Cerebral Pulsatility Index and In-Hospital Mortality in Chinese Patients with Traumatic Brain Injury: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Study Population
2.3. Trauma Type and Treatment
2.4. Measurement of the PI Value
2.5. Covariates
2.6. Statistical Analysis
3. Results
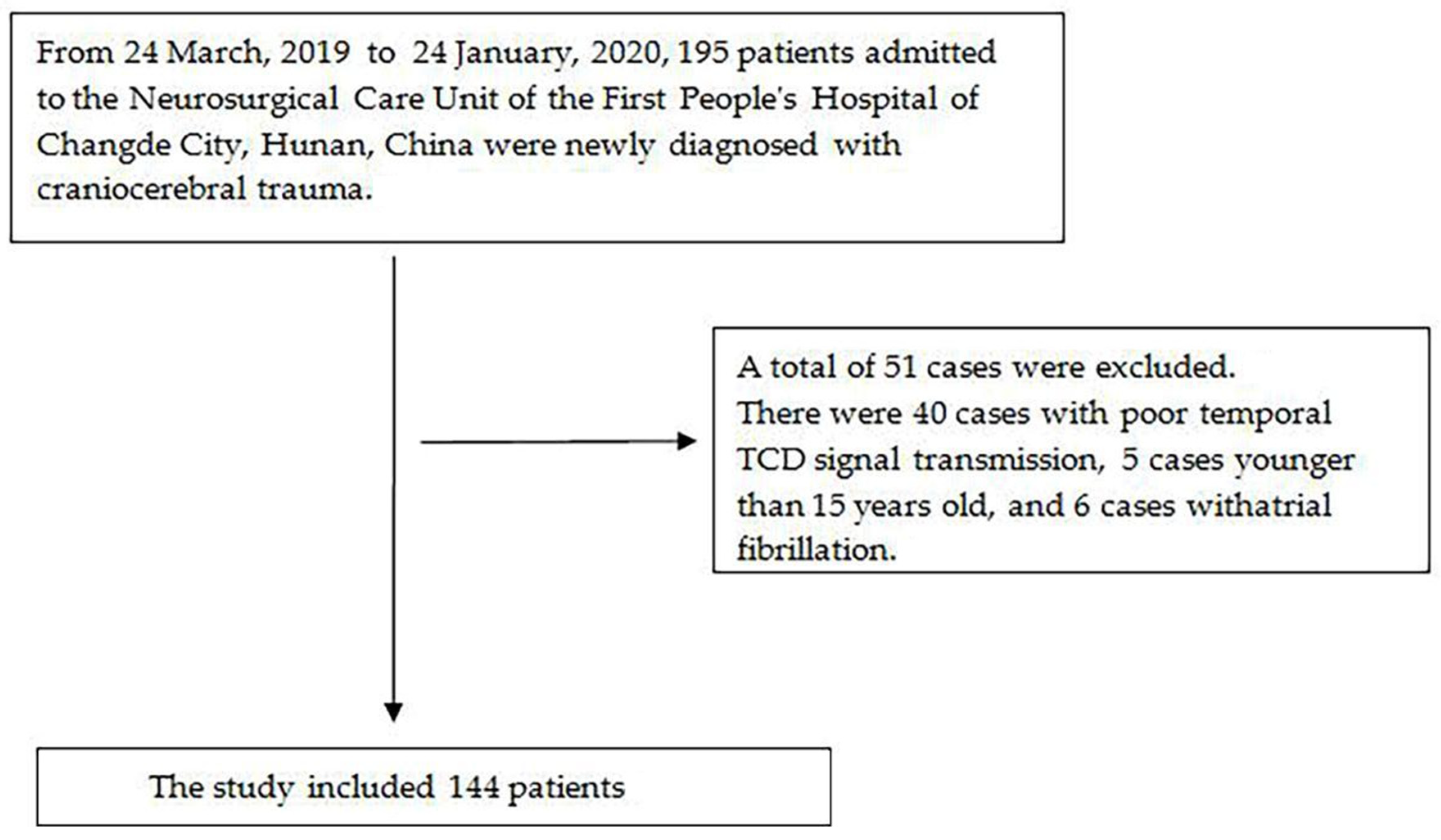
3.1. Participant Selection
3.2. Baseline Characteristics of the Selected Participants
3.3. Results of the Univariate Logistic Analysis
3.4. Results of theMultivariate Logistic Regression Models
3.5. The Nonlinear Relationship between PI and in-Hospital Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- D’Ambrosio, R.; Perucca, E. Epilepsy after head injury. Curr. Opin. Neurol. 2004, 17, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.D.; Carroll, L.J.; Peloso, P.M.; Borg, J.; von Holst, H.; Holm, L.; Kraus, J.; Coronado, V.G.; WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Incidence, risk factors and prevention of mild traumatic brain injury: Results of the WHO collaborating centre task force on mild traumatic brain injury. J. Rehabil. Med. 2004, 43, 28–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robba, C.; Cardim, D.; Sekhon, M.; Budohoski, K.; Czosnyka, M. Transcranial Doppler: A stethoscope for the brain-neurocritical care use. J. Neurosci. Res. 2018, 96, 720–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ract, C.; Le Moigno, S.; Bruder, N.; Vigué, B. Transcranial Doppler ultrasound goal-directed therapy for the early management of severe traumatic brain injury. Intensive Care Med. 2007, 33, 645–651. [Google Scholar] [CrossRef]
- Moreno, J.A.; Mesalles, E.; Gener, J.; Tomasa, A.; Ley, A.; Roca, J.; Fernández-Llamazares, J. Evaluating the outcome of severe head injury with transcranial Doppler ultrasonography. Neurosurg. Focus 2000, 8, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Ziegler, D.; Cravens, G.; Poche, G.; Gandhi, R.; Tellez, M. Use of transcranial Doppler in patients with severe traumatic brain injuries. J. Neurotrauma 2017, 34, 121–127. [Google Scholar] [CrossRef]
- Butterworth, J.E.; Prough, D.H.; Rippe, J.M. (Eds.) Intensive Care Medicine; Little, Brown: Boston, MA, USA, 1991; pp. 1459–1477. [Google Scholar]
- Czosnyka, M.; Richards, H.K.; Whitehouse, H.E.; Pickard, J.D. Relationship between transcranial Doppler-determined pulsatility index and cerebrovascular resistance: An experimental study. J. Neurosurg. 1996, 84, 79–84. [Google Scholar] [CrossRef] [Green Version]
- Lane, P.L.; Skoretz, T.G.; Doig, G.; Girotti, M.J. Intracranial pressure monitoring and outcomes after traumatic brain injury. Can. J. Surg. 2000, 43, 442–448. [Google Scholar]
