Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Imaging Analysis
2.3. Morphological and Histological Evaluation
2.4. Statistical Analysis
3. Results
3.1. Nodules on Imaging
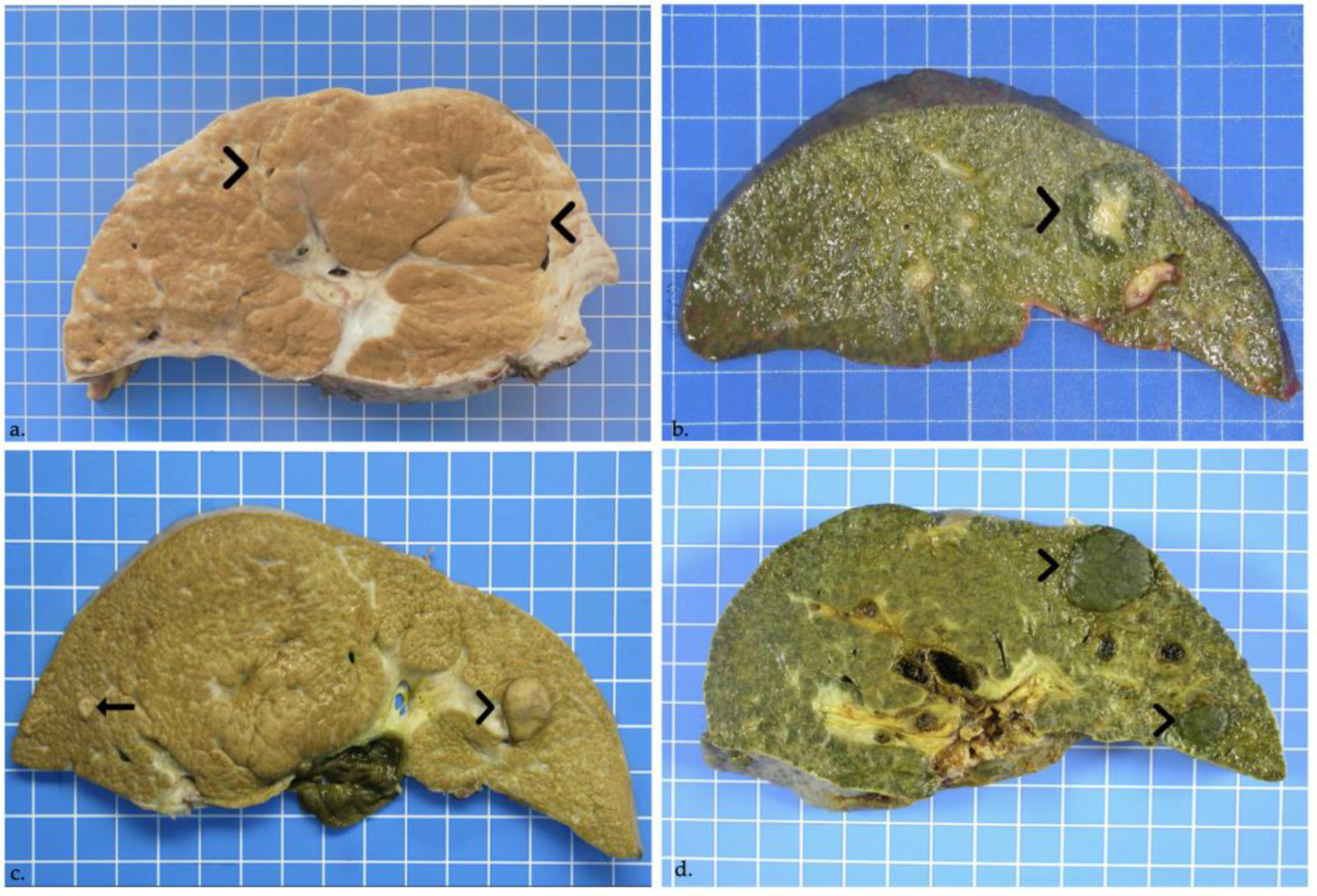
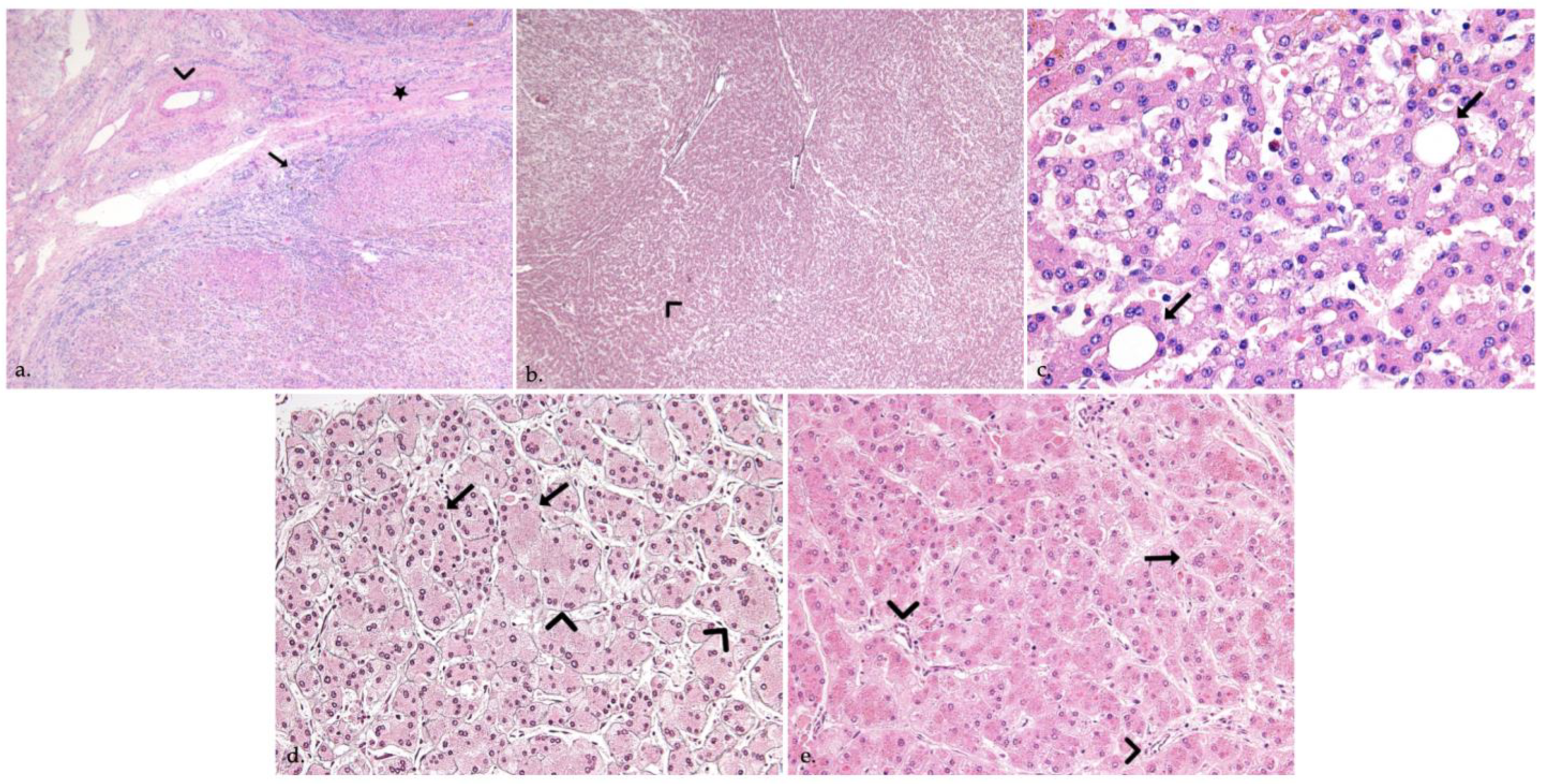
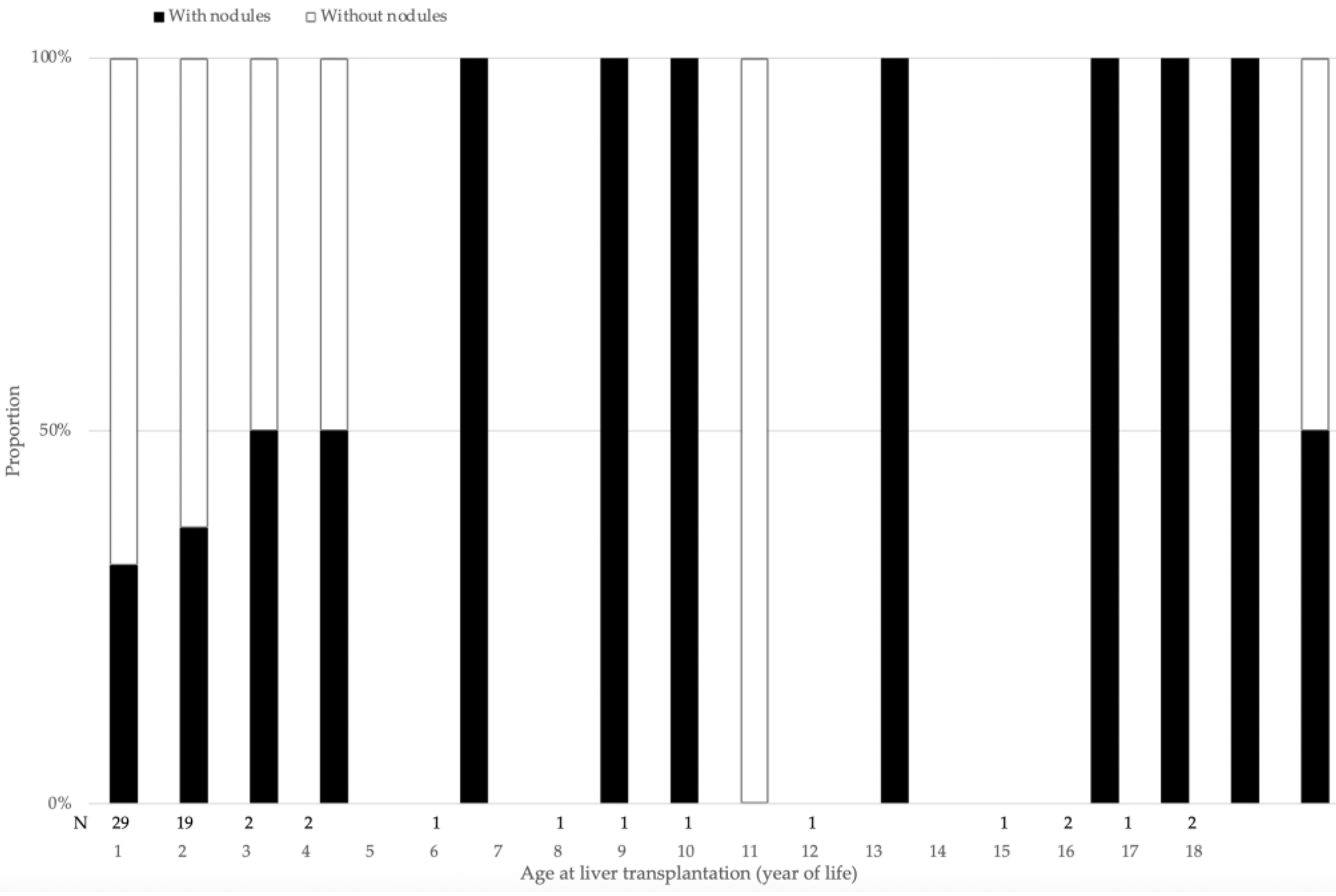
3.2. Nodules in Liver Explants
3.3. Correlation between Imaging and Histopathology
3.4. Patient Characteristics of Groups with and without Nodules in Liver Explants
4. Discussion
4.1. Half of Explants with Nodules
4.2. Features of Benign Nodules
4.2.1. Focal Nodular Hyperplasia
4.2.2. Regenerative Nodules
4.2.3. Other Benign Nodules
4.3. Features of Malignant Nodules
4.3.1. Hepatocellular Carcinoma
4.3.2. Dysplastic Nodules
4.3.3. Other Malignant Tumors
4.4. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnon, R.; Annunziato, R.A.; D’Amelio, G.; Chu, J.; Shneider, B.L. Liver Transplantation for Biliary Atresia: Is There a Difference in Outcome for Infants? J. Pediatr. Gastroenterol. Nutr. 2016, 62, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Tatekawa, Y.; Asonuma, K.; Uemoto, S.; Inomata, Y.; Tanaka, K. Liver transplantation for biliary atresia associated with malignant hepatic tumors. J. Pediatr. Surg. 2001, 36, 436–439. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.J.; Jeon, T.Y.; Yoo, S.Y.; Kim, J.H.; Eo, H.; Lee, S.K.; Kim, J.S. Hepatic tumours in children with biliary atresia: Single-centre experience in 13 cases and review of the literature. Clin. Radiol. 2014, 69, e113–e119. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.W.; Concejero, A.M.; Chen, C.L.; Cheng, Y.F.; Eng, H.L.; Huang, T.L.; Chen, T.Y.; Wang, C.C.; Wang, S.H.; Lin, C.C.; et al. Hepatic pseudotumor in long-standing biliary atresia patients undergoing liver transplantation. Liver Transplant. 2007, 13, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Libbrecht, L.; Bielen, D.; Verslype, C.; Vanbeckevoort, D.; Pirenne, J.; Nevens, F.; Desmet, V.; Roskams, T. Focal lesions in cirrhotic explant livers: Pathological evaluation and accuracy of pretransplantation imaging examinations. Liver Transplant. 2002, 8, 749–761. [Google Scholar] [CrossRef] [PubMed]
