creatinine, mg/dL | 0.74 (0.18) | 0.75 (0.15) |
| Albumin, g/dL | 4.4 (0.2) | 4.4 (0.3) |
| Total proteins, g/dL | 7.3 (0.3) | 7.2 (0.4) |
| Prealbumin, g/dL | 22.3 (4.5) | 21.8 (4.6) |
| SD) | ||
| Total extension score | 8.2 (3.2) | NA |
| Bronchial dilatation score | 1.2 (0.2) | NA |
| Bronchial wall thickness score | 1.3 (0.3) | NA |
| Global score | 10.7 (3.3) | NA |
| Baseline | One-Year Follow-Up | |
|---|---|---|
| Total leukocytes, ×103/µL | 6.3 (1.6) | 6.2 (1.5) |
| Total neutrophils, ×103/µL | 4.1 (1.4) | 4.0 (1.2) |
| Neutrophils, % | 63.0 (8.1) | 62.5 (8.1) |
| Total lymphocytes, ×103/µL | 1.5 (0.4) | 1.5 (0.5) |
| Lymphocytes, % | 24.6 (6.5) | 25.2 (8.6) |
| Total eosinophils, ×103/µL | 0.17 (0.09) | 0.16 (0.08) |
| Eosinophils, % | 2.8 (1.3) | 3.0 (1.7) |
| Platelets, ×103/µL | 262 (70) | 241 (56) * |
| CRP, mg/dL | 0.59 (0.63) | 0.51 (0.46) |
| Fibrinogen, mg/dL | 379 (62) | 396 (70) |
| Alpha-1 antitrypsin, mg/dL | 130.8 (25.3) | 131.3 (22.3) |
| Patients | Baseline | One Year Follow-Up | ||
|---|---|---|---|---|
| Germs | Score | Germs | Score | |
| Patient # 1 | Haemophilus influenza, S | 5 | Haemophilus influenza, S | 5 |
| Patient # 2 | Moraxella catarrhalis, S | 5 | NC, S | 1 |
| Patient # 3 | Pseudomonas aeruginosa, S | 3 | Pseudomonas aeruginosa, S | 5 |
| Patient # 4 | Pseudomonas aeruginosa, S | 3 | Pseudomonas aeruginosa, S | 5 |
| Patient # 5 | Commensal microbiota, S | 5 | Moraxella catarrhalis, S | 4 |
| Patient # 6 | Pseudomonas aeruginosa, S | 5 | NC, S | 2 |
| Patient # 7 | Commensal microbiota, S | 6 | NSA | NA |
| Patient # 8 | Pseudomonas aeruginosa, S | 5 | Pseudomonas aeruginosa, S | 3 |
| Patient # 9 | Pseudomonas aeruginosa, S | 5 | Pseudomonas aeruginosa, S | 6 |
| Patient # 10 | Commensal microbiota, S | 5 | NA | NA |
| Patient # 11 | Commensal microbiota, S | 5 | Commensal microbiota, S | 4 |
| Patient # 12 | Commensal microbiota, S | 5 | NC, S | 1 |
| Patient # 13 | NSA, I | NA | NSA | NA |
| Patient # 14 | Pseudomonas aeruginosa, S | 5 | Commensal microbiota, S | 4 |
| Patient # 15 | Commensal microbiota, S | 6 | NC, S | 1 |
| Patient # 16 | Pseudomonas aeruginosa, S | 5 | NSA | NA |
| Patient # 17 | Commensal microbiota, S | 5 | Stenotrophomonas maltophilia | 5 |
| Patient # 18 | NSA, I | NA | NSA | NA |
| Patient # 19 | Commensal microbiota, S | 5 | NSA | NA |
| Patient # 20 | Commensal microbiota, S | 5 | Haemophilus influenza, S | 4 |
| Patient # 21 | Commensal microbiota, S | 6 | Commensal microbiota, S | 3 |
| Patient # 22 | NC, S | 2 | NC, S | 1 |
| Patient # 23 | Commensal microbiota, S | 3 | Commensal microbiota, S | 4 |
| Patient # 24 | NSA, I | NA | NA | NA |
| Patient # 25 | NSA, I | NA | Pseudomonas aeruginosa, S | 4 |
| Patient # 26 | Commensal microbiota, S | 6 | NC, S | 1 |
| Patient # 27 | Pseudomonas aeruginosa, S | 6 | NA | NA |
| Patient # 28 | Commensal microbiota, S | 6 | Pseudomonas aeruginosa, S | 3 |
| Patient # 29 | Pseudomonas aeruginosa, S | 6 | Pseudomonas aeruginosa, S | 5 |
| Patient # 30 | Commensal microbiota, S | 6 | NSA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qin, L.; Gonçalves-Carvalho, F.; Xia, Y.; Zha, J.; Admetlló, M.; Maiques, J.M.; Esteban-Cucó, S.; Duran, X.; Marín, A.; Barreiro, E. Profile of Clinical and Analytical Parameters in Bronchiectasis Patients during the COVID-19 Pandemic: A One-Year Follow-Up Pilot Study. J. Clin. Med. 2022, 11, 1727. https://doi.org/10.3390/jcm11061727
Qin L, Gonçalves-Carvalho F, Xia Y, Zha J, Admetlló M, Maiques JM, Esteban-Cucó S, Duran X, Marín A, Barreiro E. Profile of Clinical and Analytical Parameters in Bronchiectasis Patients during the COVID-19 Pandemic: A One-Year Follow-Up Pilot Study. Journal of Clinical Medicine. 2022; 11(6):1727. https://doi.org/10.3390/jcm11061727
Chicago/Turabian StyleQin, Liyun, Filipe Gonçalves-Carvalho, Yingchen Xia, Jianhua Zha, Mireia Admetlló, José María Maiques, Sandra Esteban-Cucó, Xavier Duran, Alicia Marín, and Esther Barreiro. 2022. "Profile of Clinical and Analytical Parameters in Bronchiectasis Patients during the COVID-19 Pandemic: A One-Year Follow-Up Pilot Study" Journal of Clinical Medicine 11, no. 6: 1727. https://doi.org/10.3390/jcm11061727
APA StyleQin, L., Gonçalves-Carvalho, F., Xia, Y., Zha, J., Admetlló, M., Maiques, J. M., Esteban-Cucó, S., Duran, X., Marín, A., & Barreiro, E. (2022). Profile of Clinical and Analytical Parameters in Bronchiectasis Patients during the COVID-19 Pandemic: A One-Year Follow-Up Pilot Study. Journal of Clinical Medicine, 11(6), 1727. https://doi.org/10.3390/jcm11061727