- Bouzat, P.; Francony, G.; Declety, P.; Genty, C.; Kaddour, A.; Bessou, P.; Brun, J.; Jacquot, C.; Chabardes, S.; Bosson, J.L.; et al. Transcranial Doppler to screen on admission patients with mild to moderate traumatic brain injury. Neurosurgery 2011, 68, 1603–1609, discussion 1609–1610. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.; Li, L.; Yang, Y.; Li, M.; Qu, Y.; Gao, L. Transcranial Doppler Ultrasonography for the Management of Severe Traumatic Brain Injury After Decompressive Craniectomy. World Neurosurg. 2019, 126, e116–e124. [Google Scholar] [CrossRef]
- Titianova, E.; Velcheva, I.; Mateev, P. Effects of aging and hematocrit on cerebral blood flow velocity in patients with unilateral cerebral infarctions: A Doppler ultrasound evaluation. Angiology 1993, 44, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Tegeler, C.H.; Crutchfield, K.; Katsnelson, M.; Kim, J.; Tang, R.; Griffin, P. Transcranial Doppler velocities in a large, healthy population. J. Neuroimaging 2013, 23, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Bouzat, P.; Almeras, L.; Manhes, P.; Sanders, L.; Levrat, A.; David, J.S.; Cinotti, R.; Chabanne, R.; Gloaguen, A.; Bobbia, X.; et al. Transcranial Doppler to Predict Neurologic Outcome after Mild to Moderate Traumatic Brain Injury. Anesthesiology 2016, 125, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Jianlan, Z.; Qiang, Y.; Xing, W.; Jian, Y.; Zhuoying, D.; Yirui, S.; Xuehai, W.; Jin, H. Prediction value of blood coagulation index for in-hospital mortality in patients with craniocerebral trauma. Chin. J. Neurosurg. 2018, 34, 134. [Google Scholar]
- Yuan, F.; Ding, J.; Chen, H.; Guo, Y.; Wang, G.; Gao, W.W.; Chen, S.W.; Tian, H.L. Predicting outcomes after traumatic brain injury: The development and validation of prognostic models based on admission characteristics. J. Trauma Acute Care Surg. 2012, 73, 137–145. [Google Scholar] [CrossRef]
- Rosenfeld, J.V.; Maas, A.I.; Bragge, P.; Morganti-Kossmann, M.C.; Manley, G.T.; Gruen, R.L. Early management of severe traumatic brain injury. Lancet 2012, 380, 1088–1098. [Google Scholar] [CrossRef]
- Arlinghaus, K.A.; Shoaib, A.M.; Price, T.R. Neuropsychiatric assessment. In Textbook of Traumatic Brain Injury; Silver, J.M., McAllister, T.W., Yudofsky, S.C., Eds.; American Psychiatric Association: Washington, DC, USA, 2005; pp. 59–62. [Google Scholar]
- Martin, N.A.; Patwardhan, R.V.; Alexander, M.J.; Africk, C.Z.; Lee, J.H.; Shalmon, E.; Hovda, D.A.; Becker, D.P. Characterization of cerebral hemodynamic phases following severe head trauma: Hypoperfusion, hyperemia, and vasospasm. J. Neurosurg. 1997, 87, 9–19. [Google Scholar] [CrossRef]