- Song, H.J.; Suh, Y. Newly formed hepatic masses in children with biliary atresia after Kasai Hepatic Portoenterostomy. Korean J. Pathol. 2011, 45, 160–169. [Google Scholar] [CrossRef]
- Ijiri, R.; Tanaka, Y.; Kato, K.; Misugi, K.; Ohama, Y.Y.; Shinkai, M.; Nishi, T.; Aida, N.; Kondo, F. Clinicopathological study of a hilar nodule in the livers of long-term survivors with biliary atresia. Pathol. Int. 2001, 51, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Itai, Y.; Matsui, O. Blood flow and liver imaging. Radiology 1997, 202, 306–314. [Google Scholar] [CrossRef]
- Hussein, A.; Wyatt, J.; Guthrie, A.; Stringer, M.D. Kasai portoenterostomy--new insights from hepatic morphology. J. Pediatr. Surg. 2005, 40, 322–326. [Google Scholar] [CrossRef]
- Hadzic, N.; Quaglia, A.; Portmann, B.; Paramalingam, S.; Heaton, N.D.; Rela, M.; Mieli-Vergani, G.; Davenport, M. Hepatocellular carcinoma in biliary atresia: King’s College Hospital experience. J. Pediatr. 2011, 159, 617–622.e1. [Google Scholar] [CrossRef]
- Tocchi, A.; Mazzoni, G.; Liotta, G.; Lepre, L.; Cassini, D.; Miccini, M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: A follow-up study of more than 1,000 patients. Ann. Surg. 2001, 234, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Chakhunashvili, K.; Pavlenishvili, I.; Kakabadze, M.; Kordzaia, D.; Chakhunashvili, D.; Kakabadze, Z. Biliary Atresia: Current Concepts and Future Prospects (Review). Georgian Med. News 2016, 104–111. [Google Scholar]
- Salzedas-Netto, A.A.; Chinen, E.; de Oliveira, D.F.; Pasquetti, A.F.; Azevedo, R.A.; da Silva Patricio, F.F.; Cury, E.K.; Gonzalez, A.M.; Vicentine, F.P.; Martins, J.L. Grade IV fibrosis interferes in biliary drainage after Kasai procedure. Transplant. Proc. 2014, 46, 1781–1783. [Google Scholar] [CrossRef] [PubMed]
