Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Interventional Procedures
2.4. Ophthalmological Examinations
2.5. Main Outcome Measures
2.6. Statistical Analysis
3. Results
3.1. Patient Demographics and Baseline Characteristics
3.2. Comparison between the Two Groups after the Three Monthly Loading Injections of Aflibercept
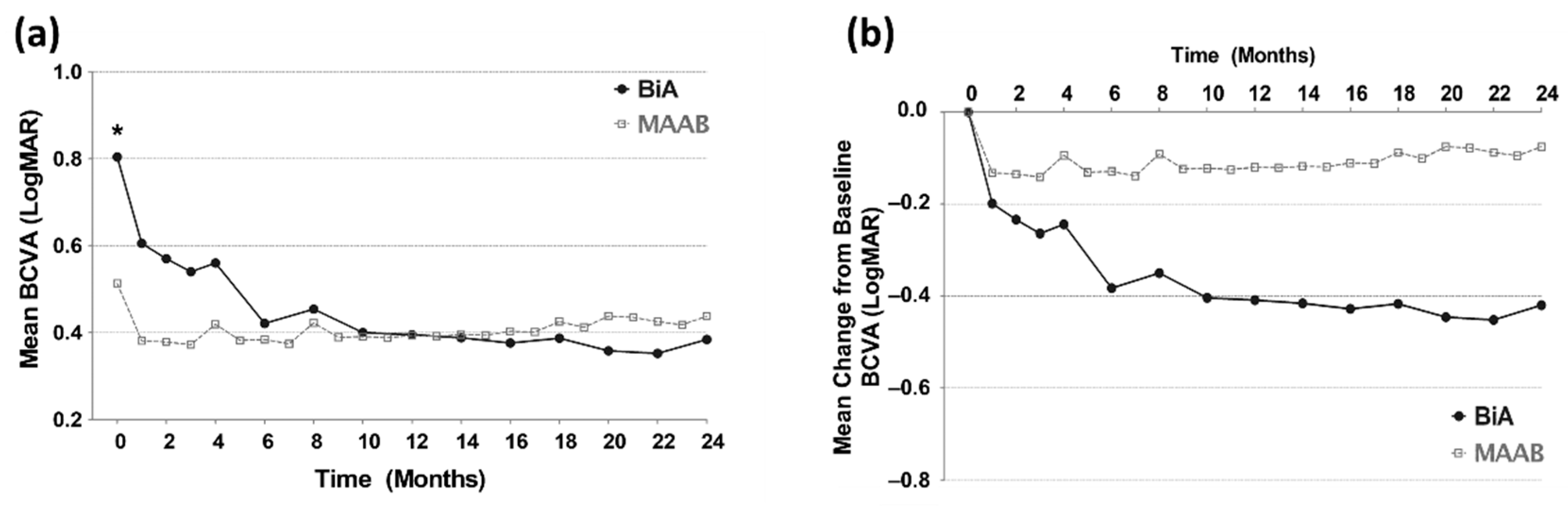
3.3. Visual Outcomes from Baseline to the 24th Month
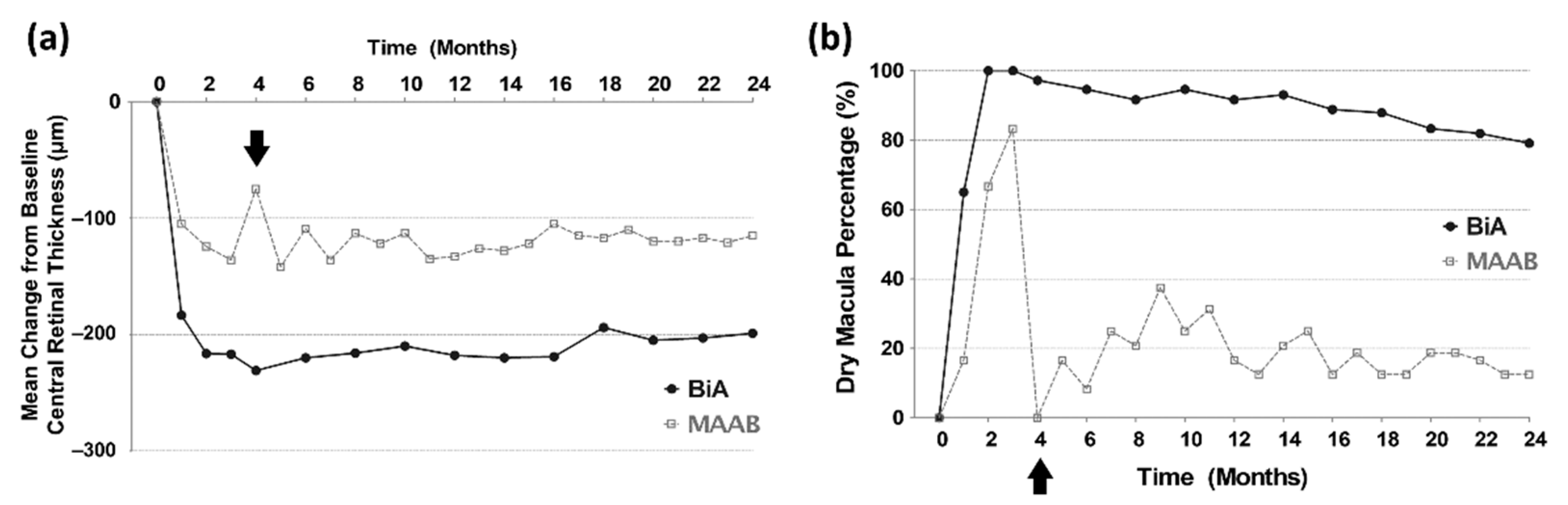
3.4. Anatomical Outcomes from Baseline to the 24th Month
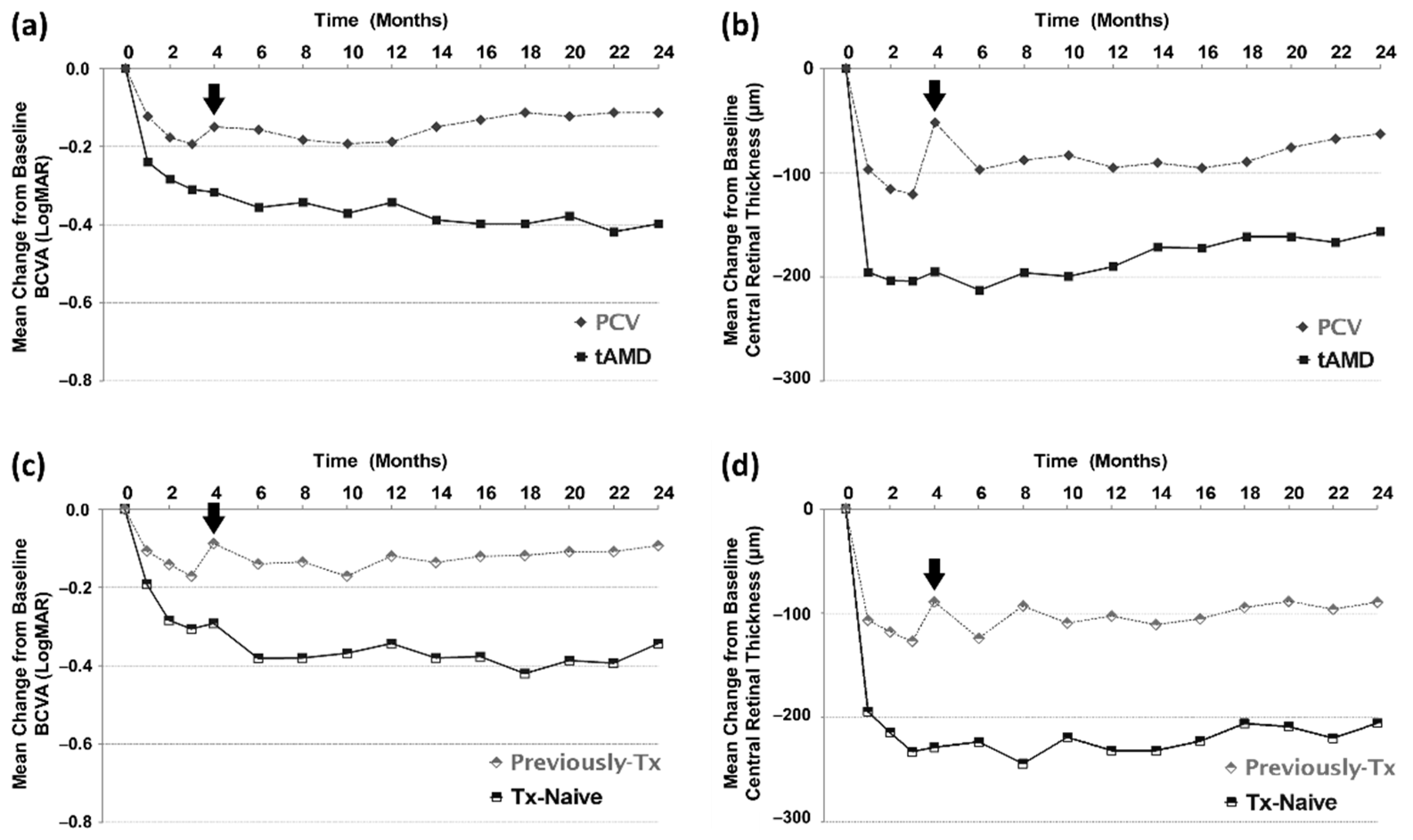
3.5. Subgroup Analyses
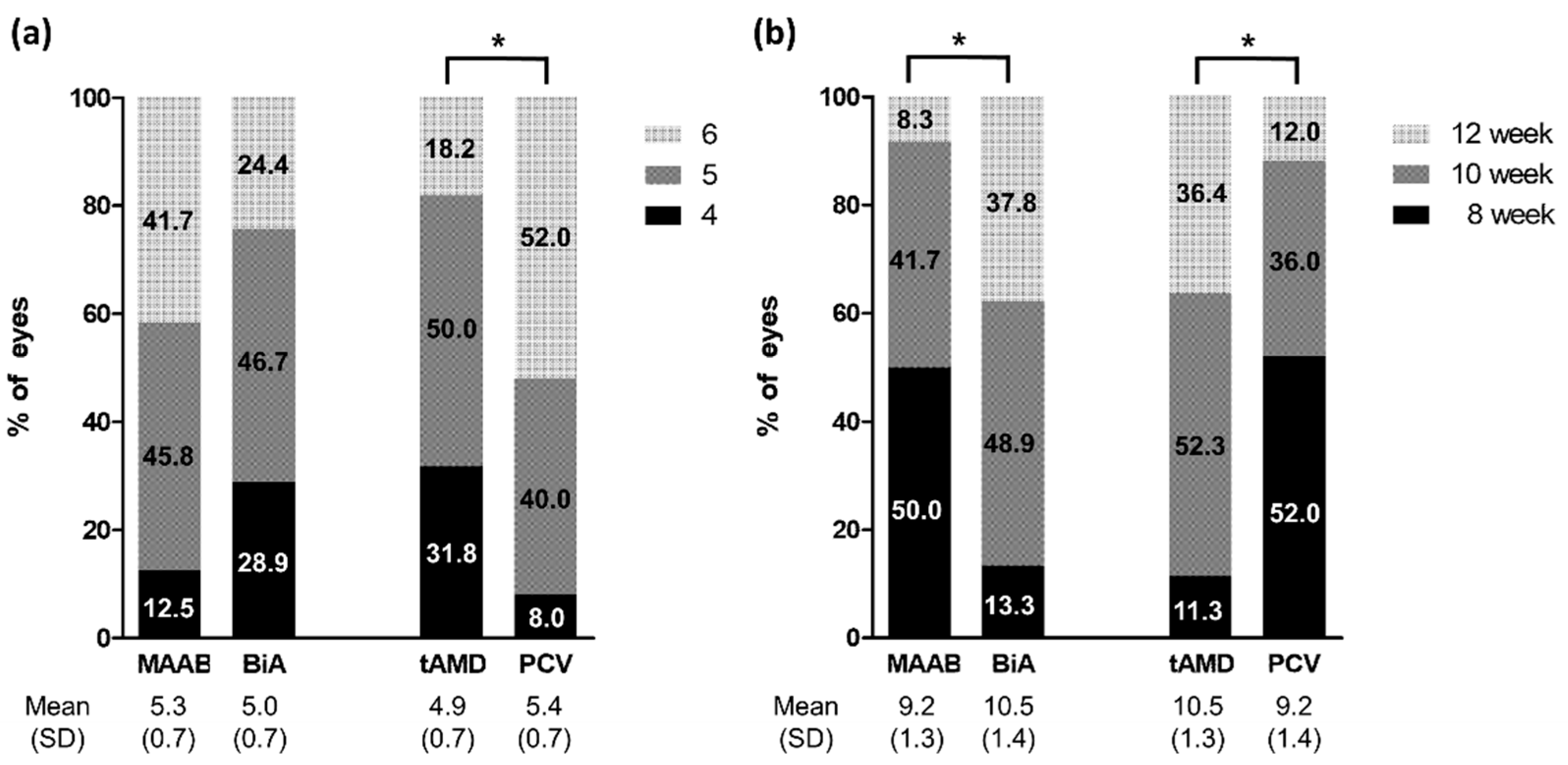
3.6. Change in Treatment Protocols in the Second Year
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jager, R.D.; Mieler, W.F.; Miller, J.W. Age-related macular degeneration. N. Engl. J. Med. 2008, 358, 2606–2617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, L.S.; Mitchell, P.; Seddon, J.M.; Holz, F.G.; Wong, T.Y. Age-related macular degeneration. Lancet 2012, 379, 1728–1738. [Google Scholar] [CrossRef]
- Holash, J.; Davis, S.; Papadopoulos, N.; Croll, S.D.; Ho, L.; Russell, M.; Boland, P.; Leidich, R.; Hylton, D.; Burova, E.; et al. VEGF-Trap: A VEGF blocker with potent antitumor effects. Proc. Natl. Acad. Sci. USA 2002, 99, 11393–11398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Kaiser, P.K.; Korobelnik, J.F.; Brown, D.M.; Chong, V.; Nguyen, Q.D.; Ho, A.C.; Ogura, Y.; Simader, C.; Jaffe, G.J.; et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: Ninety-six-week results of the VIEW studies. Ophthalmology 2014, 121, 193–201. [Google Scholar] [CrossRef]
- Jorstad, O.K.; Faber, R.T.; Moe, M.C. Initial improvements when converting eyes with treatment-resistant exudative AMD to aflibercept are substantially diminished after increasing treatment intervals from 4 to 8 weeks. Acta Ophthalmol. 2015, 93, e510–e511. [Google Scholar] [CrossRef]