- LaRovere, K.L.; O’Brien, N.F.; Tasker, R.C. Current Opinion and Use of Transcranial Doppler Ultrasonography in Traumatic Brain Injury in the Pediatric Intensive Care Unit. J. Neurotrauma 2016, 33, 2105–2114. [Google Scholar] [CrossRef]
- Splavski, B.; Radanović, B.; Vranković, D.; Has, B.; Mužević, D.; JanČuljak, D.; LegČević, J. Transcranial Doppler ultrasonography as an early outcome forecaster following severe brain injury. Br. J. Neurosurg. 2006, 20, 386–390. [Google Scholar] [CrossRef]
- Bellner, J.; Romner, B.; Reinstrup, P.; Kristiansson, K.; Ryding, E.; Brandt, L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg. Neurol. 2004, 62, 45–51. [Google Scholar] [CrossRef]
- Christou, I.; Felberg, R.A.; Demchuk, A.M.; Grotta, J.C.; Burgin, W.S.; Malkoff, M.; Alexandrov, A.V. A broad diagnostic battery for bedside transcranial Doppler to detect flow changes with internal carotid artery stenosis or occlusion. J. Neuroimaging 2001, 11, 236–242. [Google Scholar] [CrossRef]
- Fatima, N.; Shuaib, A.; Chughtai, T.S.; Ayyad, A.; Saqqur, M. The role of transcranial doppler in traumatic brain injury: A systemic review and meta-analysis. Asian J. Neurosurg. 2019, 14, 626–633. [Google Scholar] [CrossRef]
- Sawicki, K.; Placek, M.M.; Łysoń, T.; Mariak, Z.; Chrzanowski, R.; Czosnyka, M. Change in Blood Flow Velocity Pulse Waveform during Plateau Waves of Intracranial Pressure. Brain Sci. 2021, 11, 1000. [Google Scholar] [CrossRef]
- Lewis, J.R.; Sauro, J. When 100% really isn’t 100%: Improving the accuracy of small-sample estimates of completion rates. J. Usability Stud. 2006, 1, 136–150. [Google Scholar]
- Naqvi, J.; Yap, K.H.; Ahmad, G.; Ghosh, J. Transcranial Doppler ultrasound: A review of the physical principles and major applications in critical care. Int. J. Vasc. Med. 2013, 2013, 629378. [Google Scholar] [CrossRef]
- Armitage, P.; Berry, G.; Matthews, J.N. Statistical Methods in Medical Research, 4th ed.; Blackwell: Oxford, UK, 2002. [Google Scholar]

| Characteristics | PI Tertiles | p-Value | ||
|---|---|---|---|---|
| T1 (0.56–0.81) | T2 (0.82–1.01) | T3 (1.02–2.11) | ||
| Number of participants | 47 | 48 | 49 | |
| Age (years, mean ± SD) | 52.34 ± 15.77 | 54.60 ± 15.95 | 59.71 ± 14.38 | 0.058 |
| Trauma time before admission (hours, median, Q1–Q3) | 15.53 ± 42.46 | 10.82 ± 17.99 | 12.74 ± 26.43 | 0.753 |
| Hemoglobin count (g/L, mean ± SD) | 118.13 ± 20.17 | 116.08 ± 20.94 | 113.63 ± 22.25 | 0.582 |
| Na+ concentration (mmol/L, mean ± SD) | 139.48 ± 3.53 | 139.60 ± 4.16 | 140.24 ± 4.27 | 0.604 |