- Sato, A.; Rai, T.; Takahashi, A.; Saito, H.; Takagi, T.; Shibukawa, G.; Wakatsuk, T.; Takahashi, Y.; Irisawa, A.; Ise, K.; et al. A case of rapidly expanding and increasing focal nodular hyperplasia. Fukushima J. Med. Sci 2006, 52, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Ohtomo, K.; Itai, Y.; Hasizume, K.; Kosaka, N.; Iio, M. CT and MR appearance of focal nodular hyperplasia of the liver in children with biliary atresia. Clin. Radiol. 1991, 43, 88–90. [Google Scholar] [CrossRef]
- Cha, D.I.; Yoo, S.Y.; Kim, J.H.; Jeon, T.Y.; Eo, H. Clinical and imaging features of focal nodular hyperplasia in children. AJR Am. J. Roentgenol. 2014, 202, 960–965. [Google Scholar] [CrossRef] [PubMed]
- Okugawa, Y.; Uchida, K.; Inoue, M.; Kawamoto, A.; Ohtake, K.; Sakurai, H.; Uchida, K.; Isaji, S.; Miki, C.; Kusunoki, M. Focal nodular hyperplasia in biliary atresia patient after Kasai hepatic portoenterostomy. Pediatr. Surg. Int. 2008, 24, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.L.; Cheng, Y.F.; Concejero, A.M.; Huang, T.L.; Chen, T.Y.; Tsang, L.L.; Ou, H.Y. Macro-regenerative nodules in biliary atresia: CT/MRI findings and their pathological relations. World J. Gastroenterol. 2008, 14, 4529–4534. [Google Scholar] [CrossRef] [PubMed]
- Rougemont, A.L.; McLin, V.A. Central Liver Nodules in Alagille Syndrome and Biliary Atresia After Kasai Portoenterostomy. J. Pediatr. Gastroenterol. Nutr. 2016, 63, e41–e42. [Google Scholar] [CrossRef] [PubMed]
- Lack, E.E. Mesenchymal hamartoma of the liver. A clinical and pathologic study of nine cases. Am. J. Pediatr. Hematol. Oncol. 1986, 8, 91–98. [Google Scholar] [PubMed]
- Esquivel, C.O.; Gutierrez, C.; Cox, K.L.; Garcia-Kennedy, R.; Berquist, W.; Concepcion, W. Hepatocellular carcinoma and liver cell dysplasia in children with chronic liver disease. J. Pediatr. Surg. 1994, 29, 1465–1469. [Google Scholar] [CrossRef]
- Van Wyk, J.; Halgrimson, C.G.; Giles, G.; Lilly, J.; Martineau, G.; Starzl, T.E. Liver transplantation in biliary atresia with concomitant hepatoma. S. Afr. Med. J. 1972, 46, 885–889. [Google Scholar] [PubMed]