- Chang, A.A.; Li, H.; Broadhead, G.K.; Hong, T.; Schlub, T.E.; Wijeyakumar, W.; Zhu, M. Intravitreal aflibercept for treatment-resistant neovascular age-related macular degeneration. Ophthalmology 2014, 121, 188–192. [Google Scholar] [CrossRef]
- Khanani, A.M. Clinical experience with fixed bimonthly aflibercept dosing in treatment-experienced patients with neovascular age-related macular degeneration. Clin. Ophthalmol. 2015, 9, 1315–1320. [Google Scholar] [CrossRef] [Green Version]
- Dans, K.C.; Freeman, S.R.; Lin, T.; Meshi, A.; Olivas, S.; Cheng, L.; Amador-Patarroyo, M.J.; Freeman, W.R. Durability of every-8-week aflibercept maintenance therapy in treatment-experienced neovascular age-related macular degeneration. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 741–748. [Google Scholar] [CrossRef]
- Barthelmes, D.; Nguyen, V.; Daien, V.; Campain, A.; Walton, R.; Guymer, R.; Morlet, N.; Hunyor, A.P.; Essex, R.W.; Arnold, J.J.; et al. Two Year Outcomes of “Treat and Extend” Intravitreal Therapy Using Aflibercept Preferentially for Neovascular Age-Related Macular Degeneration. Retina 2018, 38, 20–28. [Google Scholar] [CrossRef]
- Papadopoulos, N.; Martin, J.; Ruan, Q.; Rafique, A.; Rosconi, M.P.; Shi, E.; Pyles, E.A.; Yancopoulos, G.D.; Stahl, N.; Wiegand, S.J. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis 2012, 15, 171–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.; Wang, X.; Fuh, G.; Yu, L.; Wakshull, E.; Khosraviani, M.; Day, E.S.; Demeule, B.; Liu, J.; Shire, S.J.; et al. Comparison of binding characteristics and in vitro activities of three inhibitors of vascular endothelial growth factor A. Mol. Pharm. 2014, 11, 3421–3430. [Google Scholar] [CrossRef] [PubMed]