| Blood transfusion volume (mL, median, Q1–Q3) | 158.72 ± 306.33 | 361.70 ± 607.31 | 954.08 ± 885.70 | <0.001 |
| Gender | 0.478 | |||
| Male | 33 (70.21%) | 38 (79.17%) | 39 (79.59%) | |
| Female | 14 (29.79%) | 10 (20.83%) | 10 (20.41%) | |
| Diabetes | 0.732 | |||
| No | 45 (95.74%) | 45 (93.75%) | 45 (91.84%) | |
| Yes | 2 (4.26%) | 3 (6.25%) | 4 (8.16%) | |
| Hypertension | 0.182 | |||
| No | 44 (93.62%) | 39 (81.25%) | 41 (83.67%) | |
| Yes | 3 (6.38%) | 9 (18.75%) | 8 (16.33%) | |
| PLR | <0.001 | |||
| Bilateral PLR exhibition | 42(89.36%) | 41 (85.42%) | 22 (44.90%) | |
| Unilateral PLR loss | 5 (10.64%) | 4 (8.33%) | 7 (14.29%) | |
| Bilateral PLR loss | 0 (0.00%) | 3 (6.25%) | 20 (40.82%) | |
| GCS | <0.001 | |||
| 3–8 | 11 (23.40%) | 26 (54.17%) | 38 (77.55%) | |
| 9–12 | 18 (38.30%) | 14 (29.17%) | 6 (12.24%) | |
| 13–15 | 18 (38.30%) | 8 (16.67%) | 5 (10.20%) | |
| Shock | 0.015 | |||
| No | 45 (95.74%) | 44 (91.67%) | 38 (77.55%) | |
| Yes | 2 (4.26%) | 4 (8.33%) | 11 (22.45%) | |
| Traumatic coagulopathy | 0.716 | |||
| No | 39 (82.98%) | 40 (83.33%) | 38 (77.55%) | |
| Yes | 8 (17.02%) | 8 (16.67%) | 11 (22.45%) | |
| Sedation and analgesia | 0.812 | |||
| No | 2 (4.26%) | 1 (2.08%) | 2 (4.08%) | |
| Yes | 45 (95.74%) | 47 (97.92%) | 47 (95.92%) | |
| Use of ventilator | <0.001 | |||
| No | 25 (53.19%) | 22 (45.83%) | 4 (8.16%) | |
| Yes | 22 (46.81%) | 26 (54.17%) | 45 (91.84%) | |
| PTCI | <0.001 | |||
| No | 47 (100.00%) | 44 (91.67%) | 37 (75.51%) | |
| Yes | 0 (0.00%) | 4 (8.33%) | 12 (24.49%) | |
| DC | <0.001 | |||
| No | 37 (78.72%) | 37 (77.08%) | 15 (30.61%) | |
| Yes | 10 (21.28%) | 11 (22.92%) | 34 (69.39%) | |
| In-hospital mortality | <0.001 | |||
| No | 47 (100.00%) | 45 (93.75%) | 17 (34.69%) | |
| Yes | 0 (0.00%) | 3 (6.25%) | 32 (65.31%) | |
| Covariate | Statistics | In-Hospital Mortality | |
|---|---|---|---|
| Age, years | 55.60 ± 15.58 | 1.03 (1.00, 1.06) | 0.0759 |
| Gender | |||
| Male | 110 (76.39%) | Reference | |
| Female | 34 (23.61%) | 1.16 (0.48, 2.80) | 0.7364 |
| Diabetes | |||
| No | 135 (93.75%) | Reference | |
| Yes | 9 (6.25%) | 2.68 (0.68, 10.61) | 0.1592 |
| Hypertension | |||
| No | 124 (86.11%) | Reference | |
| Yes | 20 (13.89%) | 1.04 (0.35, 3.11) | 0.9378 |
| PLR | |||
| Bilateral PLR exhibition | 105 (72.92%) | Reference | |
| Unilateral PLR loss | 16 (11.11%) | 4.25 (1.32, 13.64) | 0.0151 |
| Bilateral PLR loss | 23 (15.97%) | 16.18 (5.60, 46.75) | <0.0001 |
| GCS | |||
| 13–15 | 75 (52.08%) | Reference | |
| 9–12 | 38 (26.39%) | 0.20 (0.06, 0.62) | 0.0052 |
| 3–8 | 31 (21.53%) | 0.18 (0.05, 0.65) | 0.0086 |
| Shock | |||
| No | 127 (88.19%) | Reference | |
| Yes | 17 (11.81%) | 5.83 (2.02, 16.83) | 0.0011 |