- Okuyama, K. Primary Liver Cell Carcinoma Associated with Biliary Cirrhosis Due to Congenital Bile Duct Atresia. J. Pediatr. 1965, 67, 89–93. [Google Scholar] [CrossRef]
- Kohno, M.; Kitatani, H.; Wada, H.; Kajimoto, T.; Matuno, H.; Tanino, M.; Nakagawa, T.; Takarada, A. Hepatocellular carcinoma complicating biliary cirrhosis caused by biliary atresia: Report of a case. J. Pediatr. Surg. 1995, 30, 1713–1716. [Google Scholar] [CrossRef]
- Superina, R.; Bilik, R. Results of liver transplantation in children with unresectable liver tumors. J. Pediatr. Surg. 1996, 31, 835–839. [Google Scholar] [CrossRef]
- Hol, L.; van den Bos, I.C.; Hussain, S.M.; Zondervan, P.E.; de Man, R.A. Hepatocellular carcinoma complicating biliary atresia after Kasai portoenterostomy. Eur. J. Gastroenterol. Hepatol. 2008, 20, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Brunati, A.; Feruzi, Z.; Sokal, E.; Smets, F.; Fervaille, C.; Gosseye, S.; Clapuyt, P.; de Ville de Goyet, J.; Reding, R. Early occurrence of hepatocellular carcinoma in biliary atresia treated by liver transplantation. Pediatr. Transplant. 2007, 11, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Iida, T.; Zendejas, I.R.; Kayler, L.K.; Magliocca, J.F.; Kim, R.D.; Hemming, A.W.; Gonzalez-Peralta, R.P.; Fujita, S. Hepatocellular carcinoma in a 10-month-old biliary atresia child. Pediatr. Transplant. 2009, 13, 1048–1049. [Google Scholar] [CrossRef] [PubMed]
- Romano, F.; Stroppa, P.; Bravi, M.; Casotti, V.; Lucianetti, A.; Guizzetti, M.; Sonzogni, A.; Colledan, M.; D’Antiga, L. Favorable outcome of primary liver transplantation in children with cirrhosis and hepatocellular carcinoma. Pediatr. Transplant. 2011, 15, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Zen, Y.; Srinivasan, P.; Kitagawa, M.; Suzuki, K.; Heneghan, M.; Prachalias, A. De novo perihilar cholangiocarcinoma arising in the allograft liver 15 years post-transplantation for biliary atresia. Pathol. Int. 2020, 70, 563–567. [Google Scholar] [CrossRef]