- Platania, C.B.; Di Paola, L.; Leggio, G.M.; Romano, G.L.; Drago, F.; Salomone, S.; Bucolo, C. Molecular features of interaction between VEGFA and anti-angiogenic drugs used in retinal diseases: A computational approach. Front. Pharmacol. 2015, 6, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.J.; Oh, J.; Kim, Y.K.; Park, J.H.; Park, J.Y.; Hong, H.K.; Park, K.H.; Lee, J.E.; Kim, H.M.; Chung, J.Y.; et al. Intraocular pharmacokinetics of intravitreal vascular endothelial growth factor-Trap in a rabbit model. Eye 2015, 29, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.; Lum, F.; Wood, K.; Salman, C.; Burugapalli, B.; Hall, R.; Singh, S.; Parke, D.W., 2nd; Williams, G.A. Real-World Vision in Age-Related Macular Degeneration Patients Treated with Single Anti-VEGF Drug Type for 1 Year in the IRIS Registry. Ophthalmology 2018, 125, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Neves Cardoso, P.; Pinheiro, A.F.; Meira, J.; Pedrosa, A.C.; Falcao, M.S.; Pinheiro-Costa, J.; Falcao-Reis, F.; Carneiro, A.M. Switch to Aflibercept in the Treatment of Neovascular AMD: Long-Term Results. J. Ophthalmol. 2017, 2017, 6835782. [Google Scholar] [CrossRef] [Green Version]
- Slean, G.R.; Hemarat, K.; Khurana, R.N.; Stewart, J.M. Conversion back to bevacizumab or ranibizumab for recurrent neovascular activity with aflibercept in age-related macular degeneration: A case series. Int. J. Retin. Vitr. 2016, 2, 2. [Google Scholar] [CrossRef] [Green Version]
- Waizel, M.; Rickmann, A.; Blanke, B.R.; Wolf, K.; Kazerounian, S.; Szurman, P. Response to bevacizumab after treatment with aflibercept in eyes with neovascular AMD. Eur. J. Ophthalmol. 2016, 26, 469–472. [Google Scholar] [CrossRef]