| Use of ventilator | |||
| No | 51 (35.42%) | Reference | |
| Yes | 93 (64.58%) | 13.47 (3.08, 58.96) | 0.0006 |
| PTCI | |||
| No | 128 (88.89%) | Reference | |
| Yes | 16 (11.11%) | 6.87 (2.28, 20.68) | 0.0006 |
| DC | |||
| No | 89 (61.81%) | Reference | |
| Yes | 55 (38.19%) | 9.76 (3.98, 23.98) | <0.0001 |
| PI | 1.03 ±0.45 | 1.85 (1.48, 2.31) | <0.0001 |
| Blood transfusion volume, mL | 497.97 ± 728.75 | 1.00 (1.00, 1.00) | <0.0001 |
| Trauma time before admission, hours | 13.01 ± 30.41 | 0.95 (0.90, 1.01) | 0.0773 |
| Hemoglobin count, g/L | 115.92 ± 21.09 | 0.99 (0.97, 1.01) | 0.2110 |
| Na+ concentration, mmol/L | 139.78 ± 3.99 | 0.94 (0.85, 1.03) | 0.1872 |
| Traumatic coagulopathy | |||
| No | 117 (81.25%) | Reference | |
| Yes | 27 (18.75%) | 1.40 (0.55, 3.56) | 0.4756 |
| Sedation and analgesia | |||
| No | 5 (3.47%) | Reference | |
| Yes | 139 (96.53%) | 1.30 (0.14, 11.99) | 0.8198 |
| Variable OR (95% CI) p-Value | Non-Adjusted OR (95% CI) p-Value | Adjust I OR (95% CI) p-Value | Adjust II OR (95% CI) p-Value |
|---|---|---|---|
| PI * | 1.92 (1.54, 2.40) <0.0001 | 1.93 (1.54, 2.42) <0.0001 | 1.88 (1.35, 2.60) <0.001 |
| Inflection Point of PI | Non-Adjusted OR (95% CI) p-Value | Adjust I OR (95% CI) p-Value | Adjust II OR (95% CI) p-Value |
|---|---|---|---|
| <1.11 * | 4.19 (1.84, 9.56) 0.0006 | 4.30 (1.87, 9.88) 0.0006 | 4.09 (1.30, 12.83) 0.0158 |
| ≥1.11 * | 1.41 (1.06, 1.86) 0.0163 | 1.40 (1.06, 1.86) 0.0172 | 1.42 (0.93, 2.17) 0.1064 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mei, T.; Zhou, Q.; Chen, L.; Jia, Z.; Xiao, W.; Xu, L. Cerebral Pulsatility Index and In-Hospital Mortality in Chinese Patients with Traumatic Brain Injury: A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 1559. https://doi.org/10.3390/jcm11061559
Mei T, Zhou Q, Chen L, Jia Z, Xiao W, Xu L. Cerebral Pulsatility Index and In-Hospital Mortality in Chinese Patients with Traumatic Brain Injury: A Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(6):1559. https://doi.org/10.3390/jcm11061559
Chicago/Turabian StyleMei, Tao, Quan Zhou, Lie Chen, Zheyong Jia, Wei Xiao, and Lixin Xu. 2022. "Cerebral Pulsatility Index and In-Hospital Mortality in Chinese Patients with Traumatic Brain Injury: A Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 6: 1559. https://doi.org/10.3390/jcm11061559
APA StyleMei, T., Zhou, Q., Chen, L., Jia, Z., Xiao, W., & Xu, L. (2022). Cerebral Pulsatility Index and In-Hospital Mortality in Chinese Patients with Traumatic Brain Injury: A Retrospective Cohort Study. Journal of Clinical Medicine, 11(6), 1559. https://doi.org/10.3390/jcm11061559