- Hirzel, A.C.; Madrazo, B.; Rojas, C.P. Two Rare Cases of Hepatocellular Carcinoma after Kasai Procedure for Biliary Atresia: A Recommendation for Close Follow-Up. Case Rep. Pathol. 2015, 2015, 982679. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, J.M.; Lee, S.K.; Kwon, C.H.; Joh, J.W.; Choe, Y.H.; Park, C.K. Hepatocellular carcinoma in an infant with biliary atresia younger than 1 year. J. Pediatr. Surg. 2012, 47, 819–821. [Google Scholar] [CrossRef] [PubMed]
- Squires, J.H.; Bill, A.; Thieret, J.; Squires, J.E. Identification of Suspected Hepatocellular Carcinoma with Contrast-Enhanced Ultrasound. J. Pediatr. 2017, 182, 398–398.e1. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fang, C.; Anupindi, S.A.; Back, S.J.; Franke, D.; Green, T.G.; Harkanyi, Z.; Jungert, J.; Kwon, J.K.; Paltiel, H.J.; Squires, J.H.; et al. Contrast-enhanced ultrasound of benign and malignant liver lesions in children. Pediatr. Radiol. 2021, 51, 2181–2197. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Ikeda, K.; Hosaka, T.; Sezaki, H.; Someya, T.; Akuta, N.; Suzuki, F.; Suzuki, Y.; Saitoh, S.; Arase, Y.; et al. Dysplastic nodules frequently develop into hepatocellular carcinoma in patients with chronic viral hepatitis and cirrhosis. Cancer 2006, 106, 636–647. [Google Scholar] [CrossRef] [PubMed]
- Amir, A.Z.; Sharma, A.; Cutz, E.; Avitzur, Y.; Shaikh, F.; Kamath, B.M.; Ling, S.C.; Ghanekar, A.; Ng, V.L. Hepatoblastoma in Explanted Livers of Patients with Biliary Atresia. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Taat, F.; Bosman, D.K.; Aronson, D.C. Hepatoblastoma in a girl with biliary atresia: Coincidence or co-incidence. Pediatr. Blood Cancer 2004, 43, 603–605. [Google Scholar] [CrossRef] [PubMed]


| Patient | Age at LT (m) | Time KPE-LT (m) | Sex | Size (mm) | Location | US | CT Arterial/Portal Phases | AFP (µg/L) | Pathology |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 6 | 4 | F | 17 25 | IV | Hypoechoic Hypoechoic with central scar | Isodense/hypodense Isodense/hypodense with central scar | 363 | Macroregenerative nodule Focal nodular hyperplasia |