- Mimouni, M.; Meshi, A.; Vainer, I.; Gershoni, A.; Koren, T.; Geffen, N.; Nemet, A.Y.; Segal, O. Bevacizumab dosing every 2 weeks for neovascular age-related macular degeneration refractory to monthly dosing. Jpn. J. Ophthalmol. 2018, 62, 652–658. [Google Scholar] [CrossRef]
- Cheng, S.; Leng, T. Factors Associated With Poor Response to Aflibercept After Switching From Ranibizumab or Bevacizumab in Neovascular Age-related Macular Degeneration. Ophthalmic Surg. Lasers Imaging Retin. 2016, 47, 458–465. [Google Scholar] [CrossRef]
- Wakazono, T.; Yamashiro, K.; Oishi, A.; Ooto, S.; Tamura, H.; Akagi-Kurashige, Y.; Hata, M.; Takahashi, A.; Tsujikawa, A.; Yoshimura, N. Recurrence of Choroidal Neovascularization Lesion Activity after Aflibercept Treatment for Age-Related Macular Degeneration. Retina 2017, 37, 2062–2068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagai, N.; Suzuki, M.; Uchida, A.; Kurihara, T.; Kamoshita, M.; Minami, S.; Shinoda, H.; Tsubota, K.; Ozawa, Y. Non-responsiveness to intravitreal aflibercept treatment in neovascular age-related macular degeneration: Implications of serous pigment epithelial detachment. Sci. Rep. 2016, 6, 29619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koizumi, H.; Kano, M.; Yamamoto, A.; Saito, M.; Maruko, I.; Sekiryu, T.; Okada, A.A.; Iida, T. Subfoveal Choroidal Thickness during Aflibercept Therapy for Neovascular Age-Related Macular Degeneration: Twelve-Month Results. Ophthalmology 2016, 123, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.C.; Choi, S.; Koh, H.J. Inner nuclear layer cystoid spaces are a poor prognostic factor in typical age-related macular degeneration and polypoidal choroidal vasculopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 2157–2163. [Google Scholar] [CrossRef] [PubMed]
- Kokame, G.T.; Yeung, L.; Lai, J.C. Continuous anti-VEGF treatment with ranibizumab for polypoidal choroidal vasculopathy: 6-month results. Br. J. Ophthalmol. 2010, 94, 297–301. [Google Scholar] [CrossRef]