| 2 | 10 | 8 | F | 5 | V | No nodule | Hyperdense/hyperdense | 3255 | No nodule |
| 3 | 10 | 8 | M | 6 | VI | No | NA/Hyperdense | 12.9 | No nodule |
| 4 | 13 | 11 | M | 7 | IV | 4 Hyperechoic hilar nodules | Hypodense/hypodense segment IV Hypodense/hypodense segment III | 26.6 | Regenerative steatotic nodule |
| 5 | 15 | 14 | M | 11 | VI | Hyperechoic nodule | Isodense/hypodense | 7 | Regenerative steatotic nodule |
| 6 | 25 | 23 | F | 12 | Left lobe | 2 isoechoic nodules | No nodule | 1.6 | No nodule |
| 7 | 47 | 6 | M | 60 | III | Heterogeneous isoechoic | Isodense/isodense with a small central componenet hyperdense/hyperdense | 32.7 | Macroregenerative nodule |
| 8 | 66 | 65 | F | 30 | V | Isoechoic | NA | NA | Macroregenerative nodule |
| 9 | 84 | 83 | F | 30 60 | I V | No nodule | Isodense/isodense Isodense/hyperdense | 2.1 | Macroregenerative nodule |
| 10 | 133 | 132 | F | 30 | IV, VII, VIII | No nodule | Isodense/hypodense | 1 | Low-grade dysplastic nodule Regenerative cholestatic nodule |
| 11 | 174 | 173 | M | 80 | Diffuse | Isoechoic | Isodense/isodense | 2.6 | Macroregenerative nodules |
| 12 | 201 | 200 | F | 27 | III | No nodule | Isodense/isodense | 2.3 | High-grade dysplastic nodule |
| 13 | 203 | 201 | M | 16 | III | Hypoechoic nodule | No nodule | 2.2 | No nodule |
| Nodules | Nodule Type | Number of Nodules | Location * (Segments) | Size ** (mm) |
|---|---|---|---|---|
| Benign nodules | Macro regenerative nodules | 29/55 (53%) | 3xI/1xII/1xIII/8xIV/6xV/2xVI/ 5xVII/7xVIII | 9 (3–80) |
| Regenerative cholestatic nodules | 5/55 (9%) | 1xII/2xIII/1xVI/1xVII | 12 (6–60) | |
| Regenerative steatotic nodules | 3/55 (5%) | 1xIII/1xIV | 8.5 (5–12) | |
| Regenerative cholestatic and steatotic nodules | 1/55 (2%) | 1xVIII | 7 | |
| Focal nodular hyperplasia | 2/55 (4%) | 2xIV | 20 (15–25) | |
| Biliary infarction nodules | 1/55 (2%) | III | 17 | |
| Premalignant and malignant nodules | Low-grade dysplasia nodules | 3/55 (5%) | 2xIV/1xV | 7 (7–15) |
| High-grade dysplasia nodules | 7/55 (13%) | 1xII 2xIII/1xIV/ 2xV/1xVI | 7 (3–32) | |
| Hepatocellular carcinoma | 4/55 (7%) | 1xII/2xIII/1xV | 14.5 (7–23) |
| Characteristics | With Nodules (n = 27) | Without Nodules (n = 36) | p-Value |
|---|---|---|---|
| Age at LT (months) | 15 (5–207) | 11 (3–203) | <0.001 |
| KPE before LT | 26/27 (96.2%) | 34/36 (94.4%) | 0.78 |
| Age at Kasai (days) | 53 (18–87) | 64 (25–126) | 0.05 |
| Draining KPE at 6 months post KPE | 17/26 (65.3%) | 10/34 (29.4%) | 0.006 |
| Cholangitis episode(s) before LT | 16/26 (61.5%) | 23/34 (67.6%) | 0.63 |
| Portal hypertension | 23/27 (85.1%) | 32/36 (88.8%) | 0.67 |
| Direct bilirubin before LT (µmol/L) | 34 (13–169.5) | 163 (40–271.5) | 0.39 |
| Time period KPE to LT (months) | 17 (3–1412) | 8 (1–1338) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calinescu, A.M.; Rougemont, A.-L.; Anooshiravani, M.; Rock, N.M.; McLin, V.A.; Wildhaber, B.E. Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia. J. Clin. Med. 2022, 11, 1578. https://doi.org/10.3390/jcm11061578
Calinescu AM, Rougemont A-L, Anooshiravani M, Rock NM, McLin VA, Wildhaber BE. Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia. Journal of Clinical Medicine. 2022; 11(6):1578. https://doi.org/10.3390/jcm11061578
Chicago/Turabian StyleCalinescu, Ana M., Anne-Laure Rougemont, Mehrak Anooshiravani, Nathalie M. Rock, Valerie A. McLin, and Barbara E. Wildhaber. 2022. "Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia" Journal of Clinical Medicine 11, no. 6: 1578. https://doi.org/10.3390/jcm11061578
APA StyleCalinescu, A. M., Rougemont, A.-L., Anooshiravani, M., Rock, N. M., McLin, V. A., & Wildhaber, B. E. (2022). Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia. Journal of Clinical Medicine, 11(6), 1578. https://doi.org/10.3390/jcm11061578