- Tsujikawa, A.; Ooto, S.; Yamashiro, K.; Tamura, H.; Otani, A.; Yoshimura, N. Treatment of polypoidal choroidal vasculopathy by intravitreal injection of bevacizumab. Jpn. J. Ophthalmol. 2010, 54, 310–319. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.E.; Shin, J.P.; Kim, H.W.; Chang, W.; Kim, Y.C.; Lee, S.J.; Chung, I.Y.; Lee, J.E.; VAULT Study Group. Efficacy of fixed-dosing aflibercept for treating polypoidal choroidal vasculopathy: 1-year results of the VAULT study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 493–502. [Google Scholar] [CrossRef] [Green Version]

| Total | MAAB Group | BiA Group | p Value | |
|---|---|---|---|---|
| Age (years) | 68.8 ± 10.1 | 65.1 ± 6.8 | 70.6 ± 10.9 | 0.012 |
| Sex (M/F) | 42/30 | 18/6 | 24/24 | 0.048 |
| Lens (phakic/pseudophakic) | 56/16 | 22/2 | 34/14 | 0.070 |
| Previous treatments (previously treated/treatment-naïve) | 32/40 | 18/6 | 14/34 | 0.001 |
| Refractive error (diopter) | 0.090 ± 1.280 | 0.000 ± 1.552 | 0.135 ± 1.137 | 0.675 |
| Baseline BCVA (Log MAR) | 0.707 ± 0.394 | 0.513 ± 0.209 | 0.804 ± 0.429 | 0.001 |
| Baseline Angiographic finding | ||||
| Type of AMD (tAMD/PCV/RAP) | 44/25/3 | 9/15/0 | 35/10/3 | 0.002 |
| Area of CNV (mm2) | 0.904 ± 1.066 | 1.426 ± 0.689 | 0.631 ± 1.131 | 0.001 |
| Baseline OCT findings | ||||
| CRT (um) | 437.5 ± 121.4 | 386.7 ± 68.9 | 462.9 ± 134.1 | 0.002 |
| Maximum height of PED (um) | 238.1 ± 143.9 | 246.7 ± 120.7 | 233.8 ± 155.24 | 0.724 |
| Subfoveal choroidal thickness (um) | 239.7 ± 86.3 | 282.8 ± 95.1 | 218.1 ± 73.55 | 0.002 |
| Presence of IRF (yes/no) | 44/28 | 23/1 | 21/27 | 0.001 |
| Presence of SRF (yes/no) | 72/0 | 24/0 | 48/0 | NA |
| Total | MAAB Group | BiA Group | p Value | |
|---|---|---|---|---|
| Δ BCVA | −0.038 ± 0.239 | −0.042 ± 0.156 | −0.035 ± 0.273 | 0.918 |
| Angiographic findings | ||||
| CNV area (3 month/baseline, fold) | 0.49 ± 0.22 | 0.54 ± 0.25 | 0.48 ± 0.21 | 0.336 |
| OCT findings | ||||
| Δ CRT (um) | −185.1 ± 136.0 | −124.4 ± 72.1 | −216.4 ± 150.1 | 0.001 |
| PED height (3 month/baseline, fold) | 0.63 ± 0.41 | 0.87 ± 0.17 | 0.51 ± 0.44 | 0.001 |
| Choroidal thickness (3 month/baseline, fold) | 0.95 ± 0.16 | 0.91 ± 0.16 | 0.98 ± 0.17 | 0.072 |
| Dry macula (N, %) at 3 month | 64 (88.9) | 16 (66.7) | 48 (100) | 0.001 |
| MAAB Group | BiA Group | |||||
|---|---|---|---|---|---|---|
| tAMD (N = 9) | PCV (N = 15) | p Value | tAMD (N = 35) | PCV (N = 10) | p Value | |
| Number of aflibercept injection in Year 2 | 4.7 ± 0.5 | 5.7 ± 0.5 | 0.001 | 4.9 ± 0.7 | 5.1 ± 0.7 | 0.489 |
| Last aflibercept injection interval (wk) | 10.0 ± 1.4 | 8.7 ± 1.0 | 0.012 | 10.6 ± 1.2 | 10.0 ± 1.5 | 0.200 |
| Number of bevacizumab injection Year 2 | 2.9 ± 0.8 | 5.6 ± 0.5 | 0.001 | NA | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Kim, Y.N.; Kim, J.-G. Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration. J. Clin. Med. 2022, 11, 1543. https://doi.org/10.3390/jcm11061543
Lee J, Kim YN, Kim J-G. Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration. Journal of Clinical Medicine. 2022; 11(6):1543. https://doi.org/10.3390/jcm11061543
Chicago/Turabian StyleLee, Junyeop, You Na Kim, and June-Gone Kim. 2022. "Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration" Journal of Clinical Medicine 11, no. 6: 1543. https://doi.org/10.3390/jcm11061543
APA StyleLee, J., Kim, Y. N., & Kim, J.-G. (2022). Monthly Alternating Injections of Aflibercept and Bevacizumab for Neovascular Age-Related Macular Degeneration. Journal of Clinical Medicine, 11(6), 1543. https://doi.org/10.3390/jcm11061543






